Abstract
Despite adverse pregnancy outcomes for women with overweight or obesity, preconception guidelines for achieving optimal wellness for women contemplating pregnancy regarding the risks of overweight or obesity are varied based upon national affiliation. The aim of this study was to synthesize the best evidence related to preconception counseling and care focused on overweight or obesity provided to women of reproductive age. An integrative review of original studies was conducted. PubMed, Cumulative Index in Nursing and Allied Health Literature, Ovid, Scopus, Web of Science, and Embase were included. Full-text, data-based articles were searched from 2009 to 2018, with reviews and synthesis completed in 2019 and 2020. Of 8703 initial articles, 31 articles remained in the review. Quality assessment and level of evidence were evaluated based upon criteria from the Joanna Briggs Institute and the Johns Hopkins Nursing Evidence-Based Practice Quality Guide. The level of evidence for the majority of studies was non-experimental but they were of good quality with appropriate methods, samples and relevant results. Limited attention and interest in preconception counseling regarding risks of overweight or obesity by health care professionals were noted, which may contribute to women’s unawareness of these risks on preconception health.
1. Introduction
Adequate preconception counseling is important for women who are overweight or obese and are planning to become pregnant. Excess weight in the preconception period can influence fecundability (average per-cycle probability of conception), as well as the trajectory of metabolic changes during pregnancy and in the postpartum period due to inflammation, dyslipidemia and insulin resistance [1,2,3]. Overweight and obesity in the preconception period increase the risk of metabolic dysfunction, causing alterations in placental function, fetal vascular formation and gene expression during pregnancy [4,5]. Since there is an escalation of overweight and obesity in women of reproductive age, as well as the effects of delaying pregnancy until later in life, more women become vulnerable to obesity-related pregnancy complications and chronic disorders after the birth such as hypertensive disorders, impaired glucose tolerance and type 2 diabetes [6,7,8].
Metabolic processes (e.g., basal metabolic rate, protein usage and storage, triglyceride synthesis, hemodynamic changes) become altered during pregnancy to provide an optimal supply of glucose and protein to mothers and fetuses [1]. These alterations may extend to the 4th trimester (12 weeks post-delivery) or later in life with increases in the risks for complications, such as maternal stroke or delivery of macrosomic infants [9]. A continuum of care from preconception to the 4th trimester for women who are overweight or obese is essential [10,11]. Despite the known risks related to excess weight in women throughout preconception, during pregnancy and the postpartum period, little is known regarding current preconception counseling focused on overweight and obesity provided to women of reproductive age. According to the only systematic review retrieved on preconception intervention programs for improving pregnancy outcomes in women who are overweight or obese, no RCTs are available, limiting the best practice evidence for this growing population [12].
The number of pregnant women who are overweight or obese has increased in both high and middle income countries based upon country-level data collected from the World Health Organization, the World Bank and the Food and Agricultural Organization [8]. For example, in the United States, 41.2% of women aged 20 years old and older were obese in 2015–2016 [13] and about half of women (48%) start their pregnancy being overweight or obese [14]. In response to the obesity epidemic in childbearing women, the Centers for Disease Control and Prevention (CDC) and the Institute of Medicine (IOM) in the United States, and the National Institute for Health and Care Excellence (NICE) in the United Kingdom have focused on overweight and obesity in preconception health since 2006 [15,16,17,18]. The NICE recommends that women should be counseled to have a body mass index (BMI) of less than 25.0 kg/m2 when starting a pregnancy, and the Royal Australia College of General Practitioners (RACGP) and the CDC also indicate the importance of preconception care to achieve a healthy weight and lifestyle at the first prenatal visit [19,20]. Newborns of women who are obese are at a high risk for developing neural tube defects [21,22]. As a preventive measure, taking a folic acid supplement is recommended during the childbearing period, although a specific dosage for women with excess weight varies depending on national affiliation [6,20]. The Royal Australian and New Zealand College of Obstetricians and Gynaecolgists (RANZCOG), Royal College of Obstetricians and Gynaecologists (RCOG) and the Joint Centre for Maternal and Child Enquiries (CMACE) in the United Kingdom recommend increasing supplementation of folic acid to 5 mg instead of 400 mcg. The Institute of Obstetricians and Gynaecologists (IOG) in Ireland concurs with the recommendation of the RCOG and CMACE. The American College of Obstetricians and Gynecologists (ACOG) and the CDC, however, do not recommend doses of folic acid greater than 400 mcg, stating evidence does not support a greater dose [6,20].
Studies show that women who are overweight or obese have lower levels of vitamin D and calcium, which are associated with fetal growth, maternal depressive moods, and maternal and fetal bone formation requirements [23,24,25]. Thus, the RCOG and CMACE in the United Kingdom and the IOG in Ireland, but not the ACOG, include these micronutrients in preconception counseling, although recommendations for sufficient and safe amounts for women who are overweight or obese remain unanswered [6,25]. Similarly, RANZCOG recommends daily supplementation of iodine that is not included in other guidelines, including ACOG.
Systematic reviews have shown there are missed opportunities to provide lifestyle interventions to address pregnancy risks in women who are overweight or obese, as well as those who may be prone to excess weight gain in the preconception period and pregnancy [26,27,28]. A healthy, balanced, diet without excessive caloric intake during the preconception period is important to prevent teratogenesis and gestational diabetes and to generate normal fetal programming of the adrenal–pituitary–hypothalamic axis during gestation [11]. Regular physical activity in the preconception period may lead to gestational diabetes prevention, improved fecundability, and motivation to continuously exercise during pregnancy [12,28,29]. At least one-BMI-unit weight loss or 10% or more of weight loss may be beneficial to improve fecundability and reduce adverse pregnancy outcomes in women [11,30].
