Insomnia among Prison Officers and Its Relationship with Occupational Burnout: The Role of Coping with Stress in Polish and Indonesian Samples
Abstract
:1. Introduction
1.1. Occupational Burnout and Insomnia
1.2. Prison Service: Characteristics of Work in the Polish and Indonesian Penitentiary Systems
- -
- The role of strategies of coping.
- -
- The role of organizational factors, that is, penitentiary unit type (open, closed, semi-open) and single- or multi-shift work.
- -
- The role of individual factors such as gender and age.
- -
- What is the intensity of occupational burnout among POs? Are there differences between the Polish and Indonesian samples?
- -
- Do coping strategies, organizational factors, and individual factors differentiate insomnia levels?
- -
- Are there differences between the samples?
- -
- Which of the considered variables are predictors of insomnia intensity among POs in each sample?
2. Materials and Methods
2.1. Ethics Approval
- (1)
- The Athens Insomnia Scale (AIS) by Soldatos, Dikeos, and Paparrigopoulos. This is an eight-item scale measuring insomnia symptoms [83]. The scale is a self-report method comprising eight items related to various symptoms of insomnia. It is most frequently used for diagnostic purposes as well as to measure therapeutic effectiveness. The AIS has high reliability and validity. Each item is rated on a four-point Likert-type scale, where 0 denotes a lack of a given symptom and 3—its significant intensity. The assessed symptoms are: sleep induction, awakenings during the night, waking up in the morning, total sleep duration, sleep quality, wellbeing during the day, mental and physical functioning capacity the next day, and sleepiness during the day. The total score is between 0 and 24, where higher scores denote lower sleep quality. The original criteria consider scores above six as reliable indicators of early symptoms of insomnia [83,84]. The higher the scores, the more severe the symptoms [85,86]. The internal reliability of the AIS was 0.88 in the Polish sample and 0.74 in the Indonesian sample.
- (2)
- The Oldenburg Burnout Inventory (OLBI) by Demerouti and Bakker [87]. This questionnaire represents a two-factor model of occupational burnout. It consists of 16 items forming two subscales:
- (a)
- Exhaustion due to intense physical, mental, and emotional effort, the effect of chronic workplace stress related to job demands;
- (b)
- Distancing from work (described as disengagement from work by Demerouti and Bakker), its purpose, and its character [88].
- (3)
- Coping Orientation to Problems Experienced (COPE) by Carver, Scheier, and Weintraub [91].
- The engagement coping style: acceptance, positive reinterpretation, active coping, planning, restraint coping, and suppression of competing activities.
- The disengagement coping style: religion, mental disengagement, behavioral disengagement, and denial.
- The help-seeking style: seeking instrumental support, seeking emotional support, and venting of emotions.
2.2. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Insomnia among Prison Officers: Differences between the Countries
3.3. The Relationship between Coping Styles and Insomnia Levels
3.4. Organizational Factors and Insomnia Levels
3.5. Sociodemographic Factors and Insomnia Levels
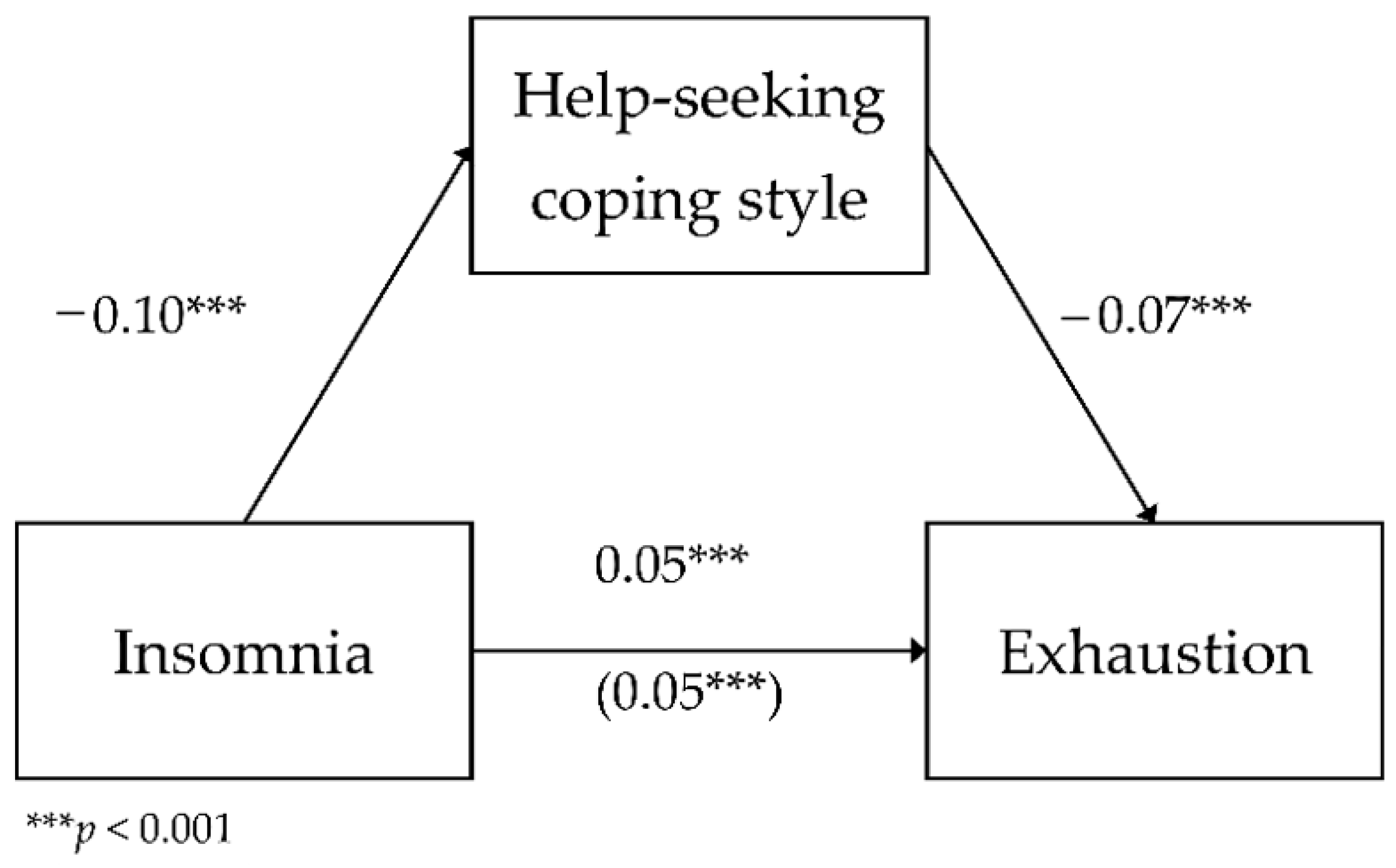
3.6. The Mediating Role of Coping Styles in the Relationship between Insomnia and Occupational Burnout
3.7. Predictors of Insomnia
4. Discussion
5. Conclusions
- -
- Scientific advances allow occupational burnout to be linked with sleep disorders. Experiences of stress are considered to factor into the etiology of these two phenomena. Nevertheless, data on the role of coping strategies in the relationship between occupational burnout and insomnia have been scarce thus far.
