Predictors of Adherence to Lifestyle Recommendations in Stroke Secondary Prevention
Abstract
1. Introduction
- (a)
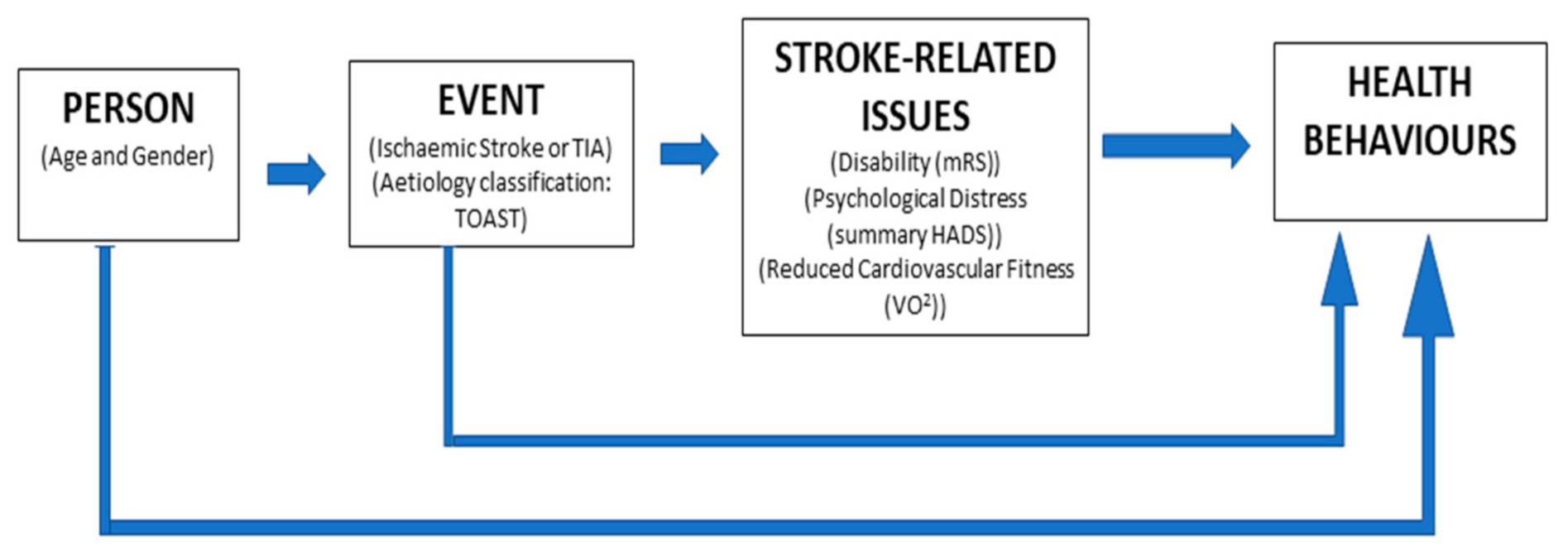
- Present an a priori conceptual model of potential factors influencing health behaviours after stroke or TIA (Figure 1). These include sociodemographic factors (age and gender), stroke-related factors (TOAST classification, stroke or TIA classification) and stroke sequalae (acquired disability, reduced cardiovascular fitness and psychological distress).
- (b)
- Establish unadjusted prevalence rates of adherence with healthy lifestyle behaviours of absolute smoking abstinence, a minimum of 30 min of moderate–vigorous physical activity (MVPA) at least 3 days per week, consumption of greater than or equal to 5 portions of fruit and vegetables per day and adherence with all three behaviours.
- (c)
- Identify determinants of each healthy lifestyle behaviour and adherence with all three from those proposed in the conceptual model (Figure 1).