Despite the potential benefits of preconception health interventions focusing on the effects of overweight or obesity in women of reproductive age, current preconception interventions delivered in public health and community settings are mostly focused on general health topics such as drinking cessation, taking multivitamin or folic acid supplements, and immunizations, rather than on obesity risk [31,32]. Furthermore, interventions to improve maternal and fetal cardiometabolic health are usually initiated after conception and results are often unsuccessful [32,33]. There is a great need for obesity-specific preconception counseling to reduce risk associated with excess weight prior to and during pregnancy.
The aim of this study was to synthesize the best evidence related to preconception counseling and care focused on the effects of overweight or obesity provided to women of reproductive age.
2. Materials and Methods
2.1. Design
An integrative literature review was conducted using the process as described by Whittemore and Knafl that allows for the combination and synthesis of both non-experimental and experimental design studies [34]. This process includes clarity in problem identification, literature review, evaluation of the data from empirical reports, data analysis from primary resources, and the final presentation of the summary of the findings that have pragmatic relevance, particularly for a practice discipline [34]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were incorporated for presenting information retrieved from the integrated review [35].
2.2. Search Methods
The electronic databases PubMed, Cumulative Index in Nursing and Allied Health Literature (CINAHL), Ovid, Scopus, Web of Science, and Embase were used for the search. Articles were retrieved that were published over a ten-year period from 2009 to 2018 with article reviews occurring in 2019 and final synthesis in 2020. A combination of search terminologies related to the integrative review topic was used (i.e., women of reproductive age; young women; childbearing women), preconception, education (i.e., counseling; education; intervention), and lifestyle (i.e., lifestyle modification; lifestyle intervention; healthy lifestyle; diet; physical activity; exercise; weight loss). To conduct a comprehensive review of the literature on preconception counseling, the terms of overweight or obesity were not included in the search terminology to prevent the inclusion of studies that included only women with overweight or obesity. Rather, the investigators manually reviewed each article during the title, abstract and full-text review steps to check the eligibility of studies that addressed overweight or obesity prior to pregnancy.
2.3. Inclusion and Exclusion Criteria
The inclusion criteria for target studies were publications that addressed preconception counseling or care in women of reproductive age and were full-text, data-based articles written in English. Due to the global epidemic of obesity, studies completed both within and outside of the U.S. were included. The exclusion criteria were: (1) abstracts or conference proceedings; or (2) articles that focused on preconception counseling and care for women with preexisting diseases (e.g., cardiac problems, diabetes, and other chronic conditions). We also conducted ancestry searches of the reference lists of the included articles to find other articles for inclusion in this review. The composite search revealed a total of 8703 potential articles for review.
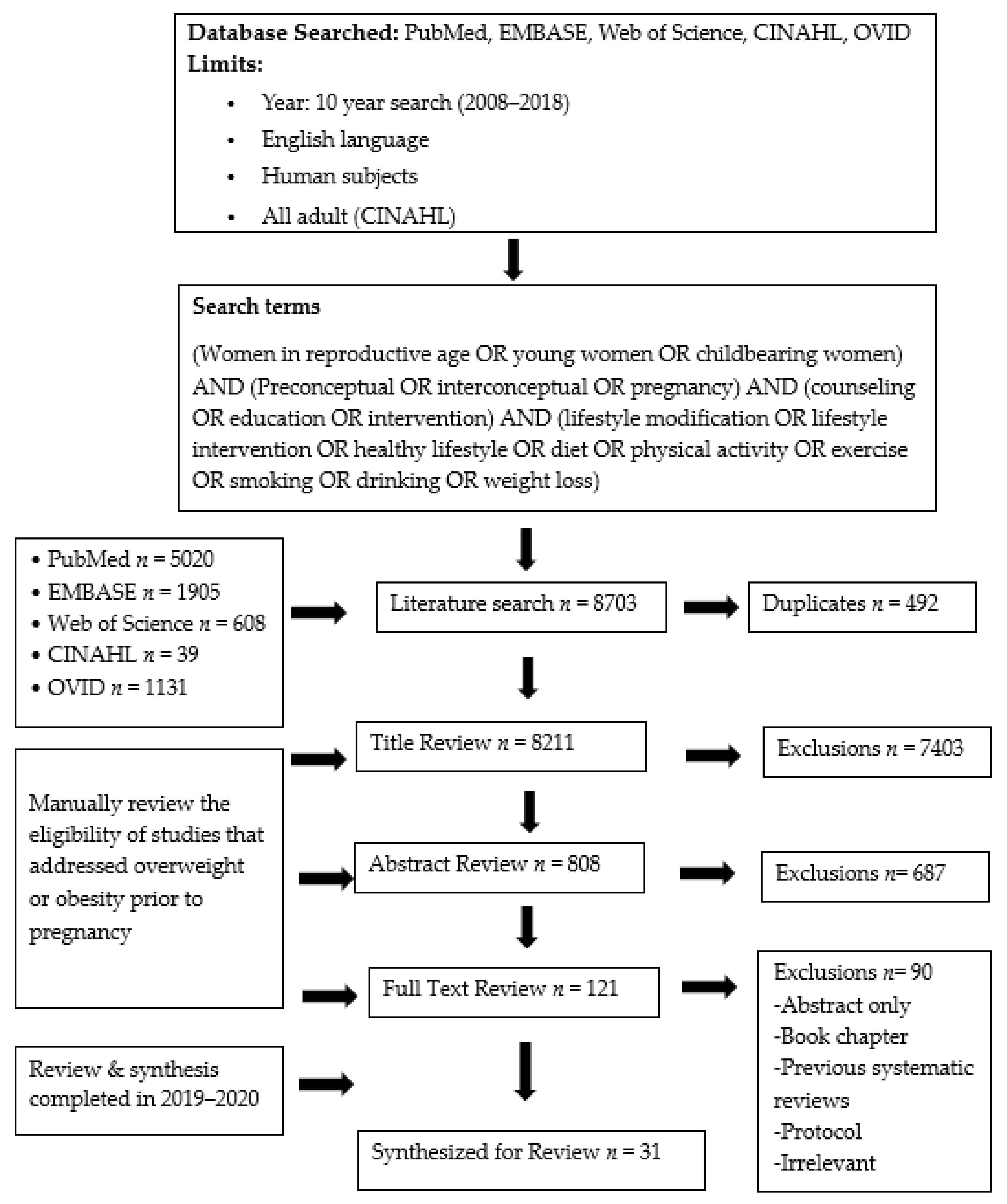
Following the search of the selected databases, teams of investigators (3 doctoral-prepared nurse researchers and 1 graduate nursing student) at 2 separate universities began the process of reviewing articles. The complete dataset of articles was split between the two respective sites. The initial screen of the articles included an examination of the title for appropriateness of content, followed by a review of abstracts and finally, a full-text review of the articles. Any duplication of articles was eliminated in the review process. Figure 1 presents the PRISMA flow diagram, numbers of the articles obtained and those excluded in each step of the review, and the final 31 full-text data-based original articles included for the synthesis of findings.
