Analysis of the Associations between Arthritis and Fall Histories in Korean Adults
Abstract
1. Introduction
2. Materials and Methods
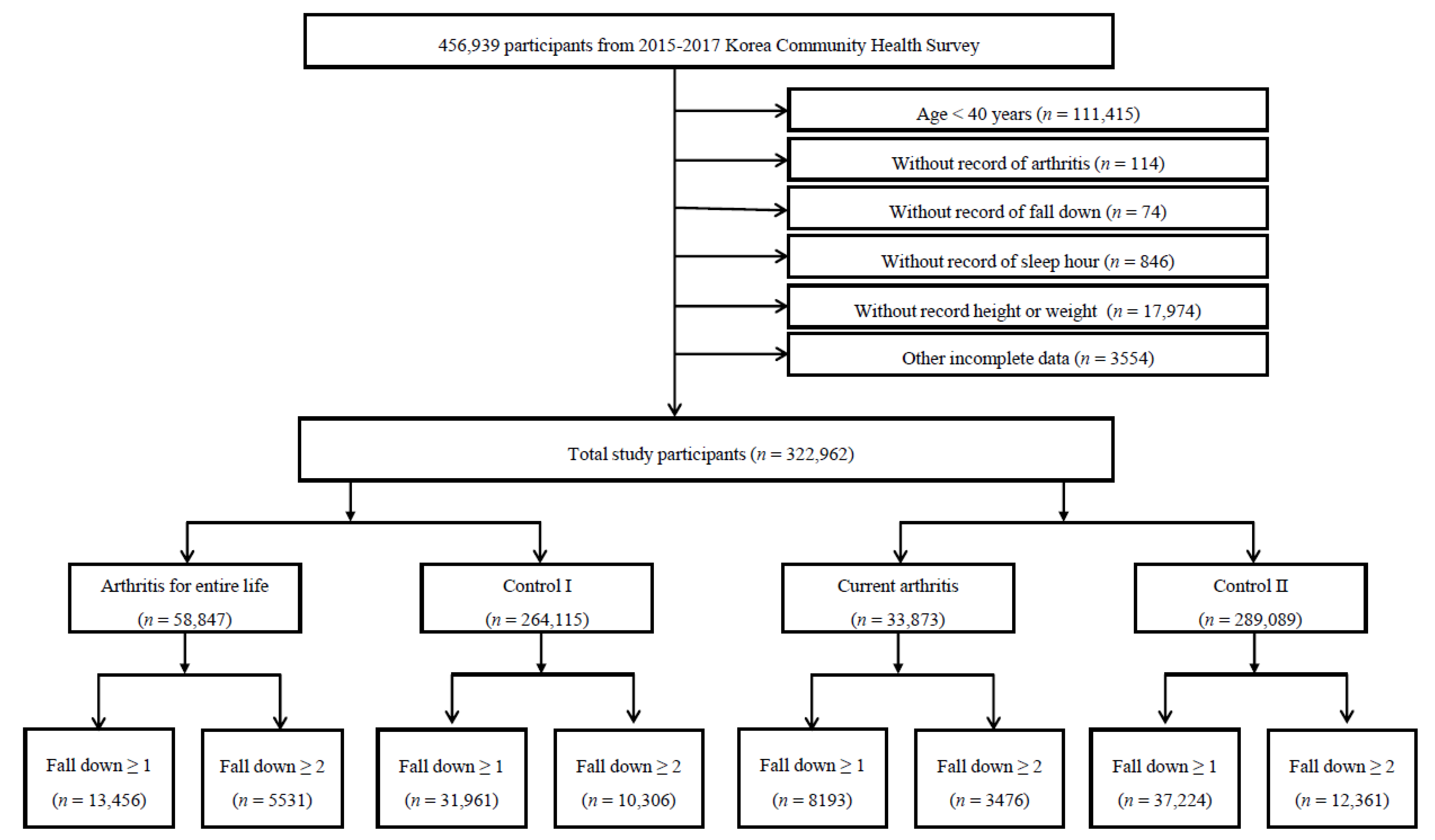
2.1. Study Population and Data Collection
2.2. Fall History Questionnaire
2.3. Arthritis History Questionnaire
2.4. Other Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Soh, S.E.; Barker, A.L.; Morello, R.T.; Ackerman, I.N. Applying the International Classification of Functioning, Disability and Health framework to determine the predictors of falls and fractures in people with osteoarthritis or at high risk of developing osteoarthritis: Data from the Osteoarthritis Initiative. BMC Musculoskelet. Disord. 2020, 21, 138. [Google Scholar] [CrossRef] [PubMed]
- Burns, E.; Kakara, R. Deaths from Falls among Persons Aged ≥65 Years—United States, 2007–2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Manlapaz, D.G.; Sole, G.; Jayakaran, P.; Chapple, C.M. Risk Factors for Falls in Adults with Knee Osteoarthritis: A Systematic Review. PM&R 2019, 11, 745–757. [Google Scholar] [CrossRef]
- Brenton-Rule, A.; Dalbeth, N.; Bassett, S.; Menz, H.B.; Rome, K. The incidence and risk factors for falls in adults with rheumatoid arthritis: A systematic review. Semin. Arthritis Rheum. 2015, 44, 389–398. [Google Scholar] [CrossRef]
- Picorelli, A.M.A.; Hatton, A.L.; Gane, E.M.; Smith, M.D. Balance performance in older adults with hip osteoarthritis: A systematic review. Gait Posture 2018, 65, 89–99. [Google Scholar] [CrossRef]
- Fazal, S.A.; Khan, M.; Nishi, S.E.; Alam, F.; Zarin, N.; Bari, M.T.; Ashraf, G.M. A Clinical Update and Global Economic Burden of Rheumatoid Arthritis. Endocr. Metab. Immune Disord. Drug Targets 2018, 18, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, K.; Matsumoto, T.; Kasai, T.; Chang, S.H.; Hirose, J.; Tanaka, S. Association between fall history and performance-based physical function and postural sway in patients with rheumatoid arthritis. Mod. Rheumatol. 2020, 1–7. [Google Scholar] [CrossRef]
- Hayashibara, M.; Hagino, H.; Katagiri, H.; Okano, T.; Okada, J.; Teshima, R. Incidence and risk factors of falling in ambulatory patients with rheumatoid arthritis: A prospective 1-year study. Osteoporos. Int. 2010, 21, 1825–1833. [Google Scholar] [CrossRef] [PubMed]
- Barbour, K.E.; Stevens, J.A.; Helmick, C.G.; Luo, Y.H.; Murphy, L.B.; Hootman, J.M.; Theis, K.; Anderson, L.A.; Baker, N.A.; Sugerman, D.E. Falls and fall injuries among adults with arthritis–United States, 2012. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 379–383. [Google Scholar]
- Doré, A.L.; Golightly, Y.M.; Mercer, V.S.; Shi, X.A.; Renner, J.B.; Jordan, J.M.; Nelson, A.E. Lower-extremity osteoarthritis and the risk of falls in a community-based longitudinal study of adults with and without osteoarthritis. Arthritis Care Res. 2015, 67, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Di Laura Frattura, G.; Filardo, G.; Giunchi, D.; Fusco, A.; Zaffagnini, S.; Candrian, C. Risk of falls in patients with knee osteoarthritis undergoing total knee arthroplasty: A systematic review and best evidence synthesis. J. Orthop. 2018, 15, 903–908. [Google Scholar] [CrossRef]
