Eating Alone or Together among Community-Living Older People—A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection Process
2.3. Data Analysis
3. Results
3.1. Study Characteristics
3.2. Eating Alone as Central Topic
3.2.1. Quantitative Studies
3.2.2. Qualitative Studies
“Therefore, whilst dining in was, for the main part, experienced alone it was not described by participants as a lonely event. By contrast, dining in alone was perceived in practical terms and, at times, symbolic of independence, competence and control” [33].(p. 38)
| Reference | Study Design | Participants | Aim | Results |
|---|---|---|---|---|
| QUANTITATIVE | ||||
| Cross-sectional | ||||
| Davis, M. A., et al., 1988. USA (Brief report) [36] | Cross-sectional study | n = 4.402, 55–98 years | To examine associations between living arrangement and several eating behaviors. | Those living alone consumed more meals alone, ate higher proportion of food away from home and skipped more meals, than those living with a spouse. |
| Ishikawa, M., et al., 2017. Japan [13] | Cross-sectional study | n = 2.196, 65–90 years | To examine the relationships between eating together and subjective health, frailty, food behaviors, food accessibility, food production, meal preparation, alcohol intake, socioeconomic factors and geography among older Japanese people who live alone. | Those who ate together less than once a month (47% men, 23% women) had significantly lower rate of subjective health, food diversity and food intake frequency than those who ate together more often. The factors most strongly related to eating together less than once a month were not having food shopping assistance, not receiving food from relatives or neighbors, income, daily alcohol intake and frailty (for men only). |
| Kimura, Y., et al., 2012. Japan [18] | Cross-sectional study | n = 856, 65+ | To clarify the relations between eating alone and geriatric functions such as depression, quantitative subjective quality of life (QOL), activities of daily living (ADL) and dietary status of community-living Japanese older people. | Those who usually ate alone (n = 248, 33.2%) were significantly more depressed and had lower QOL-score, compared to those who usually ate with others. Among the n = 697 subjects who lived with others, n = 136 (19.5%) ate alone. |
| Kuroda, A., et al., 2015. Japan [19] | Cross-sectional study | n = 1.856, 65–94 years | To examine the association between social engagement and depressive symptoms with a particular focus on eating alone and how the association changes along the aging and mental frailty trajectories. | 14.6% were eating alone and 6% were eating alone despite living with family members. Eating alone was associated with higher risks of both mild and severe depression. Those who lived with their families yet ate alone were found to be at particular risk. |
| Kwon, A. R., et al., 2018. South Korea [14] | Cross-sectional study | 7.725 adults, 19+, mean age 47.1 | To investigate the association between eating alone and the metabolic syndrome (MetS) and to identify whether sociodemographic factors can modify this association. | There was a significant dose-response association between eating alone and MetS, independent of relevant confounders including sociodemographic and life style factors. Individuals who ate alone 2 or more times per day showed higher frequency of living alone, having no spouse, skip meals, and less eating out (p < 0.05). The association between eating alone and MetS was dependent on sex and presence of spouse. |
| Lee, S. A., et al., 2016. South Korea [21] | Cross-sectional study | n = 4.181, 20+ | To investigate the association between the dinner companion and depression, and the differences in this association by sex, living arrangement and household composition. | Those who ate alone had higher depression rate compared to those who ate with family. The subgroup analysis indicated that men, those who live with others and those living in a second-generation household who ate alone had greater odds of having depressive symptoms. |
| Locher, J. L., et al., 2005. USA [12] | Cross-sectional study | n = 50, 60–95 years, mean age 77.1 | To investigate the effect of the presence of others on caloric intake in homebound older adults. | 40% of participants consumed all meals alone, 28% consumed all meals with someone else and 32% ate some meals with and some meals without others. Participants consumed more calories for all meals in the presence of others compared to eating alone. Meals in the presence of others indicates an average of 114 kilocalories more per meal. After controlling for others′ presence at meals, the presence of others in the household had no significant effect on caloric intake. |
| Motteli, S., et al., 2017. USA [37] | Cross-sectional study | Part I: n = 502 females, 19–95 years; Part II: n = 262, 19+ | To investigate women’s regular eating networks and whether these were associated with dietary behavior and body weight. | Women shared their meals most frequently with family members. Those who dined more often with healthy eaters reported a higher diet quality and lower BMI, on average. Part II showed that different diet-related factors were correlated between women and their most important eating companions. Higher diet quality of the eating companions was associated with lower BMI in women. |
| Takeda, W. et al., 2018. Japan [26] | Cross-sectional study (administered in face-to-face interviews) | n = 242, 20–85 years (n = 63, 60+) | To examine frequencies of family commensality among Japanese adults in two metropolitan areas. | Family commensality was less frequent among those living alone, and with only non-partners including adult children, parents, and non-family members, than among those living with partners. Mean frequencies for family commensality were highest for those over 60, for all meals. Adults 60+ were the only group to exceed the national average rate, with rates being much lower among younger groups, those living with non-partners, and full-time workers. |
| Tani, Y., et al., 2015. Japan [11] | Cross-sectional study | n = 82.364, 65+ | To examine whether eating alone is associated with dietary behaviors and body weight status, and assessed the modifying effects of cohabitation status in older Japanese adults. | 16% of men and 28% of women sometimes or exclusively ate alone. Among those who exclusively ate alone, 56% of men and 68% of women lived alone. Depending on cohabitation status, eating alone and living alone may be jointly associated with higher prevalence of obesity, underweight and unhealthy eating behaviors in men. |
| Torres, C. C., et al., 1992. USA [23] | Cross-sectional study (administered in face-to-face interviews) | n = 424, 58+, mean age 71.9 | To examine four identified living and eating arrangement groups and what social network, functional disability etc. determine such group membership. | Older people with greater number of companions and percentage of kin in social network, were less likely to both live and eat alone. Men with higher income and age were also less likely to live and eat alone. Most older adults either live and eat alone or live and eat with others, mixed living/eating arrangements are rare. |
| Wang, X., et al., 2016. China [22] | Cross-sectional study (administered in face-to-face interviews) | n = 7.968, 60+ | To explore the relationship between eating alone and geriatric depressive symptom. | 17% of the participants ate alone and 9% had depressive symptom, those who ate alone but lived with others had a significant increased odds of depressive symptoms. |
| Yates, L. & Warde, A. 2017. UK [24] | Cross-sectional study | n = 2.784, 18+ | To examine meal arrangements in British households in 2012. | Eating alone was associated with simpler, quicker meals, and most commonly took place in the morning and midday. Those living alone eat alone more often but at similar meal times, and they take longer over their lone meals. |
| Longitudinal | ||||
| Huang, Y. C., et al., 2017. Taiwan [15] | Longitudinal study (10-year follow up) | n = 1.894, 65+, mean age 72.9 | To investigate the sex-specific association between eating arrangements and risk of all-cause mortality among community-living older adults. | 63% of men and 56% of women ate with others three times a day. Those who ate with others were more likely to have higher meat and vegetable intake and greater dietary quality than those who ate alone. Eating-with-others two or three times per day was an independent survival factor for older men, but not for women. |
| Li, C. L., et al., 2018. Taiwan [17] | Longitudinal study (4- and 8 year follow-ups) | n = 2.584 baseline, n = 2064 4-year follow-up, n = 1570 8-year follow-up. 65+, mean age 74 | To test the combined effect of two hazards, the risk of malnutrition and eating meals alone, on the cognitive changes among a representative sample of older Taiwanese individuals over an 8-year period. | Nutritional status was a salient predictor for cognitive decline among participants. Female respondents with compromised nutritional status at baseline and eating meals alone exhibited greater decrease in mental-status scores compared with those who had a normal nutritional status and who were eating their meals with others. |
| Tani, Y., et al., 2018. Japan [16] | Longitudinal population-based study (3-year follow up) | n = 71.781, 65+ | To examined the association between eating alone and mortality accounting for confounding factors among older Japanese adults. | Compared with men who ate and lived with others, the hazard ratio after adjusting for confounding factors was significantly higher for men who ate alone yet lived with others. Among women, there was no statistically significant association, neither for women who ate alone yet lived with others or for women who ate and lived alone. |
| Tani, Y., et al., 2015. Japan [20] | Longitudinal population-based study (3-year follow up) | n = 37.193, 65+ | To examine the association between eating alone and depression in the context of cohabitation status in older adults in Japan. | After adjustment for confounding factors, depression onset in men who ate alone compared with those who ate with others was significantly higher for those living alone. Among men, the effect of eating alone on depression may be reinforced by living alone, but appears to be broadly comparable with women. |
| Experimental | ||||
| McAlpine, S. J., et al., 2003. UK [28] | Experimental study | n = 21, 60–79 years | To examine whether nutritional supplements are less preferred and less likely to be selected than other energy-dense foods, and whether eating alone further reduces intake relative to eating in a social setting. | Favorite flavor of sip-feed (nutritional supplements) compared well with other more familiar foods and was selected as part of a snack. Intake increased by 60% when consumed in a group setting compared with eating alone. |
| McHugh Power, J. E., et al., 2016. Ireland (Pilot study) [27] | Experimental pilot study (randomized controlled trial design) | n = 100, 55+ | To investigate the effects of a novel mealtime intervention (including 50 volunteers, 55+) on self-efficacy, food enjoyment and energy intake on older adults, living alone in self-reported risk of social isolation. | Participants in treatment showed improvements relative to those in control group at borderline significance (p = 0.054) for self-efficacy and at significance for food enjoyment. No clear effects for energy intake or social cognitive factors. |
