Seroprevalence of SARS-CoV-2 Infection among Occupational Groups from the Bucaramanga Metropolitan Area, Colombia
Abstract
:1. Introduction
2. Materials and Methods
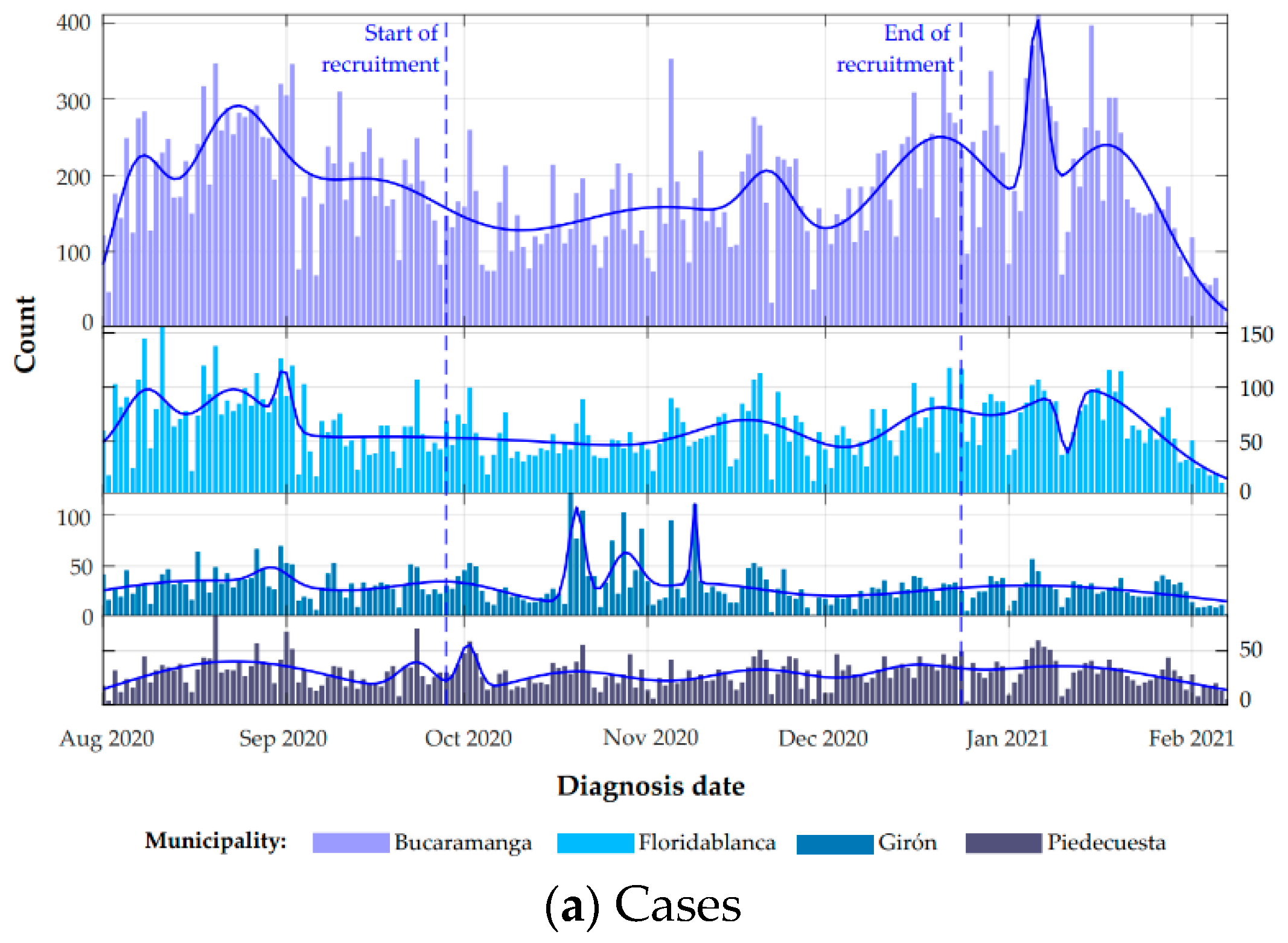
2.1. Study Design and Population Recruited
2.2. Sampling Methods
2.3. Data Collection and Variables Measured
2.4. Geolocation
2.5. IgG and IgM Measurement
2.6. Statistical Methods
3. Results
3.1. Spatial Characterization
3.2. Clinical Data
3.3. Exposure Variables
3.4. Seroprevalence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldsztejn, U.; Schwartzman, D.; Nehorai, A. Public policy and economic dynamics of COVID-19 spread: A mathematical modeling study. PLoS ONE 2020, 15, e0244174. [Google Scholar] [CrossRef] [PubMed]
- McKee, M.; Stuckler, D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat. Med. 2020, 26, 640–642. [Google Scholar] [CrossRef] [Green Version]
- Informe de Políticas Sobre los Efectos de la COVID-19 en América Latina y el Caribe. UNFPA América Latina y el Caribe. 2020. Available online: https://lac.unfpa.org/es/publications/informe-de-pol%C3%ADticas-sobre-los-efectos-de-la-covid-19-en-am%C3%A9rica-latina-y-el-caribe (accessed on 1 March 2021).