- Ng, C.T.; Tan, M.P. Osteoarthritis and falls in the older person. Age Ageing 2013, 42, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Kaz, H.K.; Johnson, D.; Kerry, S.; Chinappen, U.; Tweed, K.; Patel, S. Fall-related risk factors and osteoporosis in women with rheumatoid arthritis. Rheumatology 2004, 43, 1267–1271. [Google Scholar] [CrossRef][Green Version]
- Lee, W.K.; Kong, K.A.; Park, H. Effect of preexisting musculoskeletal diseases on the 1-year incidence of fall-related injuries. J. Prev. Med. Public Health 2012, 45, 283–290. [Google Scholar] [CrossRef]
- Mamoto, K.; Inui, K.; Okano, T.; Sugioka, Y.; Tada, M.; Koike, T.; Nakamura, H. Incidence rate of falls and its risk factors in patients with rheumatoid arthritis compared to controls: Four years of the TOMORROW study. Mod. Rheumatol. 2017, 27, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Akyol, Y.; Ulus, Y.; Tander, B.; Tomak, L.; Zahiroğlu, Y.; Bilgici, A.; Kuru, Ö. Falls, fear of falling, and associated factors in ambulatory patients with rheumatoid arthritis: A comparative study with healthy controls. Turk. J. Phys. Med. Rehabil. 2018, 64, 213–221. [Google Scholar] [CrossRef]
- Clynes, M.A.; Jameson, K.; Prieto-Alhambra, D.; Harvey, N.C.; Cooper, C.; Dennison, E.M. Impact of Rheumatoid Arthritis and Its Management on Falls, Fracture and Bone Mineral Density in UK Biobank. Front. Endocrinol. 2019, 10, 817. [Google Scholar] [CrossRef]
- Kim, M.; Chang, M.; Nam, E.; Kim, S.G.; Cho, S.I.; Ryu, D.H.; Kam, S.; Choi, B.Y.; Kim, M.J. Fall characteristics among elderly populations in urban and rural areas in Korea. Medicine 2020, 99, 46. [Google Scholar] [CrossRef] [PubMed]
- Gaino, J.Z.; Bértolo, M.B.; Nunes, C.S.; de Morais Barbosa, C.; Sachetto, Z.; Davitt, M.; de Paiva Magalhães, E. Disease-related outcomes influence prevalence of falls in people with rheumatoid arthritis. Ann. Phys. Rehabil. Med. 2019, 62, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Ai, W. Participatory Action Research into Low Literates’ Medical Needs in Rural Communities. Sci. Med. J. 2019, 1, 176–188. [Google Scholar] [CrossRef]
- Rokach, A. Loneliness in Pre and Post-operative Cancer Patients: A Mini Review. Emerg. Sci. J. 2019, 3, 53. [Google Scholar] [CrossRef]
- Quach, L.T.; Burr, J.A. Arthritis, Depression, and Falls Among Community-Dwelling Older Adults: Evidence From the Health and Retirement Study. J. Appl. Gerontol. 2018, 37, 1133–1149. [Google Scholar] [CrossRef]
- Pincus, T.; Castrejon, I.; Yazici, Y.; Gibson, K.A.; Bergman, M.J.; Block, J.A. Osteoarthritis is as severe as rheumatoid arthritis: Evidence over 40 years according to the same measure in each disease. Clin. Exp. Rheumatol. 2019, 37 (Suppl. 120), 7–17. [Google Scholar] [PubMed]
- Kim, S.Y.; Bang, W.; Kim, M.S.; Park, B.; Kim, J.H.; Choi, H.G. Nocturia Is Associated with Slipping and Falling. PLoS ONE 2017, 12, e0169690. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, S.-G.; Sim, S.; Park, B.; Choi, H.G. Excessive Sleep and Lack of Sleep Are Associated With Slips and Falls in the Adult Korean Population: A Population-Based Cross-Sectional Study. Medicine 2016, 95, e2397. [Google Scholar] [CrossRef] [PubMed]
- Byun, M.; Kim, J.; Kim, M. Physical and Psychological Factors Affecting Falls in Older Patients with Arthritis. Int. J. Environ. Res. Public Health 2020, 17, 1098. [Google Scholar] [CrossRef] [PubMed]
