Profiles of Loneliness and Social Isolation in Physically Active and Inactive Older Adults in Rural England
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Theoretical Framework
2.2. Participant Selection and Recruitment
2.3. Data Collection
2.4. Data Analysis
2.4.1. Stage 1. Coding of Qualitative Data
2.4.2. Stage 2. Classification of MVPA, Social Isolation and Loneliness Profiles
2.4.3. Stage 3. Interpretation of Socioecological Factors Relating to Profiles
3. Results
3.1. Participant Characteristics
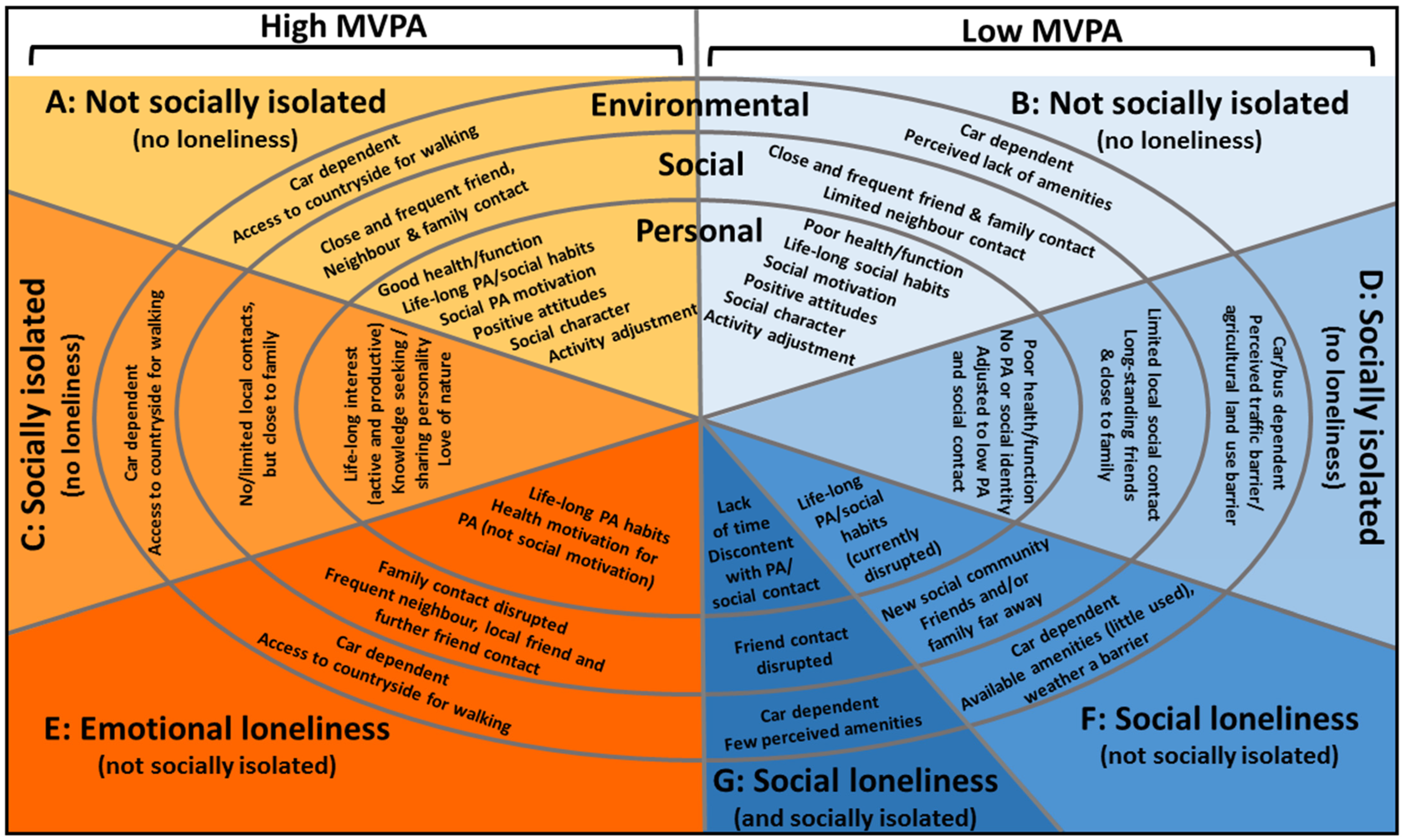
3.2. Profiles of Loneliness, Social Isolation and Physical Activity
3.2.1. High-MVPA Group
Personal Domain
“Yes I mean I’ve played tennis, ever since I was at school, so… sport and music actually, is the two things they [the school] excelled in, and I think that’s probably had a fair, um, influence on my life”(Vanessa, Profile A, age 71, 65 min. MVPA/day)
“I started coaching [athletics]… I started that and um yes, so [age] 55, 56, I’m 74, yea, so it’s continuing”; “I have always been a member of athletics clubs. Right from the age of 14 or something.”(Robert, Profile C, age 74, 58 min. MVPA/day)
“I’ve always been active dog walking and swimming”; “Even if I don’t feel like It I do it”(Margery, Profile E, age 70, 113 min. MVPA/day)
“Very much the social side, it’s very strong. Um, I wouldn’t go out and play golf on my own for example. You see one or two guys doing that but um, it’s… the fun of going.”(Phil, Profile A, age 66, 89 min. MVPA/day)
“When I go on my London [seed merchant] shows, you know, you have to be quite knowledgeable because people ask you quite searching questions. I quite like questions that I don’t know the answer to because I can go home and look them up.”(Rose, Profile C, age 68, 84 min. MVPA/day)
“I’m actually very aware of keeping very physically fit because if you’re not very physically fit you’re very restricted in what you can do.”(Barbara, Profile E, age 68, 66 min. MVPA/day)
Social Domain
“Probably one of the biggest things is I’ve got two sons and my youngest son has fallen out with the rest of the family. And um, that’s where my two grandchildren are, so I never see them… So, I feel I’ve missed out… it is quite um, I get quite distressed… quite depressed about it at times.”(Barbara, age 68, 66 min. MVPA/day)
“I was more active when I was at [age] 40 s to 50 s because, and then my partner walked out on me and broke my heart and life went down-hill”; [Interviewer: “Any significant changes since your working life?”] “Depression… And it’s still there.”(Margery, age 70, 113 min. MVPA/day)
“Yes, [my son] sings over the last few years… so whenever they put on a concert I think ‘yeah!’ I get to come you see… Well perhaps 3 or 4 times a year?”(Rose, age 68, 84 min. MVPA/day)
“There’s the regular contact with my sister in Norwich, and um my son, that may or may not be meeting with [him], if he’s down. Because he has been down to Bath on occasions, so we’ve had meals together.”(Robert, age 74, 58 min. MVPA/day)