- Informe de Política Monetaria—Abril de 2020. Banco de la República (Banco Central de Colombia). 2020. Available online: https://www.banrep.gov.co/es/informe-politica-monetaria-abril-2020 (accessed on 1 March 2021).
- Comisión Económica Para América Latina y el Caribe. Enfrentar los Efectos Cada Vez Mayores del COVID-19 Para Una Reactivación Con Igualdad: Nuevas Proyecciones. 2020. Available online: https://www.cepal.org/es/publicaciones/45782-enfrentar-efectos-cada-vez-mayores-covid-19-reactivacion-igualdad-nuevas (accessed on 5 March 2021).
- Bonet-Moron, J.A.; Ricciulli-Marin, D.; Pérez-Valbuena, G.J.; Galvis-Aponte, L.A.; Haddad, E.A.; Araújo, I.F. Impacto Económico Regional del Covid-19 en Colombia: Un Análisis Insumo-Producto. Documentos de Trabajo Sobre Economía Regional. No. 288. Available online: https://repositorio.banrep.gov.co/handle/20.500.12134/9843 (accessed on 5 March 2021).
- Narula, R. Policy opportunities and challenges from the COVID-19 pandemic for economies with large informal sectors. J. Int. Bus. Policy 2020, 3, 302–310. [Google Scholar] [CrossRef]
- Bendavid, E.; Mulaney, B.; Sood, N.; Shah, S.; Bromley-Dulfano, R.; Lai, C.; Weissberg, Z.; Saavedra-Walker, R.; Tedrow, J.; Bogan, A.; et al. COVID-19 antibody seroprevalence in Santa Clara County, California. Int. J. Epidemiol. 2021, dyab010. [Google Scholar] [CrossRef]
- Sood, N.; Simon, P.; Ebner, P.; Eichner, D.; Reynolds, J.; Bendavid, E.; Bhattacharya, J. Seroprevalence of SARS-CoV-2-specific antibodies among adults in Los Angeles County, California, on April 10–11 2020. JAMA 2020, 323, 2425–2427. [Google Scholar] [CrossRef]
- Self, W.H.; Tenforde, M.W.; Stubblefield, W.B.; Feldstein, L.R.; Steingrub, J.S.; Shapiro, N.I.; Ginde, A.A.; Prekker, M.E.; Brown, S.M.; Peltan, I.D.; et al. Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network—13 academic medical centers, April–June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1221–1226. [Google Scholar] [CrossRef]
- Anand, S.; Montez-Rath, M.; Han, J.; Bozeman, J.; Kerschmann, R.; Beyer, P.; Parsonnet, J.; Chertow, G.M. Prevalence of SARS-CoV-2 antibodies in a large nationwide sample of patients on dialysis in the USA: A cross-sectional study. Lancet 2020, 396, 1335–1344. [Google Scholar] [CrossRef]
- Lai, C.-C.; Wang, J.-H.; Hsueh, P.-R. Population-based seroprevalence surveys of anti-SARS-CoV-2 antibody: An up-to-date review. Int. J. Infect. Dis. 2020, 101, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Idrovo, A.J.; Manrique, E.F.; Cuervo, G.M.N. Crónica de una pandemia anunciada: Caso Santander (Parte 1). Salud UIS 2020, 52, 225–238. [Google Scholar] [CrossRef]
- Hurtado-Ortíz, A.; Moreno-Montoya, J.; Prieto-Alvarado, F.E.; Idrovo, A.J. Evaluación comparativa de la vigilancia en salud pública de COVID-19 en Colombia: Primer semestre. Biomédica 2020, 40, 131–138. [Google Scholar] [CrossRef] [PubMed]
- COLOMBIA—Censo Nacional de Población y Vivienda—CNPV—2018—Información General. Available online: http://microdatos.dane.gov.co/index.php/catalog/643 (accessed on 1 March 2021).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [Green Version]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Cobertura de Geocodificación—Ayuda de ArcGIS Online. Available online: https://doc.arcgis.com/es/arcgis-online/reference/geocode-coverage.htm (accessed on 1 March 2021).
