Redesigning a Healthcare Demand Questionnaire for National Population Survey: Experience of a Developing Country
Abstract
:1. Introduction
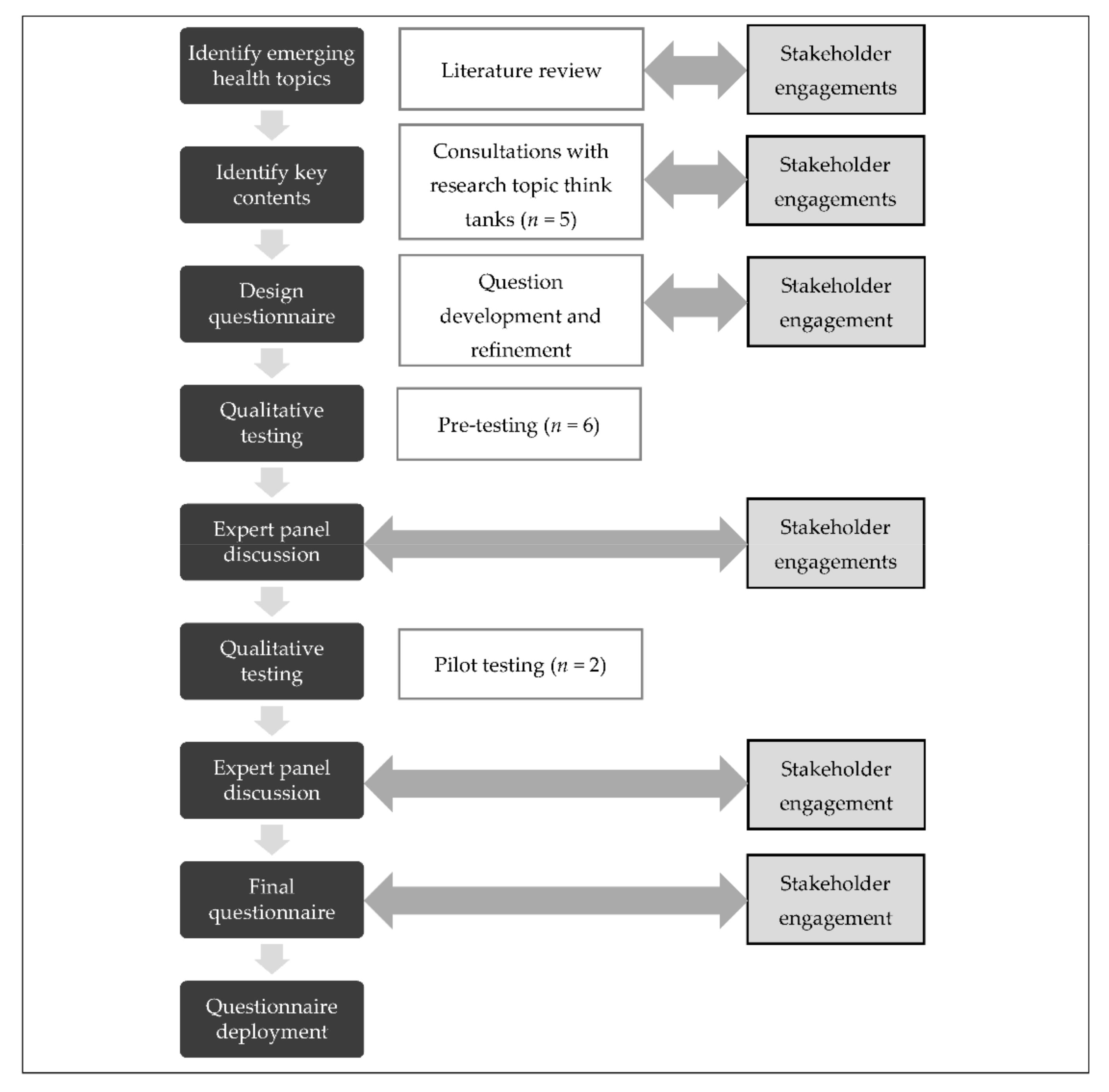
2. Materials and Methods
2.1. Principles of Redesigning the Healthcare Demand Questionnaire
2.2. Phase 1: Literature Review
2.3. Phase 2: Consultation with Research Topic Think Tanks
2.4. Phase 3: Question Development and Refinement
2.5. Phase 4: Qualitative Testing—Pretest
2.6. Phase 5: Expert Panel Discussion
2.7. Phase 6: Qualitative Testing—Pilot Test
2.8. Phase 7: Final Questionnaire
2.9. Phase 8: Questionnaire Deployment
2.10. Ethical Considerations
2.11. Analysis
3. Results
3.1. Literature Review
3.2. Stakeholders Engaged
3.3. Content Areas Added and Dropped
3.4. Survey Respondents
4. Discussion
Strengths and Limitations of this Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Institute for Health Systems Research. Revision of Healthcare Demand Questionnaire for National Health and Morbidity Survey (NHMS) 2019; Institute for Health Systems Research: Selangor, Malaysia, 2018. [Google Scholar]
- Institute for Public Health. National Health and Morbidity Survey (NHMS) 2015. Vol I: Methodology and General Findings; Institute for Public Health: Kuala Lumpur, Malaysia, 2015. [Google Scholar]
- Institute for Health Systems Research. National Health and Morbidity Survey (NHMS) 2015. Vol III: Healthcare Demand; Institute for Public Health: Kuala Lumpur, Malaysia; Institute for Health Systems Research: Selangor, Malaysia, 2015. [Google Scholar]
