Occupational Radiation Exposure and Validity of National Dosimetry Registry among Korean Interventional Radiologists
Abstract
:1. Introduction
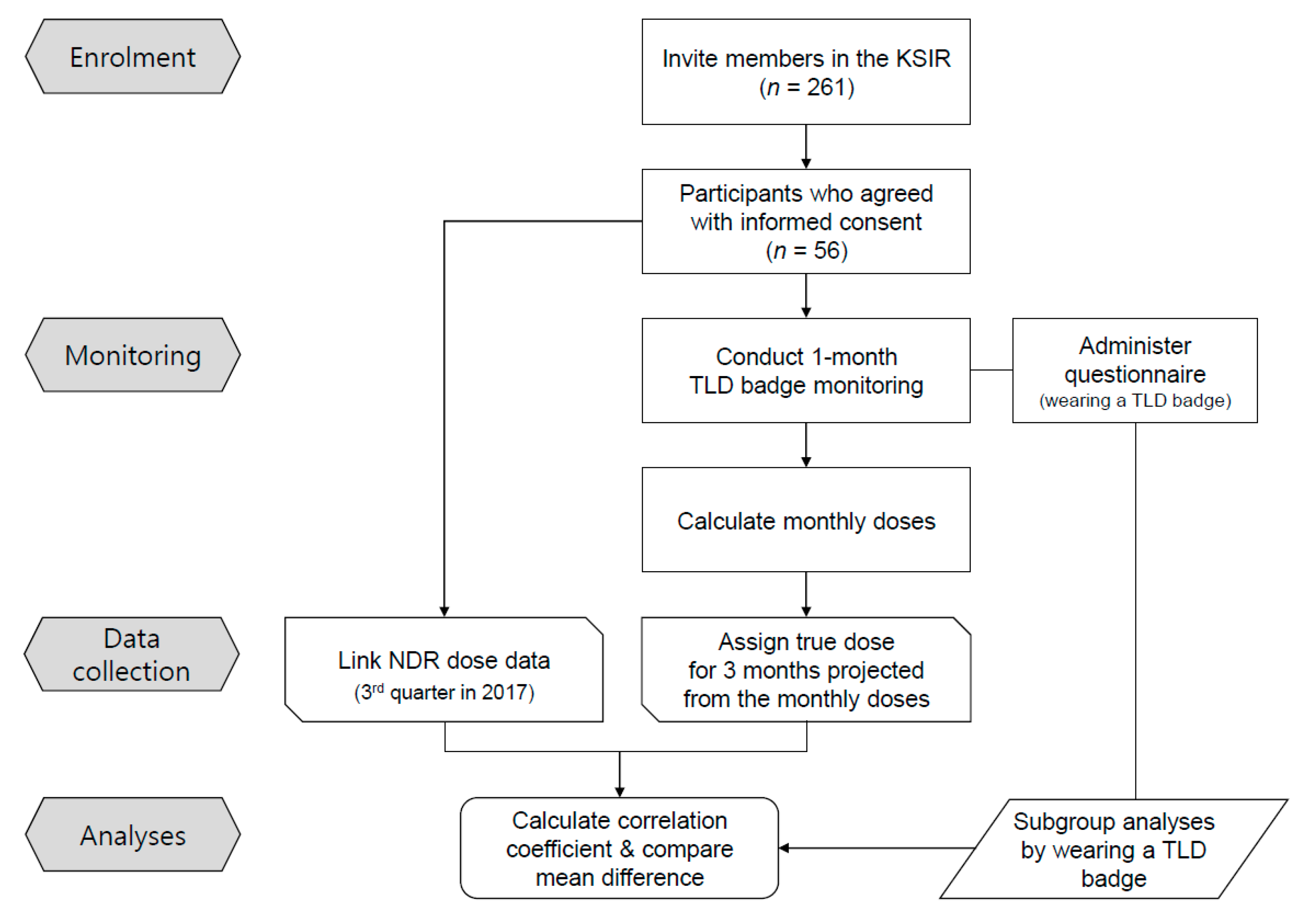
2. Materials and Methods
2.1. Study Population
2.2. Actively Monitored Personal Thermoluminescent Dosimeter Doses
2.3. Linkage with National Dose Registry Data
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ashmore, J. The design of national dose registries. Eur. J. Cancer 1997, 33, S44–S47. [Google Scholar] [CrossRef]
- National Research Council. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2; National Academies Press: Washington, DC, USA, 2006.