- De la Hoz-Restrepo, F.; Alvis-Zakzuk, N.J.; De la Hoz-Gomez, J.F.; De la Hoz, A.; Del Corral, L.G.; Alvis-Guzmán, N. Is Colombia an example of successful containment of the 2020 COVID-19 pandemic? A critical analysis of the epidemiological data, March to July 2020. Int. J. Infect. Dis. 2020, 99, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Validacion_Prueba_Serologica_SARS-CoV-2_IgG_Architect-Abbott. Available online: https://www.ins.gov.co/Direcciones/Investigacion/Informacionsobrepruebas/Pruebas%20serol%C3%B3gicas%20CLIA%20y%20ELISA/3-Validacion_prueba_serologica_SARS-CoV-2_IgG_Architect-Abbott.pdf (accessed on 1 March 2021).
- Sempos, C.T.; Tian, L. Adjusting Coronavirus Prevalence Estimates for Laboratory Test Kit Error. Am. J. Epidemiol. 2021, 190, 109–115. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2017; Available online: https://www.stata.com/ (accessed on 23 March 2021).
- Cave, E. COVID-19 Super-spreaders: Definitional Quandaries and Implications. Asian Bioeth. Rev. 2020, 12, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Idrovo, A.J.; Moreno-Montoya, J.; Pinzón-Flórez, C.E. Desempeño de las pruebas combinadas de IgM-IgG rápidas en la vigilancia ocupacional de COVID-19 en empresas colombianas. Biomédica 2020, 40, 139–147. [Google Scholar] [CrossRef]
- Estudio Nacional: Seroprevalencia. Available online: https://www.ins.gov.co/estudio-nacional-de-seroprevalencia/reporte.html#curso (accessed on 1 March 2021).