| Nakata, R. & Kawai, N. 2017. Japan [29] | Experimental study | Experiment 1: n = 16, 65–74 years, mean age 68.4; Experiment 2: n = 12, 66–74, mean age 68.9 | To analyze and answer whether the social facilitation of eating occur without the actual presence of other individuals. | Older and younger participants ate more popcorn and rated them better tasting in the self-reflecting condition than in the monitor condition. Furthermore, a similar observation of “social” facilitation of eating was made when participants ate popcorn in front of a static picture of themselves eating, suggesting that static visual information of someone eating food is enough to produce the “social” facilitation of eating. |
| QUALITATIVE | ||||
| Boyer, K., et al., 2016. Australia (Brief report) [38] | Focus group interviews and questionnaire | n = 41 older adults | To explore an innovative social eating program model for older Tasmanians, from the perspectives of its participants. | The program was meeting the social eating needs of its participants and nurturing a sense of community. |
| Keller, H. H., et al., 2015. Canada [34] | Interviews (once a year in 3 years, individual or duo) | n = 27 families, one older person with dementia and at least one family care partner | To explore the meaning and experience of mealtimes for families living with dementia. | Strategies to support quality mealtimes were devised by families: living in the moment, maintaining social engagement and continuity of mealtime activities. |
| Korsgaard, D., et al., 2019. Denmark [35] | Formative evaluation study | n = 7, 74–86 years | To address the question: What virtual environment do mobility-restricted older Danish adults perceive as engaging and suitable for pleasurable, mixed-reality solitary meals? | When evaluating a mixed-reality eating prototype, safety, realism, practicality, social acceptability, time, palatability, and indoor-outdoor considerations are found to be important aspects of food environment. |
| Martin, C. T., et al., 2005. USA [30] | Individual interviews | n = 8 women, 65+ | To investigate the factors that influence the dietary practices and eating patterns of low-weight (BMI <24) older adults and to examine the nutritional advice given by healthcare providers. | Eating alone, social isolation, and stressors are the main reasons for low weight, reported by participants. |
| McHugh, J., et al., 2015. Ireland (Letter to the Editor) [39] | Individual and focus group interviews | n = 6 older adults and n = 10 healthcare professionals | To investigate the significance of mealtimes for older adults living independently in the community, as well as the opinions of healthcare professionals working with this population. | Older adults were unaware of relationships between nutrition and health, but saw importance of sharing mealtimes with others. Healthcare professionals were more likely to discuss nutritional needs. |
| Saeed, A., et al., 2019. UK [40] | Individual and focus group interviews | n = 42, 59–89 years | To examine psychosocial barriers and facilitators to attending community-based social eating opportunities for older adults. | Four themes were identified that related to the importance of offering more than food (combine with other activity or to meet new friends); participants’ social identity (being with my kind of people and labelling of groups); taking the first step (going together and having personal connection; and embarrassment and self-consciousness about physical health. |
| Sidenvall, B., et al., 2000. Sweden [31] | Individual interviews | n = 63 women, 63+ | To delineate the meaning of preparing, cooking, and serving meals among retired single living and cohabiting women. | The meal could be seen as a gift, cohabiting women were cooking with duty and joy. For widows the whole meaning of cooking and eating was described as lost. |
| Thomas, N. & Emond, R., 2017. UK [33] | Individual interviews and 5-day food diary | n = 10, 60–88 years | To explore the perceptions and preferences of ten older people towards domestic and communal meals. | A number of key themes identified, including the meaning of mealtimes. Participants ate majority of meals at home alone. Despite this, dining alone was not necessarily experienced as lonely. |
| Vesnaver, E., et al., 2016. Canada [32] | Individual interviews | n = 15 women, 71–86 years | To explore loss of commensality among older widowed women in relation to food behavior. | Participants attributed changes to their food behaviors to the loss of commensality, including food choice, fewer regular meals, and reduced work of meal preparation. |
| MIXED DESIGN | ||||
| Jacobson, D. S., et al., 2015 Cyprus [25] | Cross-sectional survey and individual interviews | n = 625 households (quant. survey), n = 9 households (qual. interviews) | To show the relationship between food as a shared good in the economic sense, and food as a shared meal in the sociological sense. | There was relatively high expenditure on food for home consumption by older couples, which may be explained by that older people provide with food when their younger family members (i.e., children and grandchildren), frequently come to their homes for shared meals. |
3.3. Eating Alone as One Aspect
3.3.1. Quantitative Studies
3.3.2. Qualitative Studies
| Reference | Study Design | Participants | Aim | Result |
|---|---|---|---|---|
| QUANTITATIVE | ||||
| Cross-sectional | ||||
| Alberti Fidanza, A., 1984. Italy [61] | Cross-sectional study | n = 207, 65+ | To identify nutritional knowledge, food preferences and life styles connected with nutritional process. | Participants demonstrates low levels of nutritional knowledge. Women and men show similar percentages of energy expenditure, both in time and in frequency in relation to sleep and sedentary activities. Participants are well integrated in family life and eat most meals with their families. |
| Ashida, S., et al., 2019. USA [48] | Cross-sectional study (administered in face-to-face interviews) | n = 133, 60+, mean age 75.4 | To investigate whether social network functions (i.e., social support, companionship, social influence) are more likely to occur in relationships that involve active social interactions through co-engagement in activities compared to relationships that do not. | 1506 social relationships in which interactions occurred at least once a month were analyzed, 52% involved engagement in social activities together and 35% involved eating together regularly. Social relationships that involve co-engagement in social and daily activities, such as eating meals together, conveyed more social benefits compared to the relationships in which they did not. |
| Boulos, C., et al., 2017. Lebanon [46] | Cross-sectional study | n = 1.020, 65+, mean age 74.9 | To evaluate the association between three components of social isolation: social network, feeling of loneliness, commensality and nutritional status. | Social isolation and loneliness are independent risk factors for malnutrition. No significant association between the frequency of sharing meals and the risk of malnutrition. However people sharing most of the time of their meals with others were significantly less often malnourished. |
| de Castro, J. M., 1993. USA [62] | 7- day food diary | n = 307, 20+ (n = 44, 65+) | To investigate age-related changes in food intake (participants were divided into four age groups). | The lower intakes that occur with age is a consequence of smaller meals, eaten relatively slowly. Older people (65+) were as responsive to a number of influences of intake as younger people e.g., time of day and number of people present. |
| de Castro, J. M., 2002. USA [63] | 7- day food diary | n = 762, 20+ (n = 46, 65+) | To study age-related changes in the social, psychological, and temporal influences on food intake (participants were divided into four age groups). | Older people (65+) ate with fewer people present but were as responsive, as younger participants, to several factors e.g., social facilitation of intake and palatability, but showed blunted responses to self-reported hunger. |
| Dean, W. R., et al., 2014. USA [64] | Cross-sectional study | n = 2.785, 50+ | To explore the relative associations of capital assets with food insecurity across socioeconomic class through a comparative analysis of the association of intimate social capital, individual evaluations of community social capital, government capital, and interactions between social and government capital across three socioeconomic stratifications. | Social capital was not uniformly associated with food-security status across the income stratifications. There was a significantly greater proportion of participants relying on gardening, hunting, fishing, and animal husbandry in rural than in urban counties. Rural residents ate meals with family and friends more than urban and regularity of meals with family and friends increased with income level. |
| Ferry, M., et al., 2005. France [47] | Cross-sectional study (administered in face-to-face interviews) | n = 150, 70-99 years, mean age 80.8 | To determine the relationship between loneliness and nutritional status in persons aged over 70 years. | A large number of participants had an inadequate dietary intake and 21% had established undernutrition. 75% were widowed and 32% never shared a meal with family or friends. |
| Getty, M. D., et al., 2016. USA [65] | Cross-sectional study | n = 477, 59+ | To assess the presence of these risk factors in limited-resource, community-living older adults (meal site participants) to inform the development of a nutrition education interventions. | More African Americans reported having a chronic illness or condition, eating alone, and sometimes not having enough money to buy food. |
| Holm, L., et al., 2016. Denmark, Finland, Norway and Sweden [66] | Analysis of two cross-sectional surveys | n = 4.808, 15+ (1997) and n = n = n = 8.248, 15–80 years (2012) | To compare data from 1997 and 2012, in Denmark, Finland, Norway and Sweden, regarding where, with whom, and for how long people ate, and whether parallel activities take place while eating. | Primary location for eating remained the home and the workplace, the practices of eating in haste, and while watching television increased. Propensity to eat alone increased slightly in Denmark and Norway, and decreased slightly in Sweden. Signs of individualization and in formalization could be detected. |
| Holmes, B. A. & Roberts, C. L., 2011. UK [67] | Cross-sectional study (administered in face-to-face interviews) | n = 662, 65+ | To develop a single indicator of diet quality to provide a more accurate indicator of total diet in materially deprived men and women aged 65 and over, and to use this indicator to investigate risk factors associated with a poor quality diet in the low-income population. | The best quality diet was inversely associated with usually eating meals on one’s lap as opposed to at the table. For men, it was also inversely associated with difficulty chewing, whereas for women, it was inversely associated with current smoking and being 75 years or over. Results suggest that the social setting is an important determinant of diet quality in this group. |
| Holmes, B. A., et al., 2008. UK [68] | Cross-sectional study (administered in face-to-face interviews) | n = 234 men, 65+ | To investigate the influence of those social, physical and other factors collected in the LIDNS on the food consumption and nutrient intake of men aged 65 years and over who participated in the survey. | Mean energy intakes fell below the estimated average requirement (84%), while mean intakes of several micronutrients fell below the reference nutrient intake. Results suggest that interventions need to focus on improving cooking skills, especially in men who live or eat alone. |