- -
- Insomnia among Polish and Indonesian prison officers has not been examined thus far. The current study shows that its incidence is higher in Poland, while over 1/4 of the Indonesian sample reported results indicating early insomnia symptoms. Sleep disorders were revealed to influence the development of occupational burnout.
- -
- The mediating role of such coping strategies as help-seeking and engagement in the relationship between insomnia and occupational burnout dimensions has been confirmed for the total sample. Both in the total sample, as well as in the Polish sample, help-seeking was the only coping strategy predicting insomnia.
- -
- Age, gender, and multi-shift work differences exist between the current comparison of the two countries and the results of previous studies.
- -
- The current study should be followed up with further studies, which should include more precise measurement tools for sleep difficulties. This is because sleep disorders can significantly impact the work functioning of penitentiary personnel.
6. Strengths, Limitations, and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferreira, A. Prevalence and consequences of sleep disorders among traffic agents: A case study. Cienc. Trab. 2015, 17, 207–211. [Google Scholar] [CrossRef] [Green Version]
- Piotrowski, A. Self-evaulation of personal physical health, accidents while performing duty and preventive treatment of stress in Prison Service. Med. Pr. 2018, 69, 425–438. [Google Scholar] [CrossRef]
- Doi, Y. An epidemiologic review of occupational sleep research among Japanese workers. Ind. Health. 2005, 43, 3–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dinges, D.F.; Pack, F.; Williams, K.; Gillen, K.A.; Powell, J.W.; Ott, G.E.; Aptowicz, C.; Pack, A.I. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. Sleep 1997, 20, 267–277. [Google Scholar] [PubMed]
- Espie, C. Insomnia: Conceptual issues in the development, persistence and treatment of sleep disorder in adults. Annu. Rev. Psychol. 2002, 53, 215–243. [Google Scholar] [CrossRef] [Green Version]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M.; Kim, K.; Shibui, K.; Kamei, Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000, 97, 165–172. [Google Scholar] [CrossRef]
- Farrahi Moghaddam, J.; Nakhaee, N.; Sheibani, V.; Garrusi, B.; Amirkafi, A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep Breath 2012, 16, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Sateia, M.J.; Doghramji, K.; Hauri, P.J.; Morin, C.M. Evaluation of chronic insomnia. An American academy of sleep medicine review. Sleep 2000, 15, 243–308. [Google Scholar]
- Drake, C.L.; Vargas, I.; Roth, T.; Friedman, N.P. Quantitative measures of nocturnal insomnia symptoms predict greater deficits across multiple daytime impairment domains. Behav. Sleep Med. 2014, 12, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Precipitating factors of insomnia. Behav. Sleep Med. 2004, 2, 50–62. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Knutsson, A.; Westerholm, P.; Theorell, T.; Alfredsson, L.; Kecklund, G. Sleep disturbances, work stress and work hours: A cross-sectional study. J. Psychosom. Res. 2002, 53, 741–748. [Google Scholar] [CrossRef]
- Nakata, A.; Haratani, T.; Takahashi, M.; Kawakami, N.; Arito, H.; Kobayashi, F.; Araki, S. Job stress, social support, and prevalence of insomnia in a population of Japanese daytime workers. Soc. Sci. Med. 2004, 59, 1719–1730. [Google Scholar] [CrossRef] [PubMed]
- Ballenger, J.C.; Davidson, J.R.; Lecrubier, Y.; Nutt, D.; Foa, E.B.; Kessler, R.C.; McFarlane, A.C. Consensus statement on posttraumatic stress disorder from the International Consensus Group on Depression and Anxiety. Clin. Psychiatry 2000, 61, 60–66. [Google Scholar]
- Sripada, R.K.; Hoff, R.; Pfeiffer, P.N.; Ganoczy, D.; Blow, F.C.; Bohnert, K.M. Latent classes of PTSD symptoms in veterans undergoing residential PTSD treatment. Psychol. Serv. 2020, 17, 84–92. [Google Scholar] [CrossRef]
- Mellman, T.A. Psychobiology of sleep disturbances in posttraumatic stress disorder. Ann. N. Y. Acad. Sci. 1997, 21, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Linton, S.J. Does work stress predict insomnia? A prospective study. Br. J. Health Psychol. 2004, 9, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Reeth, O.; Weibel, L.; Spiegel, K.; Leproult, R.; Dugovic, C.; Maccad, S. Interactions between stress and sleep: From basic research to clinical situations. Sleep Med. Rev. 2000, 4, 201–219. [Google Scholar] [CrossRef]
- Monk, T.H. Shift work. In Understanding Sleep: The Evaluation and Treatment of Sleep Disorders; Pressman, M.R., Orr, W.C., Eds.; American Psychological Association: Washington, DC, USA, 1997; pp. 249–266. [Google Scholar]
- Chatterjee, K.; Ambekar, P. Study of insomnia in rotating shift-workers. Ind Psychiatry J. 2017, 26, 82–85. [Google Scholar] [CrossRef]
- Healey, E.S.; Kales, A.; Monroe, L.J.; Bixler, E.O.; Chamberlin, K.; Soldatos, C.R. Onset of insomnia: Role of life-stress events. Psychosom Med. 1981, 43, 439–451. [Google Scholar] [CrossRef] [PubMed]
- Sallinen, M.; Kecklund, G. Shift work, sleep, and sleepiness-differences between shift schedules and systems. Scand. J. Work Environ. Health 2010, 36, 121–133. [Google Scholar] [CrossRef]
- Tsuno, N.; Besset, A.; Ritchie, K. Sleep and depression. J. Clin. Psychiatry 2005, 66, 1254–1269. [Google Scholar] [CrossRef]