“We have family get-togethers all the time… we all meet up we go for a walk, the family”; “We’re going down to Bay at Easter. And then I shall take my kayak down there, because the children will be down there, the grandchildren now. We’ve rented, like we do, we’ve rented a big house down there so the whole family can go down.”(Reese, age 72, 71 min. of MVPA/day)
“I try and do something every day. You know, Monday I do aqua fit… the other day, the friends that I have actually met at aqua, we went to [a nearby town].”; “And I help down at the, you know, the [social] club in the village.”(Ashley, age 69, 83 min. of MVPA/day)
Environmental Domain
“You do need a car to be able to go out and do anything really.”(Barbara, Profile E, age 68, 66 min. MVPA/day)
3.2.2. Low-MVPA Group
Personal Domain
“I go to skittles but I don’t play it now... We go to the nearby village which is over that way, and it’s a damn good evening because it’s a double alley, therefore you’ve got at least 45 people there. It’s like a little party really. Cos I know most of them, so you can have a chat with anybody you know, you know, it’s a good job.”(Mike, Profile B, age 83, 4 min. MVPA/day)
“I’m not really a physical type, I mean I’ve never particularly found physical exercise to be that rewarding… running round and round a block to keep fit, never been my thing.”; “First of all I was persuaded into taking part in that [cricket club] and then I decided it was quite, quite, yea not too bad, not too good but not too bad of a game and um I quite enjoyed it.”(Daniel, Profile D, age 68, 3 min. MVPA/day)
“I keep wanting to establish some sort of daily schedule, some sort of daily routine. I haven’t managed that yet. Being retired nearly eight years I still haven’t managed that yet… Too busy! There’s always something else… errand or a job to do.”(Nathan, Profile F, age 67, 13 min. MVPA/day)
“When I was 60 [my mother] had a massive stroke and um I’ve been looking after her full time since then. …I personally would have continued going to the flower club because I love flowers and I enjoy the socialising with the people… There are a lot of things that, yes, a lot of things that I miss out on. Because I just physically can’t do it, there isn’t time.”(Christina, Profile G, age 67, 11 min. MVPA/day)
“We’ve had a very good life actually. I’m not complaining about any of it, we’ve been very, very fortunate… I’m happy with it.”(Mary, Profile B, age 81, 2 min. MVPA/day)
“Of course he and I, had thought when we retired, that we’d go to the pub and go and see the countryside and drive around the countryside and go and see places we haven’t been to before. And that, we’ve failed miserably on all of that.”(Christina, Profile G, age 67, 11 min. MVPA/day)
Social Domain
“We’ve got quite a big circle of friends, and we entertain and we go to other people’s for tea… every week we try and do something with friends.”(Ian, Profile B, age 87, 4 min. MVPA/day)
“We have a few get-togethers now and then [with friends from previous Cricket steward team]… We used to have an annual visit somewhere.”(David, Profile D, age 68, 3 min. MVPA/day)