- Schultz, C.C.; Shaffer, S.; Fink-Bennett, D.; Winokur, K. Key Performance Indicators in the Evaluation of the Quality of Radiation Safety Programs. Health Phys. 2016, 111, S155–S165. [Google Scholar] [CrossRef] [PubMed]
- Passmore, C.N.; Kirr, M. Improvements in Radiation Monitoring Trending. Health Phys. 2017, 113, 531–534. [Google Scholar] [CrossRef]
- Zielinski, J.; Shilnikova, N.; Krewski, D. Canadian National Dose Registry of Radiation Workers: Overview of Research from 1951 Through 2007. Int. J. Occup. Med. Environ. Health 2008, 21, 269–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thierry-Chef, I.; Marshall, M.; Fix, J.J.; Bermann, F.; Gilbert, E.S.; Hacker, C.; Heinmiller, B.; Murray, W.; Pearce, M.S.; Utterback, D.; et al. The 15-Country Collaborative Study of Cancer Risk among Radiation Workers in the Nuclear Industry: Study of Errors in Dosimetry. Radiat. Res. 2007, 167, 380–395. [Google Scholar] [CrossRef] [PubMed]
- Stadtmann, H.; Figel, M.; Kamenopoulou, V.; Kluszczynski, D.; Roed, H.; Van Dijk, J. Quality control and reliability of reported doses. Radiat. Prot. Dosim. 2004, 112, 169–189. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, S.; Laurier, D.; Rage, E.; Guihenneuc, C.; Ancelet, S. Shared and unshared exposure measurement error in occupational cohort studies and their effects on statistical inference in proportional hazards models. PLoS ONE 2018, 13, e0190792. [Google Scholar] [CrossRef] [Green Version]
- Livingston, G.K.; Falk, R.B.; Schmid, E. Effect of Occupational Radiation Exposures on Chromosome Aberration Rates in Former Plutonium Workers. Radiat. Res. 2006, 166, 89–97. [Google Scholar] [CrossRef]
- Little, M.P.; Kwon, D.; Doi, K.; Simon, S.L.; Preston, D.L.; Doody, M.M.; Lee, T.; Miller, J.S.; Kampa, D.M.; Bhatti, P.; et al. Association of chromosome translocation rate with low dose occupational radiation exposures in U.S. radiologic technologists. Radiat. Res. 2014, 182, 1–17. [Google Scholar] [CrossRef] [Green Version]
- NCRP. Radiation Dose Management for Fluoroscopically-Guided Interventional Medical Procedures; NCRP Report No. 168; National Council on Radiation Protection and Measurement: Bethesda, MD, USA, 2010.
- Miller, D.L. Overview of Contemporary Interventional Fluoroscopy Procedures. Health Phys. 2008, 95, 638–644. [Google Scholar] [CrossRef]
- Kim, K.P.; Miller, D.L.; De Gonzalez, A.B.; Balter, S.; Kleinerman, R.A.; Ostroumova, E.; Simon, S.L.; Linet, M.S. Occupational Radiation Doses to Operators Performing Fluoroscopically-Guided Procedures. Health Phys. 2012, 103, 80–99. [Google Scholar] [CrossRef] [Green Version]
- Vano, E.; González, L.; Guibelalde, E.; Fernandez, J.M.; I Ten, J. Radiation exposure to medical staff in interventional and cardiac radiology. Br. J. Radiol. 1998, 71, 954–960. [Google Scholar] [CrossRef]
- Ko, S.; Kang, S.; Ha, M.; Kim, J.; Jun, J.K.; Kong, K.A.; Lee, W.J. Health Effects from Occupational Radiation Exposure among Fluoroscopy-Guided Interventional Medical Workers: A Systematic Review. J. Vasc. Interv. Radiol. 2018, 29, 353–366. [Google Scholar] [CrossRef]
- Ko, S.; Chung, H.H.; Cho, S.B.; Jin, Y.W.; Kim, K.P.; Ha, M.; Bang, Y.J.; Ha, Y.W.; Lee, W.J. Occupational radiation exposure and its health effects on interventional medical workers: Study protocol for a prospective cohort study. BMJ Open 2017, 7, e018333. [Google Scholar] [CrossRef] [Green Version]
- Korea Centers for Disease Control and Prevention. Regulations for Safety Management of Diagnostic Radiation Enforcement Regulation 1; Korea Centers for Disease Control and Prevention: Cheongju-si, Korea, 2013.
- Ministry of Health and Welfare. Rules for Safety Management of Diagnostic Radiation Emitting Generators; Health and Welfare Enforcement Ordinance 3; Ministry of Health and Welfare: Sejong-si, Korea, 1995.
