Postural Sensorimotor Control on Anorectal Pressures and Pelvic Floor Muscle Tone and Strength: Effects of a Single 5P® LOGSURF Session. A Cross-Sectional Preliminary Study
Abstract
1. Introduction
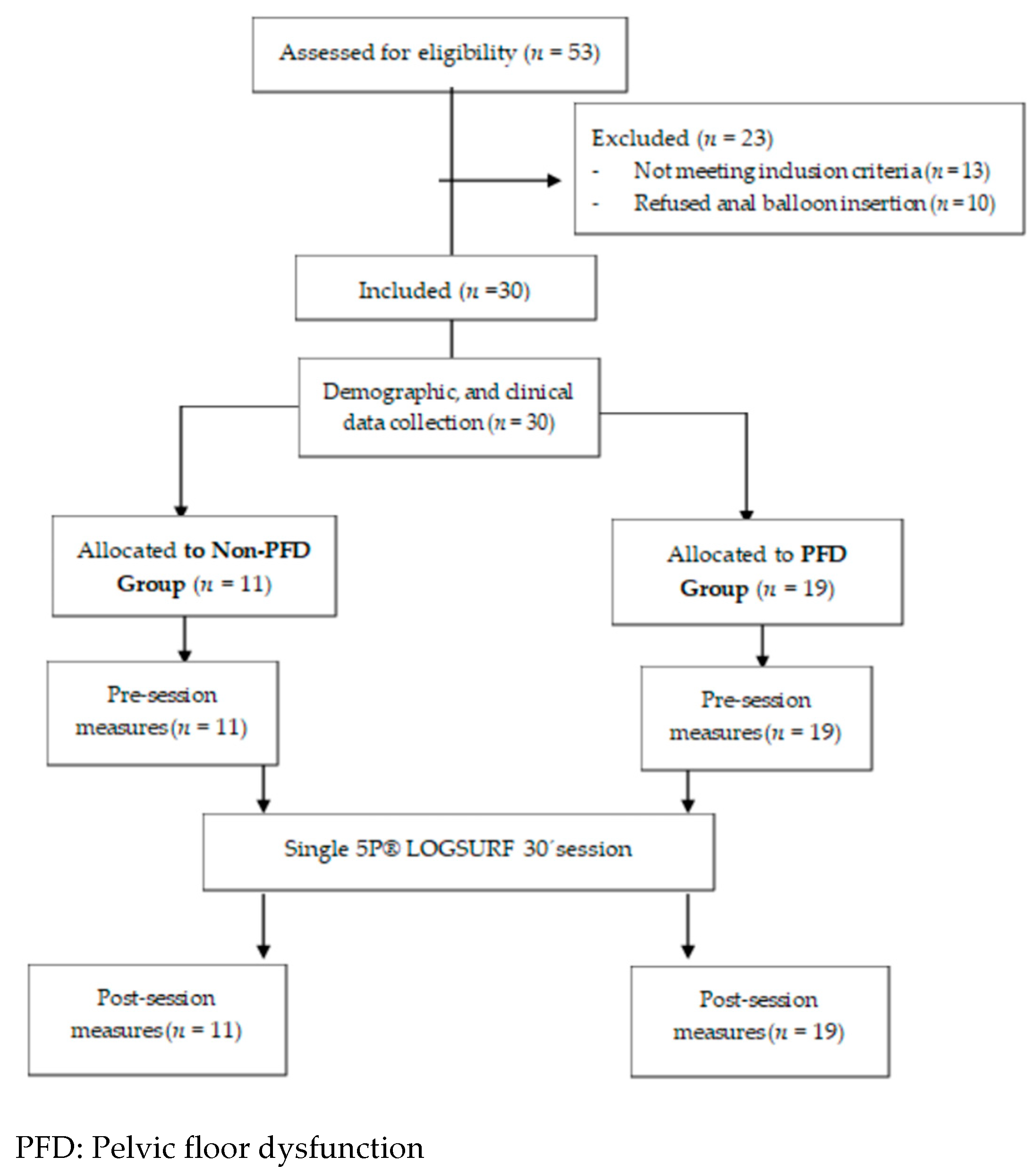
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Study Participants Characteristics
3.2. Effect of Single 5P® LOGSURF Session
3.3. 5P® LOGSURF Session Variability
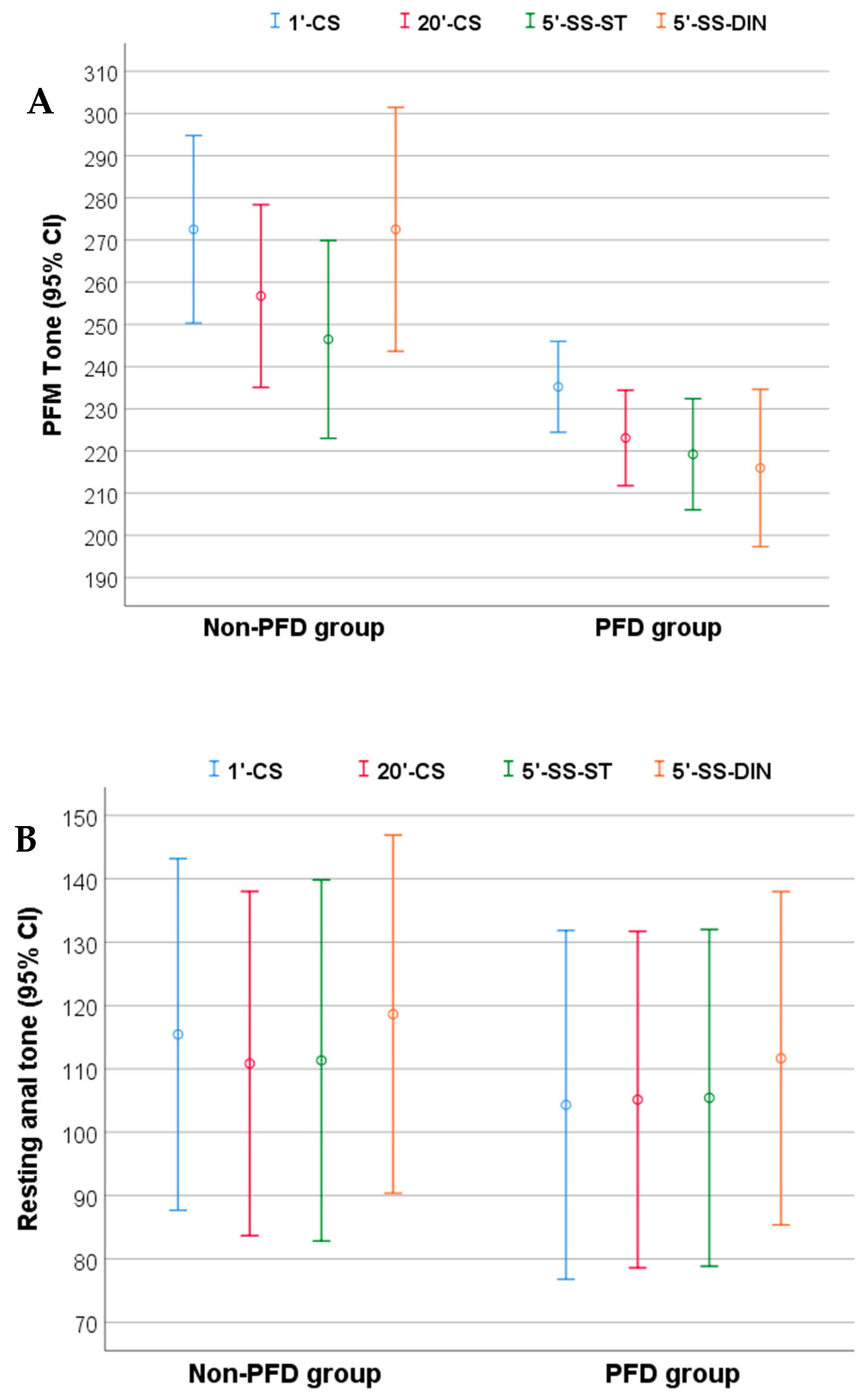
3.3.1. Session Variability on PFM Tone and Resting Anal Tone
3.3.2. Session Variability on Intrarectal Pressure and Deep Abdominal Muscle Electrical Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Riss, P.; Kargl, J. Quality of life and urinary incontinence in women. Maturitas 2011, 68, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Dumoulin, C.; Cacciari, L.P.; Hay-Smith, E.J.C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst. Rev. 2018, 10, Cd005654. [Google Scholar] [CrossRef] [PubMed]
- Alewijnse, D.; Mesters, I.; Metsemakers, J.; van den Borne, B. Predictors of long-term adherence to pelvic floor muscle exercise therapy among women with urinary incontinence. Health Educ. Res. 2003, 18, 511–524. [Google Scholar] [CrossRef] [PubMed]
- Culligan, P.J.; Scherer, J.; Dyer, K.; Priestley, J.L.; Guingon-White, G.; Delvecchio, D.; Vangeli, M. A randomized clinical trial comparing pelvic floor muscle training to a Pilates exercise program for improving pelvic muscle strength. Int. Urogynecol. J. 2010, 21, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Fozzatti, C.; Herrmann, V.; Palma, T.; Riccetto, C.L.; Palma, P.C. Global Postural Re-education: An alternative approach for stress urinary incontinence? Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 152, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Guerrero Fontiveros, A.B. Préparation Anténatale du Périnée: État des Lieux, Propositions des SF ou Attentes Des Femmes; Dumas: Marseille, France, 2019. [Google Scholar]
- Juez, L.; Nunez-Cordoba, J.M.; Couso, N.; Auba, M.; Alcazar, J.L.; Minguez, J.A. Hypopressive technique versus pelvic floor muscle training for postpartum pelvic floor rehabilitation: A prospective cohort study. Neurourol. Urodyn. 2019, 38, 1924–1931. [Google Scholar] [CrossRef] [PubMed]
- Navarro Brazález, B.; Sánchez Sánchez, B.; Prieto Gómez, V.; de La Villa Polo, P.; McLean, L.; Torres Lacomba, M. Pelvic floor and abdominal muscle responses during hypopressive exercises in women with pelvic floor dysfunction. Neurourol. Urodyn. 2020, 39, 793–803. [Google Scholar] [CrossRef]