2. Materials and Methods
2.1. Research Design
2.2. Participants
2.3. Health Behaviours
2.4. Participant Profile
2.5. Stroke-Related Issues
2.6. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strong, K.; Mathers, C.; Bonita, R. Preventing stroke: Saving lives around the world. Lancet Neurol. 2007, 6, 182–187. [Google Scholar] [CrossRef]
- World Stroke Organization. Global Stroke Fact Sheet. 18 November 2019. Available online: https://www.world-stroke.org/publications-and-resources/resources/global-stroke-fact-sheet (accessed on 11 March 2021).
- Hardie, K.; Hankey, G.J.; Jamrozik, K.; Broadhurst, R.J.; Anderson, C. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth Community Stroke Study. Stroke 2004, 35, 731–735. [Google Scholar] [CrossRef] [PubMed]
- Burn, J.; Dennis, M.; Bamford, J.; Sandercock, P.; Wade, D.; Warlow, C. Long term risk of recurrent stroke after a first ever stroke. Stroke 1994, 25, 333–337. [Google Scholar] [CrossRef]
- Sacco, R.L.; Shi, T.; Zamanillo, M.C.; Kargman, D.E. Predictors of mortality and recurrence after hospitalized cerebral infarction in an urban community: The Northern Manhattan Stroke Study. Neurology 1994, 44, 626. [Google Scholar] [CrossRef]
- Hankey, G.J.; Jamrozik, K.; Broadhurst, R.J.; Forbes, S.; Burvill, P.W.; Anderson, C.S.; Stewart-Wynne, E.G. Long-term risk of first recurrent stroke in the Perth Community Stroke Study. Stroke 1998, 29, 2491–2500. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.G.; Murphy, M.F.; Rothwell, P.M. Long term risks of stroke, myocardial infarction, and vascular death in “low risk” patients with a non-recent transient ischaemic attack. J. Neurol. Neurosurg. Psychiatry 2003, 74, 577–580. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sposato, L.A.; Lam, M.; Allen, B.; Richard, L.; Shariff, S.Z.; Saposnik, G. First-ever ischemic stroke and increased risk of incident heart disease in older adults. Neurology 2020, 94, e1559–e1570. [Google Scholar] [CrossRef] [PubMed]
- Touzeé, E.; Varenne, O.; Chatellier, G.; Peyrard, S.; Rothwell, P.M.; Mas, J.L. Risk of myocardial infarction and vascular death after transient ischemic attack and ischemic stroke: A systematic review and meta-analysis. Stroke 2005, 36, 2748–2755. [Google Scholar] [CrossRef] [PubMed]
- Boulanger, M.; Béjot, Y.; Rothwell, P.M.; Touzé, E. Long-term risk of myocardial infarction compared to recurrent stroke after transient ischemic attack and ischemic stroke: Systematic review and meta-analysis. J. Am. Heart Assoc. 2018, 7, e007267. [Google Scholar] [CrossRef]
- O’donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef]
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—A systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Blanco Mejia, S.; Rahelić, D.; Kahleová, H.; Salas-Salvadó, J.; Kendall, C.W.; Sievenpiper, J.L. DASH dietary pattern and cardiometabolic outcomes: An umbrella review of systematic reviews and meta-analyses. Nutrients 2019, 11, 338. [Google Scholar] [CrossRef] [PubMed]
- Pan, B.; Jin, X.; Jun, L.; Qiu, S.; Zheng, Q.; Pan, M. The relationship between smoking and stroke: A meta-analysis. Medicine 2019, 98, e14872. [Google Scholar] [CrossRef]