- Almeida, O.P.; Pfaff, J.J. Sleep complaints among older general practice patients: Association with depression. Br. J. Gen. Pract. 2005, 55, 864–866. [Google Scholar] [PubMed]
- Silva-Costa, A.; Araú, M.M.D.; Nagai, R.; Fischer, F.M. Environmental and organizational conditions for napping during night work: A qualitative study among nursing professionals. Sleep Scien. 2010, 3, 11–15. [Google Scholar]
- Bazrafshan, M.R.; Moravveji, F.; Soleymaninejad, N.; Zare, F.; Rahimpoor, R.; Zolghadr, R. Prevalence and effects of sleep disorders among shift-working nurse. Ann. Trop. Med. Public Health 2018, 11, 13–18. [Google Scholar] [CrossRef]
- Tang, L.; Liu, W.; Yang, Y.; Han, W.; Li, K. Relationship between sleep and cognitive function in patients with heart failure: A systematic review. J. Psychosom. Res. 2020, 130, 109913. [Google Scholar] [CrossRef] [PubMed]
- Seidler, A.; Thinschmidt, M.; Deckert, S.; Then, F.; Hegewald, J.; Nieuwenhuijsen, K.; Riedel-Heller, S.G. The role of psychosocial working conditions on burnout and its core component emotional exhaustion-a systematic review. J. Occup. Med. Toxicol. 2014, 9, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leiter, M.P.; Maslach, C. Burnout: 35 years of research and practice. Career. Dev. Int. 2009, 14, 204–220. [Google Scholar] [CrossRef] [Green Version]
- Maslach, C. Understanding burnout: Definitional issues in analyzing a complex phenomenon. In Job Stress and Burnout; Paine, W.S., Ed.; Sage: Los Angeles, CA, USA, 1982; pp. 29–40. [Google Scholar]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [Green Version]
- Armon, G.; Shirom, A.; Shapira, I.; Melamed, S. On the nature of burnout-insomnia relationships: A prospective study of employed adults. J. Psychosom. Res. 2008, 65, 5–12. [Google Scholar] [CrossRef]
- Weber, A.; Jaekel-Reinhard, A. Burnout syndrome: A disease of modern societies? Occup. Med. 2000, 50, 512–517. [Google Scholar] [CrossRef] [Green Version]
- Grossi, G.; Perski, A.; Evengård, B.; Blomkvist, V.; Orth-Gomér, K. Physiological correlates of burnout among women. J. Psychosom. Res. 2003, 55, 309–316. [Google Scholar] [CrossRef]
- Ekstedt, M.; Söderström, M.; Akerstedt, T.; Nilsson, J.; Søndergaard, H.P.; Aleksander, P. Disturbed sleep and fatigue in occupational burnout. Scand. J. Work Environ. Health 2006, 32, 121–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perski, A.; Grossi, G.; Evengård, B.; Blomkvist, V.; Ylbar, B.; Orth-Gomér, K. Emotional exhaustion common among women in the public sector. Läkartidningen 2002, 99, 2047–2052. [Google Scholar]
- Merey, Z.; Boysan, M.; Ateş, C. Sleep quality and burnout syndrome among teaching staff. J. Crisis 2008, 16, 33–41. [Google Scholar]
- Metlaine, A.; Sauvet, F.; Gomez-Merino, D.; Elbaz, M.; Delafosse, J.Y.; Leger, D.; Chennaoui, M. Association between insomnia symptoms, job strain and burnout syndrome: A cross-sectional survey of 1300 financial workers. BMJ Open 2017, 7, e012816. [Google Scholar] [CrossRef] [Green Version]
- Jansson-Fröjmark, M.; Lindblom, K. Is there a bidirectional link between insomnia and burnout? A prospective study in the Swedish workforce. Int. J. Behav. Med. 2010, 17, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Ji, J.; Kao, D. Burnout and physical health among social workers: A three-year longitudinal study. Soc. Work 2011, 56, 258–268. [Google Scholar] [CrossRef]
- Imai, H.; Nakao, H.; Tsuchiya, M.; Kuroda, Y.; Katoh, T. Burnout and work environments of public health nurses involved in mental health care. Occup. Environ. Med. 2004, 61, 764–768. [Google Scholar] [CrossRef]
- Mojsa-Kaja, J.; Golonka, K.; Marek, T. Job burnout and engagement among teachers—worklife areas and personality traits as predictors of relationships with work. Int. J. Occup. Med. Environ. Health 2015, 28, 102–119. [Google Scholar] [CrossRef]
- Kim, H.J.; Shin, K.H.; Umbreit, W.T. Hotel job burnout: The role of personality characteristics. Int. J. Hosp. Manage. 2007, 26, 421–434. [Google Scholar] [CrossRef]
- Stewart, N.H.; Arora, V.M. The Impact of Sleep and Circadian Disorders on Physician Burnout. Chest 2019, 156, 1022–1030. [Google Scholar] [CrossRef]
- Finney, C.; Stergiopoulos, E.; Hensel, J.; Bonato, S.; Dewa, C.S. Organizational stressors associated with job stress and burnout in correctional officers: A systematic review. BMC Pub. Health 2013, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erenkfeit, K.; Dudzińska, L.; Indyk, A. Work environment impact on professional burnout. Med. Środ. 2012, 15, 121–128. (In Polish) [Google Scholar]
- Cullen, F.T.; Link, B.G.; Cullen, J.B.; Wolfe, N.T. How Satisfying is Prison Work? J. Offender Couns. Services Rehab. 1990, 14, 89–108. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Peeters, M.C.W. Job Stress and Burnout Among Correctional Officers: A Literature Review. Int. J. Stress Manage. 2000, 7, 19–48. [Google Scholar] [CrossRef]
- Lourel, M.; Gana, K.; Prud’homme, V.; Cercle, A. [Burn-out among personnel of prisons: Karasek’s job demand-control model]. Encephale 2004, 30, 557–563. (In French) [Google Scholar] [CrossRef]
- Kinman, G.; Clements, A.J.; Hart, J. When Are You Coming Back? Presenteeism in U.K. Prison Officers. Prison J. 2019, 99, 363–383. [Google Scholar] [CrossRef] [Green Version]