Figure 1.
PRISMA (The Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Flowchart to select articles reviewed.
2.4. Quality Appraisal
Quality assessment and grading of evidence was completed in a 2-step process. The quality of each article was determined by scoring using the appraisal checklists for either quasi-experimental studies (non-randomized) or randomized controlled trials as appropriate based upon the Joanna Briggs Institute (https://jbi.global/critical-appraisal-tools (accessed on 9 February 2019). The authors randomly selected articles that one another reviewed to check the thoroughness and quality for each other and to determine inter-rater consistency for inclusion of articles for full review. The level of evidence for grading the published studies in the full-text review was confirmed by two investigators based upon the Johns Hopkins Nursing Evidence-Based Practice Quality Guide from Level I (randomized controlled trials), Level II (quasi-experimental studies), Level III (non-experimental studies; quasi-experimental and non-experimental studies), Level IV (clinical practice guidelines; position statements) to Level V (integrative reviews, case reports, experiential evidence of national experts) [36]. Quality rating was indicated as high, good or low depending on the adequacy of the study designs, sample sizes and appropriateness of study conclusions. Descriptions of the ratings are as follows:
- A.
- High quality: Consistent, generalizable results; sufficient sample size; adequate control; definitive conclusions; consistent recommendations based on comprehensive literature review that includes thorough reference to scientific evidence.
- B.
- Good quality: Reasonably consistent results; sufficient sample size; some control, fairly definitive conclusions; consistent recommendations based on fairly comprehensive literature review that includes some reference to scientific evidence.
- C.
- Low quality or major flaws: Little evidence with inconsistent results; insufficient sample size; conclusions cannot be drawn [36].
2.5. Data Abstraction
The 31 articles were grouped based upon the following content areas that emerged during synthesis of the findings and major categories of themes that align with the study purpose. The categories include the following: (1) knowledge of preconception health in women of reproductive age; (2) lifestyle and weight management behaviors and potential impact on maternal and neonatal health; (3) preconception counseling provided by health care professionals; and (4) preconception educational interventions for childbearing women. The categories are not mutually exclusive since some studies included findings relative to more than one category.
2.6. Synthesis
Once articles were identified for the final review, a doctoral-prepared nurse researcher and the PhD student at one-site rechecked the eligibility of the articles selected. A nurse researcher and the student each independently reviewed the study purpose, quality and findings of each study to identify a thematic category that aligned with the purpose of this review. Once themes were identified with associated studies, a second nurse researcher reviewed and validated the synthesis of the thematic categories.
3. Results
The results of the data abstraction and findings related to the major categories of themes in the data are described in the following section. A summary of information from full-text articles is included in Table 1.

Table 1.
Summary of full-text, data-based articles written in English.
3.1. Knowledge of Preconception Health in Women of Reproductive Age
Childbearing women’s awareness and knowledge of preconception health were examined by seven studies [29,37,38,39,40,41,42] and women’s perception of body size was examined by two studies [38,43]. Participants in these studies were recruited from clinics or primary care settings [38,39,40,42,43] and internet-based platforms [37,41], while one study reviewed the information accuracy of preconception health in websites using search terms developed by interviews with women and health care professionals [29].
Overall, women’s preconception health knowledge on folic acid supplementation, vaccination, mother’s age for positive health outcomes, benefits of maintaining a normal weight, smoking cessation, sexually transmitted infection screening and avoidance of substance use was high [37,39,40,41,42], and knowledge regarding the risk in obesity and avoiding high-caloric food items during pregnancy was low to moderate [29,38,39,41,42]. Many women were not aware of the benefits of physical activity during pregnancy and considered regular exercise as potentially harmful to their unborn baby [42].
Women who were overweight inaccurately perceived their body size and/or rarely understood the impact of weight on pregnancy outcomes [38,41,43]. Women with obesity versus overweight had higher intentions to lose weight [43], and the intention of overweight women to engage in behavioral changes was not high (only 53% women intended to make lifestyle changes) [42].
In research on the use of the internet to obtain information on preconception, women with excess weight sought information on “how to get pregnant”, rather than how to have a “healthy” pregnancy [29]. Risk related to obesity was rarely selected during internet searches by the women which may indicate the unawareness of the obesity-related pregnancy risk. The most common searches were folic acid supplementation, rubella vaccination, smoking cessation, preconception counseling in general by health care professionals, and doctor’s advice for medication, while topics related to managing weight such as doing regular exercise were rarely included [29].
Women were not aware of and did not accurately evaluate their overweight and obesity risks on reproductive health [43]. Their perceived health was viewed mostly as good or very good, and consulting with health care providers to lose weight was often interpreted as being rude, accusing and unrealistic advice [43,44]. The time to start to worry about health was usually noted to occur after conception [45]. While women were informed about what is needed for an optimal pregnancy experience and delivery of a healthy infant (e.g., avoidance of excessive weight gain during pregnancy and alcohol consumption, taking folic acid supplements, and healthy nutrition), they reported a lack of understanding of the reasons, which led to poor adherence [43,45].