- Kyu, H.H.; Bachman, V.F.; Alexander, L.T.; Mumford, J.E.; Afshin, A.; Estep, K.; Veerman, J.L.; Delwiche, K.; Iannarone, M.L.; Moyer, M.L.; et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: Systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ 2016, 9, 354. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.D.; Folsom, A.R.; Blair, S.N. Physical activity and stroke risk: A meta-analysis. Stroke 2003, 34, 2475–2481. [Google Scholar] [CrossRef]
- Reinholdsson, M.; Palstam, A.; Sunnerhagen, K.S. Prestroke physical activity could influence acute stroke severity (part of PAPSIGOT). Neurology 2018, 91, e1461–e1467. [Google Scholar] [CrossRef]
- Chiuve, S.; Rexrode, K.; Spiegelman, D.; Logroscino, G.; Manson, J.; Rimm, E. Primary Prevention of Stroke by Healthy Lifestyle. Circulation 2008, 118, 947–954. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- English, C.; MacDonald-Wicks, L.; Patterson, A.; Attia, J.; Hankey, G.J. The role of diet in secondary stroke prevention. Lancet Neurol. 2020, 20, 150–160. [Google Scholar] [CrossRef]
- Chen, J.; Li, S.; Zheng, K.; Wang, H.; Xie, Y.; Xu, P.; Dai, Z.; Gu, M.; Xia, Y.; Zhao, M.; et al. Impact of smoking status on stroke recurrence. J. Am. Heart Assoc. 2019, 8, e011696. [Google Scholar] [CrossRef] [PubMed]
- Turan, T.N.; Nizam, A.; Lynn, M.J.; Egan, B.M.; Le, N.A.; Lopes-Virella, M.F.; Hermayer, K.L.; Harrell, J.; Derdeyn, C.P.; Fiorella, D.; et al. Relationship between risk factor control and vascular events in the SAMMPRIS trial. Neurology 2017, 88, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Kono, Y.; Yamada, S.; Kamisaka, K.; Araki, A.; Fujioka, Y.; Yasui, K.; Hasegawa, Y.; Koike, Y. Recurrence risk after noncardioembolic mild ischemic stroke in a Japanese population. Cerebrovasc. Dis. 2011, 31, 365–372. [Google Scholar] [CrossRef]
- Chin, Y.Y.; Sakinah, H.; Aryati, A.; Hassan, B.M. Prevalence, risk factors and secondary prevention of stroke recurrence in eight countries from south, east and southeast Asia: A scoping review. Med J. Malays. 2018, 73, 90–99. [Google Scholar]
- Redfern, J.; McKevitt, C.; Dundas, R.; Rudd, A.G.; Wolfe, C.D. Behavioral risk factor prevalence and lifestyle change after stroke: A prospective study. Stroke 2000, 31, 1877–1881. [Google Scholar] [CrossRef] [PubMed]
- Amarenco, P.; Lavallée, P.C.; Labreuche, J.; Albers, G.W.; Bornstein, N.M.; Canhão, P.; Caplan, L.R.; Donnan, G.A.; Ferro, J.M.; Hennerici, M.G.; et al. One-year risk of stroke after transient ischemic attack or minor stroke. N. Engl. J. Med. 2016, 374, 1533–1542. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Pan, Y.; Liu, L.; Wang, Y.; Zhao, X.; Wang, Y. One-year outcomes and secondary prevention in patients after acute minor stroke: Results from the China National Stroke Registry. Neurol. Res. 2017, 39, 484–491. [Google Scholar] [CrossRef] [PubMed]
- Bergström, L.; Irewall, A.L.; Söderström, L.; Ögren, J.; Laurell, K.; Mooe, T. One-year incidence, time trends, and predictors of recurrent ischemic stroke in Sweden from 1998 to 2010: An observational study. Stroke 2017, 48, 2046–2051. [Google Scholar] [CrossRef]
- Wali, H.; Kurdi, S.; Bilal, J.; Riaz, I.B.; Bhattacharjee, S. Health behaviors among stroke survivors in the United States: A propensity score-matched study. J. Stroke Cerebrovasc. Dis. 2018, 27, 2124–2133. [Google Scholar] [CrossRef]