- Brazález, B.N.; Lacomba, M.T.; Martín, B.A.; Méndez, O.S. Respuesta muscular durante un ejercicio hipopresivo tras tratamiento de fisioterapia pelviperineal: Valoración con ecografía transabdominal. Fisioterapia 2017, 39, 187–194. [Google Scholar] [CrossRef]
- Navarro-Brazalez, B.; Prieto-Gomez, V.; Prieto-Merino, D.; Sanchez-Sanchez, B.; McLean, L.; Torres-Lacomba, M. Effectiveness of Hypopressive Exercises in Women with Pelvic Floor Dysfunction: A Randomised Controlled Trial. J. Clin. Med. 2020, 9, 1149. [Google Scholar] [CrossRef]
- Soriano, L.; Gonzalez-Millan, C.; Alvarez Saez, M.M.; Curbelo, R.; Carmona, L. Effect of an abdominal hypopressive technique programme on pelvic floor muscle tone and urinary incontinence in women: A randomised crossover trial. Physiotherapy 2020, 108, 37–44. [Google Scholar] [CrossRef]
- Steenstrup, B.; Behague, L.; Quehen, M. Rééducation posturale avec le jeu virtuel Wii® en pelvi périnéologie: Pourquoi pas? Kinésithér. Rev. 2015, 15, 45–50. [Google Scholar] [CrossRef]
- Steenstrup, B.; Pavy-Lebrun, M.; Aigueperse, N.; Quemener, N.; Chauveau, S.; Confalonieri, C.; Totte, F. Efficacité d’une rééducation sensori-motrice posturale réflexe sur l’incontinence urinaire et l’urgenturie chez la femme. Kinésithér. Rev. 2019, 19, 12–18. [Google Scholar] [CrossRef]
- Chmielewska, D.; Sobota, G.S.; Stania, M.; Błaszczak, E.; Słomka, K.; Juras, G. A comparison of a step-initiation task in women with and without urinary incontinence. A case-control study. Neurourol. Urodyn. 2018, 37, 2571–2577. [Google Scholar] [CrossRef]
- Madill, S.J.; Harvey, M.A.; McLean, L. Women with SUI demonstrate motor control differences during voluntary pelvic floor muscle contractions. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2009, 20, 447–459. [Google Scholar] [CrossRef]
- Madill, S.J.; Harvey, M.A.; McLean, L. Women with stress urinary incontinence demonstrate motor control differences during coughing. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2010, 20, 804–812. [Google Scholar] [CrossRef]
- Vesentini, G.; El Dib, R.; Righesso, L.A.R.; Piculo, F.; Marini, G.; Ferraz, G.A.R.; Calderon, I.M.P.; Barbosa, A.M.P.; Rudge, M.V.C. Pelvic floor and abdominal muscle cocontraction in women with and without pelvic floor dysfunction: A systematic review and meta-analysis. Clinics (Sao Paulo Braz.) 2019, 74, e1319. [Google Scholar] [CrossRef]
- Chmielewska, D.; Stania, M.; Słomka, K.; Błaszczak, E.; Taradaj, J.; Dolibog, P.; Juras, G. Static postural stability in women with stress urinary incontinence: Effects of vision and bladder filling. Neurourol. Urodyn. 2017, 36, 2019–2027. [Google Scholar] [CrossRef] [PubMed]