3.2. Lifestyle and Weight Management Behaviors and Potential Impact on Maternal and Neonatal Health
Six studies examined healthy lifestyle and weight management behaviors including diet, exercise, and weight loss strategies in women of childbearing age [43,46,47,48,49,50]. Women who wanted to become pregnant practiced diverse weight management strategies, although some of them were unhealthy [47]. Examples of unhealthy behaviors were smoking, fast food and soda consumption and fewer servings of vegetables [47]. Weight loss strategies were taking diet pills, diuretics, and vomiting and fasting for 24 h or more. Confidence in losing weight was low among women who were overweight or obese [43].
Women did exercise, although the majority of women (49.6–78.7%) did not meet current exercise recommendations of 30 min of exercise per day, five days per week [43,46,49]. Intention to adhere to exercise recommendations was low, especially in women who were overweight compared to those with normal weight or obese [43]. Likewise, a poor rate of adherence to following dietary recommendations was also found [46,47,50]. According to Berenson et al. [47], many women did not meet the daily recommended intake of fruits and vegetables: 76% consumed less than one serving of fruit, 90% consumed less than one serving of green salad, and 72.9% consumed less than one serving of vegetables. Similarly, Inskip et al. [46] found that about 53% of participants did not comply with the recommended intake of fruits and vegetables. Women with obesity showed a tendency to consume high amounts of meats and sweets, which are risk factors of developing gestational diabetes (RR of 2.08; 95% CI = 1.18−3.62) [50].
Maternal weight status and lifestyle behaviors in the preconception period influenced maternal and neonatal health according to the findings of four studies. These included online surveys [51] and national prospective cohorts [52,53,54]. Fecundability was decreased in women with BMI ≥35 or women with a waist circumference above 36 inches or who had gained ≥40 pounds since the age of 17 years [51]. Physical activity, especially vigorous physical activity during the preconception period, increased fecundability in women who were overweight or obese [51]. However, it did not prevent pre-eclampsia [53] or delivery of abnormal birth weight infants [52].
Both the time of developing overweight or obesity in women and their race were found to have effects on neonatal health [52]. While being adolescent mothers who were overweight or obese during pregnancy increased the risk for having infants with low birth weight (OR of 3.89; 95% CI = 1.26–12.04, with the OR increasing after adjusting for confounders and prenatal mediators to 4.59; 95% CI = 1.26–16.70), adult women with overweight or obesity demonstrated an increased risk for infant macrosomia (OR of 1.56; 95% CI = 1.02–2.38). A later study by Strutz et al. [54] showed a moderation effect by race. African American women that were overweight or obese had a higher risk of delivering an infant with macrosomia (OR of 3.83; 95% CI = 1.02–14.36) compared to other racial/ethnic cohorts.
3.3. Preconception Counseling Provided by Health Care
Professionals
There were seven studies that examined the effects of preconception counseling by health care professionals on women’s health and behaviors [15,17,18,40,45,48,55]. Preconception counseling encouraged women to undertake preventive and proactive health behaviors in order to have a healthy pregnancy (e.g., daily consumption of multivitamins prior to conception, first-trimester entry into prenatal care). However, benefits were not always evident in behaviors such as diet and exercise in women who were overweight or obese [17,18,40,48]. Potential reasons for this were the passive attitudes of health care providers to deliver preconception counseling and their lack of capability to provide client-centered counseling [40,45].
Less than 20% of women reported they received a health care provider’s advice on healthy behaviors during the preconception period [55]. Although counseling regarding smoking or drinking was offered more to women who were overweight or obese compared to normal weight or underweight women, the content was not obesity-specific and advice on maintaining a healthy BMI occurred more during pregnancy, not in the preconception period [15]. Women were skeptical about advice to lose weight to improve preconception health and had low confidence in changing their lifestyle during the preconception period. Additionally, health care professionals did not play an active role in changing women’s perception and behaviors [40,43,45], despite an unmet need for ways to obtain a healthy weight and maintain a physically active lifestyle.
Health care providers often reported time restrictions, low policy priority, and a “not my responsibility” attitude to providing preconception counseling [43,45,55]. General practitioners reported that preconception care was not their practice area and that it should be a targeted public health campaign or delivered by a midwife or nurse practitioner. They indicated that peer education would be better than education by health care providers [45,55]. Outsourcing education programs such as community programs, online education, or mobile applications that focus on diet and exercise were listed by health care professionals as resources they wanted to recommend to clients that need to lose weight [43]. Although there were concerns about general practitioners providing preconception care since they may lack information in reproductive health [45], women visiting an OB-GYN were found to be less likely to receive diet and exercise counseling compared to women visiting a non-OB-GYN provider [17].
About two-thirds of women reported positive feedback on receiving guidance from their health care professionals that specifically addressed pregnancy-related risk regarding alcohol consumption, tobacco use, taking certain medications, and obtaining HIV testing [40,48]. However, in other research, about half of women (49%) reported no preconception health advice was given by their health care providers [55]. Due to limited chances to obtain preconception health advice from health care professionals, women used the internet, friends and family, books and media to obtain information related to preconception health [44,55].
Childbearing women showed a desire for preconception counseling and care from health care professionals, regardless of culture, age or weight status [43,44,45]. More women (75%) wanted to receive preconception care in the future and two-thirds of them wanted to have multiple counseling sessions [44]. However, general advice on healthy lifestyle behaviors (e.g., diet or exercise) did not influence behavioral change in women [48,55]. Unfortunately, due to a lack of awareness of the importance of preconception health, obtaining information on this topic remains a low priority for some women. A dismissive attitude of health care professionals has contributed to a diminished focus on preconception health for childbearing women with overweight or obesity [18].
3.4. Preconception Educational Interventions for Childbearing Women
Nine studies examined the effects of interventions on preconception education [29,39,56,57,58,59,60,61,62]. Changes in knowledge of preconception health, self-efficacy on behavioral change and actual behavioral change were evaluated in response to varied intervention approaches: individualized education interventions [37,39,56,57,58,60,61,62], group interventions [59] and eHealth interventions [37,61]. Despite the acknowledgement of obesity’s risk on having a healthy pregnancy, some studies did not include obesity-related measures as preconception intervention outcomes [39,57,61].