- Ives, S.P.; Heuschmann, P.U.; Wolfe, C.D.; Redfern, J. Patterns of smoking cessation in the first 3 years after stroke: The South London Stroke Register. Eur. J. Prev. Cardiol. 2008, 15, 329–335. [Google Scholar] [CrossRef] [PubMed]
- van den Berg, M.J.; van der Graaf, Y.; Deckers, J.W.; de Kanter, W.; Algra, A.; Kappelle, L.J.; de Borst, G.J.; Cramer, M.J.; Visseren, F.L.; SMART Study Group. Smoking cessation and risk of recurrent cardiovascular events and mortality after a first manifestation of arterial disease. Am. Heart J. 2019, 213, 112–122. [Google Scholar] [CrossRef]
- Butler, E.N.; Evenson, K.R. Prevalence of physical activity and sedentary behavior among stroke survivors in the United States. Top. Stroke Rehabil. 2014, 21, 246–255. [Google Scholar] [CrossRef]
- Bailey, R.R.; Phad, A.; McGrath, R.; Ford, A.L.; Tabak, R.; Haire-Joshu, D. Lifestyle risk behaviors among stroke survivors with and without diabetes. Am. J. Phys. Med. Rehabil. 2019, 98, 794. [Google Scholar] [CrossRef]
- Lennon, O.C.; Doody, C.; Choisdealbh, C.N.; Blake, C. Barriers to healthy-lifestyle participation in stroke: Consumer participation in secondary prevention design. Int. J. Rehabil. Res. 2013, 36, 354–361. [Google Scholar] [CrossRef]
- Lennon, O.; Blake, C. Cardiac rehabilitation adapted to transient ischaemic attack and stroke (CRAFTS): A randomised controlled trial. BMC Neurol. 2009, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Reading, J.; Shephard, R.J. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can. J. Sport Sci. 1992, 17, 338–345. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Sampson, L.; Stampfer, M.J.; Rosner, B.; Bain, C.; Witschi, J.; Hennekens, C.H.; Speizer, F.E. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am. J. Epidemiol. 1985, 122, 51–65. [Google Scholar] [CrossRef] [PubMed]
- Biener, L.; Abrams, D. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991, 10, 360–365. [Google Scholar] [CrossRef]
- Dams, H.P., Jr.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E., 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar]
- Zigmond, A.S.; Smith, R.P. The hospital anxiety and depression scale. Acta Psychiatry Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Norton, S.; Cosco, T.; Doyle, F.; Done, J.; Sacker, A. The Hospital Anxiety and Depression Scale: A meta confirmatory factor analysis. J. Psychosom. Res. 2013, 74, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Banks, J.; Marotta, C. Outcomes Validity and Reliability of the Modified Rankin Scale: Implications for Stroke Clinical Trials: A Literature Review and Synthesis. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef]
- Holden, M.K.; Gill, K.M.; Magliozzi, M.R.; Nathan, J.; Piehl-Baker, L. Gait assessment for the neurologically impaired: Reliability and meaningfulness. Phys. Ther. 1984, 64, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Lennon, O.; Denis, R.; Grace, N.; Blake, C. Feasibility, criterion validity and retest reliability of exercise testing using the Astrand-rhyming test protocol with an adaptive ergometer in stroke patients. Disabil. Rehabil. 2012, 34, 1149–1156. [Google Scholar] [CrossRef]
- Ipsos, M.R. Healthy Ireland Survey 2019: Summary of Findings; Department of Health (DoH), Government Publications: Dublin, Ireland, 2019.