- Smith, T.O.; Higson, E.; Pearson, M.; Mansfield, M. Is there an increased risk of falls and fractures in people with early diagnosed hip and knee osteoarthritis? Data from the Osteoarthritis Initiative. Int. J. Rheum. Dis. 2018, 21, 1193–1201. [Google Scholar] [CrossRef]
- Stanmore, E.K.; Oldham, J.; Skelton, D.A.; O’Neill, T.; Pilling, M.; Campbell, A.J.; Todd, C. Risk factors for falls in adults with rheumatoid arthritis: A prospective study. Arthritis Care Res. 2013, 65, 1251–1258. [Google Scholar] [CrossRef]
- Armstrong, C.; Swarbrick, C.M.; Pye, S.R.; O’Neill, T.W. Occurrence and risk factors for falls in rheumatoid arthritis. Ann. Rheum. Dis. 2005, 64, 1602–1604. [Google Scholar] [CrossRef]
- Van Schoor, N.M.; Dennison, E.; Castell, M.V.; Cooper, C.; Edwards, M.H.; Maggi, S.; Pedersen, N.L.; van der Pas, S.; Pijnhart, J.J.M.; Lips, P.; et al. Clinical osteoarthritis of the hip and knee and fall risk: The role of low physical functioning and pain medication. Semin. Arthritis Rheum. 2020, 50, 380–386. [Google Scholar] [CrossRef]
- Furuya, T.; Yamagiwa, K.; Ikai, T.; Inoue, E.; Taniguchi, A.; Momohara, S.; Yamanaka, H. Associated factors for falls and fear of falling in Japanese patients with rheumatoid arthritis. Clin. Rheumatol. 2009, 28, 1325–1330. [Google Scholar] [CrossRef] [PubMed]
- Mat, S.; Tan, P.J.; Ng, C.T.; Fadzli, F.; Rozalli, F.I.; Khoo, E.M.; Hill, K.D.; Tan, P.M. Mild Joint Symptoms Are Associated with Lower Risk of Falls than Asymptomatic Individuals with Radiological Evidence of Osteoarthritis. PLoS ONE 2015, 10, e0141368. [Google Scholar] [CrossRef] [PubMed]
- Tsonga, T.; Michalopoulou, M.; Malliou, P.; Godolias, G.; Kapetanakis, S.; Gkasdaris, G.; Soucacos, P. Analyzing the History of Falls in Patients with Severe Knee Osteoarthritis. Clin. Orthop. Surg. 2015, 7, 449–456. [Google Scholar] [CrossRef]
- Ikutomo, H.; Nagai, K.; Tagomori, K.; Miura, N.; Nakagawa, N.; Masuhara, K. Incidence and Risk Factors for Falls in Women With End-Stage Hip Osteoarthritis. J. Geriatr. Phys. Ther. 2019, 42, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Si, H.B.; Zeng, Y.; Zhong, J.; Zhou, Z.K.; Lu, Y.R.; Cheng, J.Q.; Ning, N.; Shen, B. The effect of primary total knee arthroplasty on the incidence of falls and balance-related functions in patients with osteoarthritis. Sci. Rep. 2017, 7, 16583. [Google Scholar] [CrossRef] [PubMed]
- Mat, S.; Ng, C.T.; Fadzil, F.; Rozalli, F.I.; Tan, M.P. The mediating role of psychological symptoms on falls risk among older adults with osteoarthritis. Clin. Interv. Aging 2017, 12, 2025–2032. [Google Scholar] [CrossRef]
- Fessel, K.D.; Nevitt, M.C. Correlates of fear of falling and activity limitation among persons with rheumatoid arthritis. Arthritis Care Res. 1997, 10, 222–228. [Google Scholar] [CrossRef]
- Jamison, M.; Neuberger, G.B.; Miller, P.A. Correlates of falls and fear of falling among adults with rheumatoid arthritis. Arthritis Rheum. 2003, 49, 673–680. [Google Scholar] [CrossRef]
- Oswald, A.E.; Pye, S.R.; O’Neill, T.W.; Bunn, D.; Gaffney, K.; Marshall, T.; Silman, A.J.; Symmons, D.P.M. Prevalence and associated factors for falls in women with established inflammatory polyarthritis. J. Rheumatol. 2006, 33, 690–694. [Google Scholar]
