Effect of 4 Weeks of Cervical Deep Muscle Flexion Exercise on Headache and Sleep Disorder in Patients with Tension Headache and Forward Head Posture
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Participants
2.3. Procedures
2.4. Intervention
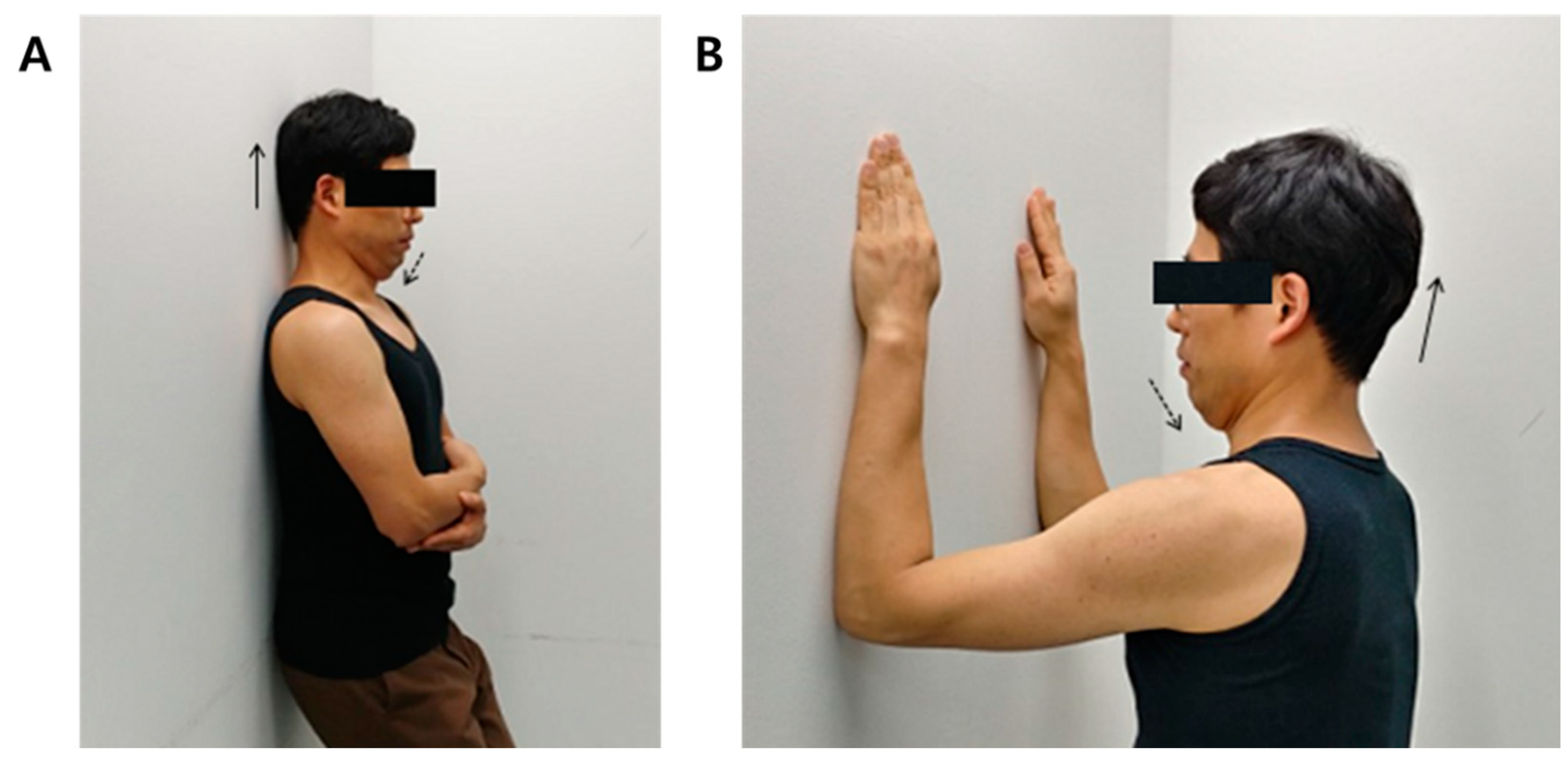
2.4.1. Cervical Deep Muscle Flexion Exercise
General Isometric Movement
Pressure Biofeedback Exercise
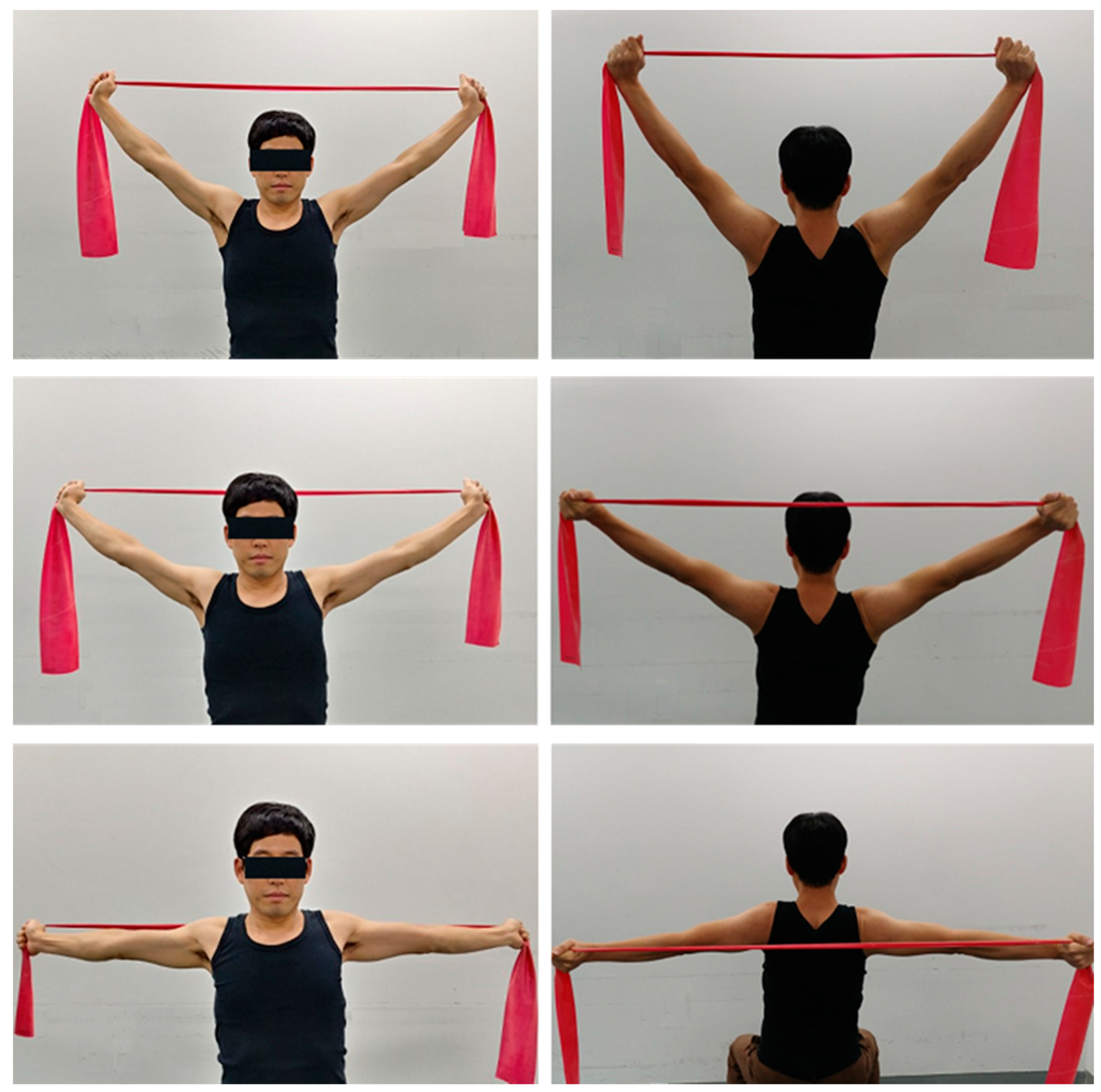
2.4.2. Stretching Exercise
Pectoralis Major and Minor Stretching
Levator Scapulae Stretching
Upper Trapezius Stretching
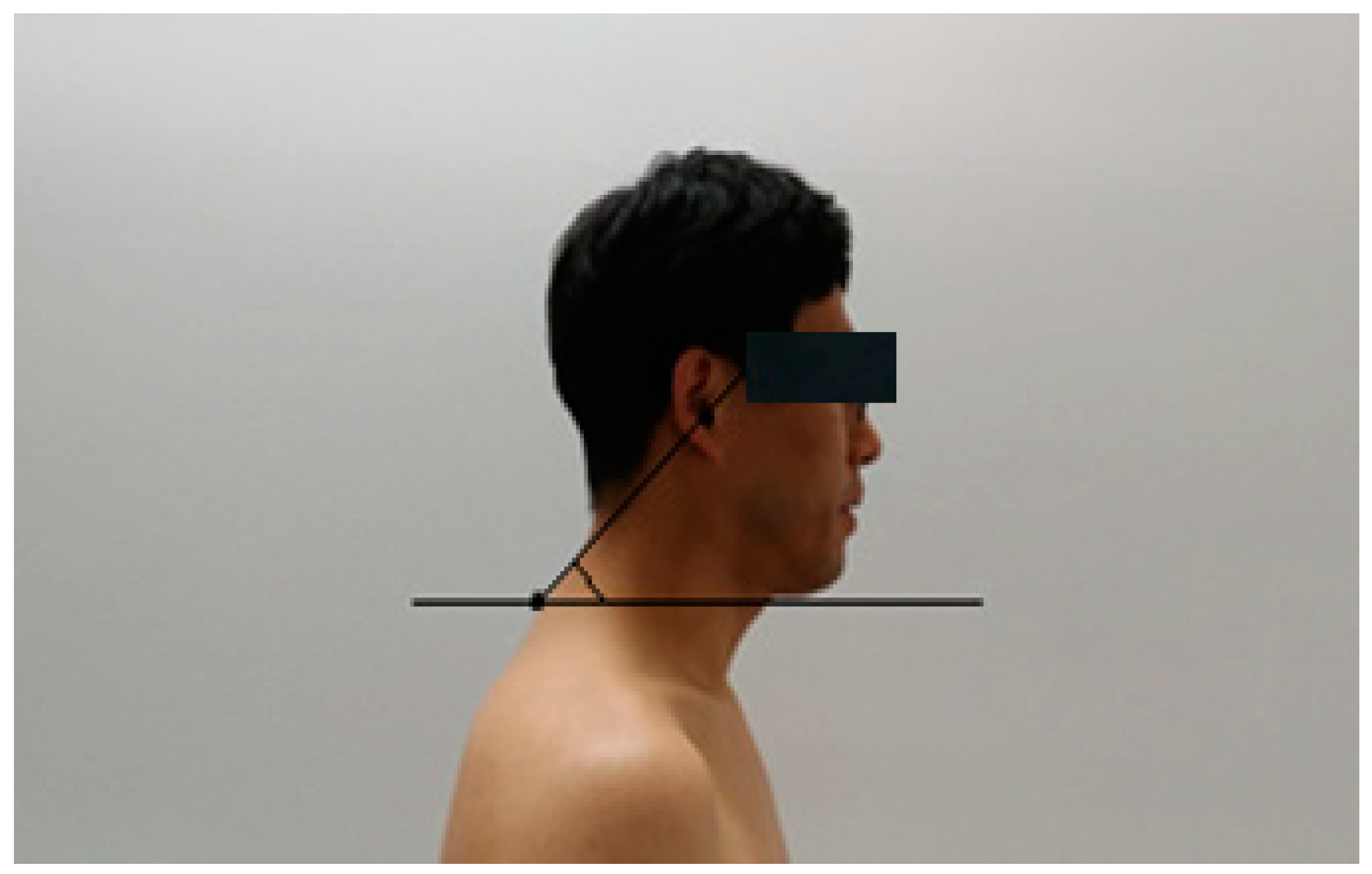
2.5. Measurements
2.5.1. Craniovertebral Angle (CVA)
2.5.2. Headache Disability Inventory
2.5.3. Sleep Quality Index
2.6. Sample Size Estimation
2.7. Statistical Analysis
3. Results
3.1. Variations in Headache Disorder
3.2. Variations in Sleep Disorder
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hudson, J.S.; Ryan, C.G. Multimodal group rehabilitation compared to usual care for patients with chronic neck pain: A pilot study. Man. Ther. 2010, 15, 552–556. [Google Scholar] [CrossRef]
- Tepper, M.; Vollenbroek-Hutten, M.M.R.; Hermens, H.J.; Baten, C. The effect of an ergonomic computer device on muscle activity of the upper trapezius muscle during typing. Appl. Ergon. 2003, 34, 125–130. [Google Scholar]
- Mekhora, K.; Liston, C.; Nanthavanij, S.; Cole, J. The effect of ergonomic intervention on discomfort in computer users with tension neck syndrome. Int. J. Ind. Ergon. 2000, 26, 367–379. [Google Scholar] [CrossRef]
- Nejati, P.; Lotfian, S.; Moezy, A.; Nejati, M. The study of correlation between forward head posture and neck pain in Iranian office workers. Int. J. Occup. Med. Environ. Health 2015, 28, 28. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.S.; Laymon, M.; Alshammari, F.; Khowailed, I.A.; Lee, H. Use of low level of continuous heat and Ibuprofen as an adjunct to physical therapy improves pain relief, range of motion and the compliance for home exercise in patients with nonspecific neck pain: A randomized controlled trial. J. Back Musculoskelet. Rehabil. 