- Le Berre, M.; Morin, M.; Corriveau, H.; Hamel, M.; Nadeau, S.; Filiatrault, J.; Dumoulin, C. Characteristics of Lower Limb Muscle Strength, Balance, Mobility, and Function in Older Women with Urge and Mixed Urinary Incontinence: An Observational Pilot Study. Physiother. Can. Physiother. Can. 2019, 71, 250–260. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.D.; Coppieters, M.W.; Hodges, P.W. Is balance different in women with and without stress urinary incontinence? Neurourol. Urodyn. 2008, 27, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Mattox, T.F.; Lucente, V.; McIntyre, P.; Miklos, J.R.; Tomezsko, J. Abnormal spinal curvature and its relationship to pelvic organ prolapse. Am. J. Obstet. Gynecol. 2000, 183, 1381–1384. [Google Scholar] [CrossRef] [PubMed]
- Nygaard, I.E.; Glowacki, C.; Saltzman, C.L. Relationship between foot flexibility and urinary incontinence in nulliparous varsity athletes. Obstet. Gynecol. 1996, 87, 1049–1051. [Google Scholar] [CrossRef]
- Hodges, P.W.; Sapsford, R.; Pengel, L.H. Postural and respiratory functions of the pelvic floor muscles. Neurourol. Urodyn. 2007, 26, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Neumann, P.; Gill, V. Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int. Urogynecol. J. Pelvic Floor Dysfunct. 2002, 13, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Sapsford, R.R.; Hodges, P.W. Contraction of the pelvic floor muscles during abdominal maneuvers. Arch. Phys. Med. Rehabil. 2001, 82, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Ferla, L.; Darski, C.; Paiva, L.L.; Sbruzzi, G.; Vieira, A. Synergism between abdominal and pelvic floor muscles in healthy women: A systematic review of observational studies. Fisioter. Em Mov. 2016, 29, 399–410. [Google Scholar] [CrossRef][Green Version]
- Chmielewska, D.; Stania, M.; Sobota, G.; Kwaśna, K.; Błaszczak, E.; Taradaj, J.; Juras, G. Impact of different body positions on bioelectrical activity of the pelvic floor muscles in nulliparous continent women. Biomed. Res. Int. 2015, 2015, 905897. [Google Scholar] [CrossRef]
- Rocca Rossetti, S. Functional anatomy of pelvic floor. Arch. Ital. Urol. Androl. Organo Uff. Soc. Ital. Ecogr. Urol. E Nefrol. 2016, 88, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Sjödahl, J.; Kvist, J.; Gutke, A.; Öberg, B. The postural response of the pelvic floor muscles during limb movements: A methodological electromyography study in parous women without lumbopelvic pain. Clin. Biomech. 2009, 24, 183–189. [Google Scholar] [CrossRef]