“[Friends in our previous village] were such a jolly lot. It was good. I miss them very much.”; “At the moment we haven’t been going out much because we’re always doing one of the flats [work]. It’s been a bit of a bugbear… I want to go and visit friends again. Because we’ve been so cut off from people recently, with the lifestyle that we’ve had. I would like to go and see friends again.”(Sandra, Profile G, age 71, 6 min. MVPA/day)
Environmental Domain
“The traffic has increased. We’ve got bicycles in the shed but we never use them because it’s too dangerous.”(Ray, Profile D, age 77, 3 min. MVPA/day)
“The road is terrible. We haven’t got a path until we get just past that mucky farm, and that’s all muddy;”(Joan, Profile B, age 80, 7 min. MVPA/day)
“The other thing round here is that the farmers have ploughed up a lot of the footpaths… You can walk round the edge of the field, under sufferance, if you don’t mind walking through some nettles and brambles and this sort of thing… there’s no way I’m going to walk along a field of vegetables.”(Barry, age 72, Profile F: 3 min. MVPA/day)
“If we didn’t have the car and we’d have to rely on buses, we’d be restricted… if they take away my licence we shall be in trouble.”(Ian, Profile B, age 87, 4 min. MVPA/day)
“If they stopped the busses then that’d be it… I suppose I’d have to move.”(Joan, Profile B, age 80, 7 min. MVPA/day)
4. Discussion
4.1. Strengths and Limitations
4.2. Research Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Elovainio, M.; Hakulinen, C.; Pulkki-Råback, L.; Virtanen, M.; Josefsson, K.; Jokela, M.; Vahtera, J.; Kivimäki, M. Contribution of risk factors to excess mortality in isolated and lonely individuals: An analysis of data from the UK Biobank cohort study. Lancet Public Health 2017, 2, e260–e266. [Google Scholar] [CrossRef] [Green Version]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and social isolation as risk factors for mortality a meta-analytic review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [Green Version]
- Valtorta, N.K.; Kanaan, M.; Gilbody, S.; Ronzi, S.; Hanratty, B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. Heart 2016, 102, 1009–1016. [Google Scholar] [CrossRef] [Green Version]
- Shankar, A.; McMunn, A.; Demakakos, P.; Hamer, M.; Steptoe, A. Social isolation and loneliness: Prospective associations with functional status in older adults. Health Psychol. 2017, 36, 179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burholt, V.; Dobbs, C. Research on rural ageing: Where have we got to and where are we going in Europe? J. Rural Stud. 2012, 28, 432–446. [Google Scholar] [CrossRef] [Green Version]
- De Koning, J.; Richards, S.H.; Stathi, A. Predictors of loneliness and different types of social isolation of rural-living older adults in the UK. Ageing Soc. 2016, 37, 2012–2043. [Google Scholar] [CrossRef] [Green Version]
- Perlman, D.; Peplau, L.A. Toward a social psychology of loneliness. Pers. Relat. 1981, 3, 31–56. [Google Scholar]
