Athletes’ Self-Assessment of Urine Color Using Two Color Charts to Determine Urine Concentration
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Urine Color Charts
2.2.1. Development of the New 7-Color Uc Chart
2.2.2. Remaking a Traditional 8-Color Chart
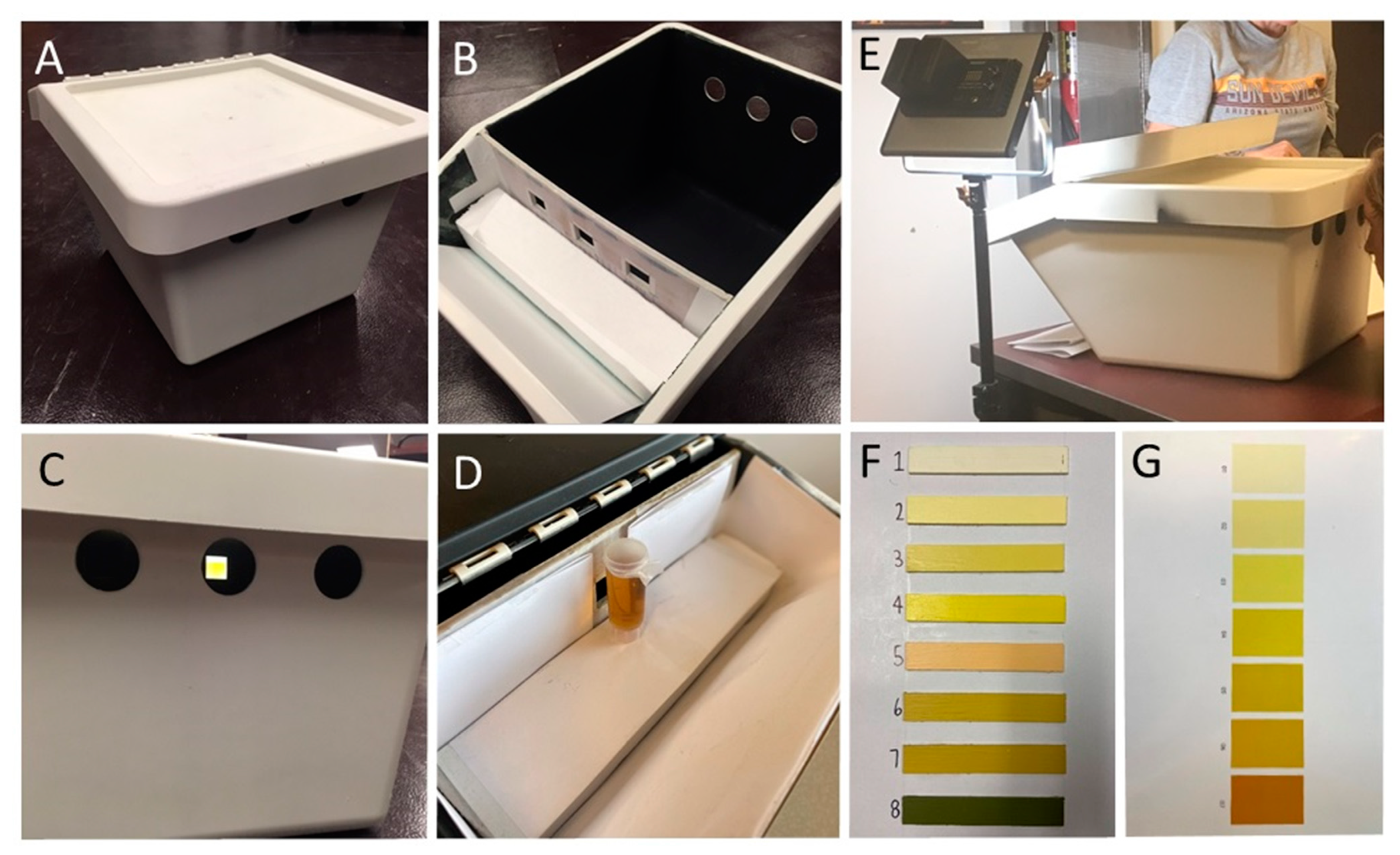
2.3. Uc Scoring Box
2.4. Procedures
2.4.1. Urine Color Scoring
2.4.2. Urinalysis
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Armstrong, L.E.; Maresh, C.M.; Castellani, J.W.; Bergeron, M.F.; Kenefick, R.W.; LaGasse, K.E.; Riebe, D. Urinary indices of hydration status. Int. J. Sport Nutr. 1994, 4, 265–279. [Google Scholar] [CrossRef]
- Armstrong, L.E.; Herrera Soto, J.A.; Hacker, F.T.; Casa, D.J.; Kavouras, S.A.; Maresh, C.M. Urinary indices during dehydration, exercise, and rehydration. Int. J. Sport Nutr. Exerc. Metab. 1998, 8, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Baron, S.; Courbebaisse, M.; Lepicard, E.M.; Friedlander, G. Assessment of hydration status in a large population. Br. J. Nutr. 2015, 113, 147–158. [Google Scholar] [CrossRef] [Green Version]
- Kavouras, S.A.; Johnson, E.C.; Bougatsas, D.; Arnaoutis, G.; Panagiotakos, D.B.; Perrier, E.; Klein, A. Validation of a urine color scale for assessment of urine osmolality in healthy children. Eur. J. Nutr. 2016, 55, 907–915. [Google Scholar] [CrossRef] [Green Version]
- Kenney, E.L.; Long, M.W.; Cradock, A.L.; Gortmaker, S.L. Prevalence of inadequate hydration among US children and disparities by gender and Race/Ethnicity: National Health and Nutrition Examination Survey, 2009–2012. Am. J. Public Health 2015, 105, e113–e118. [Google Scholar] [CrossRef] [PubMed]
- Perrier, E.T.; Bottin, J.H.; Vecchio, M.; Lemetais, G. Criterion values for urine-specific gravity and urine color representing adequate water intake in healthy adults. Eur. J. Clin. Nutr. 2017, 71, 561–563. [Google Scholar] [CrossRef] [Green Version]
- Wardenaar, F.C.; Thompsett, D.; Vento, K.A.; Bacalzo, D. A lavatory urine color (LUC) chart method can identify hypohydration in a physically active population. Eur. J. Nutr. 2021. [Google Scholar] [CrossRef]
- Kostelnik, S.B.; Davy, K.P.; Hedrick, V.E.; Thomas, D.T.; Davy, B.M. The validity of urine color as a hydration biomarker within the general adult population and athletes: A systematic review. J. Am. Coll. Nutr. 2020, 40, 172–179. [Google Scholar] [CrossRef]
- McDermott, B.P.; Anderson, S.A.; Armstrong, L.E.; Casa, D.J.; Cheuvront, S.N.; Cooper, L.; Kenney, W.L.; O’Connor, F.G.; Roberts, W.O.; Larry Kenney, W.; et al. National Athletic Trainers’ Association position statement: Fluid replacement for the physically active. J. Athl. Train. 2017, 52, 877–895. [Google Scholar] [CrossRef] [Green Version]