Most interventions were focused on general preconception education such as taking folic acid supplementation and alcohol cessation [37,39,57,58,59,61]. Approximately half of the studies were focused on the reduction of obesity risks to have a healthy pregnancy [37,56,60,61]. Only two studies emphasized the significance of a healthy lifestyle in women planning to become pregnant [59,62].
Increased preconception knowledge was associated with actual behavior changes in some studies. Once preconception knowledge was improved, improved behavioral changes were found in folic acid consumption, vaccinations, smoking and drinking, and antenatal check-ups [37,56].
Interventions on weight loss during the preconception period revealed different methods and inconsistent findings [37,56,59,60,62]. For instance, women who were overweight or obese experiencing gestational diabetes in their previous pregnancy lost their weight after one-year follow-up as the result of a 4-week lifestyle intervention prior to a subsequent pregnancy [60]. Women who received a motivational interviewing (MI) intervention lost more weight than those not receiving the MI component of the intervention prior to fertility treatment (9.3 kg vs. 7.3kg, p = 0.01) [63]. In other studies, results were not adequate. Women who were overweight or obese and received interventions about dieting or exercising to lose weight before pregnancy did not show any differences in behavioral or weight changes compared to those who did not [48,62], while the advice on smoking and taking vitamins before pregnancy successfully aided in behavior change [48]. Despite the failure of weight loss through lifestyle modification in a 6-month intervention in the preconception period completed by van Oers et al. [62], the women that did not gain additional weight, compared to those that gained weight, showed lower hypertensive complications.
4. Discussion
Screening of metabolic health risks in the preconception period aids in preventing the negative effects of obesity on maternal health and fetal development [28,64,65]. Currently, there are no specific evidence-based clinical guidelines in the US for women who are overweight or obese regarding recommendations for healthy weight, diet and physical activity during the preconception period [6,20,28]. Professional organizations such as the American Diabetes Association (ADA), American College of Obstetricians and Gynecologists (ACOG), American Heart Association (AHA) and Academy of Nutrition and Dietetics Foundation have released recommendations, which do not include adequate obesity-specific pregnancy risks in the preconception period [11,64,66,67]. The lay public can be easily confused and ignore the importance of preconception health and the effect of excess weight prior to conception.
This integrative review adds information on an under-researched health concern regarding what is known about knowledge and interventions focused on obesity-related pregnancy risks during preconception. It provides evidence on the significance of addressing obesity-related pregnancy risk and the benefits of exercise and healthy nutrition. Evidence on risks related to the use of diet pills and diuretics to promote weight loss and the absence of a diet comprised of the recommended amounts of fruits and vegetables in the preconception period supports the importance of including nutritionists or dieticians in preconception counseling. Inconsistent guidelines and deficient knowledge on the value of a healthy lifestyle during preconception, exist due to greater emphasis on women’s interest in seeking information on “how to become pregnant” and not on how to have a “healthy pregnancy”. Current research supports the need for interventions that target specific high-risk groups that experience overweight or obesity, such as during adolescence and those delaying pregnancy.
The level of evidence for the majority of studies in this integrative review was non-experimental in design, but they were of good quality with appropriate methods, samples and relevant results. Although the review process included manual examination of each article to ensure that the study addressed the risks of overweight or obesity prior to pregnancy, there is the possibility that this review was not exhaustive.
Major findings included that preconception physical activity and weight loss decreased the risk for developing gestational diabetes and hypertensive disorders in pregnancy. However, there remains a dearth of randomized, controlled studies to validate effective practice recommendations during preconception [12]. The findings of this review are primarily based on descriptive studies and should be interpreted with caution. Therefore, further investigations are needed to identify the effects of social determinants on preconception health, which are essential to design effective interventions [26,27,54].
5. Conclusions
Evidence from this review supports women’s unawareness of the risks related to overweight or obesity prior to pregnancy and the low attention paid to preconception counseling by health care professionals [40,45]. One possible explanation is the minimal emphasis on guidelines or standards of care for women who are overweight or obese and the lack of synthesis of best practices based upon well-controlled interventions for women at risk for gaining excess weight during the preconception period. Nurses, nurse midwives, nurse practitioners, and other primary care providers can take the lead in addressing the priority for establishing guidelines for standards of care for preconception counseling in this area. In particular, the collaboration of nurse researchers in the conduct of well-designed studies to further develop the best evidence to prevent overweight or obesity and address priorities of care for women who have elevated BMI prior to pregnancy is needed. Nurses in advanced practice roles can offer their voices by engaging with national and international organizations focused on women’s health for policy implementation in establishing universal standards of care related to overweight or obesity risks during preconception for ensuring a healthy pregnancy. Strategies also include partnering with nursing and other health leaders who are members of the World Health Organization’s Collaborating Centers for Nursing and Midwifery to unify a shared vision for addressing the epidemic of overweight or obesity on maternal and infant outcomes through coordinated efforts in preconception care.
Author Contributions
Conceptualization, E.S.C., B.J.B., and M.S.F.; methodology, E.S.C., M.J.S., B.J.B. and M.S.F.; validation, E.S.C. and M.S.F.; methodology, E.S.C., M.S.F., B.J.B. and M.S.F.; resources, E.S.C. and M.S.F.; data curation.; writing—original draft preparation, E.S.C., M.J.S., B.J.B. and M.S.F.; writing—review and editing, methodology, E.S.C., B.J.B. and M.J.S.; visualization, E.S.C., M.J.S. and M.S.F.; supervision, E.S.C. and M.S.F.; project administration, E.S.C.; funding acquisition, M.S.F. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Lewis Endowment Fund at the Byrdine F. Lewis College of Nursing and Health Professions, Georgia State University.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request to the first or corresponding author.