| Ishikawa, M., et al., 2018. Japan [69] | Cross-sectional study | n = 2.151, 65+ | To clarify the food and health behavior factors associated with subjective well-being in older adults with a chronic disease living alone in the community. | Individuals with good subjective well-being had significantly higher rates than those with poor subjective well-being for satisfaction with meal quality and chewing ability, food diversity, food intake frequency, perception of shopping ease, having someone to help with food shopping, eating home-produced vegetables, preparing breakfast themselves, eating with other people, and high alcohol consumption. |
| Keller, H. H., et al., 2005. USA [70] | Cross-sectional study | Study 1: n = 193 (61 from geriatric clinics); Study 2: n = 149; Study 3: n = 97, 55+ | Three studies testing the reliability and validity of an updated screening tool for nutritional risk (Seniors in the Community: Risk Evaluation for Eating and Nutrition II, SCREEN II). | Respective median scores on SCREEN II were 51, 49 and 52. Proportion responding “Yes” to “Do you eat one or more meals a day with someone?” was 33%, 42.3% and 55.7%, for Study 1, 2 and 3, respectively. |
| Nicholas, M., et al., 2020. USA [71] | Cross-sectional study | n = 25, 34+, mean age 59.9 (and n = 12 caregivers) | To examine everyday activities valued by people with aphasia (PWA) using the Life Interests and Values (LIV) Cards; to measure congruence between PWA and their caregivers on life participation goals. | PWA endorsed wanting to participate more in a wide range of activities, with common interests in walking/running, going to the beach and eating out, among others. PWA–caregiver activity agreement was fair to moderate with point-to-point agreement averaging 70%. |
| Porter, K., et al., 2016. USA [72] | Cross-sectional study | n = 289, 60+, mean age 74.6 | To explore the associations between sexual orientation and the perceived social network and nutritional value of congregate meal programs (CMPs). | Sexual minorities were more likely to have non-kin-based social networks, reported higher levels of loneliness compared with heterosexuals and travelled seven times the distance to attend CMPs. |
| Posner, B. M., et al., 1993. USA [44] | Cross-sectional study | n = 749, 70+ | To recommend items for a consumer awareness checklist for the American “Nutrition Screening Initiative” and to calibrate the instrument. | A revised 10 yes/no-item checklist was adopted and 24% of the Medicare population were estimated at high nutritional risk according to the checklist. No significant association was found between answering “Yes” to “I eat alone most of the time” and dietary inadequacy or perceived health. |
| Quigley, K. K., et al., 2008. USA (Research brief) [43] | Cross-sectional study | n = 8.892, 60+ | To determine if there were differences by demographic variables in response rates to Nutrition Screening Initiative (NSI) among Oklahoma Older Americans Act Nutrition Program OAANP, congregate meal participants | 50% of participants categorized at high nutritional risk reported “yes” to having an illness or condition that affected food eaten; eating alone; taking 3 or more medications; and inability to shop, cook and feed themselves. |
| Rosenbloom, C. A. & Whittington, F. J., 1993. USA [73] | Cross-sectional study (administered in face-to-face interviews) | n = 50 widowed and n = 50 married, 60+ | To identify the effects of recent widowhood on nutritional behaviors. | Widowhood triggered disorganization and changes in the participant’s daily routines associated with food preparation and eating. 72% of the widowed reported loneliness at mealtimes since the death of their spouse and the widowed had a significantly lower Diet Quality score than the married (t = 8.74, p < 0.001). |
| Rugel, E. J. & Carpiano, R. M., 2015. Canada [74] | Cross-sectional study (administered in face-to-face interviews) | n = 14.221, 65+ | To test hypotheses regarding direct/indirect pathways through which tangible and emotional/informational social support may facilitate adequate fruit and vegetable consumption. | Emotional/informational support was positively associated with adequate fruit and vegetable consumption. Neither social support form was directly or indirectly associated with adequate consumption in men. Adequate consumption was negatively associated with tangible support but positively associated with higher emotional/informational support in women. |
| Shahar, D., et al., 2003. Israel [45] | Cross-sectional study | n = 377, 60+ (n = 224, 65–74 years; n = 153, 75+) | To determine dietary intake and eating patterns of older persons in Israel and identify factors associated with low dietary intake. | Energy, fat, carbohydrates, vitamins E, C and B1 intake were significantly lower for people aged 75 and older. Low energy intake was associated with lower subjective health status for men (p < 0.01), poor appetite (p < 0.01) and more gastrointestinal problems (p < 0.05) for women and lower snack consumption (p < 0.01) for both sexes. Eating alone was significantly and independently associated with low energy intake among men, but not among women. |
| Swan, J. H., et al., 2016. USA [75] | Cross-sectional study (administered in face-to-face interviews) | n = 989, 60+ | To examine the effects of attending Senior Centres (SC), on nutrition and health and efforts to improve diets and weight. | Less than one sixth strongly agreed that their health improved eating at the SC, less than one fourth agreed, whereas more than one third neither agreed nor disagreed. SC attendance and social engagement explained agreement that SC-meals improved nutrition and health but were not shown to predict changes in diet or weight control. |
| Toner, H. & Morris, D., 1993. USA [76] | Cross-sectional study | n = 100, 60–83 years | To examine the relationship of self-actualization and nutrition support to dietary intake. | Significant and positive associations between the predictor variables and vitamin A, B vitamin complex, iron and dietary fiber were found. Support from family, friends and neighbors were found to positively influence dietary quality. |
| Waring, M. L. & Kosberg, J. I., 1984. USA [77] | Cross-sectional study | n = 55, 60–92 years, median age 64 | To investigate the relationship of morale to social and health conditions, level of program participation, and the differential use of social welfare services of the older black people, utilizing a congregate meals program (CMP) in a small town. | CMPs met needs of participants but support services were utilized more than counselling services. Despite that CMPs was used for nourishment and social needs, in was not associated with morale. |
| Wham, C., et al., 2011. New Zealand [42] | Cross-sectional study (administered in face-to-face interviews) | n = 51, 80–85 years, mean age 82.4 | To assess the nutrition risk status of community living older people and to identify associated risk factors. | A third of the participants (31%) were at high risk of malnutrition, the majority of participants (82%) lived alone and nearly half (47%) had supportive social networks including close relationships with local family, friends and neighbors. |
| Longitudinal | ||||
| Clausen, T., et al., 2007. Botswana [50] | Longitudinal population-based study (administered in face-to-face interviews) | n = 372, baseline, n = 249 follow-up, 60+ | To assess diminished function and lack of social support as indicators of short term risk of death. | Overall mortality rate was 10.9 per 100 person years. Age-adjusted odds ratios (OR) for death during follow-up were; 4.2 (CI 1.4–12.5) and 3.6 (CI 1.0–12.7) for those with diminished physical- and cognitive function, respectively. Older community living persons in Botswana with reduced cognitive or physical function, have a significantly increased risk of death. |
| Lengyel, C. O., et al., 2017. Canada [41] | Longitudinal study | n = 336 men, mean age 90 | To identify patterns of nutritional risk among older men over a four-year period and to project their survival rates over the next two and a half years. | Distinct nutritional risk trajectories were found for older men over a four-year period. Poor nutritional risk trajectories are associated with higher risk of mortality for very old men over a short period of time. |
| Experimental | ||||
| Husted, M. M., et al., 2019. Denmark [49] | Single-blinded cluster-controlled study | n = 123, 65+ (n = 62 intervention group, mean age 82.3; n = 61 control group, mean age 83.5) | To understand if older adults have improvement in health-related quality of life, muscle strength, and nutritional status when involved in own meals as part of a rehabilitation program. | There was a significant (p = 0.01) improvement of health-related quality of life (converted EQ5D-3L score) in intervention (0.570 vs. 0.668) compared to the control (0.666 vs. 0.580) from baseline to follow-up. |
| QUALITATIVE | ||||
| Asamane, E. A., et al., 2019. UK [78] | Individual interviews (baseline and 8-month follow-up) | n = 92, 60+ (baseline n = 92, mean age 70.6; 8-month follow-up n = 81, mean age 70.7) | To identify and compare factors influencing eating behaviors and physical function among (participants self-identified as) ethnic minorities and understand how these factors and their association with healthy eating and physical function changed over 8 months. | Participants had diverse perceptions of healthy eating and physical function. Healthy eating was viewed as more important than, and unrelated to, physical function. Personal, social and cultural/environmental factors were identified as the main factors influencing these. Eating company were reported to affect eating positively and give greater enjoyment during mealtimes. |
| Bloom, I., et al., 2017. UK [53] | Focus group interviews | n = 92, 74–83 years, mean age 78 | To explore influences on diet among community-living older people in the UK; and to gain insight into sex differences and factors linked to differences in diet stability in older age. | Age-related factors linked to food choices were lifelong food experiences, retirement, bereavement, medical conditions and environmental factors. Discussion about social activities and isolation, community spirit and loneliness within focus groups, indicated the importance of social engagement as an influence on diet. |
| Byker Shanks, C., et al., 2017. USA [79] | Focus group interviews | n=33, 50+, mean age 73.6 | To explore how the rural food environment influences food choices of older adults. | Four themes related to factors influencing food choices emerged: perception of the rural community environment, support as a means of increasing food access, personal access to food sources, and dietary factors. |
| Cohen, N. & Cribbs, K., 2017. USA [55] | Focus group interviews | n=31, 60+ | To explore the food practices of LGBT seniors. | Social connection, nostalgia, creativity, material elements and competence came up during discussions. Food practices are entities composed of meanings, materials, and competences that are structured as they are performed repeatedly in a social context. |
| Falciglia, G., et al., 1985. USA [80] | Observations | n=4 older adults | To examine factors of change as they affect older people in four main settings: grocery shopping, meal preparation, meal/snacking patterns and entertainment. | Following factors are identified to effect food changes: health concerns, change in family composition, sensory alterations, income limitations, and social isolation. |
| Falk, L. W., et al., 1996. USA [81] | Individual interviews (2 with each participant) | n=16, 65+ | To explain how factors that affect food choice in older people function as food choice processes, and to further theoretical understanding of the food choice process in older adults. | Food choices and preferences were strongly influenced by beliefs related to appropriate food behavior and expected characteristics of foods and meals. Additionally, social context, sensory perceptions, monetary considerations, convenience, and physical well-being. |