- Olzinski, S.; Beaumont, J.; Toledo, M.; Yudell, A.; Johnston, C.S.; Wardenaar, F.C. Hydration status and fluid needs of division I female collegiate athletes exercising indoors and outdoors. Sports 2019, 7, 155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maerz, A.; Paul, M.R. A Dictionary of Color; McGraw-Hill 1950: New York, NY, USA, 1985. [Google Scholar]
- Adams, J.D.; Kavouras, S.A.; Johnson, E.C.; Jansen, L.T.; Capitan-Jimenez, C.; Robillard, J.I.; Mauromoustakos, A. The effect of storing temperature and duration on urinary hydration markers. Int. J. Sport Nutr. Exerc. Metab. 2017, 27, 18–24. [Google Scholar] [CrossRef]
- Sommerfield, L.M.; McAnulty, S.R.; McBride, J.M.; Zwetsloot, J.J.; Austin, M.D.; Mehlhorn, J.D.; Calhoun, M.C.; Young, J.O.; Haines, T.L.; Utter, A.C. Validity of urine specific gravity when compared with plasma osmolality as a measure of hydration status in male and female NCAA collegiate athletes. J. Strength Cond. Res. 2016, 30, 2219–2225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armstrong, L.E.; Pumerantz, A.C.; Fiala, K.A.; Roti, M.W.; Kavouras, S.A.; Casa, D.J.; Maresh, C.M. Human hydration indices: Acute and longitudinal reference values. Int. J. Sport Nutr. Exerc. Metab. 2010, 20, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, L.E.; Johnson, E.C.; McKenzie, A.L.; Muñoz, C.X. An empirical method to determine inadequacy of dietary water. Nutrition 2016, 32, 79–82. [Google Scholar] [CrossRef]
- Cheuvront, S.N.; Ely, B.R.; Kenefick, R.W.; Sawka, M.N. Biological variation and diagnostic accuracy of dehydration assessment markers. Am. J. Clin. Nutr. 2010, 92, 565–573. [Google Scholar] [CrossRef] [Green Version]
- Hew-Butler, T.D.; Eskin, C.; Bickham, J.; Rusnak, M.; Vandermeulen, M. Dehydration is how you define it: Comparison of 318 blood and urine athlete spot checks. BMJ Open Sport Exerc. Med. 2018, 4, 297. [Google Scholar] [CrossRef] [Green Version]
- Kenefick, R.W.; Heavens, K.R.; Dennis, W.E.; Caruso, E.M.; Guerriere, K.I.; Charkoudian, N.; Cheuvront, S.N. Quantification of chromatographic effects of Vitamin B supplementation in urine and implications for hydration assessment. J. Appl. Physiol. 2015, 119, 110–115. [Google Scholar] [CrossRef] [Green Version]
- Ellis, L.A.; Yates, B.A.; McKenzie, A.L.; Muñoz, C.X.; Casa, D.J.; Armstrong, L.E. Effects of three oral nutritional supplements on human hydration indices. Int. J. Sport Nutr. Exerc. Metab. 2016, 26, 356–362. [Google Scholar] [CrossRef]
- Bottin, J.H.; Lemetais, G.; Poupin, M.; Jimenez, L.; Perrier, E.T. Equivalence of afternoon spot and 24-h urinary hydration biomarkers in free-living healthy adults. Eur. J. Clin. Nutr. 2016, 70, 904–907. [Google Scholar] [CrossRef] [Green Version]
- Suh, H.G.; Summers, L.D.G.; Seal, A.D.; Colburn, A.T.; Mauromoustakos, A.; Perrier, E.T.; Bottin, J.H.; Kavouras, S.A. Afternoon urine osmolality is equivalent to 24 h for hydration assessment in healthy children. Eur. J. Clin. Nutr. 2020, 74, 884–890. [Google Scholar] [CrossRef] [Green Version]
