The Comparisons of Physical Functional Performances between Older Adults with and without Regular Physical Activity in Two Different Living Settings
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Study Design
2.3. Physical Functional Performance
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Robb, B. Exercise and Physical Activity: What’s the Difference? 2009. Available online: http://www.everydayhealth.com/fitness/basics/difference-between-exercise-and-physical-activity.aspx (accessed on 18 November 2014).
- Daskalopoulou, C.; Stubbs, B.; Kralj, C.; Koukounari, A.; Prince, M.; Prina, A. Physical activity and healthy ageing: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res. Rev. 2017, 38, 6–17. [Google Scholar] [CrossRef] [Green Version]
- Goodpaster, B.H.; Chomentowski, P.; Ward, B.K.; Rossi, A.; Glynn, N.W.; Delmonico, M.J.; Kritchevsky, S.B.; Pahor, M.; Newman, A.B. Effects of physical activity on strength and skeletal muscle fat infiltration in older adults: A randomized controlled trial. J. Appl. Physiol. 2008, 105, 1498–1503. [Google Scholar] [CrossRef] [Green Version]
- Goh, V.H.H.; Hart, W.G. Associations of physical exercise as a lifestyle habit with lean and fat body mass and handgrip strength and age in Asian men. Aging Male 2014, 17, 131–135. [Google Scholar] [CrossRef]
- Tak, E.; Kuiper, R.; Chorus, A.; Hopman-Rock, M. Prevention of onset and progression of basic ADL disability by physical activity in community dwelling older adults: A meta-analysis. Ageing Res. Rev. 2013, 12, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Akune, T.; Muraki, S.; Oka, H.; Tanaka, S.; Kawaguchi, H.; Nakamura, K.; Yoshimura, N. Exercise habits during middle age are associated with lower prevalence of sarcopenia: The ROAD study. Osteoporos. Int. 2013, 25, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Steffl, M.; Bohannon, R.W.; Sontakova, L.; Tufano, J.J.; Shiells, K.; Holmerova, I. Relationship between sarcopenia and physical activity in older people: A systematic review and meta-analysis. Clin. Interv. Aging 2017, 12, 835–845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rantanen, T.; Heikkinen, E. The Role of Habitual Physical Activity in Preserving Muscle Strength from Age 80 to 85 Years. J. Aging Phys. Act. 1998, 6, 121–132. [Google Scholar] [CrossRef]
- Daly, R.M.; Ahlborg, H.G.; Ringsberg, K.; Gärdsell, P.; Sernbo, I.; Karlsson, M.K. Association Between Changes in Habitual Physical Activity and Changes in Bone Density, Muscle Strength, and Functional Performance in Elderly Men and Women. J. Am. Geriatr. Soc. 2008, 56, 2252–2260. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, C.; Sullivan, R.O.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef]
- Kamijo, T.; Murakami, M. Regular Physical Exercise Improves Physical Motor Functions and Biochemical Markers in Middle-Age and Elderly Women. J. Phys. Act. Health 2009, 6, 55–62. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, G.; Thomas, E.L.; McCarthy, J.P.; Fitzpatrick, J.; Durighel, G.; Mehta, S.; Morin, S.X.; Goldstone, A.P.; Bell, J.D. Fat distribution in men of different waist girth, fitness level and exercise habit. Int. J. Obes. 2009, 33, 1356–1362. [Google Scholar] [CrossRef] [Green Version]
- Samitz, G.; Egger, M.; Zwahlen, M. Domains of physical activity and all-cause mortality: Systematic review and dose—Response meta—Analysis of cohort studies. Int. J. Epidemiol. 2011, 40, 1382–1400. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira, A.S.; Santos, A.D.C.; Trombetta, I.C.; Dantas, M.M.; Silvestre, A.C.O.M.; Nascimento, L.S.D.; Barbosa, B.T.; Dos Santos, M.R.; Andrade, M.D.A.; De Lima, A.M.J.; et al. Regular physical exercise improves cardiac autonomic and muscle vasodilatory responses to isometric exercise in healthy elderly. Clin. Interv. Aging 2017, 12, 1021–1028. [Google Scholar] [CrossRef] [Green Version]