- Institute for Health Systems Research. National Health and Morbidity Survey (NHMS) 2019: Vol. II: Healthcare Demand; Institute for Public Health: Kuala Lumpur, Malaysia; Institute for Health Systems Research: Selangor, Malaysia, 2020. [Google Scholar]
- DG Speaks: NHMS 2019, the NCD War, and the Roles of Pharmacists. Available online: https://specialty.mims.com/topic/dg-speaks--nhms-2019--the-ncd-war--and-the-roles-of-pharmacists#resources (accessed on 11 March 2021).
- Atun, R.; Berman, P.; Hsiao, W.; Myers, E.W.A. Malaysia Health Systems Research Volume 1: Contextual Analysis of the Malaysian Health System; Ministry of Health Malaysia: Kuala Lumpur, Malaysia; Harvard TH Chan School of Public Health: Boston, MA, USA, 2016. [Google Scholar]
- Access to Healthcare in Malaysia. Ministry of Economic Affairs (MEA) 12th Malaysia Plan Kick-off Conference. Available online: http://rmke12.epu.gov.my/ciopapers/1fb86018e0741fe3f9e59c97e42d0f35.pdf (accessed on 11 March 2021).
- Press Release Population Projection (Revised), Malaysia, 2010–2040; The Office of Chief Statistician Malaysia, Department of Statistics: Putrajaya, Malaysia, 2016.
- Cardosa, M.S.; Ungku Ahmad, U.K.; Swan, N.K.; Bhojwani, K.; Ahmad, A.; Wahidin, H.; Perumal, M.; Abdul Rahman, P.M.N.; Muhamad Zin, F.; Adnan, A.S.; et al. Pain as the 5th Vital Sign Guideline, 3rd ed.; Medical Development Division, Ministry of Health Malaysia and the National Pain Free Programme Committee: Putrajaya, Malaysia, 2018. [Google Scholar]
- Changing Demographics Demand Healthcare Reforms. Available online: https://www.pwc.com/gx/en/industries/healthcare/emerging-trends-pwc-healthcare/changing-demographics-healthcare-reform.html (accessed on 5 October 2020).