- Smulders, E.; Schreven, C.; Weerdesteyn, V.; van den Hoogen, F.H.J.; Laan, R.; Van Lankveld, W. Fall incidence and fall risk factors in people with rheumatoid arthritis. Ann. Rheum. Dis. 2009, 68, 1795–1796. [Google Scholar] [CrossRef]
- Böhler, C.; Radner, H.; Ernst, M.; Binder, A.; Stamm, T.; Aletaha, D.; Smolen, J.S.; Koller, M. Rheumatoid arthritis and falls: The influence of disease activity. Rheumatology 2012, 51, 2051–2057. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, M.d.A.; Carli, F.V.B.O.; de Assis, M.R. Characterization of falls in adults with established rheumatoid arthritis and associated factors. Adv. Rheumatol. 2018, 58, 16. [Google Scholar] [CrossRef] [PubMed]
- Bugdayci, D.; Paker, N.; Rezvani, A.; Kesiktas, N.; Yilmaz, O.; Sahin, M.; Ince, N. Frequency and predictors for falls in the ambulatory patients with rheumatoid arthritis: A longitudinal prospective study. Rheumatol. Int. 2013, 33, 2523–2527. [Google Scholar] [CrossRef]
- Yamagiwa, K.; Iijima, S.; Furuya, T.; Ikai, T.; Inoue, E.; Taniguchi, A.; Momohara, S.; Yamanaka, H. Incidence of falls and fear of falling in Japanese patients with rheumatoid arthritis. Mod. Rheumatol. 2011, 21, 51–56. [Google Scholar] [CrossRef]
- Iijima, H.; Shimoura, K.; Aoyama, T.; Takahashi, M. Low Back Pain as a Risk Factor for Recurrent Falls in People with Knee Osteoarthritis. Arthritis Care Res. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, M.d.A.; Roma, I.; Assis, M.R. Falls and their association with physical tests, functional capacity, clinical and demographic factors in patients with rheumatoid arthritis. Rev. Bras. Reumatol. Engl. Ed. 2017, 57, 217–223. [Google Scholar] [CrossRef]
- Kitayuguchi, J.; Kamada, M.; Okada, S.; Kamioka, H.; Mutoh, Y. Association between musculoskeletal pain and trips or falls in rural Japanese community-dwelling older adults: A cross-sectional study. Geriatr. Gerontol. Int. 2015, 15, 54–64. [Google Scholar] [CrossRef]
- Scott, D.; Blizzard, L.; Fell, J.; Jones, G. Prospective study of self-reported pain, radiographic osteoarthritis, sarcopenia progression, and falls risk in community-dwelling older adults. Arthritis Care Res. 2012, 64, 30–37. [Google Scholar] [CrossRef]
- Park, D.; Jo, H.; Yoon, C.H.; Lee, E.S.; Oh, M.K.; Lee, C.H. Fall Risk Assessment of Rural Elderly Population in Korea. Ann. Rehabil. Med. 2019, 43, 269–278. [Google Scholar] [CrossRef]
- Montemurro, N.; Perrini, P.; Mangini, V.; Galli, M.; Papini, A. The Y-shaped trabecular bone structure in the odontoid process of the axis: A CT scan study in 54 healthy subjects and biomechanical considerations. J. Neurosurg. Spine 2019, 1–8. [Google Scholar] [CrossRef]
- Povoroznyuk, V.V.; Zaverukha, N.V.; Musiienko, A.S. Bone mineral density and trabecular bone score in postmenopausal women with knee osteoarthritis and obesity. Wiad. Lek. 2020, 73, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Nevitt, M.C.; Tolstykh, I.; Shakoor, N.; Nguyen, U.S.; Segal, N.A.; Lewis, C.; Felson, D.T.; The Multicenter Osteoarthritis Study Investigators. Symptoms of Knee Instability as Risk Factors for Recurrent Falls. Arthritis Care Res. 2016, 68, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