- Lee, W.J.; Cha, E.S.; Ha, M.; Jin, Y.-W.; Hwang, S.-S.; Kong, K.A.; Lee, S.W.; Lee, H.K.; Lee, K.-Y.; Kim, H.J. Occupational radiation doses among diagnostic radiation workers in South Korea, 1996–2006. Radiat. Prot. Dosim. 2009, 136, 50–55. [Google Scholar] [CrossRef]
- Choi, Y.; Cha, E.S.; Bang, Y.J.; Ko, S.; Ha, M.; Lee, C.; Lee, W.J. Estimation of Organ Doses Among Diagnostic Medical Radiation Workers in South Korea. Radiat. Prot. Dosim. 2017, 179, 142–150. [Google Scholar] [CrossRef] [PubMed]
- White, E.; Armstrong, B.K.; Saracci, R. Principles of Exposure Measurement in Epidemiology: Collecting, Evaluating and Improving Measures of Disease Risk Factors; Oxford University Press: Oxford, UK, 2008. [Google Scholar]
- Krouwer, J.S. Why Bland–Altman plots should use X, not (Y+ X)/2 when X is a reference method. Stat. Med. 2008, 27, 778–780. [Google Scholar] [CrossRef] [PubMed]
- Herve, M.C. CORTESTI: Stata Module to Test Equality of Two Correlation Coefficients; Boston College Department of Economics: Boston, MA, USA, 2000. [Google Scholar]
- Kuipers, G.; Velders, X.L.; De Winter, R.J.; Reekers, J.A.; Piek, J.J. Evaluation of the Occupational Doses of Interventional Radiologists. Cardiovasc. Interv. Radiol. 2008, 31, 483–489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marx, M.V.; Niklason, L.; Mauger, E.A. Occupational Radiation Exposure to Interventional Radiologists: A Prospective Study. J. Vasc. Interv. Radiol. 1992, 3, 597–606. [Google Scholar] [CrossRef]
- Padovani, R.; Le Heron, J.; Cruz-Suarez, R.; Lefaure, C.; Rehani, M.; Czarwinski, R.; Duran, A.; Miller, D.; Sim, H.; Vano, E. International project on individual monitoring and radiation exposure levels in interventional cardiology. Radiat. Prot. Dosim. 2010, 144, 437–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xue, X.; Shore, R.E. A Method for Estimating Occupational Radiation Doses Subject to Minimum Detection Levels. Health Phys. 2003, 84, 61–71. [Google Scholar] [CrossRef] [Green Version]
- Shin, H.; Ramsay, T.; Krewski, D.; Zielinski, J.M. The effect of censoring on cancer risk estimates based on the Canadian National Dose Registry of occupational radiation exposure. J. Exp. Sci. Environ. Epidemiol. 2004, 15, 398–406. [Google Scholar] [CrossRef] [Green Version]
- Xue, X.; Kim, M.Y.; Shore, R.E. Estimation of Health Risks Associated with Occupational Radiation Exposure: Addressing Measurement Error and Minimum Detectable Exposure Level. Health Phys. 2006, 91, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Klein, L.W.; Miller, D.L.; Balter, S.; Laskey, W.; Haines, D.; Norbash, A.; Mauro, M.A.; Goldstein, J.A. Occupational health hazards in the interventional laboratory: Time for a safer environment. Heart Rhythm. 2009, 6, 439–444. [Google Scholar] [CrossRef]
- Kang, S.; Cha, E.S.; Bang, Y.J.; Na, T.W.; Lee, D.; Song, S.Y.; Lee, W.J. Radiation exposure and fluoroscopically-guided interventional procedures among orthopedic surgeons in South Korea. J. Occup. Med. Toxicol. 2020, 15, 1–9. [Google Scholar] [CrossRef]
- Buchanan, G.L.; Chieffo, A.; Mehilli, J.; Mikhail, G.W.; Mauri, F.; Presbitero, P.; Grinfeld, L.; Petronio, A.S.; Skelding, K.A.; Hoye, A.; et al. The occupational effects of interventional cardiology: Results from the WIN for Safety survey. EuroIntervention 2012, 8, 658–663. [Google Scholar] [CrossRef]
- Klein, L.W.; Tra, Y.; Garratt, K.N.; Powell, W.; Lopez-Cruz, G.; Chambers, C.; Goldstein, J.A.; Society for Cardiovascular Angiography and Interventions. Occupational health hazards of interventional cardiologists in the current decade: Results of the 2014 SCAI membership survey. Catheter. Cardiovasc. Interv. 2015, 86, 913–924. [Google Scholar] [CrossRef]