- Mindell, J.S.; Moody, A.; Vecino-Ortiz, A.I.; Alfaro, T.; Frenz, P.; Scholes, S.; Gonzalez, S.A.; Margozzini, P.; De Oliveira, C.; Sanchez Romero, L.M.; et al. Comparison of Health Examination Survey Methods in Brazil, Chile, Colombia, Mexico, England, Scotland, and the United States. Am. J. Epidemiol. 2017, 186, 648–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mallery, C.; Ganachari, D.; Fernandez, J.; Smeeding, L.; Robinson, S.; Moon, M.; Lavallee, D.; Siegel, J. Innovative Methods for Stakeholder Engagement: An Environmental Scan; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012. [Google Scholar]
- Prince, S.A.; Butler, G.P.; Roberts, K.C.; Lapointe, P.; MacKenzie, A.M.; Colley, R.C.; Foley, M.; Saunders, T.J.; Thompson, W. Developing Content for National Population Health Surveys: An Example Using a Newly Developed Sedentary Behaviour Module. Arch. Public Health 2019, 77, 53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finger, J.D.; Tafforeau, J.; Gisle, L.; Oja, L.; Ziese, T.; Thelen, J.; Mensink, G.B.M.; Lange, C. Development of the European Health Interview Survey—Physical Activity Questionnaire (EHIS-PAQ) to Monitor Physical Activity in the European Union. Arch. Public Health Arch. Belg. Publique 2015, 73, 59. [Google Scholar] [CrossRef] [Green Version]
- Boateng, G.O.; Neilands, T.B.; Frongillo, E.A.; Melgar-Quiñonez, H.R.; Young, S.L. Best Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front. Public Health 2018, 6, 149. [Google Scholar] [CrossRef]
- Ruel, E.; Wagner, W.E.; Gillespie, B.J. Pretesting and Pilot Testing. In The Practice of Survey Research: Theory and Applications; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Lenzner, T.; Neuert, C.; Otto, W. Cognitive Pretesting. In GESIS Survey Guidelines; GESIS-Leibnitz Institute for the Social Sciences: Mannheim, Germany, 2016; ISBN 9783531178097. [Google Scholar]
- Alderman, A.K.; Salem, B. Survey Research. Plast. Reconstr. Surg. 2010, 126, 1381–1389. [Google Scholar] [CrossRef] [PubMed]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for Developing, Translating, and Validating a Questionnaire in Perioperative and Pain Medicine. Saudi J. Anaesth. 2017, 11 (Suppl. 1), S80–S89. [Google Scholar] [CrossRef] [PubMed]
- Boaz, A.; Hanney, S.; Borst, R.; O’Shea, A.; Kok, M. How to Engage Stakeholders in Research: Design Principles to Support Improvement. Health Res. Policy Syst. 2018, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Artino, A.R.; La Rochelle, J.S.; Dezee, K.J.; Gehlbach, H. Developing Questionnaires for Educational Research: AMEE Guide No. 87. Med. Teach. 2014, 36, 463–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersen, R.M. Revisiting the Behavioral Model and Access to Medical Care: Does It Matter? J. Health Soc. Behav. 1995, 36, 1. [Google Scholar] [CrossRef] [PubMed]
- Priede, C.; Farrall, S. Comparing Results from Different Styles of Cognitive Interviewing: “verbal Probing” vs. “Thinking Aloud”. Int. J. Soc. Res. Methodol. 2011. [Google Scholar] [CrossRef]
- Willis, G.B. Analysis of the Cognitive Interview in Questionnaire Design; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Institute for Public Health; Institute for Health Systems Research. National Health and Morbidity Survey (NHMS) 2019: Non-Communicable Diseases, Healthcare Demand, and Health Literacy—Key Findings; Institute for Health Systems Research: Selangor, Malaysia; Institute for Public Health: Kuala Lampur, Malaysia, 2020. [Google Scholar]
- Fadhli, Y.; Azahadi, O.; Ani, A.N.; Balkish, M.N.; Jessree, K.A.; Tahir, A. Approaches in Methodology of a Population-Based Study in Malaysia: The National Health and Morbidity Survey 2011 (NHMS 2011). Malays. J. Med. Health Sci. 2013, 9, 25–33. [Google Scholar]
- Kost, R.G.; Correa da Rosa, J. Impact of Survey Length and Compensation on Validity, Reliability, and Sample Characteristics for Ultrashort-, Short-, and Long-Research Participant Perception Surveys. J. Clin. Transl. Sci. 2018, 2, 31–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanankege, K.S.T.; Phelps, N.B.D.; Vesterinen, H.M.; Errecaborde, K.M.; Alvarez, J.; Bender, J.B.; Wells, S.J.; Perez, A.M. Lessons Learned from the Stakeholder Engagement in Research: Application of Spatial Analytical Tools in One Health Problems. Front. Vet. Sci. 2020, 7, 254. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia. Pain as the 5th Vital Sign Guidelines, 2nd ed.; Ministry of Health Malaysia: Putrajaya, Malaysia, 2013. [Google Scholar]
- Cislaghi, B.; Cislaghi, C. Self-Rated Health as a Valid Indicator for Health-Equity Analyses: Evidence from the Italian Health Interview Survey. BMC Public Health 2019, 19, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowling, A. Just One Question: If One Question Works, Why Ask Several? J. Epidemiol. Community Health 2005, 59, 342–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2019: Highlights; United Nations: Washington, DC, USA, 2020. [Google Scholar]