- Weiss, R.S. Loneliness: The Experience of Emotional and Social Isolation; The MIT Press: Cambridge, MA, USA, 1973. [Google Scholar]
- Victor, C.R.; Bond, J.; Bowling, A. Loneliness, Social Isolation and Living Alone in Later Life; Economic and Social Research Council: London, UK, 2003. [Google Scholar]
- Wenger, G.C.; Burholt, V. Changes in Levels of Social Isolation and Loneliness among Older People in a Rural Area: A Twenty-Year Longitudinal Study. Can. J. Aging 2004, 23, 115–127. [Google Scholar] [CrossRef] [PubMed]
- CCornwell, E.Y.; Waite, L.J. Social disconnectedness, perceived isolation, and health among older adults. J. Health Soc. Behav. 2009, 50, 31–48. [Google Scholar] [CrossRef] [Green Version]
- Havens, B.; Hall, M.; Sylvestre, G.; Jivan, T. Social isolation and loneliness: Differences between older rural and urban Manitobans. Can. J. Aging 2004, 23, 129–140. [Google Scholar] [CrossRef]
- Peplau, L.A.; Perlman, D. Perspectives on loneliness. In Loneliness: A Sourcebook of Current Theory, Research and Therapy; Peplau, L.A., Perlman, D., Eds.; John Wiley & Sons: New York, NY, USA, 1982; pp. 1–18. [Google Scholar]
- Graneheim, U.H.; Lundman, B. Experiences of loneliness among the very old: The Umeå 85+ project. Aging Ment. Health 2010, 14, 433–438. [Google Scholar] [CrossRef]
- Hauge, S.; Kirkevold, M. Variations in older persons’ descriptions of the burden of loneliness. Scand. J. Caring Sci. 2012, 26, 553–560. [Google Scholar] [CrossRef]
- Dahlberg, K. The enigmatic phenomenon of loneliness. Int. J. Qual. Stud. Health Well-Being 2007, 2, 195–207. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Thisted, R.A.; Cacioppo, J.T. Loneliness predicts reduced physical activity: Cross-sectional & longitudinal analyses. Health Psychol. 2009, 28, 354. [Google Scholar]
- Luo, Y.; Waite, L.J. Loneliness and mortality among older adults in China. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2014, 69, 633–645. [Google Scholar] [CrossRef] [Green Version]
- Netz, Y.; Goldsmith, R.; Shimony, T.; Arnon, M.; Zeev, A. Loneliness is associated with an increased risk of sedentary life in older Israelis. Aging Ment. Health 2013, 17, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Pels, F.; Kleinert, J. Loneliness and physical activity: A systematic review. Int. Rev. Sport Exerc. Psychol. 2016, 9, 231–260. [Google Scholar] [CrossRef]
- Shankar, A.; McMunn, A.; Banks, J.; Steptoe, A. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011, 30, 377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theeke, L.A. Predictors of loneliness in US adults over age sixty-five. Arch. Psychiatr. Nurs. 2009, 23, 387–396. [Google Scholar] [CrossRef]
- De Koning, K.; Richards, S.; Stathi, A. Loneliness, Social Isolation, and Objectively Measured Physical Activity in Rural-Living Older Adults. J. Aging Phys. Act. 2019, 28, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Harris, T.J.; Owen, C.G.; Victor, C.R.; Adams, R.; Cook, D.G. What factors are associated with physical activity in older people, assessed objectively by accelerometry? Br. J. Sports Med. 2009, 43, 442–450. [Google Scholar] [CrossRef]