- Capson, A.C.; Nashed, J.; McLean, L. The role of lumbopelvic posture in pelvic floor muscle activation in continent women. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2011, 21, 166–177. [Google Scholar] [CrossRef]
- Luginbuehl, H.; Naeff, R.; Zahnd, A.; Baeyens, J.-P.; Kuhn, A.; Radlinger, L. Pelvic floor muscle electromyography during different running speeds: An exploratory and reliability study. Arch. Gynecol. Obstet. 2016, 293, 117–124. [Google Scholar] [CrossRef]
- Smith, M.D.; Coppieters, M.W.; Hodges, P.W. Postural response of the pelvic floor and abdominal muscles in women with and without incontinence. Neurourol. Urodyn. 2007, 26, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Steenstrup, B.; Giralte, F.; Bakker, E.; Grise, P. Évaluation de l’activité électromyographique des muscles du plancher pelvien pendant des exercices posturaux à l’aide du jeu vidéo virtuel Wii Fit Plus©. Analyses et perspectives en rééducation. Prog. Urol. 2014, 24, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Araguas García, C.; Corbi Solerb, F.; Vergés Salas, C. Importance of plantar sensitivity in the regulation of postural control and movement: Review. Apunts 2017, 52, 149–158. [Google Scholar]
- Viseux, F.; Lemaire, A.; Barbier, F.; Charpentier, P.; Leteneur, S.; Villeneuve, P. How can the stimulation of plantar cutaneous receptors improve postural control? Review and clinical commentary. Neurophysiol. Clin. Clin. Neurophysiol. 2019, 49, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Haylen, B.T.; Maher, C.F.; Barber, M.D.; Camargo, S.; Dandolu, V.; Digesu, A.; Goldman, H.B.; Huser, M.; Milani, A.L.; Moran, P.A.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Organ Prolapse (POP). Neurourol. Urodyn. 2016, 35, 137–168. [Google Scholar] [CrossRef]
- Sánchez Sánchez, B.; Torres Lacomba, M.; Navarro Brazález, B.; Cerezo Téllez, E.; Pacheco Da Costa, S.; Gutiérrez Ortega, C. Responsiveness of the Spanish Pelvic Floor Distress Inventory and Pelvic Floor Impact Questionnaires Short Forms (PFDI-20 and PFIQ-7) in women with pelvic floor disorders. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 190, 20–25. [Google Scholar] [CrossRef]
- Sánchez-Sánchez, B.; Torres-Lacomba, M.; Yuste-Sánchez, M.J.; Navarro-Brazález, B.; Pacheco-da-Costa, S.; Gutiérrez-Ortega, C.; Zapico-Goñi, Á. Cultural adaptation and validation of the Pelvic Floor Distress Inventory Short Form (PFDI-20) and Pelvic Floor Impact Questionnaire Short Form (PFIQ-7) Spanish versions. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 170, 281–285. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2rd ed.; Lawrence Earlbaum Associates: Hillsdale, MI, USA, 1988. [Google Scholar]