| Foley, E. & BeLue, R., 2017. Senegal [57] | Individual interviews | n=41, mean age 58 | To identify cultural enablers and barriers to dietary management of type 2 diabetes. | Participants routinely identified the cost of food as a major obstacle to dietary management. Having a different diet or eating separately from the communal family plate creates feelings of social isolation, and reducing servings of traditional foods are described to feel like abandoning a culture. |
| Hegge, M., 1991. USA [51] | Individual interviews | n=26, 60+ | Examine problems and coping strategies of newly widowed older people. | Most frequent, troubling problems were loneliness, social isolation, disruption in eating and sleeping patterns. Coping strategies were sense of humor, faith, friends and family. |
| Howell, B. M. & Bardach, S. H., 2018. USA [82] | Individual interviews | n = 15, 57–87 years | To identify sociocultural influences on diet and activity patterns for seniors to inform the design of a larger quantitative research project. | Six major themes were identified: the media, friends and peers, family influences, social opportunities, ethnicity and subsistence practices, and weight loss/body weight concerns. |
| Jager, M. J., et al., 2019. the Netherlands [59] | Individual interviews | n = 12, 44–87 years | To explore experiences and views of ethnic minority type 2 diabetes patients regarding a healthy diet and dietetic care in order to generate information that may be used for the development of training for dieticians in culturally competent dietetic care. | Respondents acknowledged the importance of a healthy diet. What they considered healthy was determined by culturally influenced ideas about health benefits of specific foods. Social influences were experienced both as supportive and a hindrance. |
| Knutsen, I. R., et al., 2017. Five European countries [58] | Individual interviews | n = 125 (n = 94, 60+) | To achieve a better understanding of how food is perceived to be significant within persons’ network and relations at different levels, among people with type 2 diabetes. | The respondents′ reflections indicate that there are complex negotiations on different levels that influence self-management and food, including support, knowledge, and relationships within families; attention and openness in social situations; and the premises and norms of society. |
| Pettigrew, S. & Roberts, M., 2008. Australia [52] | Individual interviews | n = 19, 65+ | To generate specific intervention recommendations, working with loneliness among older adults. | Identified behaviors that ameliorated loneliness: friends and family—emotional resource, engaging in eating and drinking rituals—maintaining social contacts, reading and gardening. |
| Plastow, N. A., et al., 2015. UK [60] | Individual interviews | n = 39, 61–89 years, mean age 74 | To explore the role of food activities in identity maintenance among community-living older adults. | Two lifelong food identities were discovered: “food lover” and “nonfoodie”. Food activities that are a pleasurable and important part of daily life contribute to the maintenance of important identities and mental well-being in older adults. |
| Sriram, U., et al., 2018. USA [83] | Focus group interviews | n = 125, 40–91 years (n = 67, 65+) | To explore how social relationships influence health-related behaviors among midlife and older rural adults at increased risk of chronic disease. | Authors found actions and attitudes of family and friends to be key influences on diet, physical activity, and tobacco use behaviors, positively and negatively. Older women expressed that loneliness was a barrier for healthy eating, due to lack of motivation to prepare healthy meals. “Food-centric events”, including shared meals, also expressed by both older and middle aged persons as part of peer influences on diet. |
| Tessier, S. & Gerber, M., 2005. Sardinia/Malta [84] | Individual interviews | n = 30 mother-daughter couples, mean age 66 and 39, respectively | To compare meals, in-between meals snack consumption and total daily food intakes between Sardinia and Malta in terms of structure, social environment and times, as well as their changes. | There were striking contrasts between Sardinian and Maltese food habits, such as meal preparation times, breakfast and main meal structures, total daily food intake profiles and commensality. |
| Thompson, J., et al., 2017. UK [85] | Individual interviews | n = 20 men, 65–90 years, mean age 80 | To understand the potential for issues around food vulnerability to arise in older bereaved men and to characterize that vulnerability, if present. | Five overarching themes were identified: financial security, social networks, cooking skills, food and routine and single servings. |
| Uribe, A. C. R., 2019. Mexico [86] | Individual interviews | n = 14 women, 64–87 years, mean age 76 | To explain the cooking and eating behaviors of Mexican older women living alone using a life course perspective | Ten out of fourteen reported finding eating alone not enjoyable at all. It used to be a time for socializing with families, sharing, and having fun. Coping strategies included reading, watching television, listening to music, and inviting friends and neighbors over for shared meals. A table for one was also said to result in changed eating habits, for example by skipping meals, and eating more while cooking less. |
| Whitelock, E. & Ensaff, H., 2018. UK [54] | Focus group interviews | n = 30, 63–90 years | To explore older adults’ perceptions and practices related to dietary behavior and the factors influencing their food choice in later life. | Age-related changes, food access, on your own and relationship with food are themes that emerged where living alone and social isolation often were discussed. |
| MIXED DESIGN | ||||
| Gustafsson, K. & Sidenvall, B., 2002. Sweden [87] | Individual interviews and 3-day food diary | n = 18 women, 65–88 years | To explore food-related health perceptions and food habits among older women. | The first theme “a healthy slimming meal or the usual” summarized the women′s health perceptions related to food, where the dominating view was fear of fat. The second theme “meals—a pleasure or an obligation” showed that meals in fellowship were perceived as a pleasure, and women living alone tended to simplify cooking and eating. |
| Hughes, G., et al., 2004. UK [88] | Cross-sectional survey and individual interviews | n = 39 men, 62–94 years, mean age 74.8 | To investigate barriers to healthy eating, focusing on energy intake, food choice (specifically fruits and vegetables), cooking skills and well-being in a group of older men living alone. | BMI failed to predict patterns of intake. Men with good cooking skills reported better physical health and higher intake of vegetables. Interviews revealed that poor cooking skills and low motivation to change eating habits may constitute barriers to improving energy intake, healthy eating and appetite. |
| Johnson, C.S., 2002. Canada [56] | Cross-sectional survey and focus group interviews | n = 22, 60–85 years, mean age 72 | To examine level of nutritional risk and dietary issues faced by older adults in three groups: recently bereaved, with or without intervention and those in coupled relationships. | Bereaved individuals had moderate risk for poor nutrition, irrespectively if they had counselling for grief resolution or not. Those in coupled relationships had the lowest risk. One dietary issue for bereaved individuals was memories of shared meals, coping by changing setting (ex in front of TV) or inviting friends/family. |
| Shifflett, P.A., 1987. USA [89] | Observations, individual interviews and 7-day food record | n = 30, 60–91 years | To investigate the process of negotiating food habit changes among older people, including future time perspective and past experiences. | Future time perspective and past experiences were significant in negotiating process. Changes were either externally motivated (physician-prescribed) or internally motivated (self-prescribed). |
| Zelig, R., et al., 2019. USA [90] | Individual interviews and nutritional assessment | n = 19, 66–83 years, mean age 71.3 | To explore the eating experience and eating-related quality of life (ERQOL) of community-living older adults with tooth loss. | Some participants ate before going out or avoided eating out due to embarrassment, others had no embarrassment or self-consciousness. Participant at risk for malnutrition more frequently reported that eating got harder over time and had less social interaction, less enjoyment from food, more food avoidance, and more embarrassment related to their tooth loss. |
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Databases: PubMed, Web of Science, Cinahl and PsycInfo. | ||
| Block 1: TargetGroup | Block 2: Meals | Block 3: Social Aspects |
| Old age | Commensality | Social Engagement |
| Old people | Meals | Social Participation |
| Older people | Eating | Social Interaction |
| Old adults | Diet | Social Norm(s) |
| Older adults | Eating alone | Social Context |
| Elderly | Food intake | Social Environment |
| Aging (Only MeSH) | Dietary intake | Social Isolation |
| Aged (Only MeSH) | Food choice | Social Network(s) |
| Food habits | Social Influence | |
| Social eating | Social Facilitation | |
| Eating behavior | Social Modeling | |
| Food consumption | Single living | |
| Solo dining | Living alone | |
| Solo eating | Social Isolation (Only MeSH) | |
| Food (Only MeSH) | ||
| Meals (Only MeSH) | ||
Appendix B
| Search Number | Block | Search Terms |
|---|---|---|
| 1 | Target group | (((((((Elderly[Title/Abstract]) OR (“Old age”[Title/Abstract])) OR (“Old people”[Title/Abstract])) OR (“Older people”[Title/Abstract])) OR (“Old adults”[Title/Abstract])) OR (“Older adults”[Title/Abstract])) OR (aging[MeSH Terms])) OR (aged[MeSH Terms]) |
| 2 | Meals | (((((((((((((((Commensality[Title/Abstract]) OR (Meals[Title/Abstract])) OR (Eating[Title/Abstract])) OR (Diet[Title/Abstract])) OR (Eating alone[Title/Abstract])) OR (Food intake[Title/Abstract])) OR (Dietary intake[Title/Abstract])) OR (Food choice[Title/Abstract])) OR (Food habits[Title/Abstract])) OR (“Social eating“[Title/Abstract])) OR (“Eating behavior”[Title/Abstract])) OR (“Food consumption”[Title/Abstract])) OR (“Solo dining”[Title/Abstract])) OR (“Solo eating”[Title/Abstract])) OR (food[MeSH Terms])) OR (meals[MeSH Terms]) |
| 3 | Social aspects | (((((((((((((((Social Engagement[Title/Abstract]) OR (Social Participation[Title/Abstract])) OR (Social Interaction[Title/Abstract])) OR (Social Norm[Title/Abstract])) OR (Social Norms[Title/Abstract])) OR (“Social Context”[Title/Abstract])) OR (“Social Environment”[Title/Abstract])) OR (“Social Isolation”[Title/Abstract])) OR (“Social Network”[Title/Abstract])) OR (“Social Networks”[Title/Abstract])) OR (“Social Influence”[Title/Abstract])) OR (“Social Facilitation”[Title/Abstract])) OR (“Social Modeling”[Title/Abstract])) OR (“Single living”[Title/Abstract])) OR (“Living alone”[Title/Abstract])) OR (social isolation[MeSH Terms]) |
| 4 | Combined | 1 AND 2 AND 3 |
Appendix C
Appendix C.1. The Third Category: Eating Alone is Peripheral
Appendix C.2. Quantitative Studies
Appendix C.3. Qualitative Studies
| Reference | Study Design | Participants | Aim | Result |
|---|---|---|---|---|
| QUANTITATIVE | ||||
| Cross-sectional | ||||
| Allal, A. S., et al., 2000. Switzerland [97] | Cross-sectional study | n = 21 head and neck cancer patients, 40+, median age 63 | To evaluate quality of life (QOL) and functional outcome in patients with carcinomas of the larynx and hypopharynx treated with accelerated radiotherapy (RT). | The PSSHN scores were 89, 84, and 86, respectively, for eating in public, understandability of speech and normalcy of diet (100 = normal function). QOL and functional outcome in patients treated conservatively with concomitant boost RT for laryngeal and hypopharyngeal carcinomas appear to be similar to those obtained in patients treated with conventional or hyperfractionated RT. |