- Botek, M. Job satisfaction and turnover intentions of correctional officers in a Prague prison. J. East. Europ. Manag. Stud. 2019, 24, 545–565. [Google Scholar] [CrossRef]
- Bourbonnais, R.; Jauvin, N.; Dussault, J.; Vézina, M. Psychosocial work environment, interpersonal violence at work and mental health among correctional officers. Int. J. Law Psychiatry 2007, 30, 355–368. [Google Scholar] [CrossRef]
- Testoni, I.; Nencioni, I.; Ronconi, L.; Alemanno, F.; Zamperini, A. Burnout, Reasons for Living and Dehumanisation among Italian Penitentiary Police Officers. Int. J. Environ. Res. Public Health. 2020, 17, 3117. [Google Scholar] [CrossRef]
- Bezerra, C.M.; Assis, S.G.; Constantino, P. Psychological distress and work stress in correctional officers: A literature review. Sofrimento psíquico e estresse no trabalho de agentes penitenciários: Uma revisão da literatura. Cien Saude Colet. 2016, 21, 2135–2146. [Google Scholar] [CrossRef] [Green Version]
- Lambert, E.; Hogan, N.L.; Altheimer, I. The association between work-family conflict and job burnout among correctional staff: A preliminary study. Am. J. Crim. Justice 2010, 35, 37–55. [Google Scholar] [CrossRef]
- Lambert, E.G.; Hogan, N.L.; Altheimer, I. An exploratory examination of the consequences of burnout in terms of life satisfaction, turnover intent, and absenteeism among private correctional staff. Prison J. 2010, 90, 94–114. [Google Scholar] [CrossRef]
- Silva, A.Z.; Mota, R.M.S.; Macena, R.H.M.; Neto, R.D.J.P.; Ferreira, M.J.M.; Araújo, P.F.; Magalhães, T.M.; Seal, M.D.W.; Kendall, C.; Kerr, L.R.F.S. Prevalence of hypertension and associated factors in female prison correctional officers in a national sample in Brazil. J. Occup. Health 2020, 62, e12163. [Google Scholar] [CrossRef]
- Goldberg, P.; David, S.; Landre, M.F.; Goldberg, M.; Dassa, S.; Fuhrer, R. Work conditions and mental health among prison staff in France. Scand. J. Work Environ. Health 1996, 22, 45–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walker, E.J.; Jackson, C.A.; Egan, H.H.; Tonkin, M. Workability and mental wellbeing among therapeutic prison officers. Occup. Med. 2015, 65, 549–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bringas-Molleda, C.; Fernández-Muñiz, A.; Álvarez-Fresno, E.; Martínez-Cordero, A.; Rodríguez-Díaz, F.J. Influence of burnout on the health of prison workers. Rev. Esp. Sanid. Penit. 2015, 17, 67–73. [Google Scholar] [CrossRef] [Green Version]
- Korczyńska, J. Temperamental risk factor of burnout on the example of prison service employees. In Personality and Extreme Stress; Strelau, J., Ed.; Gdańskie Wydawnictwo Psychologiczne: Gdańsk, Poland, 2004; pp. 317–342. (In Polish) [Google Scholar]
- Lambert, E.G.; Minor, K.I.; Wells, J.B.; Hogan, N.L. Leave Your Job at Work: The Possible Antecedents of Work–Family Conflict Among Correctional Staff. Prison J. 2015, 95, 114–134. [Google Scholar] [CrossRef]
- Paleksić, V.M. Professional Stressors in Prison Officers: A Cross-Sectional Study. Paleksić. Scr. Med. 2020; 51, 166–173. [Google Scholar] [CrossRef]
- Jin, X.; Sun, I.Y.; Jiang, S.; Wang, Y.; Wen, S. The Impact of Job Characteristics on Burnout Among Chinese Correctional Workers. Int. J. Offender Ther. Comp. Criminol. 2018, 62, 551–570. [Google Scholar] [CrossRef]
- Jaegers, L.A.; Matthieu, M.M.; Werth, P.; Ahmad, S.O.; Barnidge, E.; Vaughn, M.G. Stressed Out: Predictors of Depression Among Jail Officers and Deputies. Prison J. 2020, 100, 240–261. [Google Scholar] [CrossRef]
- Campos, J.A.; Schneider, V.; Bonafé, F.S.; Maroco, J. Burnout Syndrome and alcohol consumption in prison employees. Bras. J. Epidemiol. 2016, 19, 205–216. [Google Scholar] [CrossRef]
- Lavigne, E.; Bourbonnais, R. Psychosocial work environment, interpersonal violence at work and psychotropic drug use among correctional officers. Int. J. Law Psychiatry 2010, 33, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Badru, O.A.; Ogunlesi, A.O.; Ogunwale, A.; Abdulmalik, J.O.; Yusuf, O.B. Prevalence of generalized anxiety disorder and major depression among correctional officers in a Nigerian prison. J. Forensic Psychiatry Psychol. 2018, 29, 509–526. [Google Scholar] [CrossRef]
- Turnovska, T.; Dimova, R.; Tilov, B.; Bakova, D.; Harizanova, S. Coping strategies and burn out syndrome. In New Model of Burnout Syndrome: Toward Early Diagnosis and Prevention; Stojanov, D., Ed.; River Publishers: Aalborg, Denmark, 2014; pp. 161–170. [Google Scholar]
- Cieślak, R.; Korczyńska, J.; Strelau, J.; Kaczmarek, M. Burnout predictors among prison officers: The moderating effect of temperamental endurance. Pers. Individ. Dif. 2008, 45, 666–672. [Google Scholar] [CrossRef]
- Dollard, M.F.; Winefield, A.H. A test of the demand-control/support model of work stress in correctional officers. J. Occup. Health Psych. 1998, 3, 243–264. [Google Scholar] [CrossRef]
- Tarling, R.; Dennis, R. Socio-Economic Determinants of Crime Rates: Modelling Local Area Police-Recorded Crime. Howard J. Crim. Justice 2016, 55, 207–225. [Google Scholar] [CrossRef]
- The Economist Intelligence Unit. Democracy Index 2021. In Sickness and in Health? Available online: https://pages.eiu.com/rs/753-RIQ-438/images/democracy-index-2020.pdf?mkt_tok=NzUzLVJJUS00MzgAAAF76GGaDaVYg-6wdWCs4pH92eTapmkx3zIQowzgyMiLbegflEd4DVCFbpwc62iBR6llXVZvrKcO8b-tVTPApA9jmu9zg8eFIYwKqp3i6FY9FwoxZA (accessed on 22 March 2021).