- Castro-Pardinas, M.A.; Torres-Lacomba, M.; Navarro-Brazalez, B. Muscle function of the pelvic floor in healthy, puerperal women with pelvic floor dysfunction. Actas Urol. Esp. 2017, 41, 249–257. [Google Scholar] [CrossRef]
- Morgan, D.M.; Kaur, G.; Hsu, Y.; Fenner, D.E.; Guire, K.; Miller, J.; Ashton-Miller, J.A.; Delancey, J.O.L. Does vaginal closure force differ in the supine and standing positions? Am. J. Obstet. Gynecol. 2005, 192, 1722–1728. [Google Scholar] [CrossRef]
- Sultan, A.H.; Monga, A.; Lee, J.; Emmanuel, A.; Norton, C.; Santoro, G.; Hull, T.; Berghmans, B.; Brody, S.; Haylen, B.T. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female anorectal dysfunction. Int. Urogynecol. J. 2017, 28, 5–31. [Google Scholar] [CrossRef]
- Goba, G.K.; Legesse, A.Y.; Zelelow, Y.B.; Gebreselassie, M.A.; Rogers, R.G.; Kenton, K.S.; Mueller, M.G. Reliability and validity of the Tigrigna version of the Pelvic Floor Distress Inventory-Short Form 20 (PFDI-20) and Pelvic Floor Impact Questionnaire-7 (PFIQ-7). Int. Urogynecol. J. 2019, 30, 65–70. [Google Scholar] [CrossRef]
- Henn, E.W.; Richter, B.W.; Marokane, M.M.P. Validation of the PFDI-20 and PFIQ-7 quality of life questionnaires in two African languages. Int. Urogynecol. J. 2017, 28, 1883–1890. [Google Scholar] [CrossRef]
- Yoshida, M.; Murayama, R.; Ota, E.; Nakata, M.; Kozuma, S.; Homma, Y. Reliability and validity of the Japanese version of the pelvic floor distress inventory-short form 20. Int. Urogynecol. J. 2013, 24, 1039–1046. [Google Scholar] [CrossRef] [PubMed]
- Abrams, P.; Cardozo, L.; Wagg, A.; Wein, A. Incontinence, 6th ed.; Internacional Continence Society: Tokyo, Japan, 2017; p. 2648. [Google Scholar]
- Cerruto, M.A.; Vedovi, E.; Mantovani, W.; D’Elia, C.; Artibani, W. Effects of ankle position on pelvic floor muscle electromyographic activity in female stress urinary incontinence: Preliminary results from a pilot study. Arch. Ital. Urol. Androl. Organo Uff. Soc. Ital. Ecogr. Urol. E Nefrol. 2012, 84, 184–188. [Google Scholar]
- Chen, C.H.; Huang, M.H.; Chen, T.W.; Weng, M.C.; Lee, C.L.; Wang, G.J. Relationship between ankle position and pelvic floor muscle activity in female stress urinary incontinence. Urology 2005, 66, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Sapsford, R.R.; Clarke, B.; Hodges, P.W. The effect of abdominal and pelvic floor muscle activation patterns on urethral pressure. World J. Urol. 2013, 31, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Czyrnyj, C.S.; Berube, M.E.; Varette, K.; McLean, L. The impact of a familiarization session on the magnitude and stability of active and passive pelvic floor muscle forces measured through intravaginal dynamometry. Neurourol. Urodyn. 2019, 38, 902–911. [Google Scholar] [CrossRef] [PubMed]