- Efstathopoulos, E.P.; Pantos, I.; Andreou, M.; Gkatzis, A.; Carinou, E.; Koukorava, C.; Kelekis, N.L.; Brountzos, E. Occupational radiation doses to the extremities and the eyes in interventional radiology and cardiology procedures. Br. J. Radiol. 2011, 84, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Compagnone, G.; On behalf of the Italian Working Group on Interventional Radiology; Padovani, R.; D’Avanzo, M.A.; Grande, S.; Campanella, F.; Rosi, A. Summary of the Italian inter-society recommendations for radiation protection optimization in interventional radiology. La Radiol. Med. 2018, 123, 378–384. [Google Scholar] [CrossRef] [PubMed]

| Characteristics 1 | Total Participants (N = 56) | Participants Who Wore a Badge for ≥75% of the Time (N = 37) | Participants Who Wore a Badge for <75% of the Time (N = 19) | p Value 2 | |||
|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | ||
| Sex | 0.696 | ||||||
| Male | 52 | (92.9) | 34 | (91.9) | 18 | (94.7) | |
| Female | 4 | (7.1) | 3 | (8.1) | 1 | (5.3) | |
| Age | 0.784 | ||||||
| <45 years | 31 | (55.4) | 20 | (54.1) | 11 | (57.9) | |
| ≥45 years | 25 | (44.6) | 17 | (45.9) | 8 | (42.1) | |
| Calendar year began working as an interventional radiologist | 0.778 | ||||||
| <2007 | 28 | (50.0) | 19 | (51.4) | 9 | (47.4) | |
| ≥2007 | 28 | (50.0) | 18 | (48.6) | 10 | (52.6) | |
| Years worked as an interventional radiologist | 0.505 | ||||||
| <10 years | 26 | (46.4) | 16 | (43.2) | 10 | (52.6) | |
| ≥10 years | 30 | (53.6) | 21 | (56.8) | 9 | (47.4) | |
| Wearing a lead apron | 0.470 | ||||||
| 100% | 55 | (100.0) | 36 | (100.0) | 19 | (100.0) | |
| <100% | 0 | (0.0) | 0 | (0.0) | 0 | (0.0) | |
| Wearing a thyroid shield | 0.229 | ||||||
| 100% | 52 | (94.5) | 35 | (97.2) | 17 | (89.5) | |
| <100% | 3 | (5.5) | 1 | (2.8) | 2 | (10.5) | |
| Using ceiling-suspended shielding | 0.957 | ||||||
| ≥75% | 20 | (36.4) | 13 | (36.1) | 7 | (36.8) | |
| <75% | 35 | (64.6) | 23 | (63.9) | 12 | (63.2) | |
| Using table-suspended shielding | 0.817 | ||||||
| ≥75% | 33 | (60.0) | 22 | (61.1) | 11 | (57.9) | |
| <75% | 22 | (40.0) | 14 | (38.9) | 8 | (42.1) | |
| Total Participants (n = 56) | Participants Who Wore a Badgefor ≥75% of the Time (n = 37) | Participants Who Wore a Badge for <75% of the Time (n = 19) | p Value 1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | (SD) | Median | (Range) | Mean | (SD) | Median | (Range) | Mean | (SD) | Median | (Range) | ||
| Quarterly doses (mSv) | |||||||||||||
| Actively monitored doses | 1.48 | (2.61) | 0.74 | (0.005–15.07) | 0.95 | (1.56) | 0.47 | (0.005–8.61) | 2.52 | (3.78) | 1.27 | (0.005–15.07) | 0.032 |
| NDR doses | 0.50 | (0.65) | 0.19 | (0.005–2.56) | 0.69 | (0.65) | 0.65 | (0.005–2.56) | 0.13 | (0.47) | 0.005 | (0.005–2.07) | 0.002 |
| Validation analyses | |||||||||||||
| Spearman’s correlation Coefficient (p value) | 0.058 (0.672) | 0.425 (0.009) | −0.210 (0.388) | ||||||||||
| ICC 2 (p value) | 0.049 (0.419) | 0.451 (0.037) | 0.017 (0.048) | ||||||||||
| Dose difference (mean ± SD) | 0.98 ± 2.65 | 0.26 ± 1.42 | 2.39 ± 3.78 | ||||||||||
| Paired t test | 0.008 | 0.272 | 0.013 | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ko, S.; Kim, K.P.; Cho, S.B.; Bang, Y.J.; Ha, Y.W.; Lee, W.J. Occupational Radiation Exposure and Validity of National Dosimetry Registry among Korean Interventional Radiologists. Int. J. Environ. Res. Public Health 2021, 18, 4195. https://doi.org/10.3390/ijerph18084195
Ko S, Kim KP, Cho SB, Bang YJ, Ha YW, Lee WJ. Occupational Radiation Exposure and Validity of National Dosimetry Registry among Korean Interventional Radiologists. International Journal of Environmental Research and Public Health. 2021; 18(8):4195. https://doi.org/10.3390/ijerph18084195
Chicago/Turabian StyleKo, Seulki, Kwang Pyo Kim, Sung Bum Cho, Ye Jin Bang, Yae Won Ha, and Won Jin Lee. 2021. "Occupational Radiation Exposure and Validity of National Dosimetry Registry among Korean Interventional Radiologists" International Journal of Environmental Research and Public Health 18, no. 8: 4195. https://doi.org/10.3390/ijerph18084195