- Perrier, E.; Demazières, A.; Girard, N.; Pross, N.; Osbild, D.; Metzger, D.; Guelinckx, I.; Klein, A. Circadian variation and responsiveness of hydration biomarkers to changes in daily water intake. Eur. J. Appl. Physiol. 2013, 113, 2143–2151. [Google Scholar] [CrossRef] [Green Version]
- Kenefick, R.W.; Cheuvront, S.N. Hydration for recreational sport and physical activity. Nutr. Rev. 2012, 70, S137–S142. [Google Scholar] [CrossRef]
- Kavouras, S.A. Hydration, dehydration, underhydration, optimal hydration: Are we barking up the wrong tree? Eur. J. Nutr. 2019, 58, 471–473. [Google Scholar] [CrossRef]
- Stookey, J.D.; Brass, B.; Holliday, A.; Arieff, A. What is the cell hydration status of healthy children in the USA? Preliminary data on urine osmolality and water intake. Public Health Nutr. 2012, 15, 2148–2156. [Google Scholar] [CrossRef] [Green Version]
- Reis, J.F.; Matias, C.N.; Campa, F.; Morgado, J.P.; Franco, P.; Quaresma, P.; Almeida, N.; Curto, D.; Toselli, S.; Monteiro, C.P. Bioimpedance vector patterns changes in response to swimming training: An ecological approach. Int. J. Environ. Res. Public Health 2020, 17, 4851. [Google Scholar] [CrossRef]
- Campa, F.; Piras, A.; Raffi, M.; Trofè, A.; Perazzolo, M.; Mascherini, G.; Toselli, S. The effects of dehydration on metabolic and neuromuscular functionality during cycling. Int. J. Environ. Res. Public Health 2020, 17, 1161. [Google Scholar] [CrossRef] [Green Version]
- Kavouras, S.A.; Arnaoutis, G.; Makrillos, M.; Garagouni, C.; Nikolaou, E.; Chira, O.; Ellinikaki, E.; Sidossis, L.S. Educational intervention on water intake improves hydration status and enhances exercise performance in athletic youth. Scand. J. Med. Sci. Sport. 2012, 22, 684–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, J.D.; Arnaoutis, G.; Johnson, E.C.; Jansen, L.T.; Bougatsas, D.; Capitan-Jimenez, C.; Mauromoustakos, A.; Panagiotakos, D.B.; Perrier, E.T.; Guelinckx, I.; et al. Combining urine color and void number to assess hydration in adults and children. Eur. J. Clin. Nutr. 2021. [Google Scholar] [CrossRef]

| Age (y) | Height (m) | Weight (kg) | Urine Volume (mL) | Urine Concentration | First Morning Sample (%) | Voiding Duration | |||
|---|---|---|---|---|---|---|---|---|---|
| Osmolality (mmol·kg−1) | USG | r | (sec.) | ||||||
| Total (n = 189) | 20 (19–22) | 1.73 (1.67–1.79) | 70.0 (63.0–79.0) | 248 (137–391) | 705 (456–930) | 1.019 (1.013–1.024) | 0.89 * | 58.7 | 16 (11–25) |
| Sex | |||||||||
| Male (n = 99) | 20 (19–22) | 1.77 (1.73–1.81) | 75.8 (69.2–84.0) | 273 (158–437) | 741 (505–938) | 1.020 (1.013–1.024) | 0.80 * | 62.6 | 18 (12–29) |
| Female (n = 90) | 20 (19–21) | 1.68 (1.64–1.73) | 64.4 (58.0–72.8) | 231 (123–366) | 655 (382–884) | 1.017 (1.011–1.023) | 0.97 * | 54.4 | 13 (10–21) |
| Race and ethnicity | |||||||||
| Black (n = 22) | 20 (18–21) | 172 (167–176) | 68.1 (62.8–74.8) | 174 (107–278) | 732 (499–1017) | 1.020 (1.015–1.028) | 0.88 * | 13.6 | 12 (7–17) |