- Aune, D.; Norat, T.; Leitzmann, M.F.; Tonstad, S.; Vatten, L.J. Physical activity and the risk of type 2 diabetes: A systematic review and dose—Response meta—Analysis. Eur. J. Epidemiol. 2015, 30, 529–542. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Hu, F.; Li, D.; Wang, F.; Zhu, L.; Chen, W.; Ge, J.; An, R.; Zhao, Y. Does Physical Activity Reduce the Risk of Prostate Cancer? A Systematic Review and Meta-analysis. Eur. Urol. 2011, 60, 1029–1044. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhang, D.; Kang, S. Physical activity and risk of breast cancer: A meta-analysis of prospective studies. Breast Cancer Res. Treat. 2012, 137, 869–882. [Google Scholar] [CrossRef]
- Blondell, S.J.; Hammersley-Mather, R.; Veerman, J.L. Does physical activity prevent cognitive decline and dementia? A systematic review and meta-analysis of longitudinal studies. BMC Public Health 2014, 14, 510. [Google Scholar] [CrossRef] [Green Version]
- George, E.K.; Reddy, P.H. Can Healthy Diets, Regular Exercise, and Better Lifestyle Delay the Progression of Dementia in Elderly Individuals? J. Alzheimers Dis. 2019, 72, S37–S58. [Google Scholar] [CrossRef] [PubMed]
- Lee, J. The Relationship Between Physical Activity and Dementia: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. J. Gerontol. Nurs. 2018, 44, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; De Leon, A.P.; Dunn, A.L.; Deslandes, A.C.; et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef] [PubMed]
- Geirsdottir, O.G.; Arnarson, A.; Briem, K.; Ramel, A.; Jonsson, P.V.; Thorsdottir, I. Effect of 12-Week Resistance Exercise Program on Body Composition, Muscle Strength, Physical Function, and Glucose Metabolism in Healthy, Insulin-Resistant, and Diabetic Elderly Icelanders. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2012, 67, 1259–1265. [Google Scholar] [CrossRef] [Green Version]
- Da Silva, V.D.; Tribess, S.; Meneguci, J.; Sasaki, J.E.; Garcia-Meneguci, C.A.; Carneiro, J.A.O.; Virtuoso, S., Jr. Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health 2019, 19, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Paw, M.J.M.C.A.; Van Uffelen, J.G.Z.; I Riphagen, I.; Van Mechelen, W. The Functional Effects of Physical Exercise Training in Frail Older People. Sports Med. 2008, 38, 781–793. [Google Scholar] [CrossRef] [PubMed]
- Baker, M.K.; Atlantis, E.; Singh, M.A.F. Multi-modal exercise programs for older adults. Age Ageing 2007, 36, 375–381. [Google Scholar] [CrossRef] [Green Version]
- Lord, S.R.; Matters, B.; George, R.S.; Thomas, M.; Bindon, J.; Chan, D.K.; Collings, A.; Haren, L. The effects of water exercise on physical functioning in older people. Australas. J. Ageing 2006, 25, 36–41. [Google Scholar] [CrossRef]
- Rendon, A.A.; Lohman, E.B.; Thorpe, D.; Johnson, E.G.; Medina, E.; Bradley, B. The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing 2012, 41, 549–552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, W.; Park, H.-Y.; Lim, K.; Park, J. The role of habitual physical activity on arterial stiffness in elderly Individuals: A systematic review and meta-analysis. J. Exerc. Nutr. Biochem. 2017, 21, 16–21. [Google Scholar] [CrossRef]
- Huang, P.H.; Hsueh, M.C.; Liao, Y. Physical Activity Guidelines and Recommendations for Older Adults of Different Countries. J. Sports Res. 2018, 27, 1–12. [Google Scholar] [CrossRef]
- Health Promotion Administration, Ministry of Health and Welfare, R.O.C. (Taiwan). Taiwan Physical Activity Guidelines; Health Promotion Administration, Ministry of Health and Welfare, R.O.C. (Taiwan): Taipei, Taiwan, 2017.