- Von Sarnowski, B.; Putaala, J.; Grittner, U.; Gaertner, B.; Schminke, U.; Curtze, S.; Huber, R.; Tanislav, C.; Lichy, C.; Demarin, V.; et al. Lifestyle risk factors for ischemic stroke and transient ischemic attack in young adults in the Stroke in Young Fabry Patients study. Stroke 2013, 44, 119–125. [Google Scholar] [CrossRef]
- Sabia, S.; Singh-Manoux, A.; Hagger-Johnson, G.; Cambois, E.; Brunner, E.J.; Kivimaki, M. Influence of individual and combined healthy behaviours on successful aging. CMAJ 2012, 184, 1985–1992. [Google Scholar] [CrossRef]
- Towfighi, A.; Markovic, D.; Ovbiagele, B. Impact of a healthy lifestyle on all-cause and cardiovascular mortality after stroke in the USA. J. Neurol. Neurosurg. Psychiatry 2012, 83, 146–151. [Google Scholar] [CrossRef]
- Flach, C.; Muruet, W.; Wolfe, C.D.; Bhalla, A.; Douiri, A. Risk and secondary prevention of stroke recurrence: A Population-Base Cohort Study. Stroke 2020, 51, 2435–2444. [Google Scholar] [CrossRef]
- Greenlund, K.J.; Giles, W.H.; Keenan, N.L.; Croft, J.B.; Mensah, G.A. Physician advice, patient actions, and health-related quality of life in secondary prevention of stroke through diet and exercise. Stroke 2002, 33, 565–570. [Google Scholar] [CrossRef]
- Ushio, M.; Kanaoka, M.; Kinoshita, Y.; Maeno, S.; Fujita, K. Moderate-to-vigorous physical activity and the risk of stroke recurrence in patients with a history of minor ischemic stroke in Japan: A retrospective analysis. Top. Stroke Rehabil. 2018, 25, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Thilarajah, S.; Mentiplay, B.F.; Bower, K.J.; Tan, D.; Pua, Y.H.; Williams, G.; Koh, G.; Clark, R.A. Factors associated with post-stroke physical activity: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2018, 99, 1876–1889. [Google Scholar] [CrossRef] [PubMed]
- Ivey, F.M.; Macko, R.F.; Ryan, A.S.; Hafer-Macko, C.E. Cardiovascular health and fitness after stroke. Top. Stroke Rehabil. 2005, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- MacKay-Lyons, M.J.; Makrides, L. Exercise capacity early after stroke. Arch. Phys. Med. Rehabil. 2002, 83, 1697–1702. [Google Scholar] [CrossRef]
- Macko, R.F.; Katzel, L.I.; Yataco, A.; Tretter, L.D.; DeSouza, C.A.; Dengel, D.R.; Smith, G.V.; Silver, K.H. Low-velocity graded treadmill stress testing in hemiparetic stroke patients. Stroke 1997, 28, 988–992. [Google Scholar] [CrossRef]
- Smith, A.C.; Saunders, D.H.; Mead, G. Cardiorespiratory fitness after stroke: A systematic review. Int. J. Stroke 2012, 7, 499–510. [Google Scholar] [CrossRef]
- Billinger, S.A.; Coughenour, E.; MacKay-Lyons, M.J.; Ivey, F.M. Reduced cardiorespiratory fitness after stroke: Biological consequences and exercise-induced adaptations. Stroke Res. Treat. 2012, 2012, 959120. [Google Scholar] [CrossRef]
- Lennon, O.; Gallagher, A.; Cooney, H.; O’Sullivan, M.; Ross, M.; Smith, J.; Murphy, S. A Comparison of Cardiac Rehabilitation for Non-Disabling Stroke and Cardiac Conditions: Outcomes and Healthcare Professionals’ Perceptions. EMJ Int. Cardiol. 2020, 8, 26–38. [Google Scholar]