- Kramer, H.R.; Fontaine, K.R.; Bathon, J.M.; Giles, J.T. Muscle density in rheumatoid arthritis: Associations with disease features and functional outcomes. Arthritis Rheum. 2012, 64, 2438–2450. [Google Scholar] [CrossRef] [PubMed]
- Stanmore, E.K.; Oldham, J.; Skelton, D.A.; O’Neill, T.; Pilling, M.; Campbell, A.J.; Todd, C. Fall incidence and outcomes of falls in a prospective study of adults with rheumatoid arthritis. Arthritis Care Res. 2013, 65, 737–744. [Google Scholar] [CrossRef] [PubMed]
- De Zwart, A.H.; van der Esch, M.; Pijnappels, M.A.; Hoozemans, M.J.; van der Leeden, M.; Roorda, L.D.; Dekker, J.; Lems, W.F.; van Dieen, J.H. Falls Associated with Muscle Strength in Patients with Knee Osteoarthritis and Self-reported Knee Instability. J. Rheumatol. 2015, 42, 1218–1223. [Google Scholar] [CrossRef]
- Lo-Ciganic, W.H.; Floden, L.; Lee, J.K.; Ashbeck, E.L.; Zhou, L.; Chinthammit, C.; Purdy, A.W.; Kwoh, C.K. Analgesic use and risk of recurrent falls in participants with or at risk of knee osteoarthritis: Data from the Osteoarthritis Initiative. Osteoarthr. Cartil. 2017, 25, 1390–1398. [Google Scholar] [CrossRef] [PubMed]
- Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [CrossRef]
- Hopewell, S.; Adedire, O.; Copsey, B.J.; Boniface, G.J.; Sherrington, C.; Clemson, L.; Close, J.C.T.; Lamb, S.E. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2018, 7, Cd012221. [Google Scholar] [CrossRef]
- Papalia, G.F.; Papalia, R.; Diaz Balzani, L.A.; Torre, G.; Zampogna, B.; Vasta, S.; Fossati, C.; Alifano, A.M.; Denaro, V. The Effects of Physical Exercise on Balance and Prevention of Falls in Older People: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2595. [Google Scholar] [CrossRef]
- Park, J.H.; Hong, J.Y.; Han, K.; Suh, S.W.; Park, S.Y.; Yang, J.H.; Han, S.W. Prevalence of symptomatic hip, knee, and spine osteoarthritis nationwide health survey analysis of an elderly Korean population. Medicine 2017, 96, e6372. [Google Scholar] [CrossRef]
- Turkiewicz, A.; Gerhardsson de Verdier, M.; Engström, G.; Nilsson, P.M.; Mellström, C.; Lohmander, L.S.; Englund, M. Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology 2015, 54, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Barbour, K.E.; Sagawa, N.; Boudreau, R.M.; Winger, M.E.; Cauley, J.A.; Nevitt, M.C.; Fujii, T.; Patel, K.V.; Strotmeyer, E.S. Knee Osteoarthritis and the Risk of Medically Treated Injurious Falls Among Older Adults: A Community-Based US Cohort Study. Arthritis Care Res. 2019, 71, 865–874. [Google Scholar] [CrossRef] [PubMed]
- Suh, Y.S.; Cheon, Y.-H.; Kim, H.-O.; Kim, R.-B.; Park, K.S.; Kim, S.-H.; Lee, S.-G.; Park, E.-K.; Hur, J.; Lee, S.I. Medication nonadherence in Korean patients with rheumatoid arthritis: The importance of belief about medication and illness perception. Korean J. Intern. Med. 2018, 33, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Sung, Y.-K.; Yoshida, K.; Prince, F.H.M.; Frits, M.L.; Cho, S.-K.; Choe, J.-Y.; Lee, H.-S.; Lee, J.; Lee, S.-S.; Yoo, D.-H. Prevalence and predictors for sustained remission in rheumatoid arthritis. PLoS ONE 2019, 14, e0214981. [Google Scholar] [CrossRef]
| Characteristics | Arthritis for Entire Life | Current Arthritis | |||||
|---|---|---|---|---|---|---|---|
| Patient | Comparison I | p-Value | Patient | Comparison II | p-Value | ||