- United Nations Development Programme. Human Development Data Center. Available online: http://hdr.undp.org/en/data (accessed on 27 January 2021).
- World Prison Brief Data, Poland. Institute for Crime & Justice Policy Research, Birkbeck, London. Available online: https://www.prisonstudies.org/country/poland (accessed on 27 January 2021).
- Prihatsanti, U.; Ika, Z.R.; Anggun, R.P. Reducing correctional officer work stress through cope technique. J. Psikol. 2013, 40, 159–168. [Google Scholar] [CrossRef]
- World Prison Brief Data, Indonesia; Institute for Crime & Justice Policy Research: Birkbeck, UK. Available online: https://www.prisonstudies.org/country/indonesia (accessed on 10 January 2021).
- Anggara, Z.A. Strategies to Reduce Overcrowding in Indonesia: Causes, Impacts, and Solutions; Institute for Criminal Justice Reform: Jakarta, Indonesia, 2018; pp. 59–60. [Google Scholar]
- Pomiankiewicz, J. Stress and burnout of Prison Service officers-conditions, symptoms, consequences-outline of the problem. Przegląd Więzien. Pol. 2010, 67–68, 47–60. (In Polish) [Google Scholar]
- Piotrowski, A. Media image of the Prison Service. Przegląd Więzien. Pol. 2010, 67–68, 85–93. (In Polish) [Google Scholar]
- Nowicki, Z.; Grabowski, K.; Cubała, W.J.; Nowicka-Sauer, K.; Zdrojewski, T.; Rutkowski, M.; Bandosz, P. Prevalence of self-reported insomnia in general population of Poland. Psychiatr. Pol. 2016, 50, 165–173. [Google Scholar] [CrossRef]
- Rahman, L.H.; Maurits, L.S.; Susetyowati, S. Sleep disturbances and central risk of obesity in adult males in Indonesia (an analysis of data from the Indonesian Family Life Survey / IFLS 5). BKM J. Com. Med. Pub. Health 2019, 35, 217–224. [Google Scholar] [CrossRef]
- Wulandari, I.; Adiputra, L.M.I.S.H. Relationship of sleep disturbances and fatigue in the night shift system for 24-hour minimarket employees in denpasar city. Indon. J. Ergo. 2015, 1, 51–60. [Google Scholar]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. The diagnostic validity of the Athens Insomnia Scale. J. Psychosom. Res. 2003, 55, 263–267. [Google Scholar] [CrossRef]
- Fornal-Pawłowska, M.; Wołyńczyk-Gmaj, D.; Szelenberger, W. Validation of the Polish version of the Athens Insomnia Scale. Psychiatr Pol. 2011, 45, 211–221. (In Polish) [Google Scholar]
- Bayuaji, H.; Nataprawira, H.M.N.; Sastramihardja, H.S. The Correlation of Serum Total Testosterone, Sex Hormone Binding Globulin and Free Androgen Index with Athens Insomnia Scale Score in Polycystic Ovary Syndrome. Indones. Biomed. J. 2018, 10, 46–50. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B. The Oldenburg Burnout Inventory: A good alternative to measure burnout and engagement. In Stress and Burnout in Health Care; Halbesleben, J., Ed.; Nova Sciences: Hauppage, NY, USA, 2008; pp. 65–78. [Google Scholar]
- Demerouti, E.; Mostert, K.; Bakker, A.B. Burnout and work engagement: A thorough investigation of the independency of both constructs. J. Occup. Health. Psychol. 2010, 15, 209–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baka, Ł.; Basińska, B.A. Psychometric properties of the Polish version of the Oldenburg Burnout Inventory (OLBI). Med. Pracy 2016, 67, 29–41. [Google Scholar] [CrossRef]
- Santoso, P.N.; Hartono, B. Pengaruh Job Demand-Resources Terhadap Burnout Pada Manajer Proyek Indonesia; Seminarnasional Teknik Industri Universitas Gadjah Mada: Yogyakarta, Indonesia, 2017. [Google Scholar]
- Carver, C.S.; Scheier, M.F.; Weintraub, J.K. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Juczyński, Z.; Ogińska-Bulik, N. Tools for Measuring Stress and Coping with Stress; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2009; pp. 24–44. [Google Scholar]
- Syafitri, A. Sources of stress and coping behavior Young adult individuals in dating relationships. J. Sains Psikol. 2009, 1, 1–14. [Google Scholar]
- Suhendra, D.S.; Development of Coping Stress Measurement Tool For High School Students. Undergraduate Thesis not Published. Faculty of Psychology. Tarumanegara University. Available online: http://repository.untar.ac.id/10150/1/Skripsi.pdf (accessed on 25 March 2021).
- Santoso, S.L.; Positive Youth Development Based Guidance Basic Services To Develop Stress Coping Skills In Adolescents. Thesis not Published. Guidance and Counseling Department. Indonesian Education University. Available online: http://repository.upi.edu/id/eprint/37443 (accessed on 25 March 2021).