| Allal, A. S., et al., 2003. Switzerland [98] | Cross-sectional study | n = 60 head and neck cancer patients, 42+, median age 61 | To assess quality of life (QoL) outcomes of patients after two treatment strategies: radical surgery with postoperative RT and accelerated concomitant boost RT with or without chemotherapy. | The PSSHN scores were generally higher in the RT group, with a significant difference in the speech subscale (p = 0.005), a trend for a significant difference for the eating in public subscale (p = 0.08), and an insignificant difference for the normalcy of diet subscale (p = 0.25). For early stages no clear advantage in QoL outcome was noted for the RT group compared with the surgery group, for advanced-stage disease an advantage favoring radical RT seemed apparent. |
| Byeon H., 2019. South Korea [105] | Cross-sectional study | n = 142, 65+ | To identify factors affecting the swallowing quality-of-life of older people. | 33.9% of the elderly had low swallowing quality-of-life. The proportion of the elderly with a low swallowing quality-of-life was significantly higher when the subjects were equal to or older than 75 years old (38.4%), were female (44.6%), were elementary school graduate or below (35.7%) and were living alone (31.7%). |
| Hoerster, K. D., et al., 2016. USA [100] | Cross-sectional study | n = 653, 25–97 years, mean age 60.8 | To examine individual, social environment, and physical environment correlates of general diet quality among Veterans. | Higher level of depressive symptom severity, not having others to eat healthy meals with and reduced availability of low-fat foods in stores were associated with poorer diet quality. |
| Kjaer, T. K., et al., 2016. Denmark [99] | Cross-sectional study | n = 369 head and neck cancer survivors, mean age 64 (n = 234, 60+) | To investigate associations between social factors, length of education and cohabitation status, and the occurrence of clinically relevant, patient-reported late effects, with control for important disease-related factors, such as site, stage, and HPV status, and treatment and lifestyle factors and comorbidity. | Survivors with short education were more likely to report severe problems than those with medium or long education. For survivors who lived alone, the adjusted ORs were significantly increased for physical functioning (2.17; 95% CI 5 1.01–4.68) and trouble with social eating (OR 5 2.26; 95% CI 5 1.14–4.47). |
| Lai, X. J., et al., 2019. China [106] | Cross-sectional study | n = 290 retired couples and n = 1.571 working couples | To investigate how retirement would change their activity time use and patterns. In particular, intra-household interactions are considered, to explore the interdependencies among household members’ choices, social-demographics and travel behaviors. | Retirement would substantially increase joint participations and durations in various out-of-home activities. In addition, the importance of walkability is emphasized for retired couples in a mixed-land-use and transit-dependent city, and a potential social exclusion issue is identified for the low-income retired population. |
| Quandt, S. A. & Rao, P., 1999. USA [107] | Cross-sectional study (administered in face-to-face interviews) | n = 192, 65+ | To asses level of food insecurity and identify predictors. | 24% report one or more food insecurity indicator. Eating alone is together with taking three or more prescription drugs and income less than 150% of poverty level predictors of food insecurity. |
| Wham, C. A., et al., 2015. New Zealand [101] | Cross-sectional study | n = 255 Māori and n = 400 non-Māori adults, 80–90 years | To establish the prevalence of high nutrition risk and associated health and social risk factors for New Zealand Māori and non-Māori participants. | Half (49%) of Māori and 38% of non-Māori participants were at high nutrition risk (SCREEN II score <49). For non- Māori high nutrition risk was associated with female sex (p = 0.005), living alone (p = 0.002), a lower physical health related quality of life (p = 0.02) and depressive symptoms (p = 0.002). |
| Longitudinal | ||||
| Ang, S., 2018. Singapore [102] | Longitudinal study (administered in face-to-face interviews) | n = 4.482, mean age men 71.6;mean age women 72.2 | Investigates if ethnicity accounts for sex differences in (a) the types of social activities older adults participate in and (b) the association between social participation and 4-year mortality. | Men were more likely to engage in social activities compared to women, sex difference varied by ethnicity. Going out to eat was associated with a lower risk of mortality for men only and playing sports was found to be protective for women only. |
| Arcury, T. A., et al., 2012. USA [108] | Longitudinal study (administered in face-to-face interviews, 2 with each participant and one month interval) | n = 593 (first interview); n = 563 (second interview) 60+ | To describe diabetes management behaviors and social integration among older adults, and delineate the associations of social integration with diabetes management behaviors. | Participants had high levels of social integration and largely adhered to diabetes management behaviors. Social integration was associated with social network size, particularly other relatives seen and spoken with on the telephone among others. |
| Mamalaki, E., et al., 2019. Greece [109] | Longitudinal cohort study | n = 1.933 adults, 65–99 years, mean age 73.1 | To explore the associations between social life and adherence to a healthy dietary pattern, the Mediterranean diet (MD), in a population-representative cohort of older people. | Each unit increase in the number of social contacts/month and in the frequency score of intellectual, social and physical activities was associated with a 1·6, 6·8, 4·8 and 13·7% increase in the likelihood of a participant being in the high MD adherence group, respectively. |
| QUALITATIVE | ||||
| Cerin, E., et al., 2019. Australia [104] | Focus group interviews | n = 91, 60–85 years, mean age 71.1 | To identify built and social environmental facilitators of and barriers to regular engagement in physical activity, eating a healthy diet and regular contact with other people among older Chinese immigrants to urban Australia. | For physical activity the highest ranked facilitator and barrier was “proximity to destinations” and “poor/inadequate public transport”, respectively. For healthy diet the highest ranked facilitator and barrier were “high food safety standards/regulations” and “lack of family/household members′ social support for a healthy diet”. |
| Lee, K.-I., 2009. USA [103] | Focus group interviews | n = 39, 62–92 years, mean age 78 | To explore community-living elderly beliefs for participating in congregate meal programs and to identify salient beliefs by category (behavioral beliefs, normative beliefs and control beliefs). | Advantages of participating are nutrition implication, social interaction, special diets, low price, convenience and less waste. |
| van den Heuvel, E., et al., 2018. UK [110] | Individual and focus group interviews | n = 42, 56–96 years, mean age 67 | To explore all reasons for consuming and not consuming eggs in older adults. | Thematic analyses revealed 69 different reasons for eating or not eating eggs and were related to: properties of the food, convenience, medical factors and social environment. The category “Social environment” included social influence of anyone present at an eating occasion. |
| Zou, P., 2019. Canada [111] | Individual interviews | n = 30, mean age 61 | To determine the facilitators and barriers influencing healthy eating behaviors among aged Chinese-Canadians with hypertension. | The analyze resulted in personal, familial, community and societal factors. Among “Familial factors” on diet, other people’s preferences and habits was mentioned. For example, that it is easier to cook healthy in a small family, with only two people sharing a meal. Being alone could also affect motivation to cook negatively. |
| MIXED DESIGN | ||||
| Glover, L., et al., 2020. UK [112] | Co-creation study, 4 meetings | n = 10 lay people, 70–79 years and n = 4 university members, 27–57 years | To undertake a co-creation study, explore maintenance of health and well-being in older age, and the application of co-creation with an older community population and evaluate the process to inform future work. | Findings demonstrate that state of mind and of health were key to well-being in older age. Feeling safe, comfortable and pain free were important along with being able to adapt to change, have choice and a sense of personal freedom. Social connectedness was seen as the keystone to support healthy behaviors. |
| Howell, B. M., 2020. USA [113] | Cross-sectional survey, participant observation and individual interviews | n = 82, 65+, mean age 74 | To examine the relationship between the sociocultural factors that shape diet, physical activity, and nutritional status outcomes among seniors. | T-tests indicate that diet and physical activity practices in this sample do not meet national recommendations and that diet differs adversely from national reference samples. Family influences increased fruit consumption, while participation in cultural and social events increased intake of fats and sweets. |
| Nogueira, D., et al., 2019. Portugal [114] | Three phase evaluation study | n = 105 patients (with dysarthria), 18–102 years, mean age 64; and n = 103 control (without), 18–87, mean age 50.6 | To produce a European Portuguese version of the Quality of Life Questionnaire for the Dysarthric Speaker (QoL-DyS). | The QoLDyS correlated positively with the QAD, PEAT-10, and EQ5D. Cronbach′s α was 0.973, and it remained excellent when any item was deleted. |
Appendix D
| Geographic Regions | Total | Central Topic | One Aspect | Peripheral |
|---|---|---|---|---|
| Northern Africa | 0 (0%) | |||
| Sub-Saharan Africa | 2 (2%) | 2 | ||
| Northern America | 39 (40%) | 7 | 26 | 6 |
| Caribbean | 0 (0%) | |||
| Central America | 1 (1%) | 1 | ||
| Latin America | 0 (0%) | |||
| Central Asia | 0 (0%) | |||
| Eastern Asia | 16 (16%) | 13 | 1 | 2 |
| South-Eastern Asia | 0 (0%) | |||
| Southern Asia | 1 (1%) | 1 | ||
| Western Asia | 3 (3%) | 1 | 2 | |
| Northern Europe | 23 (24%) | 8 | 12 | 3 |
| Eastern Europe | 0 (0%) | |||
| Southern Europe | 4 (4%) | 2 | 2 | |
| Western Europe | 4 (4%) | 2 | 2 | |
| Oceania | 5 (5%) | 1 | 2 | 2 |
| 98 (100%) | 30 | 50 | 18 |
References
- Courtin, E.; Knapp, M. Social isolation, loneliness and health in old age: A scoping review. Health Soc. Care Commun. 2017, 25, 799–812. [Google Scholar] [CrossRef]
- Keller, H.H. Promoting food intake in older adults living in the community: A review. Appl. Physiol. Nutr. Metab. 2007, 32, 991–1000. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Capitanio, J.P. Perceived social isolation, evolutionary fitness and health outcomes: A lifespan approach. Philos. Trans. R. Soc. B Biol. Sci. 2015, 370. [Google Scholar] [CrossRef] [Green Version]
- Warde, A. The Practice of Eating; Polity Press: Cambridge, UK, 2016. [Google Scholar]
- Vesnaver, E.; Keller, H.H. Social influences and eating behavior in later life: A review. J. Nutr. Gerontol. Geriatr. 2011, 30, 2–23. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Report on Ageing and Health. Available online: https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=574F13482630EAACA3B27638854F0100?sequence=1 (accessed on 15 May 2020).