| Falling ≥ 1 (n, %) | 13,456 (22.9) | 31,961 (12.1) | <0.001 † | 8193 (24.2) | 37,224 (12.9) | <0.001 † | |
| Falling ≥ 2 (n, %) | 5531 (9.4) | 10,306 (3.9) | <0.001 † | 3476 (10.3) | 12,361 (4.3) | <0.001 † | |
| Number (n, %) | 58,847 (18.2) | 264,115 (81.8) | 33,873 (10.5) | 289,089 (89.5) | |||
| Vigorous exercise/day (d, mean, SD) | 0.59 (1.6) | 0.83 (1.7) | <0.001 * | 0.55 (1.5) | 0.81 (1.7) | <0.001 * | |
| Moderate exercise/day (d, mean, SD) | 1.29 (2.2) | 1.39 (2.2) | <0.001 * | 1.25 (2.2) | 1.39 (2.2) | <0.001 * | |
| Age (n, %) | <0.001 † | <0.001 † | |||||
| 40–49 years | 2668 (4.5) | 76,851 (29.1) | 1063 (3.1) | 78,456 (27.1) | |||
| 50–59 years | 9784 (16.6) | 78,555 (29.7) | 4753 (14.0) | 83,586 (28.9) | |||
| 60–69 years | 18,289 (31.1) | 57,612 (21.8) | 10,166 (30.0) | 65,735 (22.7) | |||
| ≥70 years | 28,106 (47.8) | 51,097 (19.4) | 17,891 (52.8) | 61,312 (21.2) | |||
| Sex (n, %) | <0.001 † | <0.001 † | |||||
| Males | 13,022 (22.1) | 135,395 (51.3) | 6992 (20.6) | 141,425 (48.9) | |||
| Females | 45,825 (77.9) | 128,720 (48.7) | 26,881 (79.4) | 147,664 (51.1) | |||
| Income (n, %) | <0.001 † | <0.001 † | |||||
| Lowest | 26,043 (44.3) | 51,825 (19.6) | 16,503 (48.7) | 61,365 (21.2) | |||
| Low-middle | 20,684 (35.2) | 94,732 (35.9) | 11,416 (33.7) | 104,000 (36.0) | |||
| Upper-middle | 7793 (13.2) | 71,157 (26.9) | 3913 (11.6) | 75,037 (26.0) | |||
| Highest | 4327 (7.4) | 46,401 (17.6) | 2041 (6.0) | 48,687 (16.8) | |||
| Education level (n, %) | <0.001 † | <0.001 † | |||||
| Low | 44,713 (76.0) | 98,668 (37.4) | 27,264 (80.5) | 116,117 (40.2) | |||
| Middle | 10,005 (17.0) | 93,633 (35.5) | 4847 (14.3) | 98,791 (34.2) | |||
| High | 4129 (7.0) | 71,814 (27.2) | 1762 (5.2) | 74,181 (25.7) | |||
| Region of residence (n, %) | |||||||
| Urban | 21,836 (37.1) | 123,772 (46.9) | 11,589 (34.2) | 134,019 (46.4) | |||
| Rural | 37,011 (62.9) | 140,343 (53.1) | 22,284 (65.8) | 155,070 (53.6) | |||
| Smoking (n, %) | <0.001 † | <0.001 † | |||||
| None | 46,296 (78.7) | 150,853 (57.1) | 26,976 (79.6) | 170,173 (58.9) | |||
| Past smoker | 7772 (13.2) | 57,791 (21.9) | 4376 (12.9) | 61,187 (21.2) | |||
| Current smoker | 4779 (8.1) | 55,471 (21.0) | 2521 (7.4) | 57,729 (20.0) | |||
| Alcohol consumption (n, %) | <0.001 † | <.001 † | |||||
| None | 31,413 (53.4) | 85,486 (32.4) | 19,218 (56.7) | 97,681 (33.8) | |||
| ≤1 time a month | 14,233 (24.2) | 62,292 (23.6) | 7912 (23.4) | 68,613 (23.7) | |||
| 2–4 times a month | 6101 (10.4) | 50,175 (19.0) | 3141 (9.3) | 53,135 (18.4) | |||
| ≥2 times a week | 7100 (12.1) | 66,162 (25.1) | 3602 (10.6) | 69,660 (24.1) | |||
| Obesity (n, %) | <0.001 † | <.001 † | |||||
| Underweight | 2756 (4.7) | 9880 (3.7) | 1808 (5.3) | 10,828 (3.8) | |||
| Normal weight | 22,020 (37.4) | 112,818 (42.7) | 12,845 (37.9) | 121,993 (42.2) | |||
| Overweight | 15,307 (26.0) | 72,137 (27.3) | 8648 (25.5) | 78,796 (27.3) | |||
| Obese I | 16,617 (28.2) | 63,673 (24.1) | 9366 (27.7) | 70,924 (24.5) | |||
| Obese II | 2147 (3.7) | 5607 (2.1) | 1206 (3.6) | 6548 (2.3) | |||
| Subjective health status (n, %) | <0.001 † | <0.001 † | |||||
| Good | 7679 (13.1) | 95,345 (36.1) | 3457 (10.2) | 99,567 (34.4) | |||
| Normal | 21,374 (36.3) | 118,572 (44.9) | 10,847 (32.0) | 129,099 (44.7) | |||