- Carver, C.S. COPE (Complete Version). College of Arts and Sciences. The Department of Psychology. University of Miami. Available online: https://local.psy.miami.edu/faculty/ccarver/sclCOPEF.phtml (accessed on 23 March 2021).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017; pp. 120–141. [Google Scholar]
- Gaskin, J.; Lim, J. Multigroup Analysis; AMOS Plugin: Provo, UT, USA, 2018; pp. 1–5. [Google Scholar]
- Ogeil, R.P.; Rajaratnam, S.M.; Lockley, S.W.; O’Brien, C.S.; Sullivan, J.P.; Qadri, S.; Lubman, D.I.; Czeisler, C.A.; Barger, L.K. Symptoms consistent with shift work disorder are common across groups of first responders. Sleep 2017, 40, 255–256. [Google Scholar] [CrossRef]
- El-Solh, A.A.; Riaz, U.; Roberts, J. Sleep Disorders in Patients With Posttraumatic Stress Disorder. Chest 2018, 154, 427–439. [Google Scholar] [CrossRef] [PubMed]
- Ballesio, A.; Cerolini, S.; Ferlazzo, F.; Cellini, N.; Lombardo, C. The effects of one night of partial sleep deprivation on executive functions in individuals reporting chronic insomnia and good sleepers. J. Behav. Ther. Exp. Psychiatry 2018, 60, 42–45. [Google Scholar] [CrossRef]
- Wąsiewicz, P.; Skalski, M.; Fornal-Pawlowska, M. Chronic insomnia cases detection with a help of Athens Insomnia Scale and SF-36 health survey. Phot. App. Astron. Com. Indu. High.-Energy Physics Exper. 2011, 8008, 80081K. [Google Scholar] [CrossRef]
- Wolińska, W.; Tatol, P.; Zdziarski, K.; Karpeta-Pawlak, I.E.; Mroczek, B. Occurrence of insomnia and daytime somnolence among professional drivers. Fam. Med. Prim. Care. Rev. 2017, 19, 277–282. [Google Scholar] [CrossRef]
- Zdanowicz, T.; Turowski, K.; Celej-Szuster, J.; Lorencowicz, R.; Przychodzka, E. Insomnia, Sleepiness, and Fatigue Among Polish Nurses. Workplace Health Saf. 2020, 68, 272–278. [Google Scholar] [CrossRef]
- Sun, J.L.; Chiou, J.F.; Lin, C.C. Validation of the Taiwanese version of the Athens Insomnia Scale and assessment of insomnia in Taiwanese cancer patients. J. Pain. Symptom. Manage. 2011, 41, 904–914. [Google Scholar] [CrossRef] [PubMed]
- Peltzer, K.; Pengpid, S. Prevalence, social and health correlates of insomnia among persons 15 years and older in Indonesia. Psychol. Health Med. 2019, 24, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Young, T.B. Epidemiology of daytime sleepiness: Definitions, symptomatology, and prevalence. J. Clin. Psychiatry 2004, 65, 12–16. [Google Scholar]
- Dewa, L.H.; Hassan, L.; Shaw, J.J.; Senior, J. Trouble sleeping inside: A cross-sectional study of the prevalence and associated risk factors of insomnia in adult prison populations in England. Sleep Med. 2017, 32, 129–136. [Google Scholar] [CrossRef]
- Zhang, B.; Wing, Y.K. Sex differences in insomnia: A meta-analysis. Sleep 2006, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.S.; Jeon, Y.; Ma, J.; Choi, Y.; Ban, S.; Lee, S.; Lee, B.; Im, J.J.; Yoon, S.; Kim, J.E.; et al. Validation of the Athens Insomnia Scale for screening insomnia in South Korean firefighters and rescue workers. Qual. Life Res. 2015, 24, 2391–2395. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Smirne, S. Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med. 2002, 3, 115–120. [Google Scholar] [CrossRef]
- Metlaine, A.; Sauvet, F.; Gomez-Merino, D.; Boucher, T.; Elbaz, M.; Delafosse, J.Y.; Leger, D.; Chennaoui, M. Sleep and biological parameters in professional burnout: A psychophysiological characterization. PLoS ONE. 2018, 13, e0190607. [Google Scholar] [CrossRef] [Green Version]
- Ancoli-Israel, S.; Roth, T. Characteristics of insomnia in the United States: Results of the 1991 National Sleep Foundation Survey. Sleep 1999, 22, 347–353. [Google Scholar]
- Średniawa, A.; Drwiła, D.; Krotos, A.; Wojtaś, D.; Kostecka, N.; Tomasik, T. Insomnia and the level of stress among students in Krakow, Poland. Trends Psychiatry Psychother. 2019, 41, 60–68. [Google Scholar] [CrossRef] [Green Version]
- Morin, C.M.; Rodrigue, S.; Ivers, H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom. Med. 2003, 65, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Cooper, C.; Cartwright, S.; Donald, I.; Taylor, P.; Millet, C. The experience of work-related stress across occupations. J. Manag. Psychol. 2005, 20, 178–187. [Google Scholar] [CrossRef] [Green Version]
- Agustin, D. Factors that influence sleep quality for shift workers at Krakatau Tirta Industri Cilegon (University of Indonesia). Available online: http://lib.ui.ac.id/file?file=digital/20313608-S43780 (accessed on 9 December 2020).