- Fine, L.J.; Philogene, G.S.; Gramling, R.; Coups, E.J.; Sinha, S. Prevalence of multiple chronic disease risk factors: 2001 National Health Interview Survey. Am. J. Prev. Med. 2004, 27, 18–24. [Google Scholar] [CrossRef]
- Spring, B.; Moller, A.C.; Coons, M.J. Multiple health behaviours: Overview and implications. J. Public Health 2012, 34 (Suppl. 1), i3–i10. [Google Scholar] [CrossRef]
- Chasandra, M.; Goudas, M.; Theodorakis, Y. Exercise and smoking: A literature overview. Health 2015, 7, 1477–1491. [Google Scholar] [CrossRef]
- Ussher, M.H.; Taylor, A.H.; Faulkner, G.E. Exercise interventions for smoking cessation. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef] [PubMed]
- Ussher, M.H.; Faulkner, G.E.J.; Angus, K.; Hartmann-Boyce, J.; Taylor, A.H. Exercise interventions for smoking cessation. Cochrane Database Syst. Rev. 2019, CD002295. [Google Scholar] [CrossRef]
- Huang, Z.X.; Lin, X.L.; Lu, H.K.; Liang, X.Y.; Fan, L.J.; Liu, X.T. Lifestyles correlate with stroke recurrence in Chinese inpatients with first-ever acute ischemic stroke. J. Neurol. 2019, 266, 1194–1202. [Google Scholar] [CrossRef] [PubMed]
- Park, E.W.; Schult, J.K.; Tudiver, F.; Campbell, T.; Becker, L. Enhancing partner support to improve smoking cessation. Cochrane Database Syst. Rev. 2004, CD002928-3. [Google Scholar] [CrossRef]
- Ball, K.; Jeffery, R.W.; Abbott, G.; McNaughton, S.A.; Crawford, D. Is healthy behavior contagious: Associations of social norms with physical activity and healthy eating. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 86. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, M.; Kerr, S.; Watson, H.; Paton, G.; Ellis, G. An exploration of lifestyle beliefs and lifestyle behaviour following stroke: Findings from a focus group study of patients and family members. BMC Fam. Pract. 2010, 11, 97. [Google Scholar] [CrossRef] [PubMed]
- Mendelsohn, C. Smoking and depression: A review. Aust. Fam. Physician 2012, 41, 304. [Google Scholar]
- Hillen, T.; Coshall, C.; Tilling, K.; Rudd, A.G.; McGovern, R.; Wolfe, C.D. Cause of stroke recurrence is multifactorial: Patterns, risk factors, and outcomes of stroke recurrence in the South London Stroke Register. Stroke 2003, 34, 1457–1463. [Google Scholar] [CrossRef]
| N = 142 | ||
|---|---|---|
| Mean (SD) | ||
| Age | 63.1 (12.7) | |
| Time since stroke/TIA (months) | 37.3 (32) | |
| BMI | 28.3 (5.4) | |
| Blood pressure (SBP/DBP mmHg) | 136 (19)/82 (12) | |
| Initial VO2 peak (LO2/kg/min) | 1.3 (0.6) | |
| Median (range) | ||
| Modified Rankin Scale | 1 (0–4) | |
| Functional ambulatory category | 5 (0–5) | |
| N (%) | ||
| Male | 100 (70.5) | |
| Female | 42 (29.5) | |
| Left CVA | 54 (38) | |
| Right CVA | 42 (29.6) | |
| TIA | 46 (32.4) | |
| TOAST classification | 1 | 94 (66) |
| 2 | 23 (17) | |
| 3 | 18 (13) | |
| 4 | 01 (0.5) | |
| 5 | 06 (5) | |
| Smoking Cessation | ≥5 Portions Daily Fruit and Vegetables/Week | Minimum 30 min MVPA 3/Week | Compliance with All Three Health Behaviours | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Total compliance | 119 (84) | 76 (54) | 44 (31) | 26 (18) |
| Male (n = 100) | 87 (87) | 49 (49) | 30 (30) | 17 (17) |