Acknowledgments
The authors are sincerely grateful to Jihye Jeong, Sunghyun Yang, and Hyesun Shim, who were former students at the Chungnam National University College of Nursing for their support on the beginning of the work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Blackburn, S.T. Maternal, Fetal, & Neonatal Physiology: A Clinical Perspective, 4th ed.; Elsevier: Philadelphia, PA, USA, 2013. [Google Scholar]
- Cnattingius, S.; Villamor, E. Weight change between successive pregnancies and risks of stillbirth and infant mortality: A nationwide cohort study. Lancet 2016, 387, 558–565. [Google Scholar] [CrossRef]
- Correa, A.; Marcinkevage, J. Prepregnancy obesity and the risk of birth defects: An update. Nutr. Rev. 2013, 71 (Suppl. 1), S68–S77. [Google Scholar] [CrossRef]
- Bozkurt, L.; Gobl, C.S.; Hormayer, A.T.; Luger, A.; Pacini, G.; Kautzky-Willer, A. The impact of preconceptional obesity on trajectories of maternal lipids during gestation. Sci. Rep. 2016, 6, 29971. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, K.L.; Brennan, L.; Rath, A.; Maguire, O.C.; Smith, T.; McAuliffe, F.M. Gestational weight gain in obese pregnancy: Impact on maternal and foetal metabolic parameters and birthweight. J. Obstet. Gynaecol. 2018, 38, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Kominiarek, M.A.; Chauhan, S.P. Obesity Before, During, and After Pregnancy: A Review and Comparison of Five National Guidelines. Am. J. Perinatol. 2016, 33, 433–441. [Google Scholar] [CrossRef]
- American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020, 43, S183–S192. [Google Scholar] [CrossRef]
- Chen, C.; Xu, X.; Yan, Y. Estimated global overweight and obesity burden in pregnant women based on panel data model. PLoS ONE 2018, 13, e0202183. [Google Scholar] [CrossRef]
- Zambrano, M.D.; Miller, E.C. Maternal Stroke: An Update. Curr. Atheroscler. Rep. 2019, 21, 33. [Google Scholar] [CrossRef]
- Delissaint, D.; McKyer, E.L.J. A Systematic Review of Factors Utilized in Preconception Health Behavior Research. Health Educ. Behav. 2011, 38, 603–616. [Google Scholar] [CrossRef]
- Stang, J.; Huffman, L.G. Position of the Academy of Nutrition and Dietetics: Obesity, Reproduction, and Pregnancy Outcomes. J. Acad. Nutr. Diet. 2016, 116, 677–691. [Google Scholar] [CrossRef]
- Opray, N.; Grivell, R.M.; Deussen, A.R.; Dodd, J.M. Directed preconception health programs and interventions for improving pregnancy outcomes for women who are overweight or obese. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- National Center for Health Statistics. Health, United States, 2018; National Center for Health Statistics: Yattsville, MD, USA, 2019. [Google Scholar]
- Dudenhausen, J.W.; Grunebaum, A.; Kirschner, W. Prepregnancy body weight and gestational weight gain-recommendations and reality in the USA and in Germany. Am. J. Obstet. Gynecol. 2015, 213, 591–592. [Google Scholar] [CrossRef]
- Bye, A.; Shawe, J.; Stephenson, J.; Bick, D.; Brima, N.; Micali, N. Differences in pre-conception and pregnancy healthy lifestyle advice by maternal BMI: Findings from a cross sectional survey. Midwifery 2016, 42, 38–45. [Google Scholar] [CrossRef]
- Yamamoto, A.; McCormick, M.C.; Burris, H.H. US provider-reported diet and physical activity counseling to pregnant and non-pregnant women of childbearing age during preventive care visits. Matern. Child Health J. 2014, 18, 1610–1618. [Google Scholar] [CrossRef] [PubMed]
- Williams, L.; Zapata, L.B.; D’Angelo, D.V.; Harrison, L.; Morrow, B. Associations between preconception counseling and maternal behaviors before and during pregnancy. Matern. Child Health J. 2012, 16, 1854–1861. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Posner, S.F.; Biermann, J.; Cordero, J.F.; Atrash, H.K.; Parker, C.S.; Boulet, S.; Curtis, M.G.; CDC/ATSDR Preconception Care Work Group; Select Panel on Preconception Care. Recommendations to improve preconception health and health care—United States: A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm. Rep. 2006, 55, 1–23. [Google Scholar] [PubMed]
- Lang, A.Y.; Boyle, J.A.; Fitzgerald, G.L.; Teede, H.; Mazza, D.; Moran, L.J.; Harrison, C. Optimizing preconception health in women of reproductive age. Minerva Ginecol. 2018, 70, 99–119. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Planning for Pregnancy. Available online: cdc.gov/preconception/planning.html (accessed on 4 January 2019).