- Nowak, G.; Żelazko, A.; Nowak, D.; Waliczek, M.; Pawlas, K. Relationship between Health Behavior Patterns and the Level of Stress, Insomnia, and Depression among the Students of Public Health Faculty. Nursing Publ. Health 2015, 5, 231–238. [Google Scholar]
- Castle, T.L.; Martin, J.S. Occupational hazard: Predictors of stress among jail correctional officers. Am. J. Crim. Just. 2006, 31, 65–80. [Google Scholar] [CrossRef]
- Taxman, F.S.; Gordon, J.A. Do fairness and Equity Matter? An Examination of Organizational Justice among Correctional Officers in Adult Prisons. Crim. Justice Behav. 2009, 695–711. [Google Scholar] [CrossRef]
- Kupcewicz, E.; Grochans, E.; Kadučáková, H.; Mikla, M.; Jóźwik, M. Analysis of the Relationship between Stress Intensity and Coping Strategy and the Quality of Life of Nursing Students in Poland, Spain and Slovakia. Int. J. Environ. Res. Public Health 2020, 17, 4536. [Google Scholar] [CrossRef] [PubMed]
- Li, M.H.; Nishikawa, T. The relationship between active coping and trait resilience across US and Taiwanese college student samples. J. Coll. Couns. 2012, 15, 157–171. [Google Scholar] [CrossRef]
- Wirkus, Ł.; Babicka-Wirkus, A.; Opora, R.; Stasiak, K. Burnout among Probation Officers in Poland and the Role of Preferred Styles of Coping with Stress. Int J. Environ. Res. Public Health. 2021, 18, 355. [Google Scholar] [CrossRef]
- Faber, J.; Schlarb, A.A. The Relation of Sleep, Distress, and Coping Strategies—What Male and Female Students Can Learn from Each Other? Health 2016, 8, 1356–1367. [Google Scholar] [CrossRef] [Green Version]
- Palagini, L.; Bruno, R.M.; Cheng, P.; Mauri, M.; Taddei, S.; Ghiadoni, L.; Drake, C.L.; Morin, C.M. Relationship between insomnia symptoms, perceived stress and coping strategies in subjects with arterial hypertension: Psychological factors may play a modulating role. Sleep Med. 2016, 19, 108–115. [Google Scholar] [CrossRef]
- Irish, L.A.; Kline, C.E.; Gunn, H.E.; Buysse, D.J.; Hall, M.H. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Med. Rev. 2015, 22, 23–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vincent, N.; Cox, B.; Clara, I. Are personality dimensions associated with sleep length in a large nationally representative sample? Compr. Psychiat. 2009, 50, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Kales, A.; Caldwell, A.B.; Soldatos, C.R.; Bixler, E.O.; Kales, J.D. Biopsychobehavioral correlates of insomnia. II. Pattern specificity and consistency with the Minnesota Multiphasic Personality Inventory. Psychosom. Med. 1983, 45, 341–356. [Google Scholar] [CrossRef] [PubMed]
- Regehr, C.; Carey, M.; Wagner, S.; Alden, L.E.; Buys, N.; Corneil, W.; Fyfe, T.; Fraess-Phillips, A.; Krutop, E.; Matthews, L.; et al. Prevalence of PTSD, depression and anxiety disorders in correctional officers: A systematic review. Correct. Policy Pract. Res. 2019, 1–13. [Google Scholar] [CrossRef]
- Thorpy, M. Understanding and diagnosing shift work disorder. Postgrad Med. 2011, 123, 96–105. [Google Scholar] [CrossRef]
- Winata, S.D. Relationship of shift Work and other factors with Insomnia in Male Workers at Shoe Factory. J. Kedok. Med. 2018, 24, 66. (In Indonesian) [Google Scholar]
- Saftarina, F.; Hasanah, L. The Relationship between Work Shift and Sleep Pattern Disorders in Inpatient Nursing Installation at Abdul Moeloek Hospital. Medula Unila 2014, 2, 28–38. Available online: http://juke.kedokteran.unila.ac.id/index.php/medula/article/view/313/311 (accessed on 7 December 2020).
- Hamel, R.S.; Rompas, R.M.; Doda, V.D. Relationship between work loading, tenure of works and work shift with sleep pattern disorders in nurses in general hospital Manado. J. Keper. 2018, 6, 1–10. Available online: https://ejournal.unsrat.ac.id/index.php/jkp/article/view/24982 (accessed on 7 December 2020).
- Saraswati, A.W.; Paskarini, I. Relationship of sleep disorder in shift workers with work accidents in the packaging terminals. Indones. J. Occup. Safety Health 2018, 7, 72–80. [Google Scholar] [CrossRef] [Green Version]
- Khodadadi, S.; Adibsereshki, N.; Movallali, G.; Bakhshi, E. Effect of coping with stress training on the social adjustment of students with learning disability. J. Res. Med. Sci. 2017, 7, 915–920. [Google Scholar] [CrossRef]
- Sharon-David, H.; Tenenbaum, G. The effectiveness of exercise interventions on coping with stress: Research synthesis. Stud. Sport Humanit. 2017, 21, 19–29. [Google Scholar] [CrossRef]
- Pashib, M.; Abadi, M.M.; Bahrainian, A.; Vahabi, S.A.; Askari, M. Effects of Training the Methods of Coping with Stress on Reducing Anxiety in Student. J. Appl. Environ. Biol. Sci. 2014, 4, 133–136. [Google Scholar]
- Gutiérrez, F.; Peri, J.M.; Torres, X.; Caseras, X.; Valdés, M. Three dimensions of coping and a look at their evolutionary origin. J. Res. Pers. 2007, 41, 1032–1053. [Google Scholar] [CrossRef]
- Martino, F.; Abreu, A.C.B.; Barbosa, M.F.D.S.; Teixeira, J.E.M. The relationship between shift work and sleep patterns in nurses. Cien. Saude Colet. 2013, 18, 763–768. [Google Scholar] [CrossRef] [Green Version]
- Spiegelhalder, K.; Regen, W.; Feige, B.; Hirscher, V.; Unbehaun, T.; Nissen, C.; Riemann, D.; Baglioni, C. Sleep-related arousal versus general cognitive arousal in primary insomnia. J. Clin. Sleep Med. 2012, 8, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Kploanyi, E.E.; Dwomoh, D.; Dzodzomenyo, M. The effect of occupational stress on depression and insomnia: A cross-sectional study among employees in a Ghanaian telecommunication company. BMC Pub. Health 2020, 20, 1045. [Google Scholar] [CrossRef]