- Mattar, S.; Alvis-Guzman, N.; Garay, E.; Rivero, R.; García, A.; Botero, Y.; Miranda, J.; Galeano, K.; De La Hoz, F.; Martínez, C.; et al. Severe Acute Respiratory Syndrome Coronavirus 2 Seroprevalence among Adults in a Tropical City of the Caribbean Area, Colombia: Are We Much Closer to Herd Immunity than Developed Countries? Open Forum Infect. Dis. 2020, 7, ofaa550. [Google Scholar] [CrossRef] [PubMed]
- Malagón-Rojas, J.N.; Rubio, V.; Parra-Barrera, E. Seroprevalence and seroconversions for SARS-CoV-2 infections in workers at Bogota Airport, Colombia, 2020. J. Travel Med. 2021, 2021, taab006. [Google Scholar] [CrossRef]
- Ariza, B.; Torres, X.; Salgado, D.; Cepeda, M.; Restrepo, C.G.; Castellanos, J.C.; Suárez-Obando, F.; Cuellar, A.; Cardozo, C.; Ángel, J.; et al. Seroprevalence and seroconversion rates to SARS-CoV-2 in interns, residents, and medical doctors in a University Hospital in Bogotá, Colombia. Infectio 2021, 25, 145–152. [Google Scholar] [CrossRef]
- Gonzalez, J.M.; Santos-Barbosa, J.C.; Jaller, C.; Otalora, G.; Hernandez, L.J.; Guevara-Suarez, M.; Restrepo, S. Seroreactivity to SARS-CoV-2 in individuals attending a university campus in Bogotá Colombia. medRxiv 2021. [Google Scholar] [CrossRef]
- Shakiba, M.; Nazemipour, M.; Salari, A.; Mehrabian, F.; Nazari, S.S.H.; Rezvani, S.M.; Ghasempour, Z.; Heidarzadeh, A.; Mansournia, M.A. Seroprevalence of SARS-CoV-2 in Guilan Province, Iran, April 2020. Emerg. Infect. Dis. 2021, 27, 636–638. [Google Scholar] [CrossRef] [PubMed]
- Rostami, A.; Sepidarkish, M.; Leeflang, M.M.; Riahi, S.M.; Shiadeh, M.N.; Esfandyari, S.; Mokdad, A.H.; Hotez, P.J.; Gasser, R.B. SARS-CoV-2 seroprevalence worldwide: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; Pérez-Olmeda, M.; Yotti, R. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): A nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Mercado, M.; Ospina, M. Seroprevalencia de SARS-CoV-2 Durante la Epidemia en Colombia: Estudio País. Available online: https://www.ins.gov.co/BibliotecaDigital/Seroprevalencia-estudio-colombia.pdf (accessed on 1 March 2021).
- Arévalo, A.; Franco-Muñoz, C.; Duque-Beltrán, S.; Muñoz-Galindo, L.; Herrera-Sepulveda, M.; Lozano, J.M.; Salazar, L.M.; Ospina-Martinez, M.L.; Mercado-Reyes, M. ELIPSE-COL: A novel ELISA test based on rational envisioned synthetic peptides for detection of SARS-CoV-2 infection in Colombia. medRxiv 2020. [Google Scholar] [CrossRef]
- Ng, Q.X.; Liew, M.F.; Yeo, W.S. Making sense of a negative COVID-19 swab test. Quant. Imaging Med. Surg. 2020, 10, 2212–2214. [Google Scholar] [CrossRef] [PubMed]





| Variable | All | Negative | IgG+ Only | IgG/IgM+ | IgM+ Only |
|---|---|---|---|---|---|
| n | 7045 | 5738 | 677 | 434 | 196 |
| Age (years, n = 6629) * | 37.4 | 37.2 | 35.1 | 39.5 | 34.3 |
| (36.3–38.4) | (36.6–37.8) | (33.9–36.3) | (38.3–40.7) | (32.6–36.1) | |
| Sex | |||||
| Men | 2821 (40.0) | 2308 (40.3) | 264 (38.6) | 186 (43.1) | 63 (31.5) |
