Risk of Pneumonia in Pediatric Patients Following Minor Chest Trauma: A Population-Based Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
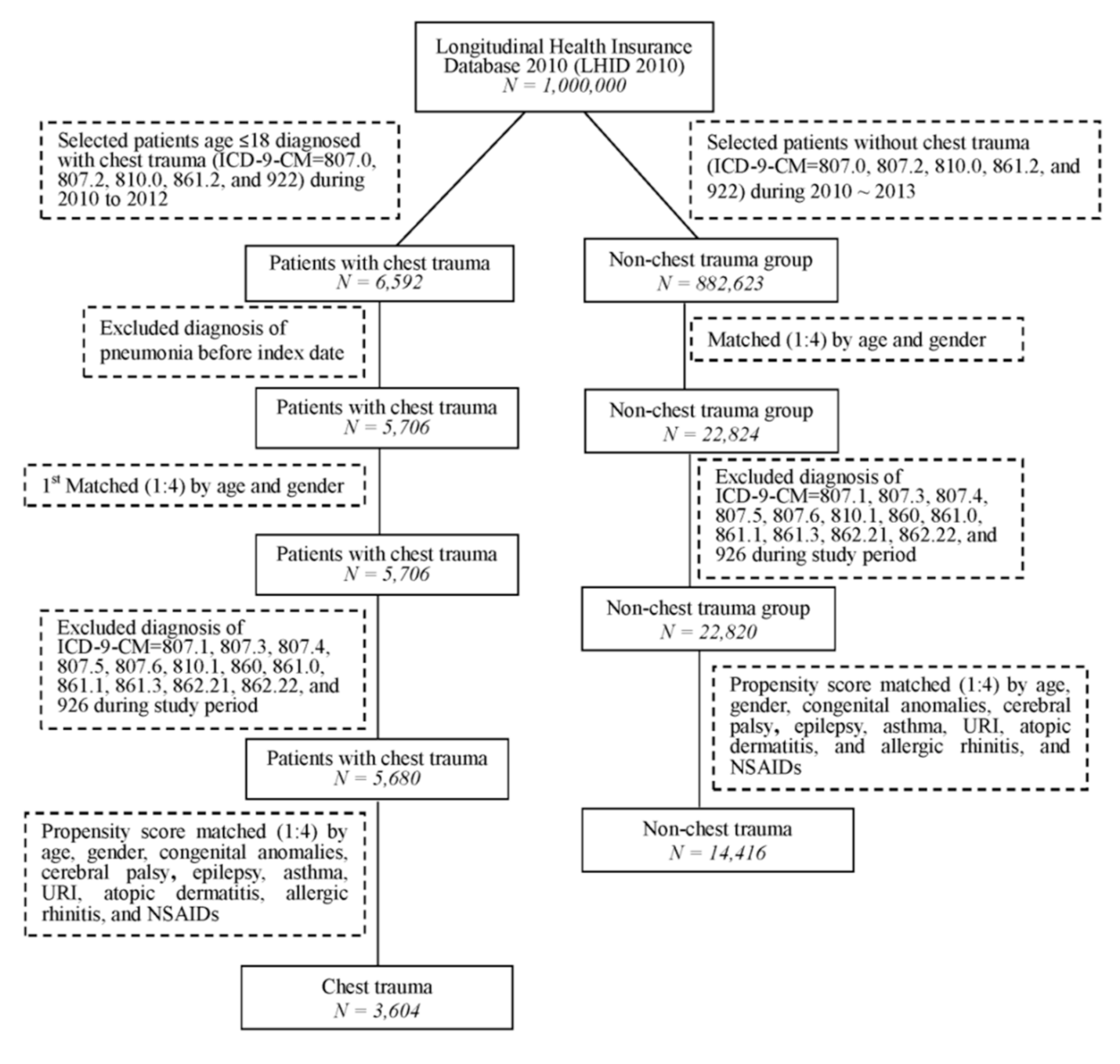
2.2. Study Group
2.3. Statistical Analysis
3. Results
3.1. Characteristics of Study Patients
3.2. Risk of Pneumonia After Exposure to Chest Trauma
3.3. Risk of Pneumonia among Patients with and without Chest Trauma and Subgroup-Specific Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khandhar, S.J.; Johnson, S.B.; Calhoon, J.H. Overview of thoracic trauma in the United States. Thorac. Surg. Clin. 2007, 17, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chauny, J.M.; Émond, M.; Plourde, M.; Guimont, C.; Le Sage, N.; Vanier, L.; Bergeron, E.; Dufresne, M.; Allain-Boulé, N.; Fratu, R. Patients with rib fractures do not develop delayed pneumonia: A prospective, multicenter cohort study of minor thoracic injury. Ann. Emerg. Med. 2012, 60, 726–731. [Google Scholar] [CrossRef] [PubMed]
- Lien, Y.C.; Chen, C.H.; Lin, H.C. Risk factors for 24-hour mortality after traumatic rib fractures owing to motor vehicle accidents: A nationwide population-based study. Ann. Thorac. Surg. 2009, 88, 1124–1130. [Google Scholar] [CrossRef] [PubMed]
- Demirhan, R.; Onan, B.; Oz, K.; Halezeroglu, S. Comprehensive analysis of 4205 patients with chest trauma: A 10-year experience. Interact. Cardiovasc. Thorac. Surg. 2009, 9, 450–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eghbalzadeh, K.; Sabashnikov, A.; Zeriouh, M.; Choi, Y.H.; Bunck, A.C.; Mader, N.; Wahlers, T. Blunt chest trauma: A clinical chameleon. Heart Br. Card. Soc. 2018, 104, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, D.W.; Agarwal, N.N. The morbidity and mortality of rib fractures. J. