Using WHODAS 2.0 to Assess Functional Impairment in People with Depression: Should Employment Receive More Attention?
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurement Tools
2.3. Data Collection
2.4. Statistical Analysis
3. Results
3.1. Characteristics of People with MDD-Associated Disability
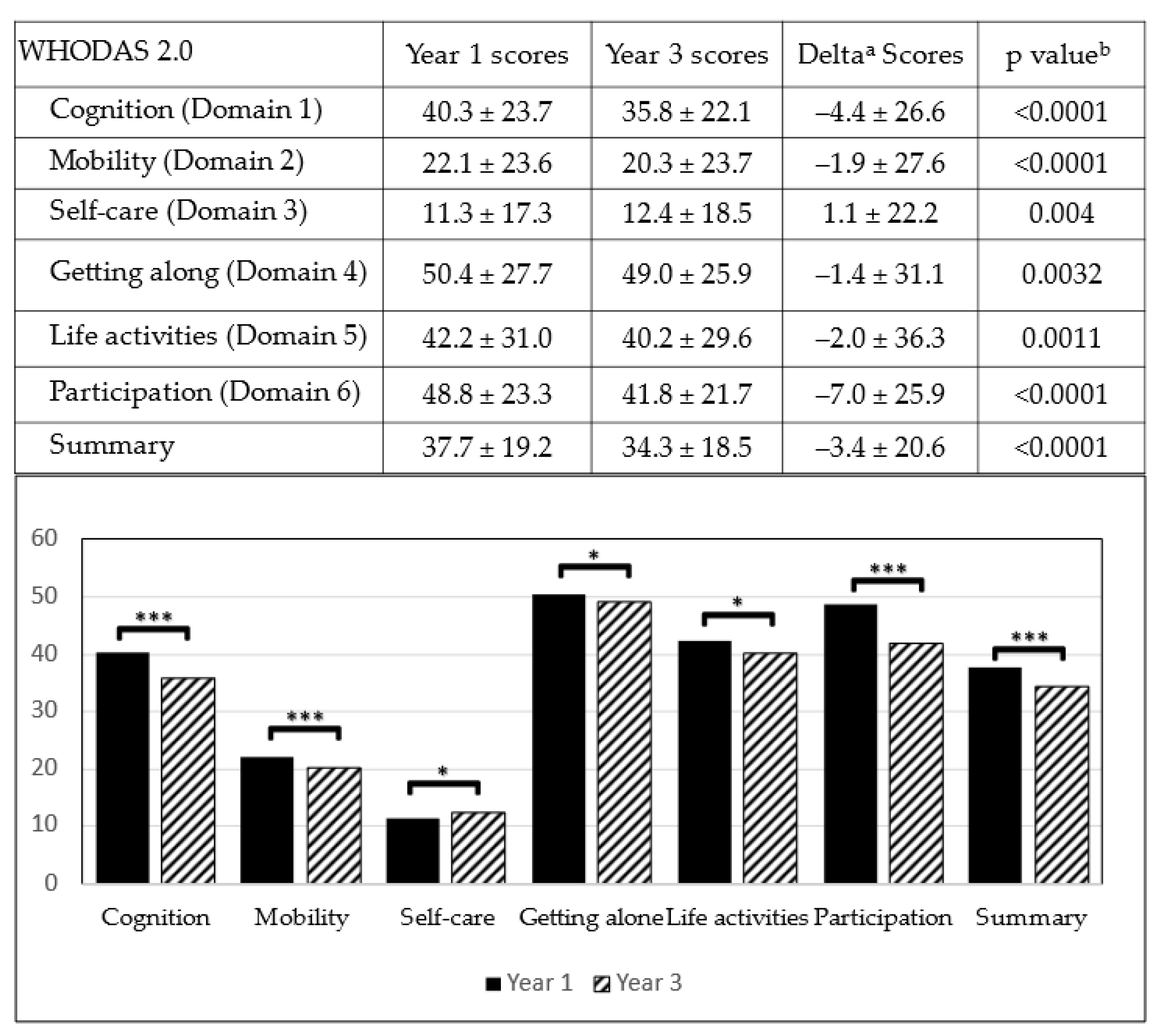
3.2. Changes in WHODAS 2.0 Scores after 3 Years in People with MDD-Associated Disability
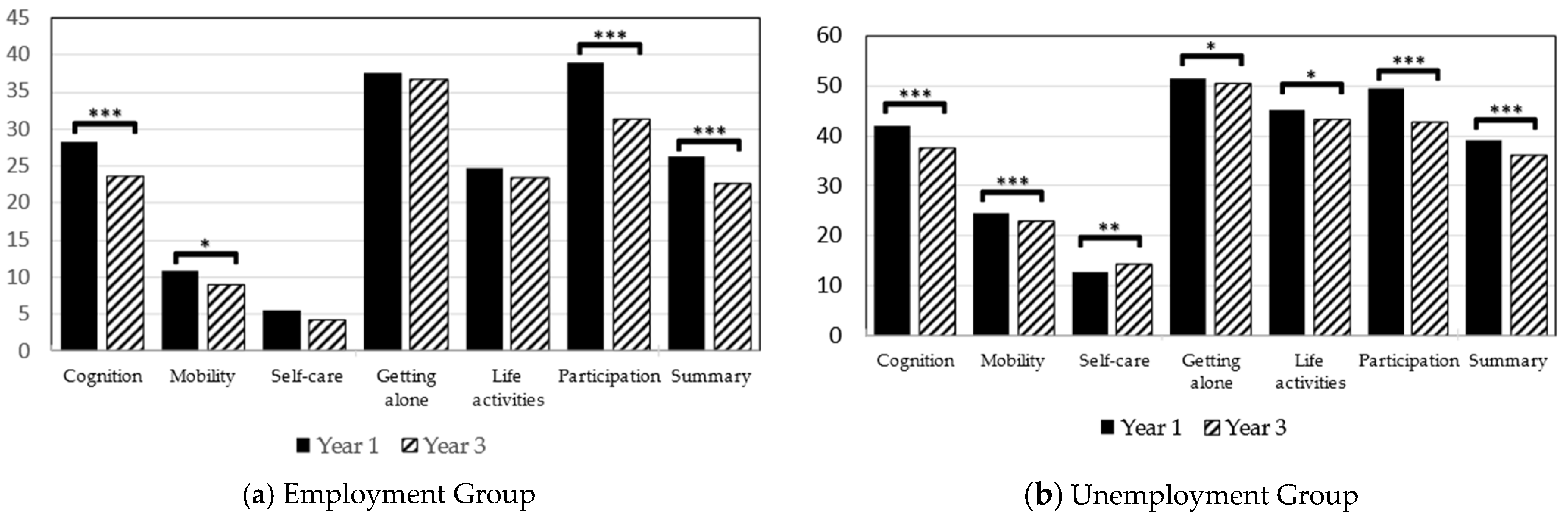
3.3. Stratified Analysis of Employment Status
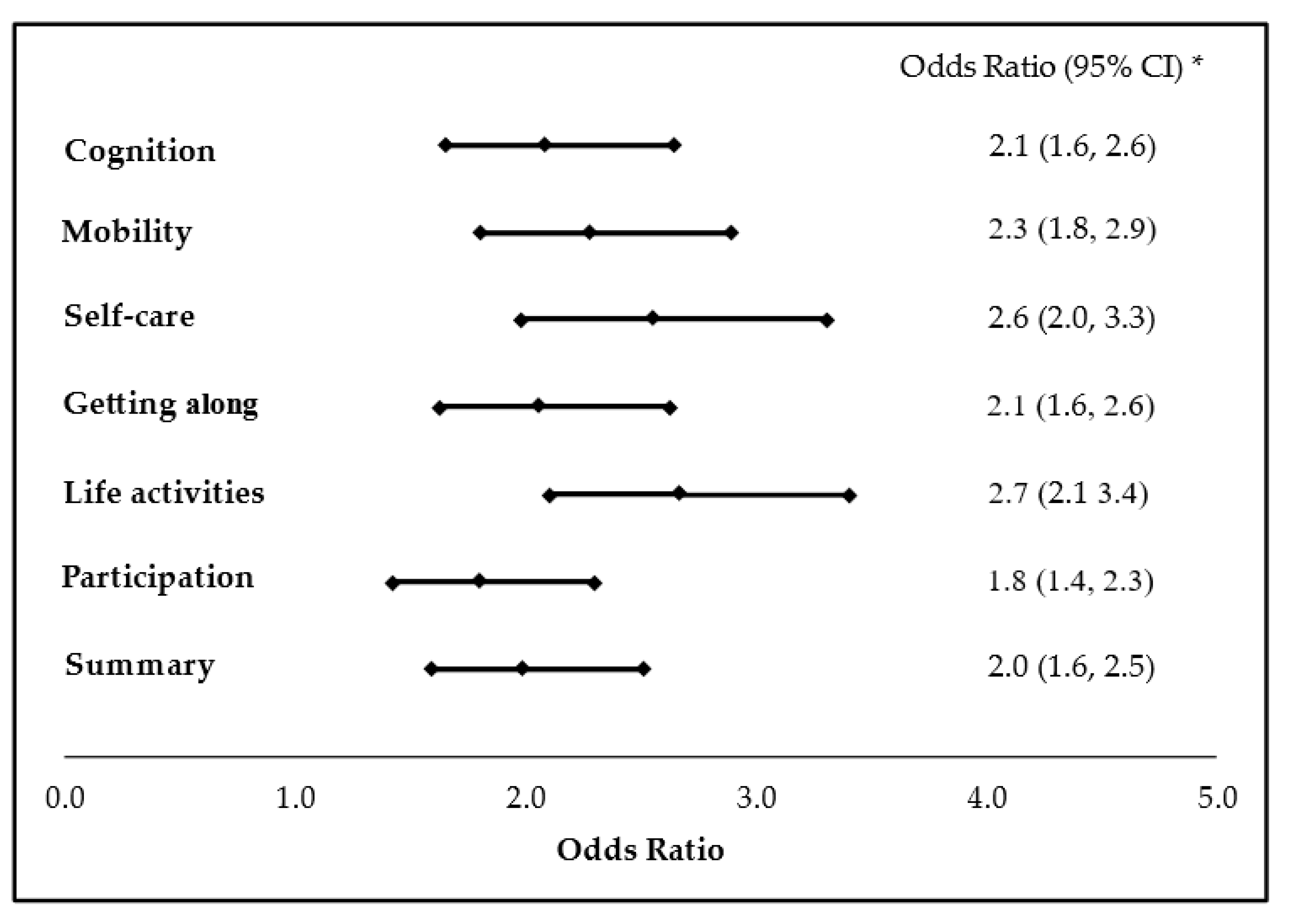
3.4. The Association between Employment and Functional Improvement
4. Discussion
4.1. Functional Impairment and Depression
4.2. Employability and Depression
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Keller, M.B.; Lavori, P.W.; Rice, J.; Coryell, W.; Hirschfeld, R.M. The persistent risk of chronicity in recurrent episodes of nonbipolar major depressive disorder: A prospective follow-up. Am. J. Psychiatry 1986, 143, 24–28. [Google Scholar] [CrossRef]
- Eaton, W.W.; Shao, H.; Nestadt, G.; Lee, H.B.; Bienvenu, O.J.; Zandi, P. Population-Based Study of First Onset and Chronicity in Major Depressive Disorder. Arch. Gen. Psychiatry 2008, 65, 513–520. [Google Scholar] [CrossRef]
- Burcusa, S.L.; Iacono, W.G. Risk for recurrence in depression. Clin. Psychol. Rev. 2007, 27, 959–985. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-M.; Stewart, R.; Glozier, N.; Prince, M.; Kim, S.-W.; Yang, S.-J.; Shin, I.-S.; Yoon, J.-S. Physical health, depression and cognitive function as correlates of disability in an older Korean population. Int. J. Geriatr. Psychiatry 2005, 20, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Van Der Voort, T.Y.G.; Seldenrijk, A.; Van Meijel, B.; Goossens, P.J.J.; Beekman, A.T.F.; Penninx, B.W.J.H.; Kupka, R.W. Functional Versus Syndromal Recovery in Patients with Major Depressive Disorder and Bipolar Disorder. J. Clin. Psychiatry 2015, 76, e809–e814. [Google Scholar] [CrossRef] [PubMed]
- Mogga, S.; Prince, M.; Alem, A.; Kebede, D.; Stewart, R.; Glozier, N.; Hotopf, M. Outcome of major depression in Ethiopia. Br. J. Psychiatry 2006, 189, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Antunes, A.; Frasquilho, D.; Azeredo-Lopes, S.; Neto, D.; Silva, M.; Cardoso, G.; Caldas-De-Almeida, J.M. Disability and common mental disorders: Results from the World Mental Health Survey Initiative Portugal. Eur. Psychiatry 2018, 49, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Rytsälä, H.J.; Melartin, T.K.; Leskelä, U.S.; Sokero, T.P.; Lestelä-Mielonen, P.S.; Isometsä, E.T. Functional and Work Disability in Major Depressive Disorder. J. Nerv. Ment. Dis. 2005, 193, 189–195. [Google Scholar] [CrossRef]
- Rytsälä, H.J.; Melartin, T.K.; Leskelä, U.S.; Lestelä-Mielonen, P.S.; Sokero, T.P.; Isometsä, E.T. Determinants of Functional Disability and Social Adjustment in Major Depressive Disorder. J. Nerv. Ment. Dis. 2006, 194, 570–576. [Google Scholar] [CrossRef]
- Israel, J.A. The Impact of Residual Symptoms in Major Depression. Pharmaceuticals 2010, 3, 2426–2440. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Estimates 2016: Disease Burden by Cause, Age, Sex, by Country and by Region, 2000–2016; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Heinz, A.J.; Meffert, B.N.; Halvorson, M.A.; Blonigen, D.; Timko, C.; Cronkite, R. Employment characteristics, work environment, and the course of depression over 23 years: Does employment help foster resilience? Depress. Anxiety 2018, 35, 861–867. [Google Scholar] [CrossRef]
- Shiba, K.; Kondo, N.; Kondo, K.; Kawachi, I. Retirement and mental health: Does social participation mitigate the association? A fixed-effects longitudinal analysis. BMC Public Health 2017, 17, 526. [Google Scholar] [CrossRef]