- Maffoni, S.; De Giuseppe, R.; Stanford, F.C.; Cena, H. Folate status in women of childbearing age with obesity: A review. Nutr. Res. Rev. 2017, 30, 265–271. [Google Scholar] [CrossRef]
- Rasmussen, S.A.; Chu, S.Y.; Kim, S.Y.; Schmid, C.H.; Lau, J. Maternal obesity and risk of neural tube defects: A metaanalysis. Am. J. Obstet. Gynecol. 2008, 198, 611–619. [Google Scholar] [CrossRef]
- McKay, J.; Ho, S.; Jane, M.; Pal, S. Overweight & obese Australian adults and micronutrient deficiency. BMC Nutr. 2020, 6, 12. [Google Scholar] [CrossRef]
- Mohaddesi, H.; Saei Ghare Naz, M.; Najarzadeh, M.; Yeganehpour, M.; Khalkhali, H. Correlation between Depression with Serum Levels of Vitamin D, Calcium and Magnesium in Women of Reproductive Age. J. Caring Sci. 2019, 8, 117–119. [Google Scholar] [CrossRef]
- Procter, S.B.; Campbell, C.G. Position of the Academy of Nutrition and Dietetics: Nutrition and lifestyle for a healthy pregnancy outcome. J. Acad. Nutr. Diet. 2014, 114, 1099–1103. [Google Scholar] [CrossRef]
- Lan, L.; Harrison, C.L.; Misso, M.; Hill, B.; Teede, H.J.; Mol, B.W.; Moran, L.J. Systematic review and meta-analysis of the impact of preconception lifestyle interventions on fertility, obstetric, fetal, anthropometric and metabolic outcomes in men and women. Hum. Reprod. 2017, 32, 1925–1940. [Google Scholar] [CrossRef]
- Forsum, E.; Brantsæter, A.L.; Olafsdottir, A.S.; Olsen, S.F.; Thorsdottir, I. Weight loss before conception: A systematic literature review. Food Nutr. Res. 2013, 57. [Google Scholar] [CrossRef]
- Lassi, Z.S.; Bhutta, Z.A. Risk factors and interventions related to maternal and pre-pregnancy obesity, pre-diabetes and diabetes for maternal, fetal and neonatal outcomes: A systematic review. Expert Rev. Obstet. Gynecol. 2013, 8, 639–660. [Google Scholar] [CrossRef]
- Agricola, E.; Gesualdo, F.; Pandolfi, E.; Gonfiantini, M.V.; Carloni, E.; Mastroiacovo, P.; Tozzi, A.E. Does googling for preconception care result in information consistent with international guidelines: A comparison of information found by Italian women of childbearing age and health professionals. BMC Med Inform. Decis. Mak. 2013, 13. [Google Scholar] [CrossRef] [PubMed]
- Villamor, E.; Cnattingius, S. Interpregnancy weight change and risk of adverse pregnancy outcomes: A population-based study. Lancet 2006, 368, 1164–1170. [Google Scholar] [CrossRef]
- Dean, S.V.; Lassi, Z.S.; Imam, A.M.; Bhutta, Z.A. Preconception care: Closing the gap in the continuum of care to accelerate improvements in maternal, newborn and child health. Reprod. Health 2014, 11. [Google Scholar] [CrossRef]
- Brown, H.K.; Mueller, M.; Edwards, S.; Mill, C.; Enders, J.; Graves, L.; Telner, D.; Dennis, C.L. Preconception health interventions delivered in public health and community settings: A systematic review. Can. J. Public Health 2017, 108, e388–e397. [Google Scholar] [CrossRef] [PubMed]
- Catalano, P.; deMouzon, S.H. Maternal obesity and metabolic risk to the offspring: Why lifestyle interventions may have not achieved the desired outcomes. Int. J. Obes. 2015, 39, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Group, P.-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Dang, D.; Dearholt, S. Johns Hopkins Nursing Evidence-Based Practice: Model and Guidelines, 3rd ed.; Sigma Theta Tau International: Indianapolis, IN, USA, 2017. [Google Scholar]
- Agricola, E.; Pandolfi, E.; Gonfiantini, M.V.; Gesualdo, F.; Romano, M.; Carloni, E.; Mastroiacovo, P.; Tozzi, A.E. A cohort study of a tailored web intervention for preconception care. BMC Med. Inform. Decis. Mak. 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Berenson, A.B.; Pohlmeier, A.M.; Laz, T.H.; Rahman, M.; Saade, G. Obesity Risk Knowledge, Weight Misperception, and Diet and Health-Related Attitudes among Women Intending to Become Pregnant. J. Acad. Nutr. Diet. 2016, 116, 69–75. [Google Scholar] [CrossRef]
- Dunlop, A.L.; Logue, K.M.; Thorne, C.; Badal, H.J. Change in women’s knowledge of general and personal preconception health risks following targeted brief counseling in publicly funded primary care settings. Am. J. Health Promot. 2013, 27, S50–S57. [Google Scholar] [CrossRef] [PubMed]
- Harelick, L.; Viola, D.; Tahara, D. Preconception Health of Low Socioeconomic Status Women: Assessing Knowledge and Behaviors. Women’s Health Issues 2011, 21, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Pandolfi, E.; Agricola, E.; Gonfiantini, M.V.; Gesualdo, F.; Romano, M.; Carloni, E.; Mastroiacovo, P.; Tozzi, A.E. Women participating in a web-based preconception study have a high prevalence of risk factors for adverse pregnancy outcomes. BMC Pregnancy Childbirth 2014, 14. [Google Scholar] [CrossRef]
- Vause, T.D.R.; Jones, L.; Evans, M.; Wilkie, V.; Leader, A. Pre-conception health awareness in infertility patients. J. Obstet. Gynaecol. Can. JOGC 2009, 31, 717–720. [Google Scholar] [CrossRef]
- Harden, S.M.; Ramalingam, N.P.S.; Wilson, K.E.; Evans-Hoeker, E. Informing the development and uptake of a weight management intervention for preconception: A mixed-methods investigation of patient and provider perceptions. BMC Obes. 2017, 4. [Google Scholar] [CrossRef]
- Goossens, J.; Delbaere, I.; Dhaenens, C.; Willems, L.; Van Hecke, A.; Verhaeghe, S.; Beeckman, D. Preconception-related needs of reproductive-aged women. Midwifery 2016, 33, 64–72. [Google Scholar] [CrossRef]