2017, 30, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Bryden, L.; Fitzgerald, D. The influence of posture and alteration of function upon the craniocervical and craniofacial regions. In Craniofacial Dysfunction and Pain: Manual Therapy, Assessment and Management; Butterworth-Heinemann: Oxfod, UK, 2001; pp. 163–187. [Google Scholar]
- Szeto, G.P.; Straker, L.; Raine, S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl. Ergon. 2002, 33, 75–84. [Google Scholar] [CrossRef]
- Quek, J.; Pua, Y.-H.; Clark, R.A.; Bryant, A.L. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man. Ther. 2013, 18, 65–71. [Google Scholar] [CrossRef]
- Harrison, D.E.; Harrison, D.D.; Betz, J.J.; Janik, T.J.; Holland, B.; Colloca, C.J.; Haas, J.W. Increasing the cervical lordosis with chiropractic biophysics seated combined extension-compression and transverse load cervical traction with cervical manipulation: Nonrandomized clinical control trial. J. Manip. Physiol. Ther. 2003, 26, 139–151. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Pérez-de-Heredia, M.; Molero-Sánchez, A.; Miangolarra-Page, J. Performance of the craniocervical flexion test, forward head posture, and headache clinical parameters in patients with chronic tension-type headache: A pilot study. J. Orthop. Sports Phys. Ther. 2007, 37, 33–39. [Google Scholar] [CrossRef]
- Dodick, D.W.; Eross, E.J.; Parish, J.M. Clinical, anatomical, and physiologic relationship between sleep and headache. J. Head Face Pain 2003, 43, 282–292. [Google Scholar] [CrossRef]
- Jull, G.A. Deep cervical flexor muscle dysfunction in whiplash. J. Musculoskelet. Pain 2000, 8, 143–154. [Google Scholar] [CrossRef]
- Rubini, E.C.; Costa, A.L.; Gomes, P.P.S.C. The Effects of Stretching on Strength Performance. Sports Med. 2007, 37, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Stovner, L.; Hagen, K.; Jensen, R.; Katsarava, Z.; Lipton, R.; Scher, A.; Steiner, T.; Zwart, J.J.C. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia 2007, 27, 193–210. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Hansen, K.; Mortensen, O.S.; Zebis, M.K. Prevalence and anatomical location of muscle tenderness in adults with nonspecific neck/shoulder pain. BMC Musculoskelet. Disord. 2011, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bronfort, G.; Assendelft, W.J.; Evans, R.; Haas, M.; Bouter, L. Efficacy of spinal manipulation for chronic headache: A systematic review. J. Manip. Physiol. Ther. 2001, 24, 457–466. [Google Scholar] [CrossRef]
- Lipchik, G.L.; Holroyd, K.A.; France, C.R.; Kvaal, S.A.; Segal, D.; Cordingley, G.E.; Rokicki, L.A.; McCool, H.R. Central and peripheral mechanisms in chronic tension-type headache. Pain 1996, 64, 467–475. [Google Scholar] [CrossRef]
- Fernández-de-las-Peñas, C.; Alonso-Blanco, C.; Cuadrado, M.L.; Gerwin, R.D.; Pareja, J.A. Trigger Points in the Suboccipital Muscles and Forward Head Posture in Tension-Type Headache. Headache J. Head Face Pain 2006, 46, 454–460. [Google Scholar] [CrossRef]
- Jung, K.Y. Sleep and Headache. Korean J. Headache 2006, 7, 23–26. [Google Scholar]
- Kelman, L.; Rains, J.C. Headache and sleep: Examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache J. Head Face Pain 2005, 45, 904–910. [Google Scholar] [CrossRef]
- Lynch, S.S.; Thigpen, C.A.; Mihalik, J.P.; Prentice, W.E.; Padua, D. The effects of an exercise intervention on forward head and rounded shoulder postures in elite swimmers. Br. J. Sports Med. 2010, 44, 376–381. [Google Scholar] [CrossRef]
- Miller, J.; Gross, A.; D’Sylva, J.; Burnie, S.J.; Goldsmith, C.H.; Graham, N.; Haines, T.; Brønfort, G.; Hoving, J.L. Manual therapy and exercise for neck pain: A systematic review. Man. Ther. 2010, 15, 334–354. [Google Scholar] [CrossRef]
- Boyd-Clark, L.; Briggs, C.; Galea, M.J.S. Muscle spindle distribution, morphology, and density in longus colli and multifidus muscles of the cervical spine. Spine 2002, 27, 694–701. [Google Scholar] [CrossRef]
- Cagnie, B.; Dirks, R.; Schouten, M.; Parlevliet, T.; Cambier, D.; Danneels, L. Functional reorganization of cervical flexor activity because of induced muscle pain evaluated by muscle functional magnetic resonance imaging. Man. Ther. 2011, 16, 470–475. [Google Scholar] [CrossRef]