- Hao, G.; Bishwajit, G.; Tang, S.; Nie, C.; Ji, L.; Huang, R. Social participation and perceived depression among elderly population in South Africa. Clin. Interv. Aging 2017, 12, 971–976. [Google Scholar] [CrossRef]
- Wu, T.-Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Liou, T.-H.; Chang, K.-H.; Yen, C.-F.; Liao, H.-F.; Chi, W.-C.; Chou, K.-R. Assessment of functioning and disability in patients with schizophrenia using the WHO Disability Assessment Schedule 2.0 in a large-scale database. Eur. Arch. Psychiatry Clin. Neurosci. 2017, 268, 65–75. [Google Scholar] [CrossRef]
- TB Üstün NKSCJR. Measuring Health and Disabilities Manual for WHO Disability Assessment Schedule, WHODAS 2.0; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Yen, C.-F.; Hwang, A.-W.; Liou, T.-H.; Chiu, T.-Y.; Hsu, H.-Y.; Chi, W.-C.; Wu, T.-F.; Chang, B.-S.; Lu, S.-J.; Liao, H.-F.; et al. Validity and reliability of the Functioning Disability Evaluation Scale-Adult Version based on the WHODAS 2.0—36 items. J. Med. Assoc. 2014, 113, 839–849. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.-Y.; Yen, C.-F.; Chou, C.-H.; Lin, J.-D.; Hwang, A.-W.; Liao, H.-F.; Chi, W.-C. Development of traditional Chinese version of World Health Organization Disability Assessment Schedule 2.0 36—Item (WHODAS 2.0) in Taiwan: Validity and reliability analyses. Res. Dev. Disabil. 2014, 35, 2812–2820. [Google Scholar] [CrossRef]
- Federici, S.; Bracalenti, M.; Meloni, F.; Luciano, J.V. World Health Organization disability assessment schedule 2.0: An international systematic review. Disabil. Rehabil. 2017, 39, 2347–2380. [Google Scholar] [CrossRef] [PubMed]
- McKnight, P.E.; Kashdan, T.B. The importance of functional impairment to mental health outcomes: A case for reassessing our goals in depression treatment research. Clin. Psychol. Rev. 2009, 29, 243–259. [Google Scholar] [CrossRef] [PubMed]
- Hirschfeld, R.M.A.; Montgomery, S.A.; Keller, M.B.; Kasper, S.; Schatzberg, A.F.; Moller, H.-J.; Healy, D.; Baldwin, D.; Humble, M.; Versiani, M.; et al. Social Functioning in Depression. J. Clin. Psychiatry 2000, 61, 268–275. [Google Scholar] [CrossRef]
- Kupferberg, A.; Bicks, L.; Hasler, G. Social functioning in major depressive disorder. Neurosci. Biobehav. Rev. 2016, 69, 313–332. [Google Scholar] [CrossRef]
- Tse, W.S.; Bond, A.J. The Impact of Depression on Social Skills: A Review. J. Nerv. Ment. Dis. 2004, 192. [Google Scholar] [CrossRef] [PubMed]
- Rhebergen, D.; Beekman, A.T.; de Graaf, R.; Nolen, W.A.; Spijker, J.; Hoogendijk, W.J.; Penninx, B.W. Trajectories of recovery of social and physical functioning in major depression, dysthymic disorder and double depression: A 3-year follow-up. J. Affect. Disord. 2010, 124, 148–156. [Google Scholar] [CrossRef]
- Liao, S.-C.; Chen, W.J.; Lee, M.-B.; Lung, F.-W.; Lai, T.-J.; Liu, C.-Y.; Lin, C.-Y.; Yang, M.-J.; Chen, C.-C. Low prevalence of major depressive disorder in Taiwanese adults: Possible explanations and implications. Psychol. Med. 2011, 42, 1227–1237. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Co-Operation and Development. Sickness, Disability and Work; 2010. Available online: https://www.oecd.org/employment/emp/42699911.pdf (accessed on 7 March 2021).
- Lerner, D.; Henke, R.M. What Does Research Tell Us about Depression, Job Performance, and Work Productivity? J. Occup. Environ. Med. 2008, 50, 401–410. [Google Scholar] [CrossRef]
- Elinson, L.; Houck, P.; Marcus, S.C.; Pincus, H.A. Depression and the Ability to Work. Psychiatr. Serv. 2004, 55, 29–34. [Google Scholar] [CrossRef]
- Dooley, D.; Prause, J.; Ham-Rowbottom, K.A. Underemployment and Depression: Longitudinal Relationships. J. Health Soc. Behav. 2000, 41, 421–436. [Google Scholar] [CrossRef] [PubMed]
- Doshi, J.A.; Cen, L.; Polsky, D. Depression and Retirement in Late Middle-Aged U.S. Workers. Health Serv. Res. 2008, 43, 693–713. [Google Scholar] [CrossRef]
- Rizvi, S.J.; Cyriac, A.; Grima, E.; Tan, M.; Lin, P.; Gallaugher, L.A.; McIntyre, R.S.; Kennedy, S.H. Depression and Employment Status in Primary and Tertiary Care Settings. Can. J. Psychiatry 2015, 60, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Stewart, W.F.; Ricci, J.A.; Chee, E.; Hahn, S.R.; Morganstein, D. Cost of Lost Productive Work Time among US Workers with Depression. JAMA 2003, 289, 3135–3144. [Google Scholar] [CrossRef]
- Van Der Noordt, M.; Ijzelenberg, H.; Droomers, M.; Proper, K.I. Health effects of employment: A systematic review of prospective studies. Occup. Environ. Med. 2014, 71, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Theorell, T.; Hammarström, A.; Aronsson, G.; Bendz, L.T.; Grape, T.; Hogstedt, C.; Marteinsdottir, I.; Skoog, I.; Hall, C. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015, 15, 1–14. [Google Scholar] [CrossRef] [PubMed]

| Variables | Male (No., Col%, Row%) (n = 1328, 32.5%) | Female (No., Col%, Row%) (n = 2751, 67.4%) | p-Value a | Total Number (No., %) |
|---|---|---|---|---|
| Age (years) | 0.0392 | |||
| 18-44 | 554 (41.7%, 34.4%) | 1055 (38.4%, 65.6%) | 1609 (39.5%) | |
| 45-64 | 774 (58.3%, 31.3%) | 1696 (61.7%, 68.7%) | 2470 (60.6%) | |
| Mean ± SD | 46.1 (± 11.4) | 47.5 (± 9.9) | 0.0097 b | 47.0 (± 10.4) |
| Education years | 0.0246 | |||
| Less than 9 | 909 (68.5%, 31.5%) | 1977 (71.9%, 68.5%) | 2886 (70.8%) | |
| 9 and above | 419 (31.6%, 35.1%) | 774 (28.1%, 64.9%) | 1193 (29.3%) | |
| Work Status | <0.0001 | |||
| Employment | 191 (14.4%, 44.4%) | 239 (8.7%, 55.6%) | 430 (10.5%) | |
| Unemployment | 1137 (85.6%, 31.2%) | 2512 (91.3%, 68.8%) | 3649 (89.5%) | |
| Family Economic Status | 0.087 | |||
| General | 1282 (96.5%, 32.8%) | 2624 (95.4%, 67.2%) | 3906 (95.8%) | |
| Middle low & Low | 46 (3.5%, 26.6%) | 127 (4.6%, 73.4%) | 173 (4.2%) | |
| Urbanization level | 0.6353 | |||
| Suburban & Rural | 611 (46.0%, 32.9%) | 1244 (45.2%, 67.1%) | 1855 (45.5%) | |
| Urban | 717 (54.0%, 32.2%) | 1507 (54.8%, 67.8%) | 2224 (54.5%) | |
| Severity of disability c | 0.1097 | |||
| Mild | 732 (55.1%, 31.2%) | 1611 (58.6%, 68.8%) | 2343 (57.4%) | |
| Moderate | 488 (36.8%, 34.5%) | 927 (33.7%, 65.5%) | 1415 (34.7%) | |
| Severe & Profound | 108 (8.1%, 33.6%) | 213 (7.7%, 66.4%) | 321 (7.9%) |
| Variables | Employment (No., Col%, Row%) (n = 430, 10.5%) | Unemployment (No., Col%, Row%) (n = 3649, 89.5%) | p value a |
|---|---|---|---|
| Sex | <0.0001 | ||
| Male | 191 (44.4%, 14.4%) | 1137 (31.2%, 85.6%) | |
| Female | 239 (55.6%, 8.7%) | 2512 (68.8%, 91.3%) | |
| Age (years) | <0.0001 | ||
| 18–44 | 247 (57.4%, 15.4%) | 1362 (37.3%, 84.7%) | |
| 45–64 | 183 (42.6%, 7.4%) | 2287 (62.7%, 92.6%) | |
| Total (mean ± SD) | 42.8 (± 8.6) | 47.5 (± 10.5) | <0.0001 b |
| Education years | 0.1106 | ||
| Less than 9 | 290 (67.4%, 10.1%) | 2596 (71.1%, 90.0%) | |
| 9 and above | 140 (32.6%, 11.7%) | 1053 (28.9%, 88.3%) | |
| Family Economic Status | 0.1146 | ||
| General | 418 (97.2%, 10.7%) | 3488 (95.6%, 89.3%) | |
| Middle low and low | 12 (2.8%, 6.9%) | 161 (4.4%, 93.1%) | |
| Urbanization level | 0.1988 | ||
| Suburban and Rural | 183 (42.6%, 9.9%) | 1672 (45.8%, 90.1%) | |
| Urban | 247 (57.4%, 11.1%) | 1977 (54.2%, 88.9%) | |
| Severity of disability | <0.0001 | ||
| Mild | 297 (69.1%, 12.7%) | 2046 (56.1%, 87.3%) | |
| Moderate | 116 (27.0%, 8.2%) | 1299 (35.6%, 91.8%) | |
| Severe and Profound | 17 (4.0%, 5.3%) | 304 (8.3%, 94.7%) |
| Employment Group (Mean ± SD) | Unemployment Group (Mean ± SD) | |||||
|---|---|---|---|---|---|---|
| WHODAS 2.0 | Year 1 | Year 3 | Deltac,* | Year 1 | Year 3 | Delta |
| Cognition | 28.4 ± 20.0 | 23.6 ± 18.3 b | −4.9 ± 22.3 | 41.6 ± 23.7 a | 37.3 ± 22.0 b | −4.4 ± 27.1 c |
| Mobility | 10.9 ± 16.1 | 9.0 ± 15.6 b | −1.9 ± 19.0 | 23.5 ± 24.0 a | 21.6 ± 24.1 b | −1.8 ± 28.4 c |
| Self-care | 5.5 ± 10.7 | 4.3 ± 9.0 | −1.2 ± 12.8 | 12.0 ± 17.8 a | 13.4 ± 19.1 b | 1.4 ± 23.0 c |
| Getting along | 37.6 ± 25.7 | 36.8 ± 24.6 | −0.8 ± 28.1 | 51.9 ± 27.6 a | 50.4 ± 25.7 b | −1.5 ± 31.4 |
| Life activities | 24.7 ± 26.0 | 23.4 ± 24.6 | −1.3 ± 31.7 | 44.2 ± 30.9 a | 42.2 ± 29.5 b | −2.1 ± 36.9 c |
| Participation | 38.9 ± 22.4 | 31.3 ± 19.5 b | −7.6 ± 23.4 | 50.0 ± 23.1 a | 43.1 ± 21.6 b | −6.9 ± 26.2 |
| Summary | 26.4 ± 16.0 | 22.7 ± 14.8 b | −3.7 ± 16.5 | 39.0 ± 19.1 a | 35.7 ± 18.4 b | −3.3 ± 21.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiang, Y.-C.; Liou, T.-H.; Lee, H.-C.; Escorpizo, R. Using WHODAS 2.0 to Assess Functional Impairment in People with Depression: Should Employment Receive More Attention? Int. J. Environ. Res. Public Health 2021, 18, 4552. https://doi.org/10.3390/ijerph18094552
Chiang Y-C, Liou T-H, Lee H-C, Escorpizo R. Using WHODAS 2.0 to Assess Functional Impairment in People with Depression: Should Employment Receive More Attention? International Journal of Environmental Research and Public Health. 2021; 18(9):4552. https://doi.org/10.3390/ijerph18094552
Chicago/Turabian StyleChiang, Yu-Chen, Tsan-Hon Liou, Hsin-Chien Lee, and Reuben Escorpizo. 2021. "Using WHODAS 2.0 to Assess Functional Impairment in People with Depression: Should Employment Receive More Attention?" International Journal of Environmental Research and Public Health 18, no. 9: 4552. https://doi.org/10.3390/ijerph18094552
APA StyleChiang, Y.-C., Liou, T.-H., Lee, H.-C., & Escorpizo, R. (2021). Using WHODAS 2.0 to Assess Functional Impairment in People with Depression: Should Employment Receive More Attention? International Journal of Environmental Research and Public Health, 18(9), 4552. https://doi.org/10.3390/ijerph18094552