- Bortolus, R.; Oprandi, N.C.; Morassutti, F.R.; Marchetto, L.; Filippini, F.; Agricola, E.; Tozzi, A.E.; Castellani, C.; Lalatta, F.; Rusticali, B.; et al. Why women do not ask for information on preconception health? A qualitative study. BMC Pregnancy Childbirth 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Berenson, A.B.; Pohlmeier, A.M.; Laz, T.H.; Rahman, M.; McGrath, C.J. Nutritional and Weight Management Behaviors in Low-Income Women Trying to Conceive. Obstet. Gynecol. 2014, 124, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Inskip, H.M.; Crozier, S.R.; Godfrey, K.M.; Borland, S.E.; Cooper, C.; Robinson, S.M. Women’s compliance with nutrition and lifestyle recommendations before pregnancy: General population cohort study. BMJ 2009, 338, b481. [Google Scholar] [CrossRef] [PubMed]
- Oza-Frank, R.; Kachoria, R.; Keim, S.A.; Klebanoff, M.A. Provision of specific preconception care messages and associated maternal health behaviors before and during pregnancy. Am. J. Obstet. Gynecol. 2015, 212, 372.e371–372.e378. [Google Scholar] [CrossRef] [PubMed]
- Robbins, C.; Boulet, S.L.; Morgan, I.; D’Angelo, D.V.; Zapata, L.B.; Morrow, B.; Sharma, A.; Kroelinger, C.D. Disparities in Preconception Health Indicators-Behavioral Risk Factor Surveillance System, 2013-2015, and Pregnancy Risk Assessment Monitoring System, 2013–2014. MMWR Surveill. Summ. 2018, 67, 1–16. [Google Scholar] [CrossRef]
- Schoenaker, D.A.; Soedamah-Muthu, S.S.; Callaway, L.K.; Mishra, G.D. Pre-pregnancy dietary patterns and risk of gestational diabetes mellitus: Results from an Australian population-based prospective cohort study. Diabetologia 2015, 58, 2726–2735. [Google Scholar] [CrossRef]
- McKinnon, C.J.; Hatch, E.E.; Rothman, K.J.; Mikkelsen, E.M.; Wesselink, A.K.; Hahn, K.A.; Wise, L.A. Body mass index, physical activity and fecundability in a North American preconception cohort study. Fertil. Steril. 2016, 106, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Strutz, K.L.; Richardson, L.J.; Hussey, J.M. Preconception health trajectories and birth weight in a national prospective cohort. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2012, 51, 629–636. [Google Scholar] [CrossRef]
- Tyldum, E.V.; Romundstad, P.R.; Slordahl, S.A. Pre-pregnancy physical activity and preeclampsia risk: A prospective population-based cohort study. Acta Obstet. Gynecol. Scand. 2010, 89, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Strutz, K.L.; Richardson, L.J.; Hussey, J.M. Selected preconception health indicators and birth weight disparities in a national study. Women’s Health Issues 2014, 24, e89–e97. [Google Scholar] [CrossRef]
- Stephenson, J.; Patel, D.; Barrett, G.; Howden, B.; Copas, A.; Ojukwu, O.; Pandya, P.; Shawe, J. How do women prepare for pregnancy? Preconception experiences of women attending antenatal services and views of health professionals. PLoS ONE 2014, 9, e103085. [Google Scholar] [CrossRef] [PubMed]
- Beckmann, M.M.; Widmer, T.; Bolton, E. Does preconception care work? Aust. N. Z. J. Obstet. Gynaecol. 2014, 54, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, A.L.; Dretler, A.W.; Badal, H.J.; Logue, K.M. Acceptability and potential impact of brief preconception health risk assessment and counseling in the WIC setting. Am. J. Health Promot. AJHP 2013, 27, S58–S65. [Google Scholar] [CrossRef] [PubMed]
- Elsinga, J.; de Jong-Potjer, L.C.; van der Pal-de Bruin, K.M.; le Cessie, S.; Assendelft, W.J.; Buitendijk, S.E. The effect of preconception counselling on lifestyle and other behaviour before and during pregnancy. Women’s Health Issues 2008, 18, S117–S125. [Google Scholar] [CrossRef]
- Hillemeier, M.M.; Downs, D.S.; Feinberg, M.E.; Weisman, C.S.; Chuang, C.H.; Parrott, R.; Velott, D.; Francis, L.A.; Baker, S.A.; Dyer, A.M.; et al. Improving women’s preconceptional health: Findings from a randomized trial of the Strong Healthy Women intervention in the Central Pennsylvania women’s health study. Women’s Health Issues 2008, 18, S87–S96. [Google Scholar] [CrossRef]
- Hu, G.; Tian, H.; Zhang, F.; Liu, H.; Zhang, C.; Zhang, S.; Wang, L.; Liu, G.; Yu, Z.; Yang, X.; et al. Tianjin Gestational Diabetes Mellitus Prevention Program: Study design, methods, and 1-year interim report on the feasibility of lifestyle intervention program. Diabetes Res. Clin. Pract. 2012, 98, 508–517. [Google Scholar] [CrossRef]
- van Dijk, M.R.; Koster, M.P.H.; Willemsen, S.P.; Huijgen, N.A.; Laven, J.S.E.; Steegers-Theunissen, R.P.M. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod. Biomed. Online 2017, 35, 453–460. [Google Scholar] [CrossRef]
- van Oers, A.M.; Mutsaerts, M.A.Q.; Burggraaff, J.M.; Kuchenbecker, W.K.H.; Perquin, D.A.M.; Koks, C.A.M.; van Golde, R.; Kaaijk, E.M.; Broekmans, F.J.; de Bruin, J.P.; et al. Association between periconceptional weight loss and maternal and neonatal outcomes in obese infertile women. PLoS ONE 2018, 13, e0192670. [Google Scholar] [CrossRef] [PubMed]
- Karlsen, K.; Humaidan, P.; Sorensen, L.H.; Alsbjerg, B.; Ravn, P. Motivational interviewing: A part of the weight loss program for overweight and obese women prior to fertility treatment. Gynecol. Endocrinol. 2013, 29, 839–842. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 13. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2018. Diabetes Care 2018, 41, S137–S143. [Google Scholar] [CrossRef]
- Farahi, N.; Zolotor, A. Recommendations for preconception counseling and care. Am. Fam. Physician 2013, 88, 499–506. [Google Scholar] [PubMed]
- American College of Obstetricians and Gynecologists. Prepregnncy counseling. ACOG Committee Opinion No. 762. Obstet. Gynecol. 2019, 133, e78–e89. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Rajagopalan, S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Soc. Hypertens. JASH 2018, 12, 238. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).