- Chang, S.; Chien, N.; Wai, J.P.; Chiang, C.; Yu, C. Examining the links between regular leisure-time physical activity, sitting time and prefrailty in community-dwelling older adults. J. Adv. Nurs. 2021. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Lindquist, L.A.; Chang, R.W.; Semanik, P.A.; Ehrlich-Jones, L.S.; Lee, J.; Sohn, M.-W.; Dunlop, D.D. Sedentary Behavior as a Risk Factor for Physical Frailty Independent of Moderate Activity: Results From the Osteoarthritis Initiative. Am. J. Public Health 2015, 105, 1439–1445. [Google Scholar] [CrossRef]
- Król-Zielińska, M.; Kusy, K.; Zieliński, J.; Osiński, W. Physical activity and functional fitness in institutionalized vs. independently living elderly: A comparison of 70–80-year-old city-dwellers. Arch. Gerontol. Geriatr. 2011, 53, e10–e16. [Google Scholar] [CrossRef]
- Papiol, M.; Serra-Prat, M.; Vico, J.; Jerez, N.; Salvador, N.; García, M.; Camps, M.; Alpiste, X.; López, J. Poor Muscle Strength and Low Physical Activity are the Most Prevalent Frailty Components in Community-Dwelling Older Adults. J. Aging Phys. Act. 2016, 24, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.-H.; Hwang, C.-L.; Wu, Y.-T. Effect of Exercise on Physical Function, Daily Living Activities, and Quality of Life in the Frail Older Adults: A Meta-Analysis. Arch. Phys. Med. Rehabil. 2012, 93, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z.; Josephson, K.R.; Trueblood, P.R.; Loy, S.; Harker, J.O.; Pietruszka, F.M.; Robbins, A.S. Effects of a Group Exercise Program on Strength, Mobility, and Falls Among Fall-Prone Elderly Men. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2000, 55, M317–M321. [Google Scholar] [CrossRef]
- Morgan, R.O.; Virnig, B.A.; Duque, M.; Abdel-Moty, E.; DeVito, C.A. Low-Intensity Exercise and Reduction of the Risk for Falls Among At-Risk Elders. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2004, 59, M1062–M1067. [Google Scholar] [CrossRef]
- Lord, S.R.; Castell, S.; Corcoran, J.; Dayhew, J.; Matters, B.; Shan, A.; Williams, P. The Effect of Group Exercise on Physical Functioning and Falls in Frail Older People Living in Retirement Villages: A Randomized, Controlled Trial. J. Am. Geriatr. Soc. 2003, 51, 1685–1692. [Google Scholar] [CrossRef] [PubMed]
- Sahin, U.K.; Kirdi, N.; Bozoglu, E.; Meric, A.; Buyukturan, G.; Ozturk, A.; Doruk, H. Effect of low-intensity versus high-intensity resistance training on the functioning of the institutionalized frail elderly. Int. J. Rehabil. Res. 2018, 41, 211–217. [Google Scholar] [CrossRef]
- Shimada, H.; Uchiyama, Y.; Kakurai, S. Specific effects of balance and gait exercises on physical function among the frail elderly. Clin. Rehabil. 2003, 17, 472–479. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E. Measuring functional fitness of older adults. J. Act. Aging 2002, 1, 25–30. [Google Scholar]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Clarkson, H.M. Musculoskeletal Assessment: Joint Range of Motion and Manual Muscle Strength; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2000. [Google Scholar]
- Mathiowetz, V.; Volland, G.; Kashman, N.; Weber, K. Adult Norms for the Box and Block Test of Manual Dexterity. Am. J. Occup. 1985, 39, 386–391. [Google Scholar] [CrossRef] [Green Version]