| Bad | 29,794 (50.6) | 50,198 (19.0) | 19,569 (57.8) | 60,423 (20.9) | |||
| Stress (n, %) | <0.001 † | <0.001 † | |||||
| No | 15,992 (27.2) | 65,276 (24.7) | 9222 (27.2) | 72,046 (24.9) | |||
| Some | 27,383 (46.5) | 142,227 (53.9) | 15,479 (45.7) | 154,131 (53.3) | |||
| Moderate | 13,239 (22.5) | 49,632 (18.8) | 7794 (23.0) | 55,077 (19.1) | |||
| Severe | 2233 (3.8) | 6980 (2.6) | 1378 (4.1) | 7835 (2.7) | |||
| Sleep (hour, n, %) | <0.001 † | <0.001 † | |||||
| ≤5 | 16,400 (27.9) | 46,570 (17.6) | 9528 (28.1) | 53,442 (18.5) | |||
| 6 | 15,428 (26.2) | 80,671 (30.5) | 8633 (25.5) | 87,466 (30.3) | |||
| 7 | 14,766 (25.1) | 84,867 (32.1) | 8399 (24.8) | 91,234 (31.6) | |||
| 8 | 9849 (16.7) | 44,046 (16.7) | 5796 (17.1) | 48,099 (16.6) | |||
| ≥9 | 2404 (4.1) | 7961 (3.0) | 1517 (4.5) | 8848 (3.1) | |||
| Characteristics | Number | pORs of Falling (≥1 time) | pORs of Falling (≥2 times) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Crude | p-Value | Adjusted † | p-Value | Crude | p-Value | Adjusted † | p-Value | ||
| Total participants | |||||||||
| Arthritis for entire life | 58,847 | 2.15 (2.11–2.20) | <0.001 * | 1.42 (1.38–1.46) | <0.001 * | 2.56 (2.47–2.64) | <0.001 * | 1.69 (1.62–1.76) | <0.001 * |
| Comparison I | 264,115 | 1 | 1 | 1 | 1 | ||||
| Aged 40–49 years, men | |||||||||
| Arthritis for entire life | 823 | 2.09 (1.75–2.50) | <0.001 * | 1.69 (1.41–2.03) | <0.001 * | 2.60 (2.06–3.29) | <0.001 * | 1.93 (1.51–2.46) | <0.001 * |
| Comparison I | 36,815 | 1 | 1 | 1 | 1 | ||||
| Aged 50–59 years, men | |||||||||
| Arthritis for entire life | 2018 | 2.07 (1.84–2.34) | <0.001 * | 1.62 (1.43–1.83) | <0.001 * | 2.78 (2.36–3.28) | <0.001 * | 1.96 (1.65–2.33) | <0.001 * |
| Comparison I | 38,724 | 1 | 1 | 1 | 1 | ||||
| Aged 60–69 years, men | |||||||||
| Arthritis for entire life | 3900 | 1.84 (1.68–2.02) | <0.001 * | 1.52 (1.39–1.67) | <0.001 * | 2.44 (2.13–2.80) | <0.001 * | 1.81 (1.57–2.09) | <0.001 * |
| Comparison I | 31,259 | 1 | 1 | 1 | 1 | ||||
| Aged ≥ 70 years, men | |||||||||
| Arthritis for entire life | 6281 | 1.69 (1.58–1.81) | <0.001 * | 1.46 (1.36–1.57) | <0.001 * | 2.07 (1.87–2.29) | <0.001 * | 1.65 (1.49–1.83) | <0.001 * |
| Comparison I | 28,597 | 1 | 1 | 1 | 1 | ||||
| Aged 40–49 years, women | |||||||||
| Arthritis for entire life | 1845 | 2.23 (1.99–2.51) | <0.001 * | 1.72 (1.53–1.94) | <0.001 * | 2.96 (2.52–3.48) | <0.001 * | 1.99 (1.68–2.36) | <0.001 * |
| Comparison I | 40,036 | 1 | 1 | 1 | 1 | ||||
| Aged 50–59 years, women | |||||||||
| Arthritis for entire life | 7766 | 1.81 (1.70–1.93) | <0.001 * | 1.46 (1.37–1.56) | <0.001 * | 2.42 (2.19–2.68) | <0.001 * | 1.71 (1.54–1.90) | <0.001 * |
| Comparison I | 39,831 | 1 | 1 | 1 | 1 | ||||
| Aged 60–69 years, women | |||||||||
| Arthritis for entire life | 14,389 | 1.56 (1.48–1.64) | <0.001 * | 1.32 (1.25–1.40) | <0.001 * | 2.18 (2.00–2.38) | <0.001 * | 1.65 (1.50–1.81) | <0.001 * |
| Comparison I | 26,353 | 1 | 1 | 1 | 1 | ||||
| Aged ≥ 70 years, women | |||||||||
| Arthritis for entire life | 21,825 | 1.54 (1.48–1.61) | <0.001 * | 1.37 (1.31–1.44) | <0.001 * | 1.92 (1.80–2.06) | <0.001 * | 1.61 (1.50–1.73) | <0.001 * |
| Comparison I | 22,500 | 1 | 1 | 1 | 1 | ||||