- Jonsson, A.-S.; Nyberg, M.; Jonsson, I.M.; Öström, Å. Older patients’ perspectives on mealtimes in hospitals: A scoping review of qualitative studies. Scand. J. Caring Sci. 2020. [Google Scholar] [CrossRef]
- Vucea, V.; Keller, H.H.; Ducak, K. Interventions for Improving Mealtime Experiences in Long-Term Care. J. Nutr. Gerontol. Geriatr. 2014, 33, 249–324. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5. [Google Scholar] [CrossRef] [Green Version]
- Tani, Y.; Kondo, N.; Takagi, D.; Saito, M.; Hikichi, H.; Ojima, T.; Kondo, K. Combined effects of eating alone and living alone on unhealthy dietary behaviors, obesity and underweight in older Japanese adults: Results of the JAGES. Appetite 2015, 95, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Locher, J.L.; Robinson, C.O.; Roth, D.L.; Ritchie, C.S.; Burgio, K.L. The effect of the presence of others on caloric intake in homebound older adults. J. Gerontol. Ser. Biol. Sci. Med. Sci. 2005, 60, 1475–1478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ishikawa, M.; Takemi, Y.; Yokoyama, T.; Kusama, K.; Fukuda, Y.; Nakaya, T.; Nozue, M.; Yoshiike, N.; Yoshiba, K.; Hayashi, F.; et al. “Eating together” is associated with food behaviors and demographic factors of older Japanese people who live alone. J. Nutr. Health Aging 2017, 21, 662–672. [Google Scholar] [CrossRef]
- Kwon, A.R.; Yoon, Y.S.; Min, K.P.; Lee, Y.K.; Jeon, J.H. Eating alone and metabolic syndrome: A population-based Korean National Health and Nutrition Examination Survey 2013–2014. Obes. Res. Clin. Pract. 2018, 12, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Cheng, H.L.; Wahlqvist, M.L.; Lo, Y.C.; Lee, M.S. Gender differences in longevity in free-living older adults who eat-with-others: A prospective study in Taiwan. BMJ Open 2017, 7, e016575. [Google Scholar] [CrossRef] [Green Version]
- Tani, Y.; Kondo, N.; Noma, H.; Miyaguni, Y.; Saito, M.; Kondo, K. Eating Alone Yet Living With Others Is Associated With Mortality in Older Men: The JAGES Cohort Survey. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2018, 73, 1330–1334. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.L.; Tung, H.J.; Yeh, M.C. Combined effect of eating alone and a poor nutritional status on cognitive decline among older adults in Taiwan. Asia Pac. J. Clin. Nutr. 2018, 27, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Wada, T.; Okumiya, K.; Ishimoto, Y.; Fukutomi, E.; Kasahara, Y.; Chen, W.; Sakamoto, R.; Fujisawa, M.; Otsuka, K.; et al. Eating alone among community-dwelling Japanese elderly: Association with depression and food diversity. J. Nutr. Health Aging 2012, 16, 728–731. [Google Scholar] [CrossRef]
- Kuroda, A.; Tanaka, T.; Hirano, H.; Ohara, Y.; Kikutani, T.; Furuya, H.; Obuchi, S.P.; Kawai, H.; Ishii, S.; Akishita, M.; et al. Eating Alone as Social Disengagement is Strongly Associated With Depressive Symptoms in Japanese Community-Dwelling Older Adults. J. Am. Med. Dir. Assoc. 2015, 16, 578–585. [Google Scholar] [CrossRef] [Green Version]
- Tani, Y.; Sasaki, Y.; Haseda, M.; Kondo, K.; Kondo, N. Eating alone and depression in older men and women by cohabitation status: The JAGES longitudinal survey. Age Ageing 2015, 44, 1019–1026. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.A.; Park, E.C.; Ju, Y.J.; Nam, J.Y.; Kim, T.H. Is one’s usual dinner companion associated with greater odds of depression? Using data from the 2014 Korean National Health and Nutrition Examination Survey. Int. J. Soc. Psychiatry 2016, 62, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shen, W.; Wang, C.; Zhang, X.; Xiao, Y.; He, F.; Zhai, Y.; Li, F.; Shang, X.; Lin, J. Association between eating alone and depressive symptom in elders: A cross-sectional study. BMC Geriatr. 2016, 16, 19. [Google Scholar] [CrossRef] [Green Version]
- Torres, C.C.; McIntosh, W.A.; Kubena, K.S. Social network and social background characteristics of elderly who live and eat alone. J. Aging Health 1992, 4, 564–578. [Google Scholar] [CrossRef]
- Yates, L.; Warde, A. Eating together and eating alone: Meal arrangements in British households. Br. J. Sociol. 2017, 68, 97–118. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, D.S.; McMullan, C.; Minas, C. Engel and Simmel: Sharing meals at home in Cyprus. Br. Food J. 2015, 117, 677–687. [Google Scholar] [CrossRef]
- Takeda, W.; Melby, M.K.; Ishikawa, Y. Who eats with family and how often? Household members and work styles influence frequency of family meals in urban Japan. Appetite 2018, 125, 160–171. [Google Scholar] [CrossRef]
- McHugh Power, J.E.; Lee, O.; Aspell, N.; McCormack, E.; Loftus, M.; Connolly, L.; Lawlor, B.; Brennan, S. RelAte: Pilot study of the effects of a mealtime intervention on social cognitive factors and energy intake among older adults living alone. Br. J. Nutr. 2016, 116, 1573–1581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McAlpine, S.J.; Harper, J.; McMurd, M.E.T.; Bolton-Smith, C.; Hetherington, M.M. Nutritional supplementation in older adults: Pleasantness, preference and selection of sip-feeds. Br. J. Health Psychol. 2003, 8, 57–66. [Google Scholar] [CrossRef]
- Nakata, R.; Kawai, N. The ‘social’ facilitation of eating without the presence of others: Self-reflection on eating makes food taste better and people eat more. Physiol. Behav. 2017, 179, 23–29. [Google Scholar] [CrossRef]
- Martin, C.T.; Kayser-Jones, J.; Stotts, N.A.; Porter, C.; Froelicher, E.S. Factors contributing to low weight in community-living older adults. J. Am. Acad. Nurse Pract. 2005, 17, 425–431. [Google Scholar] [CrossRef]
- Sidenvall, B.; Nydahl, M.; Fjellstrom, C. The meal as a gift—The meaning of cooking among retired women. J. Appl. Gerontol. 2000, 19, 405–423. [Google Scholar] [CrossRef]
- Vesnaver, E.; Keller, H.H.; Sutherland, O.; Maitland, S.B.; Locher, J.L. Alone at the Table: Food Behavior and the Loss of Commensality in Widowhood. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 71, 1059–1069. [Google Scholar] [CrossRef] [PubMed]
- Thomas, N.; Emond, R. Living alone but eating together: Exploring lunch clubs as a dining out experience. Appetite 2017, 119, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Keller, H.H.; Martin, L.S.; Dupuis, S.; Reimer, H.; Genoe, R. Strategies to support engagement and continuity of activity during mealtimes for families living with dementia; a qualitative study. BMC Geriatr. 2015, 15, 119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korsgaard, D.; Bjoner, T.; Nilsson, N.C. Where would you like to eat? A formative evaluation of mixed-reality solitary meals in virtual environments for older adults with mobility impairments who live alone. Food Res. Int. 2019, 117, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.A.; Murphy, S.P.; Neuhaus, J.M. Living arrangements and eating behaviors of older adults in the United States. J. Gerontol. 1988, 43, S96–S98. [Google Scholar] [CrossRef] [PubMed]
- Motteli, S.; Siegrist, M.; Keller, C. Women’s social eating environment and its associations with dietary behavior and weight management. Appetite 2017, 110, 86–93. [Google Scholar] [CrossRef]
- Boyer, K.; Orpin, P.; King, A.C. ‘I come for the friendship’: Why social eating matters. Australas. J. Ageing 2016, 35, E29–E31. [Google Scholar] [CrossRef]
- McHugh, J.; Lee, O.; Lawlor, B.; Brennan, S. The meaning of mealtimes: Social and nutritional needs identified among older adults attending day services and by healthcare professionals. Int. J. Geriatr. Psychiatry 2015, 30, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Saeed, A.; Fisher, J.; Mitchell-Smith, Z.; Brown, L.J.E. “You’ve Got to Be Old to Go There”: Psychosocial Barriers and Facilitators to Social Eating in Older Adults. Gerontologist 2020, 60, 628–637. [Google Scholar] [CrossRef]
- Lengyel, C.O.; Jiang, D.; Tate, R.B. Trajectories of nutritional risk: The Manitoba follow-up study. J. Nutr. Health Aging 2017, 21, 604–609. [Google Scholar] [CrossRef]
- Wham, C.; Carr, R.; Heller, F. Country of origin predicts nutrition risk among community living older people. J. Nutr. Health Aging 2011, 15, 253–258. [Google Scholar] [CrossRef]
- Quigley, K.K.; Hermann, J.R.; Warde, W.D. Nutritional risk among Oklahoma congregate meal participants. J. Nutr. Educ. Behav. 2008, 40, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Posner, B.M.; Jette, A.M.; Smith, K.W.; Miller, D.R. Nutrition and health risks in the elderly: The nutrition screening initiative. Am. J. Public Health 1993, 83, 972–978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shahar, D.; Shai, I.; Vardi, H.; Fraser, D. Dietary intake and eating patterns of elderly people in Israel: Who is at nutritional risk? Eur. J. Clin. Nutr. 2003, 57, 18–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boulos, C.; Salameh, P.; Barberger-Gateau, P. Social isolation and risk for malnutrition among older people. Geriatr. Gerontol. Int. 2017, 17, 286–294. [Google Scholar] [CrossRef]