- Falla, D.L.; Jull, G.A.; Hodges, P.W. Patients With Neck Pain Demonstrate Reduced Electromyographic Activity of the Deep Cervical Flexor Muscles During Performance of the Craniocervical Flexion Test. Spine 2004, 29, 2108–2114. [Google Scholar] [CrossRef]
- Randløv, A.; Østergaard, M.; Manniche, C.; Kryger, P.; Jordan, A.; Heegaardand, S.; Holm, B. Intensive dynamic training for females with chronic neck/shoulder pain. A randomized controlled trial. Clin. Rehabil. 1998, 12, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Nemmers, T.M.; Miller, J.W.; Hartman, M.D. Variability of the Forward Head Posture in Healthy Community-dwelling Older Women. J. Geriatr. Phys. Ther. 2009, 32, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Comerford, M.; Mottram, S. Kinetic Control-e-Book: The Management of Uncontrolled Movement; Elsevier Health Sciences: Chatswood, Australia, 2012. [Google Scholar]
- Comerford, M.; Mottram, S.L. Diagnosis of Uncontrolled Movement, Subgroup Classification and Motor Control Retraining of the Neck; Kinetic Control: Bristol, UK, 2011. [Google Scholar]
- Jesus, F.M.; Ferreira, P.H.; Ferreira, M.L. Ultrasonographic measurement of neck muscle recruitment: A preliminary investigation. J. Man. Manip. Ther. 2008, 16, 89–92. [Google Scholar] [CrossRef]
- Evjenth, O. Autostretching: The Complete Manual of Specific Stretching; Alfta Rehab Forlag: Alfta, Sweden, 2001. [Google Scholar]
- Jacobson, G.P.; Ramadan, N.M.; Aggarwal, S.K.; Newman, C.W. The Henry Ford Hospital Headache Disability Inventory (HDI). Neurology 1994, 44, 837–842. [Google Scholar] [CrossRef]
- Sohn, S.I.; Kim, D.H.; Lee, M.Y.; Cho, Y.W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath 2012, 16, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Lee, G.-H. Postural Control in the Patients with Chronic Tension-Type Headache. J. Korean Neurol. Assoc. 2007, 25, 324–331. [Google Scholar] [CrossRef][Green Version]
- Chae, Y.-W.; Lee, H.-M. The effect of craniocervical exercise on tension-type headache. J. Korean Phys. Therapy 2009, 21, 9–16. [Google Scholar]