- Newall, N.E.; Chipperfield, J.G.; Bailis, D.S.; Stewart, T.L. Consequences of loneliness on physical activity and mortality in older adults and the power of positive emotions. Health Psychol. 2013, 32, 921–924. [Google Scholar] [CrossRef]
- Eckert, K.G.; Lange, M.A. Comparison of physical activity questionnaires for the elderly with the International Classification of Functioning, Disability and Health (ICF)—An analysis of content. BMC Public Health 2015, 15, 249. [Google Scholar] [CrossRef] [Green Version]
- Rastad, C.; Martin, C.; Åsenlöf, P. Barriers, benefits, and strategies for physical activity in patients with schizophrenia. Phys. Ther. 2014, 94, 1467–1479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doyle, L.; Brady, A.-M.; Byrne, G. An overview of mixed methods research. J. Res. Nurs. 2009, 14, 175–185. [Google Scholar] [CrossRef]
- Davis, M.G.; Fox, K.R.; Hillsdon, M.; Sharp, D.J.; Coulson, J.C.; Thompson, J.L. Objectively measured physical activity in a diverse sample of older urban UK adults. Med. Sci. Sports Exerc. 2011, 43, 647–654. [Google Scholar] [CrossRef]
- Jefferis, B.J.; Sartini, C.; Lee, I.-L.; Choi, M.; Amuzu, A.; Gutierrez, C.; Casas, J.P.; Ash, S.; Lennnon, L.T.; Wannamethee, S.G.; et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health 2014, 14, 382. [Google Scholar] [CrossRef] [Green Version]
- McMurdo, M.E.T.; Argo, I.; Crombie, I.K.; Feng, Z.; Sniehotta, F.F.; Vadiveloo, T.; Witham, M.D.; Donnan, P.T. Social, environmental and psychological factors associated with objective physical activity levels in the over 65s. PLoS ONE 2012, 7, e31878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef]
- Yang, K.; Victor, C. Age and loneliness in 25 European nations. Ageing Soc. 2011, 31, 1368–1388. [Google Scholar] [CrossRef]
- Harper, R.; Kelly, M. Measuring Social Capital in the United Kingdom; Office for National Statistics: London, UK, 2003. Available online: https://lemosandcrane.co.uk/resources/National%20Stats%20-%20Measuring%20Social%20Capital.pdf (accessed on 7 April 2021).
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.; Martin, B.W.; Group, L.P.A.S.W. Correlates of physical activity: Why are some people physically active and others not? Lancet 2012, 380, 258–271. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Timperio, A.; Bull, F.; Pikora, T. Understanding physical activity environmental correlates: Increased specificity for ecological models. Exerc. Sport Sci. Rev. 2005, 33, 175–181. [Google Scholar] [CrossRef]
- Sallis, J.F.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Annu. Rev. Public Health 2006, 27, 297–322. [Google Scholar] [CrossRef] [Green Version]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- UK Government. UK Chief Medical Officers’ Physical Activity Guidelines. Available online: https://www.gov.uk/government/publications/physical-activity-guidelines-uk-chief-medical-officers-report (accessed on 20 September 2019).