- Rikli, R.E.; Jones, C.J. Development and Validation of a Functional Fitness Test for Community-Residing Older Adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Thomas, D.R.; Marren, K.; Banks, W.; Morley, J. Do Objective Measurements of Physical Function in Ambulatory Nursing Home Women Improve Assessment of Functional Status? J. Am. Med. Dir. Assoc. 2007, 8, 469–476. [Google Scholar] [CrossRef]
- Weiner, D.K.; Duncan, P.W.; Chandler, J.; Studenski, S.A. Functional Reach: A Marker of Physical Frailty. J. Am. Geriatr. Soc. 1992, 40, 203–207. [Google Scholar] [CrossRef]
- Buchner, D.M.; Beresford, S.A.; Larson, E.B.; Lacroix, A.Z.; Wagner, E.H. Effects of Physical Activity on Health Status in Older Adults II: Intervention Studies. Annu. Rev. Public Health 1992, 13, 469–488. [Google Scholar] [CrossRef] [PubMed]
- Chittrakul, J.; Siviroj, P.; Sungkarat, S.; Sapbamrer, R. Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 3102. [Google Scholar] [CrossRef] [PubMed]
- Rogers, N.T.; Marshall, A.; Roberts, C.H.; Demakakos, P.; Steptoe, A.; Scholes, S. Physical activity and trajectories of frailty among older adults: Evidence from the English Longitudinal Study of Ageing. PLoS ONE 2017, 12, e0170878. [Google Scholar] [CrossRef] [PubMed]
- Chiacchiero, M.; Dresely, B.; Silva, U.; Delosreyes, R.; Vorik, B. The Relationship Between Range of Movement, Flexibility, and Balance in the Elderly. Top. Geriatr. Rehabil. 2010, 26, 148–155. [Google Scholar] [CrossRef] [Green Version]
- Emilio, E.J.M.-L.; Hita-Contreras, F.; Jiménez-Lara, P.M.; Latorre-Román, P.; Martínez-Amat, A. The Association of Flexibility, Balance, and Lumbar Strength with Balance Ability: Risk of Falls in Older Adults. J. Sports Sci. Med. 2014, 13, 349–357. [Google Scholar] [PubMed]
- Rossi, P.G.; Carnavale, B.F.; Farche, A.C.S.; Ansai, J.H.; de Andrade, L.P.; Takahashi, A.C.D.M. Effects of physical exercise on the cognition of older adults with frailty syndrome: A systematic review and meta-analysis of randomized trials. Arch. Gerontol. Geriatr. 2021, 93, 104322. [Google Scholar] [CrossRef]
- Lopez, P.; Izquierdo, M.; Radaelli, R.; Sbruzzi, G.; Grazioli, R.; Pinto, R.S.; Cadore, E.L.; Shurzzi, G. Effectiveness of Multimodal Training on Functional Capacity in Frail Older People: A Meta-Analysis of Randomized Controlled Trials. J. Aging Phys. Act. 2018, 26, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Iosimuta, N.C.R.; Pessanha, F.P.A.S.; Alves, N.; Marques, L.T.; Porto, J.M.; Freire, R.C., Jr.; Ferriolli, E.; De Abreu, D.C.C. The effects of a multi-component intervention on the functional capacity, lower-body muscle strength, balance and gait in frail community-dwelling older people: A randomised controlled trial protocol. Eur. J. Physiother. 2019, 22, 262–273. [Google Scholar] [CrossRef]
- Zhang, J.-G.; Ohta, T.; Ishikawa-Takata, K.; Tabata, I.; Miyashita, M. Effects of daily activity recorded by pedometer on peak oxygen consumption (V˙O2peak), ventilatory threshold and leg extension power in 30- to 69-year-old Japanese without exercise habit. Graefe’s Arch. Clin. Exp. Ophthalmol. 2003, 90, 109–113. [Google Scholar] [CrossRef]
- Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; US Department of Health and Human Services: Washington, DC, USA, 2018.