| Women | 4219 (59.9) | 3426 (59.6) | 412 (61.2) | 248 (56.9) | 133 (68.5) |
| Other | 5 (0.1) | 4 (0.1) | 1 (0.1) | - | - |
| Municipality | |||||
| Bucaramanga | 3347 (47.5) | 2752 (48.8) | 310 (45.7) | 202 (46.4) | 83 (42.8) |
| Floridablanca | 2226 (31.6) | 1836 (25.5) | 201 (23.0) | 123 (21.9) | 66 (26.4) |
| Girón | 628 (8.9) | 466 (11.9) | 87 (18.5) | 56 (18.6) | 19 (14.1) |
| Piedecuesta | 774 (10.9) | 633 (13.8) | 69 (12.5) | 46 (13.0) | 26 (16.5) |
| Other | 70 (0.9) | - | - | - | - |
| Socioeconomic status | |||||
| 1 (lowest) | 575 (8.2) | 412 (7.4) | 94 (13.9) | 48 (10.3) | 21 (10.5) |
| 2 | 1563 (22.2) | 1175 (20.7) | 213 (31.2) | 126 (29.1) | 49 (24.9) |
| 3 | 2442 (34.6) | 1977 (35.2) | 240 (36.4) | 154 (36.6) | 71 (37.5) |
| 4 | 1712 (24.3) | 1496 (25.6) | 102 (14.6) | 78 (17.8) | 36 (18.1) |
| 5 | 395 (5.6) | 352 (5.4) | 15 (1.9) | 17 (3.5) | 11 (4.9) |
| 6 (higher) | 320 (4.5) | 296 (4.9) | 8 (1.1) | 9 (1.9) | 7 (3.3) |
| Unknown | 38 (0.5) | 30 (0.5) | 5 (0.7) | 2 (0.4) | 1 (0.5) |
| Occupational sector | |||||
| Health | 3295 (46.8) | 2.697 (47.2) | 309 (45.6) | 183 (43.1) | 106 (55.1) |
| Public transportation | 282 (4.0) | 237 (4.1) | 25 (3.7) | 11 (2.7) | 9 (4.3) |
| Public forces (police/army) | 148 (2.1) | 114 (1.8) | 17 (2.2) | 15 (3.5) | 2 (1.0) |
| Public services | |||||
| Security | 242 (3.4) | 213 (3.7) | 19 (2.9) | 8 (1.7) | 2 (1.0) |
| Construction | 114 (1.6) | 91 (1.6) | 10 (1.6) | 6 (1.4) | 7 (3.5) |
| Food | 440 (6.2) | 343 (6.0) | 59 (8.2) | 33 (6.9) | 5 (2.2) |
| Education | 151 (2.1) | 118 (2.0) | 18 (2.4) | 13 (2.9) | 2 (1.3) |
| Grocery store tenants/informal commerce | 136 (1.9) | 120 (2.0) | 7 (1.2) | 5 (1.0) | 4 (2.2) |
| Independent worker | 194 (2.7) | 141 (2.4) | 23 (3.4) | 25 (5.7) | 5 (2.5) |
| Administrative municipal services | |||||
| Cleaning | 398 (5.6) | 309 (5.1) | 35 (5.2) | 45 (10.5) | 9 (3.8) |
| Bike delivery workers | 1095 (15.5) | 920 (15.9) | 94 (13.8) | 53 (12.2) | 28 (14.1) |
| Other | |||||
| 106 (1.5) | 79 (1.5) | 15 (2.3) | 9 (2.0) | 3 (1.4) | |
| 13 (0.2) | 9 (0.1) | 1 (0.1) | 3 (0.6) | - | |
| 422 (6.0) | 338 (6.0) | 45 (6.3) | 25 (5.2) | 14 (7.2) |
| Variable | All | Negative | IgG+ Only | IgG/IgM+ | IgM+ Only |
|---|---|---|---|---|---|
| n | 7045 | 5738 | 677 | 434 | 196 |
| Smoking | |||||
| Yes (currently) | 345 (4.9) | 302 (5.3) | 25 (3.8) | 9 (1.9) | 9 (4.3) |
| Yes (past) | 1421 (20.2) | 1.177 (20.3) | 110 (15.9) | 96 (22.1) | 38 (19.2) |
| Yes (passive) | 419 (5.9) | 341 (6.0) | 35 (5.1) | 31 (7.1) | 12 (6.6) |
| No | 4860 (69.0) | 3.918 (68.2) | 507 (75.0) | 298 (68.6) | 137 (69.7) |
| Medical conditions | |||||
| Yes | 1333 (18.9) | 1.105 (18.9) | 110 (15.7) | 83 (18.6) | 35 (17.3) |
| No | 5509 (78.2) | 4.474 (78.2) | 549 (81.3) | 332 (77.2) | 154 (79.2) |
| Do not know | 203 (2.9) | 159 (2.8) | 18 (2.8) | 19 (4.2) | 7 (3.3) |
| Contact with people with suspected or confirmed COVID-19 | |||||