- Coudin, G.; Alexopoulos, T. ‘Help me! I’m old!’ How negative aging stereotypes create dependency among older adults. Aging Ment. Health 2010, 14, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Morse, J.M.; Barrett, M.; Mayan, M.; Olson, K.; Spiers, J. Verification strategies for establishing reliability and validity in qualitative research. Int. J. Qual. Methods 2002, 1, 13–22. [Google Scholar] [CrossRef]
- Guba, E.; Lincoln, Y. Chapter 8; Paradigmatic Controversies, contradictions and emerging confluences. In The Sage Handbook of Qualitative Research, 3rd ed.; Sage Publications: London, UK, 2005. [Google Scholar]
- Miles, M.B.; Huberman, A.M.; Saldana, J. Qualitative Data Analysis, 3rd ed.; Sage: London, UK, 2014. [Google Scholar]
- Camfield, L.; Crivello, G.; Woodhead, M. Wellbeing research in developing countries: Reviewing the role of qualitative methods. Soc. Ind. Res. 2009, 90, 5–31. [Google Scholar] [CrossRef]
- Holloway, I.; Biley, F.C. Being a qualitative researcher. Qual. Health Res. 2011, 21, 968–975. [Google Scholar] [CrossRef]
- Shiovitz-Ezra, S.; Ayalon, L. Use of direct versus indirect approaches to measure loneliness in later life. Res. Aging 2012, 34, 572–591. [Google Scholar] [CrossRef]
- Victor, C.R.; Grenade, L.; Boldy, D. Measuring loneliness in later life: A comparison of differing measures. Rev. Clin. Gerontol. 2005, 15, 63–70. [Google Scholar] [CrossRef]
- Cowan, D.; Taylor, I.M. ‘I’m proud of what I achieved; I’m also ashamed of what I done’: A soccer coach’s tale of sport, status, and criminal behaviour. Qual. Res. Sport Exerc. Health 2016, 8, 505–518. [Google Scholar] [CrossRef] [Green Version]
- De Koning, J.; Stathi, A.; Fox, K.R. Similarities and differences in the determinants of trips outdoors performed by UK urban-and rural-living older adults. J. Aging Phys. Act. 2015, 23, 613–621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barg, F.K.; Huss-Ashmore, R.; Wittink, M.N.; Murray, G.F.; Bogner, H.R.; Gallo, J.J. A mixed-methods approach to understanding loneliness and depression in older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2006, 61, S329–S339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lou, V.W.; Ng, J.W. Chinese older adults’ resilience to the loneliness of living alone: A qualitative study. Aging Ment. Health 2012, 16, 1039–1046. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machielse, A. The heterogeneity of socially isolated older adults: A social isolation typology. J. Gerontol. Soc. Work 2015, 58, 338–356. [Google Scholar] [CrossRef] [PubMed]
- McHugh Power, J.E.; Hannigan, C.; Carney, S.; Lawlor, B.A. Exploring the meaning of loneliness among socially isolated older adults in rural Ireland: A qualitative investigation. Qual. Res. Psychol. 2017, 14, 394–414. [Google Scholar] [CrossRef]
- Sullivan, M.P.; Victor, C.R.; Thomas, M.; Poland, F.; Milne, A. Understanding and alleviating loneliness in later life: Perspectives of older people. Qual. Ageing Older Adults 2016, 17, 168–178. [Google Scholar] [CrossRef]
- Brittain, K.; Kingston, A.; Davies, K.; Collerton, J.; Robinson, L.A.; Kirkwood, T.B.; Bond, J.; Jagger, C. An investigation into the patterns of loneliness and loss in the oldest old—Newcastle 85+ Study. Ageing Soc. 2017, 37, 39–62. [Google Scholar] [CrossRef]