- Choi, J.; Cho, Y.; Kim, Y.; Lee, S.; Lee, J.; Yi, Y.; Tak, Y.; Hwang, H.; Lee, S.; Park, E.; et al. The Relationship of Sitting Time and Physical Activity on the Quality of Life in Elderly People. Int. J. Environ. Res. Public Health 2021, 18, 1459. [Google Scholar] [CrossRef]
- Santos, D.A.; Silva, A.M.; Baptista, F.; Santos, R.; Vale, S.; Mota, J.; Sardinha, L.B. Sedentary behavior and physical activity are independently related to functional fitness in older adults. Exp. Gerontol. 2012, 47, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Zubala, A.; MacGillivray, S.; Frost, H.; Kroll, T.; Skelton, D.A.; Gavine, A.; Gray, N.M.; Toma, M.; Morris, J. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS ONE 2017, 12, e0180902. [Google Scholar] [CrossRef]



| Community-Dwelling (CD) Group | Day Care (DC) Center Group | |||
|---|---|---|---|---|
| RPA subgroup | NPA subgroup | RPA subgroup | NPA subgroup | |
| Item | (n = 35) | (n = 40) | (n = 47) | (n = 41) |
| Age | 74.4 ± 6.4 * | 77.9 ± 7.3 * | 79.8 ± 7.1 | 80.8 ± 6.8 |
| Gender | Female: 26 | Female: 22 | Female: 35 | Female: 32 |
| Male: 9 | Male: 18 | Male: 12 | Male: 9 | |
| Height (cm) | 154.99 ± 5.85 | 156.19 ± 8.91 | 151.62 ± 7.74 | 153.46 ± 9.1 |
| Weight (kg) | 57.23 ± 11.76 | 58.06 ± 9.24 | 54.70 ± 9.77 * | 58.59 ± 8.77 * |
| BMI (kg/m2) | 23.85 ± 4.93 | 24.23 ± 3.37 | 23.80 ± 3.81 | 25.04 ± 4.44 |
| Item | Description | Measure |
|---|---|---|
| BBT | The subjects are instructed to move one block at a time from one compartment to the other one of the test box as fast as possible, but in one minute. | Number of blocks |
| CSRT | The subjects are seated on a chair with knee straight, then being instructed to place one hand on the other with tips of the middle fingers flush. The subjects reach slowly toward the toes by bending their trunks while exhaling. Distance between the fingers and the toes was measured. Average of two trials. *A negative distance means that the fingertips did not reach the toes, while a positive score means that the fingertips reached beyond the toes. | cm |
| Muscle strength | Measured by a hand dynamometer (Jamar® Lafayette Instrument Company, Lafayette, IN, USA) for grip, a finger pinch gauge for pinch, and a digital dynamometer (MicroFET 3) for lower extremities. Average of three trials. | |