- Martin-Herrero, C.; Rodrigues de Souza, D.P.; Alburquerque-Sendin, F.; Ortega-Santiago, R.; Fernández-de-Las-Peñas, C. Myofascial trigger points, pain, disability and quality of sleep in patients with chronic tension-type headache: A pilot study. Rev. Neurol. 2012, 55, 193–199. [Google Scholar] [PubMed]
- Peck, D.; Buxton, D.; Nitz, A. A comparison of spindle concentrations in large and small muscles acting in parallel combinations. J. Morphol. 1984, 180, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Dugailly, P.-M.; Sobczak, S.; Moiseev, F.; Sholukha, V.; Salvia, P.; Feipel, V.; Rooze, M.; Jan, S.V. Musculoskeletal modeling of the suboccipital spine: Kinematics analysis, muscle lengths, and muscle moment arms during axial rotation and flexion extension. Spine 2011, 36, E413–E422. [Google Scholar] [CrossRef] [PubMed]
- Canseco, J.A.; Schroeder, G.D.; Patel, P.D.; Grasso, G.; Chang, M.; Kandziora, F.; Vialle, E.N.; Oner, F.C.; Schnake, K.J. Regional and experiential differences in surgeon preference for the treatment of cervical facet injuries: A case study survey with the AO Spine Cervical Classification Validation Group. Eur. Spine J. 2021, 30, 517–523. [Google Scholar] [CrossRef]
- Bogduk, N. The anatomical basis for cervicogenic headache. J. Manip. Physiol. Ther. 1992, 15, 67–70. [Google Scholar]
- Bendtsen, L. Central sensitization in tension-type headache—Possible pathophysiological mechanisms. Cephalalgia 2000, 20, 486–508. [Google Scholar] [CrossRef]
- Harris, K.D.; Heer, D.M.; Roy, T.C.; Santos, D.M.; Whitman, J.M.; Wainner, R.S. Reliability of a Measurement of Neck Flexor Muscle Endurance. Phys. Ther. 2005, 85, 1349–1355. [Google Scholar] [CrossRef] [PubMed]
- Provini, F.; Vetrugno, R.; Lugaresi, E.; Montagna, P. Sleep-related breathing disorders and headache. Neurol. Sci. 2006, 27, s149–s152. [Google Scholar] [CrossRef] [PubMed]
- Rains, J.C.; Poceta, J.S. Headache and Sleep Disorders: Review and Clinical Implications for Headache Management. Headache J. Head Face Pain 2006, 46, 1344–1363. [Google Scholar] [CrossRef]