- Ferry, M.; Sidobre, B.; Lambertin, A.; Barberger-Gateau, P. The SOLINUT study: Analysis of the interaction between nutrition and loneliness in persons aged over 70 years. J. Nutr. Health Aging 2005, 9, 261–268. [Google Scholar]
- Ashida, S.; Sewell, D.K.; Schafer, E.J.; Schroer, A.; Friberg, J. Social network members who engage in activities with older adults: Do they bring more social benefits than other members? Ageing Soc. 2019, 39, 1050–1069. [Google Scholar] [CrossRef] [Green Version]
- Husted, M.M.; Beck, A.M.; Ulrikkeholm, L.K. Involving community-dwelling older adults in activities related to meals as part of a rehabilitation program: A single-blinded cluster-controlled study. Clin. Rehabil. 2019, 33, 1185–1196. [Google Scholar] [CrossRef]
- Clausen, T.; Wilson, A.O.; Molebatsi, R.M.; Holmboe-Ottesen, G. Diminished mental- and physical function and lack of social support are associated with shorter survival in community dwelling older persons of Botswana. BMC Public Health 2007, 7. [Google Scholar] [CrossRef] [Green Version]
- Hegge, M. A qualitative retrospective study of coping strategies of newly widowed elderly: Effects of anticipatory grieving on the caregiver. Am. J. Hosp. Palliat. Care 1991, 8, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Pettigrew, S.; Roberts, M. Addressing loneliness in later life. Aging Ment. Health 2008, 12, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Bloom, I.; Lawrence, W.; Barker, M.; Baird, J.; Dennison, E.; Sayer, A.A.; Cooper, C.; Robinson, S. What influences diet quality in older people? A qualitative study among community-dwelling older adults from the Hertfordshire Cohort Study, UK. Public Health Nutr. 2017, 20, 2685–2693. [Google Scholar] [CrossRef] [Green Version]
- Whitelock, E.; Ensaff, H. On Your Own: Older Adults’ Food Choice and Dietary Habits. Nutrients 2018, 10, 413. [Google Scholar] [CrossRef] [Green Version]
- Cohen, N.; Cribbs, K. The everyday food practices of community-dwelling Lesbian, Gay, Bisexual, and Transgender (LGBT) older adults. J. Aging Stud. 2017, 41, 75–83. [Google Scholar] [CrossRef] [Green Version]
- Johnson, C.S. Nutritional considerations for bereavement and coping with grief. J. Nutr. Health Aging 2002, 6, 171–176. [Google Scholar]
- Foley, E.; BeLue, R. Identifying Barriers and Enablers in the Dietary Management of Type 2 Diabetes in M’Bour, Senegal. J. Transcult. Nurs. 2017, 28, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Knutsen, I.R.; Foss, I.C.; Todorova, E.; Roukova, P.; Kennedy, A.; Portillo, M.C.; Regaira, E.; Serrano-Gil, M.; Lionis, C.; Angelaki, A.; et al. Negotiating Diet in Networks: A Cross-European Study of the Experiences of Managing Type 2 Diabetes. Qual. Health Res. 2017, 27, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Jager, M.J.; van der Sande, R.; Essink-Bot, M.L.; van den Muijsenbergh, M. Views and experiences of ethnic minority diabetes patients on dietetic care in the Netherlands—A qualitative study. Eur. J. Public Health 2019, 29, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Plastow, N.A.; Atwal, A.; Gilhooly, M. Food Activities and Identity Maintenance Among Community-Living Older Adults: A Grounded Theory Study. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 2015, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti Fidanza, A. Nutritional status of the elderly. IV. Nutritional knowledge, food preferences and life styles connected with the nutritional process. Int. J. Vitam. Nutr. Res. 1984, 54, 361–369. [Google Scholar]
- De Castro, J.M. Age-related-changes in spontaneous food-intake and hunger in humans. Appetite 1993, 21, 255–272. [Google Scholar] [CrossRef]
- De Castro, J.M. Age-related changes in the social, psychological, and temporal influences on food intake in free-living, healthy, adult humans. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2002, 57, M368–M377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dean, W.R.; Sharkey, J.R.; Nalty, C.C.; Xu, J. Government Capital, Intimate and Community Social Capital, and Food Security Status in Older Adults with Different Income Levels. Rural Sociol. 2014, 79, 505–531. [Google Scholar] [CrossRef]
- Getty, M.D.; Mueller, M.; Amella, E.J.; Fraser, A.M. Differences in Medical and Life-style Risk Factors for Malnutrition in Limited-Resource Older Adults in a Rural U.S. State: A Descriptive Study. J. Nutr. Health Aging 2016, 20, 121–127. [Google Scholar] [CrossRef]
- Holm, L.; Lauridsen, D.; Lund, T.B.; Gronow, J.; Niva, M.; Makela, J. Changes in the social context and conduct of eating in four Nordic countries between 1997 and 2012. Appetite 2016, 103, 358–368. [Google Scholar] [CrossRef] [PubMed]
- Holmes, B.A.; Roberts, C.L. Diet quality and the influence of social and physical factors on food consumption and nutrient intake in materially deprived older people. Eur. J. Clin. Nutr. 2011, 65, 538–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holmes, B.A.; Roberts, C.L.; Nelson, M. How access, isolation and other factors may influence food consumption and nutrient intake in materially deprived older men in the UK. Nutr. Bull. 2008, 33, 212–220. [Google Scholar] [CrossRef]
- Ishikawa, M.; Yokoyama, T.; Hayashi, F.; Takemi, Y.; Nakaya, T.; Fukuda, Y.; Kusama, K.; Nozue, M.; Yoshiike, N.; Murayama, N. Subjective Well-Being Is Associated with Food Behavior and Demographic Factors in Chronically Ill Older Japanese People Living Alone. J. Nutr. Health Aging 2018, 22, 341–353. [Google Scholar] [CrossRef]
- Keller, H.H.; Goy, R.; Kane, S.L. Validity and reliability of SCREEN II (Seniors in the Community: Risk evaluation for eating and nutrition, Version II). Eur. J. Clin. Nutr. 2005, 59, 1149–1157. [Google Scholar] [CrossRef] [Green Version]
- Nicholas, M.; Jennelle, L.; Connor, L.T.; Haynes, C.; Zipse, L. Do caregiver proxy reports and congruence of client-proxy activity participation goals relate to quality of life in people with aphasia? Int. J. Lang. Commun. Disord. 2020, 55, 373–386. [Google Scholar] [CrossRef]
- Porter, K.; Keary, S.; VanWagenen, A.; Bradford, J. Social Network and Nutritional Value of Congregate Meal Programs: Differences by Sexual Orientation. J. Appl. Gerontol. 2016, 35, 960–981. [Google Scholar] [CrossRef] [PubMed]
- Rosenbloom, C.A.; Whittington, F.J. The effects of bereavement on eating behaviors and nutrient intakes in elderly widowed persons. J. Gerontol. 1993, 48, S223–S229. [Google Scholar] [CrossRef]
- Rugel, E.J.; Carpiano, R.M. Gender differences in the roles for social support in ensuring adequate fruit and vegetable consumption among older adult Canadians. Appetite 2015, 92, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Swan, J.H.; Severance, J.J.; Turner, K. Senior Centers and Nutritional Outcomes: A Texas Example. Soc. Work Public Health 2016, 31, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Toner, H.; Morris, J. A Social-Psychological Perspective of Dietary Quality in Later Adulthood. J. Nutr. Elder. 1993, 11, 35–53. [Google Scholar] [CrossRef]
- Waring, M.L.; Kosberg, J.I. Morale and the differential use among the Black elderly of social welfare services delivered by volunteers. J. Gerontol. Soc. Work 1984, 6, 81–94. [Google Scholar] [CrossRef]
- Asamane, E.A.; Greig, C.A.; Aunger, J.A.; Thompson, J.L. Perceptions and Factors Influencing Eating Behaviours and Physical Function in Community-Dwelling Ethnically Diverse Older Adults: A Longitudinal Qualitative Study. Nutrients 2019, 11, 1224. [Google Scholar] [CrossRef] [Green Version]
- Byker Shanks, C.; Haack, S.; Tarabochia, D.; Bates, K.; Christenson, L. Factors Influencing Food Choices Among Older Adults in the Rural Western USA. J. Community Health 2017, 42, 511–521. [Google Scholar] [CrossRef] [PubMed]
- Falciglia, G.; Wahlbrink, D.; Suszkiw, D. Factors of change in elderly eating-related behaviors: An anthropological perspective. J. Nutr. Elder. 1985, 5, 67–77. [Google Scholar] [CrossRef]
- Falk, L.W.; Bisogni, C.A.; Sobal, J. Food choice processes of older adults: A qualitative investigation. J. Nutr. Educ. 1996, 28, 257–265. [Google Scholar] [CrossRef]
- Howell, B.M.; Bardach, S.H. “It’s a Social Thing”: Sociocultural Experiences with Nutrition and Exercise in Anchorage, Alaska. Arct. Anthrop. 2018, 55, 1–16. [Google Scholar] [CrossRef]