- Gajdosik, R.L. Passive extensibility of skeletal muscle: Review of the literature with clinical implications. Clin. Biomech. (Bristol Avon) 2001, 16, 87–101. [Google Scholar] [CrossRef]
- Taylor, D.C.; Dalton, J.D., Jr.; Seaber, A.V.; Garrett, W.E., Jr. Viscoelastic properties of muscle-tendon units. The biomechanical effects of stretching. Am. J. Sports Med. 1990, 18, 300–309. [Google Scholar] [CrossRef]
- Kraemer, W.J.; Adams, K.; Cafarelli, E.; Dudley, G.A.; Dooly, C.; Feigenbaum, M.S.; Fleck, S.J.; Franklin, B.; Fry, A.C.; Hoffman, J.R.; et al. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med. Sci. Sports Exerc. 2002, 34, 364–380. [Google Scholar] [CrossRef] [PubMed]
- Crommert, M.E.; Ekblom, M.M.; Thorstensson, A. Activation of transversus abdominis varies with postural demand in standing. Gait Posture 2011, 33, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.L.; Lay, B.; Allison, G.T. Transversus abdominis is part of a global not local muscle synergy during arm movement. Hum. Mov. Sci. 2013, 32, 1176–1185. [Google Scholar] [CrossRef] [PubMed]
- Prott, G.; Hansen, R.; Badcock, C.; Kellow, J.; Malcolm, A. What is the optimum methodology for the clinical measurement of resting anal sphincter pressure? Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2005, 17, 595–599. [Google Scholar] [CrossRef] [PubMed]

| Non-PFD Group | PFD Group | p-Value | |
|---|---|---|---|
| (n = 11) | (n = 19) | ||
| Demographic and Anthropometric Data | |||
| Age (years), Χ (SD) | 31.18 (6.11) | 39.11 (6.20) | 0.002 *** |
| Education level | 0.000 ** | ||
| Elementary or professional education | 0 (0) | 4 (21.05) | |
| University Degree | 11 (100) | 15 (78.90) | |
| Body mass index (kg/m2), Χ (SD) | 23.31 (2.95) | 24.68 (4.93) | 0.576 * |
| Parity, Χ (SD) | 1.64 (2.15) | 2.16 (1.21) | 0.168 * |
| Type of delivery | |||
| Caesarean | 1 (9.1) | 3 (15.80) | 1 ** |
| Vaginal | 5 (45.50) | 19 (100) | 0.001 ** |
| Clinical Data | |||
| Urinary incontinence | - | 13 (68.40) | - |
| SUI | - | 9 (47.40) | - |
| UUI | - | 2 (10.50) | - |
| MUI | - | 2 (10.50) | - |
| Anal incontinence | - | 9 (47.40) | - |
| PFDI-20 total, Median (IQR) | 8.3 (20.8–0) | 22.9 (50–16.7) | 0.011 * |
| POPDI, Median (IQR) | 0 (8.3–0) | 8.3 (16.7–0) | 0.063 * |