- Kuziemsky, C.; Lau, F. Handbook of eHealth Evaluation: An Evidence-Based Approach; University of Victoria: Victoria, BC, Canada, 2016. [Google Scholar]
- Abu Bakar, N.S.; Manual, A.; Ab Hamid, J. Socioeconomic Status Affecting Inequity of Healthcare Utilisation in Malaysia. Malays. J. Med Sci. 2019, 26, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Zulkefli, Z.K. Gender Differences in Healthcare Utilisation among the Elderly in Malaysia: A Decomposition Analysis. Int. J. Manag. Stud. 2015, 22, 73–91. [Google Scholar]
- McDonald, J.A.; Burnett, N.; Coronado, V.G.; Johnson, R.L. Questionnaire Design. In Reproductive Health Epidemiology Series; Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion: Atlanta, GA, USA, 2003. [Google Scholar]
- Corbin, J.; Strauss, A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 3rd ed.; Sage Publication: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Egger-Rainer, A. Enhancing Validity through Cognitive Interviewing. A Methodological Example Using the Epilepsy Monitoring Unit Comfort Questionnaire. J. Adv. Nurs. 2019, 75, 224–233. [Google Scholar] [CrossRef] [PubMed]

| Area of Expertise (n) | |
|---|---|
| Health policy (4) | Pharmaceutical care (2) |
| Family health (2) | Traditional and complementary medicine (2) |
| Public health (3) | Geriatric care (1) |
| Oral health (1) | Oncology (1) |
| Health planning (4) | Pain condition and management (1) |
| Health financing (8) | Palliative care (1) |
| Health statistics (2) | Questionnaire design and survey methodology (2) |
| Characteristic | Pretest (N = 242) Number of Cycles: 6 | Pilot Test (N = 113) Number of Cycles: 2 | ||
|---|---|---|---|---|
| n | % | n | % | |
| Sex | ||||
| Male | 87 | 36.0 | 51 | 45.1 |
| Female | 151 | 62.4 | 62 | 54.9 |
| Age (years) | ||||
| 17 and below | 6 | 2.5 | 2 | 1.8 |
| 18–29 | 44 | 18.2 | 18 | 15.9 |
| 30–49 | 90 | 37.2 | 26 | 23.0 |
| 50–69 | 84 | 34.7 | 56 | 49.6 |
| 70+ | 14 | 5.8 | 11 | 9.7 |
| Ethnicity | ||||
| Malay | 161 | 66.5 | 74 | 65.5 |
| Chinese | 25 | 10.3 | 13 | 11.5 |
| Indian | 43 | 17.8 | 25 | 22.1 |
| Others | 7 | 2.9 | 1 | 0.9 |
| Citizenship 1 | ||||
| Malaysian | 201 | 94.8 | 113 | 100.0 |
| Non-Malaysian | 5 | 2.4 | 0 | - |
| Marital status 1 | ||||
| Never married | 33 | 15.6 | 20 | 17.7 |
| Married | 157 | 74.1 | 79 | 69.9 |
| Separated/Divorced/Widow(er) | 19 | 9.0 | 14 | 12.4 |
| Education level 1 | ||||
| No formal education | 12 | 5.7 | 11 | 9.7 |
| Completed primary education | 22 | 10.4 | 13 | 11.5 |
| Completed secondary education | 101 | 47.6 | 59 | 52.2 |
| Completed tertiary education | 76 | 35.9 | 30 | 26.6 |
| Employment status | ||||
| Yes | 141 | 58.3 | 61 | 54.0 |
| No | 101 | 41.7 | 52 | 46.0 |
| Issue | Original Item | Action Taken | Revised Item |
|---|---|---|---|
| Reasons for no coverage of any personal health insurance plans were identified as important to cater to current demand and assist in policy-making. | Are you covered by any personal health insurance plans which you or a family member had purchased? | New question added | Are you covered by any personal health insurance plans which you or a family member had purchased? If no, why? |
| Information on how people perceived their health generally was identified as important. The literature review found that the question was included in almost half (21) of the total number of countries included in the review. | How would you rate your health? | Question added | - |
| The question was problematic to measure the prevalence of chronic pain among participants. For instance, one respondent mentioned muscle pain after physical activity, which will eventually go away after rest. Thus, a duration to imply chronic pain and definition of persistent pain was included in the question’s text. | In the last two weeks, from [fill month and year] till today, did you experience any bodily pain? (e.g., headache, joint pain, muscle aches, etc.). If yes, how long you have been experiencing the pain? | Accept original question with major edits | In the last six months, from [fill month and year] till today, have you had persistent pain in any part of your body lasting for three months or more? (Persistent pain means that the pain is felt every day, or most days, during that period). |
| Cognitive testing confirmed that participants were primarily thinking of pharmacies with a pharmacist who sells medicines when they responded to this question, as intended. | In the last two weeks, from [fill month and year] till today, did you go to a community pharmacy for yourself or other health reasons? | Accept original question | - |