- Sriram, U.; Morgan, E.H.; Graham, M.L.; Folta, S.C.; Seguin, R.A. Support and Sabotage: A Qualitative Study of Social Influences on Health Behaviors Among Rural Adults. J. Rural Health 2018, 34, 88–97. [Google Scholar] [CrossRef] [Green Version]
- Tessier, S.; Gerber, M. Comparison between Sardinia and Malta: The Mediterranean diet revisited. Appetite 2005, 45, 121–126. [Google Scholar] [CrossRef]
- Thompson, J.; Tod, A.; Bissell, P.; Bond, M. Understanding food vulnerability and health literacy in older bereaved men: A qualitative study. Health Expect. 2017, 20, 1342–1349. [Google Scholar] [CrossRef] [PubMed]
- Uribe, A.C.R. “I Go Upstairs and Eat in Front of the Television”: The Cooking and Eating Behaviors of Mexican Older Women Living Alone. J. Cross. Cult. Gerontol. 2019, 34, 171–186. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, K.; Sidenvall, B. Food-related health perceptions and food habits among older women. J. Adv. Nurs. 2002, 39, 164–173. [Google Scholar] [CrossRef]
- Hughes, G.; Bennett, K.M.; Hetherington, M.M. Old and alone: Barriers to healthy eating in older men living on their own. Appetite 2004, 43, 269–276. [Google Scholar] [CrossRef]
- Shifflett, P.A. Future time perspective, past experiences, and negotiation of food use patterns among the aged. Gerontologist 1987, 27, 611–615. [Google Scholar] [CrossRef]
- Zelig, R.; Jones, V.M.; Touger-Decker, R.; Hoskin, E.R.; Singer, S.R.; Byham-Gray, L.; Radler, D.R.; Rothpletz-Puglia, P. The Eating Experience: Adaptive and Maladaptive Strategies of Older Adults with Tooth Loss. JDR Clin. Transl. Res. 2019, 4, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Porter, J.; Ottrey, E.; Huggins, C.E. Protected Mealtimes in Hospitals and Nutritional Intake: Systematic Review and Meta-Analyses; Elsevier Ltd.: London, UK, 2017; Volume 65, pp. 62–69. [Google Scholar]
- Valtorta, N.K.; Kanaan, M.; Gilbody, S.; Hanratty, B. Loneliness, social isolation and social relationships: What are we measuring? A novel framework for classifying and comparing tools. BMJ Open 2016, 6, e010799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Victor, C.; Grenade, L.; Boldy, D. Measuring loneliness in later life: A comparison of differing measures. Rev. Clin. Gerontol. 2006, 15, 63–70. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.; Glorieux, I.; Minnen, J.; van Tienoven, T.P. More than preparing a meal? Concerning the meanings of home cooking. Appetite 2012, 58, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
- Neuman, N.; Gottzén, L.; Fjellström, C. Masculinity and the sociality of cooking in men’s everyday lives. Sociol. Rev. 2017, 65, 816–831. [Google Scholar] [CrossRef]
- Allal, A.S.; Dulguerov, P.; Bieri, S.; Lehmann, W.; Kurtz, J.M. Assessment of quality of life in patients treated with accelerated radiotherapy for laryngeal and hypopharyngeal carcinomas. Head Neck 2000, 22, 288–293. [Google Scholar] [CrossRef]
- Allal, A.S.; Nicoucar, K.; Mach, N.; Dulguerov, P. Quality of life in patients with oropharynx carcinomas: Assessment after accelerated radiotherapy with or without chemotherapy versus radical surgery and postoperative radiotherapy. Head Neck 2003, 25, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Kjær, T.K.; Johansen, C.; Andersen, E.; Karlsen, R.; Nielsen, A.L.; Frederiksen, K.; Rorth, M.; Ibfelt, E.; Dalton, S.O. Influence of social factors on patient-reported late symptoms: Report from a controlled trial among long-term head and neck cancer survivors in Denmark. Head Neck 2016, 38 (Suppl. 1), E1713–E1721. [Google Scholar] [CrossRef] [PubMed]
- Hoerster, K.D.; Wilson, S.; Nelson, K.M.; Reiber, G.E.; Masheb, R.M. Diet quality is associated with mental health, social support, and neighborhood factors among Veterans. Eat. Behav. 2016, 23, 168–173. [Google Scholar] [CrossRef]
- Wham, C.A.; Teh, R.; Moyes, S.; Dyall, L.; Kepa, M.; Hayman, K.; Kerse, N. Health and social factors associated with nutrition risk: Results from life and living in advanced age: A cohort study in New Zealand (LILACS NZ). J. Nutr. Health Aging 2015, 19, 637–645. [Google Scholar] [CrossRef]
- Ang, S. Social Participation and Mortality Among Older Adults in Singapore: Does Ethnicity Explain Gender Differences? J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2018, 73, 1470–1479. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.-I. Using the Theory of Planned Behavior to Assess Participation in Congregate Meal Programs; ProQuest Information & Learning: Ann Arbor, MI, USA, 2009. [Google Scholar]
- Cerin, E.; Nathan, A.; Choi, W.K.; Ngan, W.; Yin, S.; Thornton, L.; Barnett, A. Built and social environmental factors influencing healthy behaviours in older Chinese immigrants to Australia: A qualitative study. Int. J. Behav. Nutr. Phys. Act. 2019, 16. [Google Scholar] [CrossRef] [Green Version]
- Byeon, H. Predicting the Swallow-Related Quality of Life of the Elderly Living in a Local Community Using Support Vector Machine. Int. J. Environ. Res. Public Health 2019, 16, 4269. [Google Scholar] [CrossRef] [Green Version]
- Lai, X.J.; Lam, W.H.K.; Su, J.B.; Fu, H. Modelling intra-household interactions in time-use and activity patterns of retired and dual-earner couples. Transp. Res. Part A Policy Pract. 2019, 126, 172–194. [Google Scholar] [CrossRef]
- Quandt, S.A.; Rao, P. Hunger and food security among older adults in a rural community. Hum. Organ. 1999, 58, 28–35. [Google Scholar] [CrossRef]
- Arcury, T.A.; Grzywacz, J.G.; Ip, E.H.; Saldana, S.; Nguyen, H.T.; Bell, R.A.; Kirk, J.K.; Quandt, S.A. Social integration and diabetes management among rural older adults. J. Aging Health 2012, 24, 899–922. [Google Scholar] [CrossRef] [PubMed]
- Mamalaki, E.; Anastasiou, C.A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Scarmeas, N.; Yannakoulia, M. Social life characteristics in relation to adherence to the Mediterranean diet in older adults: Findings from the Hellenic Longitudinal Investigation of Aging and Diet (HELIAD) study. Public Health Nutr. 2020, 23, 439–445. [Google Scholar] [CrossRef] [PubMed]
- van den Heuvel, E.; Murphy, J.L.; Appleton, K.M. Could Eggs Help Increase Dietary Protein Intake in Older Adults?—Exploring Reasons for the Consumption and Non-Consumption of Eggs in People over 55 years old. J. Nutr. Gerontol. Geriatr. 2018, 37, 292–309. [Google Scholar] [CrossRef] [PubMed]
- Zou, P. Facilitators and Barriers to Healthy Eating in Aged Chinese Canadians with Hypertension: A Qualitative Exploration. Nutrients 2019, 11, 111. [Google Scholar] [CrossRef] [Green Version]
- Glover, L.; Dyson, J.; Cowdell, F.; Kinsey, D. Healthy ageing in a deprived northern UK city: A co-creation study. Health Soc. Care Commun. 2020. [Google Scholar] [CrossRef]
- Howell, B.M. Interactions between Diet, Physical Activity, and the Sociocultural Environment for Older Adult Health in the Urban Subarctic. J. Commun. Health 2020, 45, 252–263. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, D.; Reis, E.; Ferreira, P.; Schindler, A. Measuring Quality of Life in the Speaker with Dysarthria: Reliability and Validity of the European Portuguese Version of the QoL-DyS. Folia Phoniatr. Logop. 2019, 71, 176–190. [Google Scholar] [CrossRef]
- United Nations. Methodology: Geographic Regions. Available online: https://unstats.un.org/unsd/methodology/m49/ (accessed on 15 May 2020).
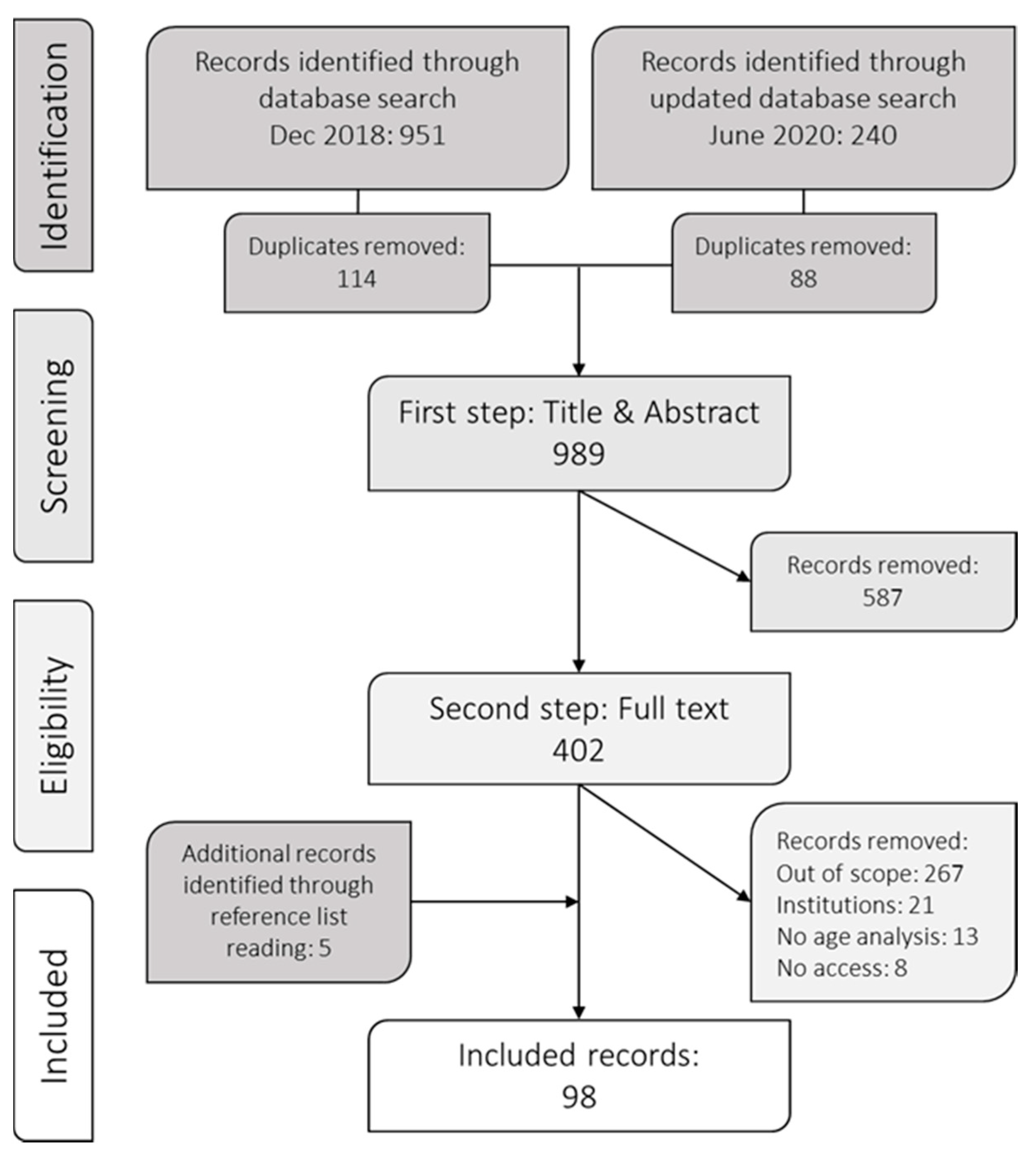
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Björnwall, A.; Mattsson Sydner, Y.; Koochek, A.; Neuman, N. Eating Alone or Together among Community-Living Older People—A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 3495. https://doi.org/10.3390/ijerph18073495
Björnwall A, Mattsson Sydner Y, Koochek A, Neuman N. Eating Alone or Together among Community-Living Older People—A Scoping Review. International Journal of Environmental Research and Public Health. 2021; 18(7):3495. https://doi.org/10.3390/ijerph18073495
Chicago/Turabian StyleBjörnwall, Amanda, Ylva Mattsson Sydner, Afsaneh Koochek, and Nicklas Neuman. 2021. "Eating Alone or Together among Community-Living Older People—A Scoping Review" International Journal of Environmental Research and Public Health 18, no. 7: 3495. https://doi.org/10.3390/ijerph18073495
APA StyleBjörnwall, A., Mattsson Sydner, Y., Koochek, A., & Neuman, N. (2021). Eating Alone or Together among Community-Living Older People—A Scoping Review. International Journal of Environmental Research and Public Health, 18(7), 3495. https://doi.org/10.3390/ijerph18073495