| Female (n = 42) | 32 (76) | 27 (64) | 14 (33) | 9 (21) |
| p = 0.11 | p = 0.096 | p = 0.69 | p = 0.53 | |
| Stroke (n = 95) | 81 (85) | 51 (54) | 24 (25) | 14 (15) |
| TIA (n = 47) | 38 (81) | 25 (53) | 20 (43) | 12 (26) |
| p = 0.50 | p = 0.96 | p = 0.04 * | p = 0.12 | |
| TOAST 1 (n = 94) | 79 (84) | 49 (52) | 27 (29) | 17 (18) |
| TOAST 2 (n = 23) | 21 (91) | 15 (65) | 6 (20) | 4 (17) |
| TOAST 3 (n = 18) | 13 (72) | 9 (50) | 8 (44) | 2 (11) |
| TOAST 4 and 5 (n = 7) | 6 (86) | 3 (43) | 3 (43) | 3 (43) |
| p = 0.57 | p = 0.63 | p = 0.48 | p = 0.30 |
| Health Behaviour | Non-Smoking 1 | 5 Fruit and Vegetables/Day 2 | Minimum MVPA/Week 3 | Meeting 3 Health Behaviours 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Independent Variables | aOR | 95% CI | p | aOR | 95% CI | p | aOR | 95% CI | p | aOR | 95% CI | p |
| Gender (Male) | 1.06 | 0.26; 4.24 | 0.94 | 0.36 | 0.14; 0.96 | 0.04 | 0.44 | 0.15; 1.26 | 0.13 | 0.45 | 0.14; 1.53 | 0.2 |
| Age | 1.08 | 1.01; 1.16 | 0.03 | 1.01 | 0.97; 1.06 | 0.61 | 0.99 | 0.94; 1.04 | 0.74 | 1.02 | 0.96; 1.08 | 0.57 |
| Stroke or Tia (Stroke) | 1.85 | 0.29; 11.61 | 0.51 | 0.92 | 0.26; 3.23 | 0.90 | 2.15 | 0.53; 8.90 | 0.29 | 1.30 | 0.28; 5.93 | 0.74 |
| TOAST | 0.32 | 0.52 | 0.54 | 0.74 | ||||||||
| TOAST 1 | 0.12 | 0.01; 2.92 | 0.19 | 2.13 | 0.28; 16.31 | 0.47 | 0.96 | 0.11; 8.43 | 0.97 | 0.51 | 0.05; 4.92 | 0.56 |
| TOAST 2 | 0.14 | 0.00; 5.47 | 0.29 | 4.93 | 0.46; 53.28 | 0.20 | 1.35 | 0.11; 17.12 | 0.82 | 1.01 | 0.07; 15.22 | 0.99 |
| TOAST 3 | 0.05 | 0.00; 1.41 | 0.08 | 2.24 | 0.24; 21.03 | 0.48 | 2.77 | 0.26; 29.06 | 0.49 | 0.40 | 0.03; 5.24 | 0.49 |
| Disability (Mrs) | 1.09 | 0.59; 2.03 | 0.79 | 1.12 | 0.73; 1.72 | 0.62 | 1.20 | 0.70; 2.06 | 0.51 | 1.44 | 0.76; 2.71 | 0.26 |
| Psychological Distress (Hadstotal) | 0.9 | 0.82; 0.98 | 0.02 | 0.95 | 0.89; 1.01 | 0.10 | 0.94 | 0.87; 1.02 | 0.14 | 0.92 | 0.83; 1.01 | 0.09 |
| Cardiovascular Fitness (VO2peak) | 1.51 | 0.23; 9.70 | 0.67 | 2.76 | 0.74; 10.27 | 0.13 | 7.55 | 1.65; 34.64 | 0.01 | 12.08 | 2.08; 70.05 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lennon, O.; Hall, P.; Blake, C. Predictors of Adherence to Lifestyle Recommendations in Stroke Secondary Prevention. Int. J. Environ. Res. Public Health 2021, 18, 4666. https://doi.org/10.3390/ijerph18094666
Lennon O, Hall P, Blake C. Predictors of Adherence to Lifestyle Recommendations in Stroke Secondary Prevention. International Journal of Environmental Research and Public Health. 2021; 18(9):4666. https://doi.org/10.3390/ijerph18094666
Chicago/Turabian StyleLennon, Olive, Patricia Hall, and Catherine Blake. 2021. "Predictors of Adherence to Lifestyle Recommendations in Stroke Secondary Prevention" International Journal of Environmental Research and Public Health 18, no. 9: 4666. https://doi.org/10.3390/ijerph18094666
APA StyleLennon, O., Hall, P., & Blake, C. (2021). Predictors of Adherence to Lifestyle Recommendations in Stroke Secondary Prevention. International Journal of Environmental Research and Public Health, 18(9), 4666. https://doi.org/10.3390/ijerph18094666