- Kogler, A.; Lindfors, J.; Ödkvist, L.; Ledin, T. Postural stability using different neck positions in normal subjects and patients with neck trauma. Acta Oto-Laryngol. 2000, 120, 151–155. [Google Scholar]


| EG (n = 16) | CG (n = 16) | p | |
|---|---|---|---|
| Female sex, n (%) * | 8 (50%) | 5 (31.2%) | 0.280 |
| Age (years) | 30.1 ± 2.7 | 31.0 ± 5.2 | 0.525 |
| Height (cm) | 164.4 ± 7.7 | 163.8 ± 8.2 | 0.843 |
| Weight (kg) | 61.8 ± 10.5 | 63.4 ± 9.9 | 0.656 |
| EG (n = 16) | EG (n = 16) | t | p | ||
|---|---|---|---|---|---|
| HDI (score) | Pre-test | 64.56 ± 13.38 | 57.88 ± 10.24 | −2519 | 0.017 |
| Post-test | 48.12 ± 10.78 | 57.38 ± 9.98 | |||
| t | 10.520 | 0.421 | |||
| p | <0.001 | 0.679 | |||
| PSQI-K (score) | Pre-test | 10.81 ± 1.97 | 10.50 ± 2.03 | −3.316 | 0.002 |
| Post-test | 7.56 ± 2.39 | 10.00 ± 2.25 | |||
| t | 10.070 | 1.936 | |||
| p | <0.001 | 0.072 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, W. Effect of 4 Weeks of Cervical Deep Muscle Flexion Exercise on Headache and Sleep Disorder in Patients with Tension Headache and Forward Head Posture. Int. J. Environ. Res. Public Health 2021, 18, 3410. https://doi.org/10.3390/ijerph18073410
Choi W. Effect of 4 Weeks of Cervical Deep Muscle Flexion Exercise on Headache and Sleep Disorder in Patients with Tension Headache and Forward Head Posture. International Journal of Environmental Research and Public Health. 2021; 18(7):3410. https://doi.org/10.3390/ijerph18073410
Chicago/Turabian StyleChoi, Wonho. 2021. "Effect of 4 Weeks of Cervical Deep Muscle Flexion Exercise on Headache and Sleep Disorder in Patients with Tension Headache and Forward Head Posture" International Journal of Environmental Research and Public Health 18, no. 7: 3410. https://doi.org/10.3390/ijerph18073410
APA StyleChoi, W. (2021). Effect of 4 Weeks of Cervical Deep Muscle Flexion Exercise on Headache and Sleep Disorder in Patients with Tension Headache and Forward Head Posture. International Journal of Environmental Research and Public Health, 18(7), 3410. https://doi.org/10.3390/ijerph18073410