- Dahlberg, L.; McKee, K.J. Correlates of social and emotional loneliness in older people: Evidence from an English community study. Aging Ment. Health 2014, 18, 504–514. [Google Scholar] [CrossRef] [Green Version]
- Dykstra, P.A.; Fokkema, T. Social and emotional loneliness among divorced and married men and women: Comparing the deficit and cognitive perspectives. Basic Appl. Soc. Psychol. 2007, 29, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Tiilikainen, E.; Seppanen, M. Lost and unfulfilled relationships behind emotional loneliness in old age. Ageing Soc. 2017, 37, 1068–1088. [Google Scholar] [CrossRef] [Green Version]
- Vasileiou, K.; Barnett, J.; Barreto, M.; Vines, J.; Atkinson, M.; Lawson, S.; Wilson, M. Experiences of Loneliness Associated with Being an Informal Caregiver: A Qualitative Investigation. Front. Psychol. 2017, 8, 585. [Google Scholar] [CrossRef] [Green Version]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Koeneman, M.A.; Verheijden, M.W.; Chinapaw, M.J.; Hopman-Rock, M. Determinants of physical activity and exercise in healthy older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, e142. [Google Scholar] [CrossRef] [Green Version]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [Green Version]
- Cuddy, A.J.; Norton, M.I.; Fiske, S.T. This old stereotype: The pervasiveness and persistence of the elderly stereotype. J. Soc. Issues 2005, 61, 267–285. [Google Scholar] [CrossRef]
- Dykstra, P.A. Older adult loneliness: Myths and realities. Eur. J. Ageing 2009, 6, 91–100. [Google Scholar] [CrossRef] [Green Version]
- Pikhartova, J.; Bowling, A.; Victor, C. Is loneliness in later life a self-fulfilling prophecy? Aging Ment. Health 2016, 20, 543–549. [Google Scholar] [CrossRef] [Green Version]
- Baxter, S.; Johnson, M.; Payne, N.; Buckley-Woods, H.; Blank, L.; Hock, E.; Daley, A.; Taylor, A.; Pavey, T.; Mountain, G. Promoting and maintaining physical activity in the transition to retirement: A systematic review of interventions for adults around retirement age. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 12. [Google Scholar] [CrossRef] [Green Version]
- McMahon, S.; Fleury, J. External validity of physical activity interventions for community-dwelling older adults with fall risk: A quantitative systematic literature review. J. Adv. Nurs. 2012, 68, 2140–2154. [Google Scholar] [CrossRef]
| Example Statements | |
| Social isolation | “I hardly ever see XXX” “I only see XXX about twice a year” |
| Discrepancy Theory of Loneliness | |
| Emotional loneliness | “I miss a really close relationship…” “I don’t feel close to anyone…” |
| Social loneliness | “I miss seeing my old friends/neighbours…” |
| Cognitive Theory of Loneliness | |
| Dissatisfaction with levels of contact | “I don’t have enough contact with my family/friends/neighbours…” “In my retirement I expected to have more contact with my friends…” “I get very sad about not seeing my family…” |
| Pseudonym (Sex) | Age | MVPA | PF 1 | Interview Data | Questionnaire Data | ||
|---|---|---|---|---|---|---|---|
| Loneliness 2 | Social Isolation | Loneliness | Social Isolation | ||||
| High MVPA | |||||||
| Phil (M) | 66 | 89 | 12 | Not lonely | Not SI | Hardly ever | Not SI |
| Mark (M) | 66 | 87 | 11 | Not lonely | Not SI | Hardly ever | SI family |
| Rose (F) | 68 | 84 | 9 | Not lonely | SI all | Hardly ever | SI all |
| Bill (M) | 68 | 81 | 10 | Not lonely | Not SI | Hardly ever | SI family |