| CRADI, Median (IQR) | 0 (13.1–0) | 6.25 (15.6–3.1) | 0.011 * |
| UDI, Median (IQR) | 0 (8.3–0) | 4.2 (25–0) | 0.156 * |
| PFIQ-7 total, Median (IQR) | 0 (4.8–0) | 19.1 (33.3–4.8) | 0.001 * |
| POPIQ, Median (IQR) | 0 (0–0) | 0 (14.3–0) | 0.068 * |
| CRAIQ, Median (IQR) | 0 (0–0) | 0 (9.5–0) | 0.081 * |
| UIQ, Median (IQR) | 0 (0–0) | 4.8 (19–0) | 0.014 * |
| Concomitant diseases | |||
| Anxiety | 0 (0.00) | 4 (21.10) | 0.268 ** |
| Other pathologies (scoliosis, auditive diseases, etc.) | 1 (9.10) | 5 (26.40) | 0.372 ** |
| Pads/day, Χ (SD) | - | 0.16 (0.38) | - |
| Constipation | 6 (54.50) | 9 (47.40) | 1 ** |
| Regular physical activity | 10 (90.90) | 10 (52.60) | 0.099 ** |
| Physical activity (minutes/week), Median (IQR) | 120 (60–240) | 120 (90–150) | 0.567 * |
| Postural training experience | |||
| 5P® LOGSURF method | 1 (9.10) | 1 (5.30) | 1 ** |
| Other postural methods | 10 (91) | 18 (95) | 1 ** |
| Outcomes | Group | Pre-5P® Session | Post-5P® Session | Pre-Post 5P® Session Difference | Intragroup Pre- vs. Post-5P® Session, p-Value | Between Groups Pre-Post 5P® Session Difference, p-Value | Between Groups Pre-5P® Session, p-Value |
|---|---|---|---|---|---|---|---|
| PFM Tone (g) | PFD | 238.60 (18.33) | 222.65 (24.89) | −15.95 (23.79) | 0.009 *** | 0.442 **** | 0.052 **** |
| Non-PFD | 266.64 (40.96) | 244.09 (27.58) | −22.55 (19.36) | 0.003 *** | |||
| PFM MVC (g) | PFD | 284.23 (88.50) | 249.45 (77.72) | −34.66 (49.45) | 0.000 * | 0.179 ** | 0.003 ** |
| Non-PFD | 394.54 (90.45) | 337.20 (79.34) | −52.60 (34.28) | 0.005 * | |||
| Resting anal tone (mmHg) | PFD | 110.89 (57.99) | 104.54 (54.57) | −6.35 (15.34) | 0.088 *** | 0.741 **** | 0.848 **** |
| Non-PFD | 114.77(42.73) | 106.59 (42.65) | −8.18 (12.72) | 0.059 *** | |||
| Intrarectal pressure (mmHg) | PFD | 104.31 (34.18) | 101,44 (37,76) | −2.87 (8.81) | 0.372 * | 0.667 ** | 0.863 ** |
| Non-PFD | 111.88 (23.82) | 101.65 (42.69) | −10.24 (22.62) | 0.285 * | |||
| Deep abdominal muscle activity (µV) | PFD | 5.64 (7.62) | 4.29 (2.11) | −1.34 (7.52) | 0.753 * | 0.596 ** | 0.288 ** |
| Non-PFD | 5.55 (3.55) | 6.55 (5.00) | 1 (2.48) | 0.248 * | |||
| Deep abdominal muscle activity MVC (µV) | PFD | 17.24 (14.10) | 20.34 (13.73) | 1.85 (7.70) | 0.000 * | 0.853 ** | 0.143 ** |
| Non-PFD | 26.77 (17.15) | 30.20 (18.34) | 0.56 (10.28) | 0.003 * |
| 1′-CS | 20′-CS | 5′-SS-ST | 5′-SS-DIN | ||
|---|---|---|---|---|---|
| PFM Tone (g). Χ (SD) | PFD | 235.21 | 223.09 | 219.23 | 215.98 |
| (22.35) | (23.48) | (27.34) | (38.69) | ||
| Non-PFD | 272.55 | 256.78 | 246.45 | 272.54 | |