- Portela, L.F.; Kröning Luna, C.; Rotenberg, L.; Silva-Costa, A.; Toivanen, S.; Araújo, T.; Griep, R.H. Job Strain and Self-Reported Insomnia Symptoms among Nurses: What about the Influence of Emotional Demands and Social Support? BioMed Res. Int. 2015, 820610. [Google Scholar] [CrossRef]
- Eldevik, M.F.; Flo, E.; Moen, B.E.; Pallesen, S.; Bjorvatn, B. Insomnia, excessive sleepiness, excessive fatigue, anxiety, depression and shift work disorder in nurses having less than 11 hours in-between shifts. PLoS ONE 2013, 8, e70882. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.E.; Hwang, W.T.; Scott, L.D. The effects of work breaks on staff nurse performance. J. Nurs. Adm. 2004, 34, 512–519. [Google Scholar] [CrossRef]
- Dongen, H.P.; Dinges, D.F. Investigating the interaction between the homeostatic and circadian processes of sleep-wake regulation for the prediction of waking neurobehavioural performance. J. Sleep. Res. 2003, 12, 181–187. [Google Scholar] [CrossRef]
- Riemann, D.; Perlis, M.L. The treatments of chronic insomnia: A review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med. Rev. 2009, 13, 205–214. [Google Scholar] [CrossRef] [PubMed]







| N | Age | Woman | Multi-Shift System | Secondary Education | Bachelor’s Degree | Master’s Degree | Open | Semi-Open | Closed | |
|---|---|---|---|---|---|---|---|---|---|---|
| Poland | 288 | 34.12 (SD 7.4) | 33 (11.8%) | 194 (68.6%) | 143 (50.4%) | 58 (20.4%) | 83 (29.2%) | 3 (1.1%) | 60 (21.4%) | 217 (77.5%) |
| Indonesia | 376 | 33.61 (SD 9.4) | 76 (20.2%) | 175 (46.7%) | 157 (41.8%) | 190 (50.5%) | 29 (7.7%) | 0 | 60 (16.0%) | 316 (84.0%) |
| M | Me | SD | Sc. | Kurt. | Min. | Max. | D | p | |
|---|---|---|---|---|---|---|---|---|---|
| Insomnia | 5.45 | 4.00 | 4.34 | 1.15 | 1.14 | 0.00 | 21.00 | 0.15 | <0.001 |
| Occupational burnout | |||||||||
| Exhaustion | 2.28 | 2.25 | 0.48 | −0.06 | 0.57 | 1.00 | 4.00 | 0.09 | <0.001 |
| Distancing | 2.29 | 2.25 | 0.50 | 0.12 | 0.23 | 1.00 | 4.00 | 0.07 | <0.001 |
| Coping styles | |||||||||
| Engagement | 16.56 | 16.75 | 2.87 | −0.30 | 0.56 | 6.00 | 24.00 | 0.04 | 0.001 |
| Disengagement | 9.25 | 9.50 | 1.62 | −0.24 | 0.58 | 4.00 | 15.25 | 0.08 | <0.001 |
| Help-seeking | 8.27 | 8.25 | 1.69 | −0.16 | 0.02 | 3.00 | 12.00 | 0.05 | 0.001 |
| Insomnia | Z | P | ||||||
|---|---|---|---|---|---|---|---|---|
| Total Sample | Poland | Indonesia | ||||||
| r | p | r | p | R | p | |||
| Engagement | −0.20 | <0.001 | −0.18 | 0.001 | −0.03 | 0.575 | −2.19 | 0.029 |
| Disengagement | −0.04 | 0.245 | 0.09 | 0.126 | 0.12 | 0.010 | −0.45 | 0.651 |
| Help-seeking | −0.25 | <0.001 | −0.23 | <0.001 | −0.02 | 0.736 | −2.97 | 0.003 |
| Insomnia | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | ||||||||
| Me | IQR | Me | IQR | Z | P | r | |||
| Total sample | 415.30 | 5.00 | 6.00 | 352.57 | 4.00 | 5.00 | −3.89 | <0.001 | 0.14 |
| Poland | 156.82 | 7.00 | 8.00 | 123.54 | 7.00 | 7.00 | −2.11 | 0.035 | 0.12 |
| Indonesia | 238.12 | 4.00 | 4.00 | 219.44 | 3.00 | 3.00 | −1.25 | 0.212 | 0.06 |
| Poland | Indonesia | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Me | IQR | Me | IQR | Z | p | r | |||
| Multi-shift system | 252.71 | 7.00 | 8.00 | 230.87 | 4.00 | 4.00 | −6.24 | <0.001 | 0.30 |
| Single-shift system | 178.07 | 7.00 | 7.00 | 151.37 | 3.00 | 3.00 | −6.54 | <0.001 | 0.35 |
| Women | Men | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Me | IQR | Me | IQR | Z | p | R | |||
| Total sample | 329.13 | 3.50 | 4.00 | 398.99 | 5.00 | 6.00 | −3.35 | 0.001 | 0.12 |
| Poland | 123.54 | 5.00 | 7.00 | 156.82 | 7.00 | 7.00 | −2.11 | 0.035 | 0.12 |
| Indonesia | 219.44 | 3.00 | 4.00 | 238.12 | 3.00 | 4.00 | −1.25 | 0.212 | 0.06 |
| X | Y | Poland | Indonesia | Z–Score | ||||
|---|---|---|---|---|---|---|---|---|
| B | Β | p | b | β | P | |||
| Gender | Insomnia | 1.33 | 0.08 | 0.160 | 0.28 | 0.04 | 0.416 | −1.04 |
| Age | Insomnia | 0.10 | 0.14 | 0.011 | −0.01 | −0.04 | 0.437 | −2.65 *** |
| Penitentiary unit type | Insomnia | <−0.01 | <0.01 | 0.996 | 0.05 | 0.01 | 0.900 | 0.07 |
| Engagement | Insomnia | −0.11 | −0.05 | 0.520 | −0.16 | −0.15 | 0.068 | −0.21 |
| Disengagement | Insomnia | 0.30 | 0.11 | 0.055 | 0.45 | 0.19 | <0.001 | 0.70 |
| Help-seeking | Insomnia | −0.64 | −0.18 | 0.029 | 0.03 | 0.02 | 0.848 | 2.05 ** |
| Multi-shift work | Insomnia | 0.40 | 0.04 | 0.545 | −0.52 | −0.09 | 0.076 | −1.28 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sygit-Kowalkowska, E.; Piotrowski, A.; Hamzah, I. Insomnia among Prison Officers and Its Relationship with Occupational Burnout: The Role of Coping with Stress in Polish and Indonesian Samples. Int. J. Environ. Res. Public Health 2021, 18, 4282. https://doi.org/10.3390/ijerph18084282
Sygit-Kowalkowska E, Piotrowski A, Hamzah I. Insomnia among Prison Officers and Its Relationship with Occupational Burnout: The Role of Coping with Stress in Polish and Indonesian Samples. International Journal of Environmental Research and Public Health. 2021; 18(8):4282. https://doi.org/10.3390/ijerph18084282
Chicago/Turabian StyleSygit-Kowalkowska, Ewa, Andrzej Piotrowski, and Imaduddin Hamzah. 2021. "Insomnia among Prison Officers and Its Relationship with Occupational Burnout: The Role of Coping with Stress in Polish and Indonesian Samples" International Journal of Environmental Research and Public Health 18, no. 8: 4282. https://doi.org/10.3390/ijerph18084282