| grip | The subjects are seated, squeezing the hand dynamometer with their fingers as hard as they can without any body movement. | kg |
| pinch | The subjects are seated, squeezing the pinch gauge with their thumb and index fingers as hard as they can without any body movement. | kg |
| knee extensor | The subjects are seated, extending their knees against the resistance of the examiner applying on the anterior aspect of shanks proximal to their ankles. | kg |
| knee flexor | The subjects are prone, flexing their knees against the resistance of the examiner applying on the posterior aspect of shanks proximal to their ankles. | kg |
| hip abductor | The subjects are side lying, abducting their hips against the resistance of the examiner applying on the lateral aspect of their knee. | kg |
| STS | The subjects stand up and sit back from a straight-back chair three times as fast as possible with arm folded across the chest if possible. Time of three-time movements will be measured. Average of two trials. | sec |
| MST | The subjects are stepping alternatively as fast as possible while being seated for one minute. When one leg is raising, the foot should be completely off the ground. The score is the repetition number of stepping for one minute. | 1/min |
| 6-M walk | The subjects have to walk 6 m as fast as possible (with or without walking aid). Time of the movement will be recorded. | sec |
| FRT | The subjects are standing upright, stretching their arms forward, maintaining a fixed base of support while leaning forward is allowed. The distance between the front end of their fists before and after the movement will be measured. Average of two trials. | cm |
| CD-RPA | CD-NPA | p-Value | |
|---|---|---|---|
| Item | (n = 35) | (n = 40) | |
| Grip (kg) | |||
| dominant | 21.05 ± 6.68 | 18.03 ± 5.25 | 0.031 * |
| nondominant | 18.67 ± 6.18 | 18.57 ± 5.69 | 0.942 |
| Pinch (kg) | |||
| dominant | 7.85 ± 3.89 | 4.74 ± 1.46 | <0.001 *** |
| nondominant | 6.86 ± 3.73 | 4.44 ± 1.47 | 0.001 ** |
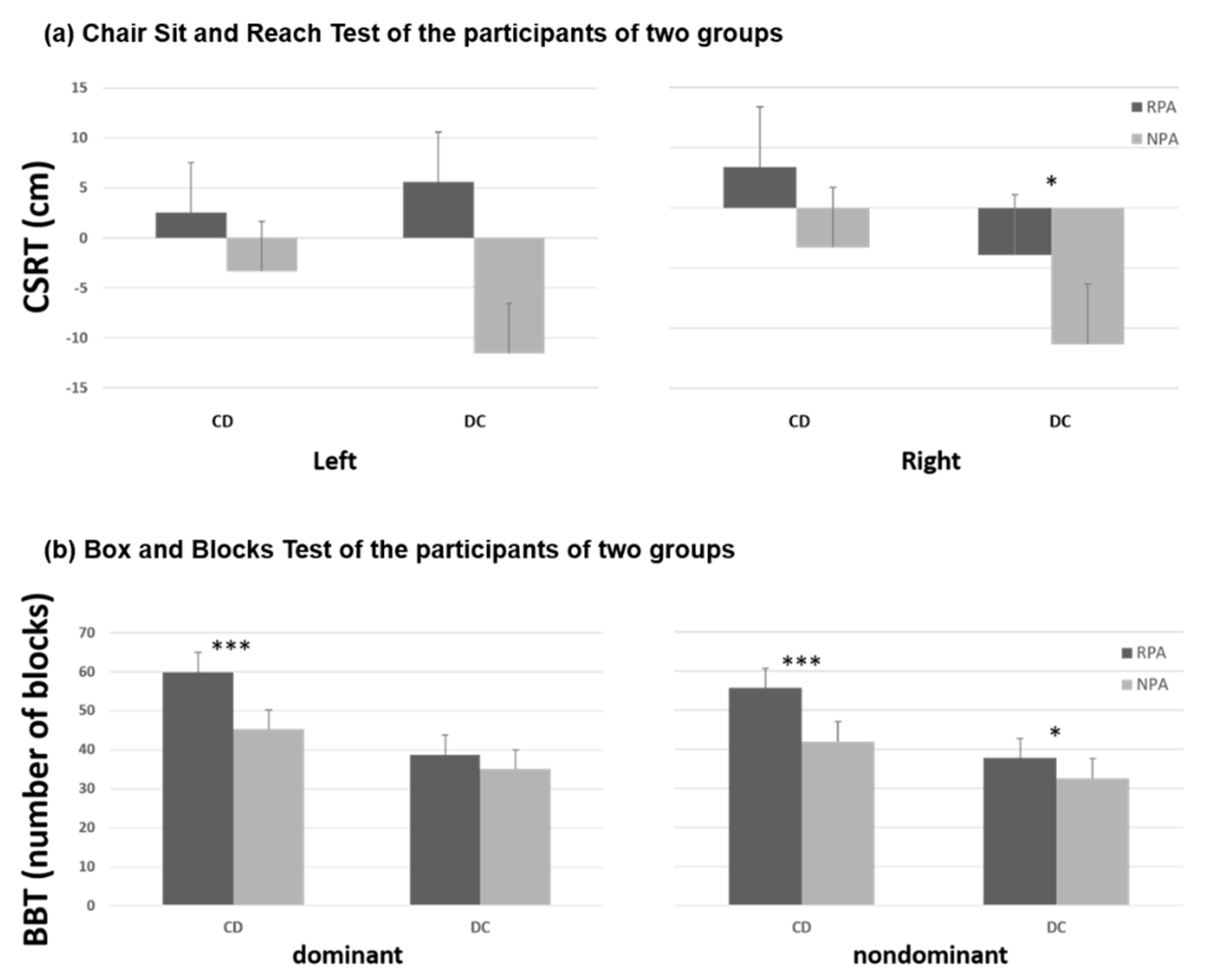
| CSRT (cm) | |||
| right | 3.40 ± 11.27 | −3.32 ± 11.23 | 0.059 |
| left | 2.57 ± 11.58 | −3.38 ± 11.32 | 0.101 |
| BBT (number of blocks) | |||