| Barbara (F) | 68 | 66 | 10 | E. lonely | Not SI | Often | SI family |
| Ashley (F) | 69 | 83 | 11 | Not lonely | Not SI | Sometimes | SI family |
| Margery (F) | 70 | 113 | 11 | E. lonely | Not SI | Sometimes | SI family |
| Vanessa (F) | 71 | 65 | 11 | Not lonely | Not SI | Hardly ever | Not SI |
| Reese (M) | 72 | 71 | 10 | Not lonely | Not SI | Hardly ever | SI family |
| Robert (M) | 74 | 58 | 9 | Not lonely | SI friends and neighbours | Hardly ever | SI family and friends |
| Warren (M) | 77 | 39 | 10 | Not lonely | Not SI | Hardly ever | SI family |
| Isla (F) | 81 | 40 | 10 | Not lonely | Not SI | Hardly ever | SI friends |
| Low MVPA | |||||||
| Nathan (M) | 67 | 13 | 12 | S. lonely | Not SI | Hardly ever | SI family |
| Christina (F) | 67 | 11 | 10 | S. lonely | SI friends | Hardly ever | SI family |
| Daniel (M) | 68 | 3 | 7 | Not lonely | SI friends | Hardly ever | SI family and friends |
| Sandra (F) | 71 | 6 | 11 | S. lonely | SI friends and neighbours | Hardly ever | SI family and friends |
| Barry (M) | 72 | 3 | 6 | S. lonely | Not SI | Hardly ever | SI friends |
| Janice (F) | 73 | 4 | 6 | Not lonely | Not SI | Hardly ever | SI family |
| Eve (F) | 77 | 4 | 8 | Not lonely | Not SI | Hardly ever | SI family |
| Ray (M) | 77 | 3 | 11 | Not lonely | Not SI | Often | SI family |
| Joan (F) | 80 | 7 | 6 | Not lonely | Not SI | Hardly ever | SI friends and neighbours |
| Mary (F) | 81 | 2 | 9 | Not lonely | Not SI | Hardly ever | SI family |
| Mike (M) | 83 | 4 | 9 | Not lonely | Not SI | Hardly ever | Not SI |
| Ian (M) | 87 | 4 | 9 | Not lonely | Not SI | Hardly ever | SI family |
| High MVPA | Low MVPA | |
|---|---|---|
| Not Socially Isolated | Profile A: Not socially isolated/ not lonely (8/12) | Profile B: Not socially isolated/ not lonely (7/12) |
| Profile C: Socially isolated/ not lonely (2/12) | Profile D: Socially isolated/ not lonely (1/12) | |
| Lonely | Profile E: Emotional loneliness/ not socially isolated (2/12) | Profile F: Social loneliness/ not socially isolated (2/12) |
| Profile G: Social loneliness/ socially isolated (2/12) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Koning, J.; Richards, S.H.; Wood, G.E.R.; Stathi, A. Profiles of Loneliness and Social Isolation in Physically Active and Inactive Older Adults in Rural England. Int. J. Environ. Res. Public Health 2021, 18, 3971. https://doi.org/10.3390/ijerph18083971
de Koning J, Richards SH, Wood GER, Stathi A. Profiles of Loneliness and Social Isolation in Physically Active and Inactive Older Adults in Rural England. International Journal of Environmental Research and Public Health. 2021; 18(8):3971. https://doi.org/10.3390/ijerph18083971
Chicago/Turabian Stylede Koning, Jolanthe, Suzanne H Richards, Grace E R Wood, and Afroditi Stathi. 2021. "Profiles of Loneliness and Social Isolation in Physically Active and Inactive Older Adults in Rural England" International Journal of Environmental Research and Public Health 18, no. 8: 3971. https://doi.org/10.3390/ijerph18083971
APA Stylede Koning, J., Richards, S. H., Wood, G. E. R., & Stathi, A. (2021). Profiles of Loneliness and Social Isolation in Physically Active and Inactive Older Adults in Rural England. International Journal of Environmental Research and Public Health, 18(8), 3971. https://doi.org/10.3390/ijerph18083971