| Yes | 3153 (44.8) | 2.525 (43.9) | 314 (46.4) | 223 (52.0) | 91 (45.0) |
| No | 2898 (41.1) | 2.411 (41.9) | 262 (38.4) | 144 (32.9) | 81 (42.5) |
| Do not know | 994 (14.1) | 802 (14.0) | 101 (15.1) | 67 (15.0) | 24 (12.4) |
| Symptoms related to COVID-19 since March 2020 | |||||
| Yes | 1643 (23.3) | 1.074 (18.7) | 297 (44.4) | 230 (54.0) | 42 (21.5) |
| No | 5041 (71.5) | 4.375 (76.1) | 344 (50.3) | 176 (39.7) | 146 (74.4) |
| Do not know | 361 (5.1) | 289 (5.1) | 36 (5.1) | 28 (6.1) | 8 (3.9) |
| Due to beginning of symptoms, COVID-19 diagnosis was confirmed | |||||
| Yes | 401 (5.7) | 101 (9.6) | 159 (53.9) | 130 (55.9) | 11 (27.5) |
| No | 474 (6.7) | 405 (38.2) | 25 (8.3) | 25 (11.8) | 19 (4.6) |
| No PCR | 694 (9.8) | 516 (48.5) | 101 (34.6) | 68 (30.1) | 9 (22.1) |
| Do not know | 56 (0.8) | 40 (3.5) | 8 (3.0) | 6 (2.1) | 2 (4.3) |
| Not applicable | 5420 (76.9) | ||||
| Due to beginning of symptoms, was hospitalized for COVID-19 symptoms | |||||
| Yes | 32 (0.4) | 9 (0.6) | 7 (2.4) | 15 (5.7) | 1 (1.3) |
| No | 1846 (26.2) | 1266 (99.1) | 301 (97.1) | 223 (93.5) | 26 (98.6) |
| Do not know | 4 (0.1) | 2 (0.2) | - | 2 (0.8) | - |
| Not applicable | 5420 (76.9) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colmenares-Mejía, C.C.; Serrano-Díaz, N.; Quintero-Lesmes, D.C.; Meneses, L.; Salazar Acosta, I.; Idrovo, Á.J.; Sanabria-Echeverry, D.Y.; Cordero-Rebolledo, H.; Castillo, V. Seroprevalence of SARS-CoV-2 Infection among Occupational Groups from the Bucaramanga Metropolitan Area, Colombia. Int. J. Environ. Res. Public Health 2021, 18, 4172. https://doi.org/10.3390/ijerph18084172
Colmenares-Mejía CC, Serrano-Díaz N, Quintero-Lesmes DC, Meneses L, Salazar Acosta I, Idrovo ÁJ, Sanabria-Echeverry DY, Cordero-Rebolledo H, Castillo V. Seroprevalence of SARS-CoV-2 Infection among Occupational Groups from the Bucaramanga Metropolitan Area, Colombia. International Journal of Environmental Research and Public Health. 2021; 18(8):4172. https://doi.org/10.3390/ijerph18084172
Chicago/Turabian StyleColmenares-Mejía, Claudia C., Norma Serrano-Díaz, Doris C. Quintero-Lesmes, Ligia Meneses, Isail Salazar Acosta, Álvaro J. Idrovo, Duván Y. Sanabria-Echeverry, Helmer Cordero-Rebolledo, and Víctor Castillo. 2021. "Seroprevalence of SARS-CoV-2 Infection among Occupational Groups from the Bucaramanga Metropolitan Area, Colombia" International Journal of Environmental Research and Public Health 18, no. 8: 4172. https://doi.org/10.3390/ijerph18084172
APA StyleColmenares-Mejía, C. C., Serrano-Díaz, N., Quintero-Lesmes, D. C., Meneses, L., Salazar Acosta, I., Idrovo, Á. J., Sanabria-Echeverry, D. Y., Cordero-Rebolledo, H., & Castillo, V. (2021). Seroprevalence of SARS-CoV-2 Infection among Occupational Groups from the Bucaramanga Metropolitan Area, Colombia. International Journal of Environmental Research and Public Health, 18(8), 4172. https://doi.org/10.3390/ijerph18084172