| Testing revealed that participants have difficulty estimating the duration when they last received dental care. The answer options were simplified into multiple choice answers. | When was the last time you received dental care? (please write estimated month and year) Original answer options: … month … year Never received | Modified | When was the last time you received dental care? (please write estimated month and year) Final answer options: 1–2 years ago More than 2 years ago Never received |
| Testing revealed that participants have difficulty answering the questions on which person they cared for. For instance, one respondent who had provided care for two persons reported the same amount of time spent for both persons, but one is in the household, and another is not in the household. | If assists more than one, the respondent only has to answer for one individual cared for. | New clearer instruction used in the questionnaire with additional guideline in the manual to guide the interviewers during data collection | Instruction: If assists more than one, the respondent only has to answer for one individual who is most often taken care of. Additional guideline: Adopted from: Survey of Carers in Households—England, 2009–2010. a. If assists more than one person, select the one that the respondent spends most time helping. b. If the same amount of time is spent assisting two people, select the one that lives in the respondent’s household. c. If the same amount of time is spent assisting two people, both of whom live in the respondent’s household, select the person on whom more time is spent. If the respondent is unable to say for which person, she/he spends most time caring, select the first one listed. d. If there is more than one person cared for and they all live outside the household, select the one with the highest number of hours helped. e. If the same amount of assistance is given to more than one person, all of whom live outside the household, choose the first one listed. |
| The question was problematic as participants tend to answer 24 h per day (168 h per week) when they perceive care provision is intensive, excluding the number of hours when they are asleep. For participants who were not living in the same household with the cared-for person, the participants tend to exclude the traveling time to and from their home. | In total, how many hours per week do you normally spend providing the care to [fill cared-for person’s name]? | Accept original question with minor edits | If the cared-for person is in the household: In total, how many hours per week do you normally spend providing the care to [fill cared-for person’s name], apart from when you are asleep? If the cared-for person is not in the household: In total, how many hours per week do you normally spend providing the care to [fill cared-for person’s name], including time traveling to and from his/her home? |
| Testing confirmed that the question was not necessary, as it was already mentioned in the instruction that informal care does not involve wage/salary. | Were you paid to provide care? | Question dropped | - |
| Reasons for no coverage of any personal health insurance plans were identified as important to cater to current demand and assist in policy-making. | Are you covered by any personal health insurance plans which you or a family member had purchased? | New question added | Are you covered by any personal health insurance plans which you or a family member had purchased? If no, why? |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chong, D.W.Q.; Jawahir, S.; Tan, E.H.; Sararaks, S. Redesigning a Healthcare Demand Questionnaire for National Population Survey: Experience of a Developing Country. Int. J. Environ. Res. Public Health 2021, 18, 4435. https://doi.org/10.3390/ijerph18094435
Chong DWQ, Jawahir S, Tan EH, Sararaks S. Redesigning a Healthcare Demand Questionnaire for National Population Survey: Experience of a Developing Country. International Journal of Environmental Research and Public Health. 2021; 18(9):4435. https://doi.org/10.3390/ijerph18094435
Chicago/Turabian StyleChong, Diane Woei Quan, Suhana Jawahir, Ee Hong Tan, and Sondi Sararaks. 2021. "Redesigning a Healthcare Demand Questionnaire for National Population Survey: Experience of a Developing Country" International Journal of Environmental Research and Public Health 18, no. 9: 4435. https://doi.org/10.3390/ijerph18094435
APA StyleChong, D. W. Q., Jawahir, S., Tan, E. H., & Sararaks, S. (2021). Redesigning a Healthcare Demand Questionnaire for National Population Survey: Experience of a Developing Country. International Journal of Environmental Research and Public Health, 18(9), 4435. https://doi.org/10.3390/ijerph18094435