| (33.10) | (32.23) | (34.92) | (43.02) | ||
| Resting anal tone (mmHg). Χ (SD) | PFD | 104.32 | 105.15 | 105.42 | 111.67 |
| (57.12) | (55.09) | (55.14) | (54.58) | ||
| Non-PFD | 115.44 | 110.85 | 111.34 | 118.64 | |
| (41.32) | (40.45) | (42.42) | (42.07) | ||
| Intrarectal pressure (mmHg). Median (IQR) | PFD | 117.90 | 117.20 | 114.60 | 121.20 |
| (134.50–117.90) | (130.10–86.90) | (128.10–80.30) | (135.10–81.40) | ||
| Non-PFD | 122.30 | 122.20 | 125.60 | 128.90 | |
| (125.60–82.30) | (131.10–75.60) | (126.70–67.90) | (130.20–90.00) | ||
| Deep abdominal muscle activity (µV). Median (IQR) | PFD | 4.50 | 4.50 | 4.50 | 8.00 |
| (6.00–3.50) | (6.00–3.50) | (7.00–3.50) | (10.00–6.00) | ||
| Non-PFD | 5.00 | 6.00 | 5.00 | 9.50 | |
| (15.00–4.00) | (12.00–3.00) | (18.00–3.00) | (23.00–6.00) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuentes-Aparicio, L.; Arranz-Martín, B.; Navarro-Brazález, B.; Bailón-Cerezo, J.; Sánchez-Sánchez, B.; Torres-Lacomba, M. Postural Sensorimotor Control on Anorectal Pressures and Pelvic Floor Muscle Tone and Strength: Effects of a Single 5P® LOGSURF Session. A Cross-Sectional Preliminary Study. Int. J. Environ. Res. Public Health 2021, 18, 3708. https://doi.org/10.3390/ijerph18073708
Fuentes-Aparicio L, Arranz-Martín B, Navarro-Brazález B, Bailón-Cerezo J, Sánchez-Sánchez B, Torres-Lacomba M. Postural Sensorimotor Control on Anorectal Pressures and Pelvic Floor Muscle Tone and Strength: Effects of a Single 5P® LOGSURF Session. A Cross-Sectional Preliminary Study. International Journal of Environmental Research and Public Health. 2021; 18(7):3708. https://doi.org/10.3390/ijerph18073708
Chicago/Turabian StyleFuentes-Aparicio, Laura, Beatriz Arranz-Martín, Beatriz Navarro-Brazález, Javier Bailón-Cerezo, Beatriz Sánchez-Sánchez, and María Torres-Lacomba. 2021. "Postural Sensorimotor Control on Anorectal Pressures and Pelvic Floor Muscle Tone and Strength: Effects of a Single 5P® LOGSURF Session. A Cross-Sectional Preliminary Study" International Journal of Environmental Research and Public Health 18, no. 7: 3708. https://doi.org/10.3390/ijerph18073708
APA StyleFuentes-Aparicio, L., Arranz-Martín, B., Navarro-Brazález, B., Bailón-Cerezo, J., Sánchez-Sánchez, B., & Torres-Lacomba, M. (2021). Postural Sensorimotor Control on Anorectal Pressures and Pelvic Floor Muscle Tone and Strength: Effects of a Single 5P® LOGSURF Session. A Cross-Sectional Preliminary Study. International Journal of Environmental Research and Public Health, 18(7), 3708. https://doi.org/10.3390/ijerph18073708