| White (n = 105) | 20 (19–21) | 173 (168–179) | 70.4 (64.5–79.6) | 248 (140–391) | 722 (388–931) | 1.019 (1.010–1.024) | 0.86 * | 60.0 | 17 (11–25) |
| Hispanic (n = 29) | 19 (19–21) | 170 (165–179) | 67.3 (58.1–77.2) | 206 (123–340) | 656 (465–932) | 1.017 (1.013–1.024) | 0.90 * | 51.7 | 13 (9–17) |
| Other (n = 33) | 34 (22–39) | 174 (167–180) | 73.0 (60.4–81.7) | 358 (197–555) | 661 (472–859) | 1.018 (1.013–1.023) | 0.95 * | 90.9 | 28 (17–37) |
| Exercise level | |||||||||
| Student athlete (n = 132) | 20 (19–21) | 172 (167–178) | 68.7 (62.4–78.4) | 217 (122–364) | 724 (459–941) | 1.019 (1.012–1.025) | 0.86 * | 41.7 | 13 (10–21) |
| Army ROTC (n = 33) | 19 (18–21) | 175 (166–180) | 70.6 (65.5–78.8) | 281 (175–424) | 616 (385–860) | 1.016 (1.012–1.023) | 0.98 * | 97.0 | 20 (14–29) |
| Coach (n = 24) | 37 (34–39) | 174 (168–180) | 73.3 (60.8–84.7) | 400 (329–620) | 663 (471–834) | 1.019 (1.014–1.022) | 0.91 * | 100 | 34 (22–40) |
| Category | Urine Concentration Markers | Receiver Operator Characteristics | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uc | Min-Max | r (Uc vs. Concentration) | AUC | Sensitivity | Specificity | TP | TN | FP | FN | Accuracy | Cut-off Uc | |
| 8-color chart vs. Osm | 2 (1–3) | 1–7 | 0.65 * (0.56–0.73) | 0.76 | 47.5% | 91.3% | 57 | 63 | 6 | 63 | 63.5% | 1 |
| 8-color chart vs. USG | 2 (1–3) | 1–7 | 0.74 * (0.67–0.80) | 0.86 | 95.1% | 56.3% | 97 | 49 | 38 | 5 | 77.2% | ≤2 |
| 7-color chart vs. Osm | 2 (1–2) | 1–7 | 0.58 * (0.48–0.67) | 0.74 | 57.5% | 81.2% | 69 | 56 | 13 | 51 | 66.1% | 1 |
| 7-color chart vs. USG | 2 (1–2) | 1–7 | 0.68 * (0.60–0.75) | 0.83 | 68.6% | 86.2% | 70 | 75 | 12 | 32 | 76.7% | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wardenaar, F.C.; Thompsett, D.; Vento, K.A.; Pesek, K.; Bacalzo, D. Athletes’ Self-Assessment of Urine Color Using Two Color Charts to Determine Urine Concentration. Int. J. Environ. Res. Public Health 2021, 18, 4126. https://doi.org/10.3390/ijerph18084126
Wardenaar FC, Thompsett D, Vento KA, Pesek K, Bacalzo D. Athletes’ Self-Assessment of Urine Color Using Two Color Charts to Determine Urine Concentration. International Journal of Environmental Research and Public Health. 2021; 18(8):4126. https://doi.org/10.3390/ijerph18084126
Chicago/Turabian StyleWardenaar, Floris C., Daniel Thompsett, Kaila A. Vento, Kathryn Pesek, and Dean Bacalzo. 2021. "Athletes’ Self-Assessment of Urine Color Using Two Color Charts to Determine Urine Concentration" International Journal of Environmental Research and Public Health 18, no. 8: 4126. https://doi.org/10.3390/ijerph18084126
APA StyleWardenaar, F. C., Thompsett, D., Vento, K. A., Pesek, K., & Bacalzo, D. (2021). Athletes’ Self-Assessment of Urine Color Using Two Color Charts to Determine Urine Concentration. International Journal of Environmental Research and Public Health, 18(8), 4126. https://doi.org/10.3390/ijerph18084126