| Characteristics | Number | pORs of Falling (≥1 time) | pORs of Falling (≥2 times) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Crude | p-Value | Adjusted † | p-Value | Crude | p-Value | Adjusted † | p-Value | ||
| Total participants | |||||||||
| Current arthritis | 33,873 | 2.16 (2.10–2.22) | <0.001 * | 1.35 (1.31–1.39) | <0.001 * | 2.56 (2.46–2.66) | <0.001 * | 1.56 (1.50–1.63) | <0.001 * |
| Comparison II | 289,089 | 1 | 1 | 1 | 1 | ||||
| Aged 40–49 years, men | |||||||||
| Current arthritis | 301 | 2.20 (1.66–2.93) | <0.001 * | 1.60 (1.19–2.14) | <0.002 * | 2.68 (1.84–3.91) | <0.001 * | 1.70 (1.15–2.51) | <0.007 * |
| Comparison II | 37,337 | 1 | 1 | 1 | 1 | ||||
| Aged 50–59 years, men | |||||||||
| Current arthritis | 916 | 2.17 (1.83–2.58) | <0.001 * | 1.53 (1.28–1.83) | <0.001 * | 2.84 (2.25–3.58) | <0.001 * | 1.69 (1.33–2.16) | <0.001 * |
| Comparison II | 39,826 | 1 | 1 | 1 | 1 | ||||
| Aged 60–69 years, men | |||||||||
| Current arthritis | 1986 | 1.92 (1.70–2.16) | <0.001 * | 1.49 (1.32–1.69) | <0.001 * | 2.60 (2.20–3.09) | <0.001 * | 1.75 (1.46–2.09) | <0.001 * |
| Comparison II | 33,173 | 1 | 1 | 1 | 1 | ||||
| Aged ≥ 70 years, men | |||||||||
| Current arthritis | 3789 | 1.76 (1.62–1.91) | <0.001 * | 1.47 (1.35–1.60) | <0.001 * | 2.11 (1.88–2.37) | <0.001 * | 1.61 (1.43–1.82) | <0.001 * |
| Comparison II | 31,089 | 1 | 1 | 1 | 1 | ||||
| Aged 40–49 years, women | |||||||||
| Current arthritis | 762 | 2.43 (2.05–2.88) | <0.001 * | 1.75 (1.47–2.09) | <0.001 * | 3.31 (2.63–4.17) | <0.001 * | 2.03 (1.59–2.58) | <0.001 * |
| Comparison II | 41,119 | 1 | 1 | 1 | 1 | ||||
| Aged 50–59 years, women | |||||||||
| Current arthritis | 3837 | 1.92 (1.77–2.08) | <0.001 * | 1.49 (1.37–1.62) | <0.001 * | 2.56 (2.27–2.89) | <0.001 * | 1.71 (1.50–1.94) | <0.001 * |
| Comparison II | 43,760 | 1 | 1 | 1 | 1 | ||||
| Aged 60–69 years, women | |||||||||
| Current arthritis | 8180 | 1.52 (1.43–1.62) | <0.001 * | 1.27 (1.19–1.35) | <0.001 * | 2.04 (1.85–2.24) | <0.001 * | 1.50 (1.36–1.66) | <0.001 * |
| Comparison II | 32,562 | 1 | 1 | 1 | 1 | ||||
| Aged ≥ 70 years, women | |||||||||
| Current arthritis | 14,102 | 1.44 (1.37–1.50) | <0.001 * | 1.28 (1.22–1.34) | <0.001 * | 1.74 (1.63–1.86) | <0.001 * | 1.46 (1.36–1.56) | <0.001 * |
| Comparison II | 30,223 | 1 | 1 | 1 | 1 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.W.; Kang, S.H.; Choi, H.G. Analysis of the Associations between Arthritis and Fall Histories in Korean Adults. Int. J. Environ. Res. Public Health 2021, 18, 3758. https://doi.org/10.3390/ijerph18073758
Lee JW, Kang SH, Choi HG. Analysis of the Associations between Arthritis and Fall Histories in Korean Adults. International Journal of Environmental Research and Public Health. 2021; 18(7):3758. https://doi.org/10.3390/ijerph18073758
Chicago/Turabian StyleLee, Jung Woo, Seong Hun Kang, and Hyo Geun Choi. 2021. "Analysis of the Associations between Arthritis and Fall Histories in Korean Adults" International Journal of Environmental Research and Public Health 18, no. 7: 3758. https://doi.org/10.3390/ijerph18073758
APA StyleLee, J. W., Kang, S. H., & Choi, H. G. (2021). Analysis of the Associations between Arthritis and Fall Histories in Korean Adults. International Journal of Environmental Research and Public Health, 18(7), 3758. https://doi.org/10.3390/ijerph18073758