| dominant | 59.9 ± 9.2 | 45.2 ± 11.9 | <0.001 *** |
| nondominant | 55.7 ± 7.6 | 42.0 ± 9.9 | <0.001 *** |
| Knee extensor (kg) | |||
| right | 13.31 ± 3.46 | 10.82 ± 5.42 | 0.057 |
| left | 12.50 ± 3.45 | 10.94 ± 5.46 | 0.228 |
| Knee flexor (kg) | |||
| right | 11.70 ± 3.01 | 10.51 ± 4.49 | 0.357 |
| left | 11.29 ± 2.99 | 10.04 ± 4.49 | 0.335 |
| Hip abductor (kg) | |||
| right | 13.80 ± 3.42 | 12.16 ± 4.36 | 0.158 |
| left | 14.12 ± 7.26 | 11.16 ± 4.49 | 0.151 |
| DC-RPA | DC-NPA | p-Value | |
|---|---|---|---|
| Item | (n = 47) | (n = 41) | |
| Grip (kg) | |||
| dominant | 16.33 ± 7.81 | 10.71 ± 4.12 | <0.001 *** |
| nondominant | 14.55 ± 6.56 | 9.74 ± 6.07 | 0.001 *** |
| Pinch (kg) | |||
| dominant | 4.29 ± 1.49 | 3.57 ± 1.43 | 0.023 * |
| nondominant | 3.86 ± 1.43 | 3.36 ± 2.72 | 0.286 |
| CSRT (cm) | |||
| right | −3.89 ± 8.53 | −11.35 ± 12.95 | 0.031 * |
| left | 5.61 ± 9.27 | −11.55 ± 12.62 | 0.083 |
| BBT (number of blocks) | |||
| dominant | 38.7 ± 10.1 | 35.0 ± 12.9 | 0.131 |
| nondominant | 37.8 ± 11.0 | 32.6 ± 11.8 | 0.039 * |
| STS (sec) | 9.18 ± 5.96 | 13.83 ± 9.98 | 0.037 * |
| MST (1/min) | 188.00 ± 62.14 | 130.54 ± 46.51 | 0.002 ** |
| 6-M walk (sec) | 22.04 ± 20.66 | 23.75 ± 20.29 | 0.772 |
| FRT (cm) | 16.53 ± 6.26 | 16.46 ± 9.36 | 0.98 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, I.-F.; Kuo, L.-C.; Tsai, Y.-J.; Su, F.-C. The Comparisons of Physical Functional Performances between Older Adults with and without Regular Physical Activity in Two Different Living Settings. Int. J. Environ. Res. Public Health 2021, 18, 3561. https://doi.org/10.3390/ijerph18073561
Cheng I-F, Kuo L-C, Tsai Y-J, Su F-C. The Comparisons of Physical Functional Performances between Older Adults with and without Regular Physical Activity in Two Different Living Settings. International Journal of Environmental Research and Public Health. 2021; 18(7):3561. https://doi.org/10.3390/ijerph18073561
Chicago/Turabian StyleCheng, I-Fang, Li-Chieh Kuo, Yi-Jung Tsai, and Fong-Chin Su. 2021. "The Comparisons of Physical Functional Performances between Older Adults with and without Regular Physical Activity in Two Different Living Settings" International Journal of Environmental Research and Public Health 18, no. 7: 3561. https://doi.org/10.3390/ijerph18073561





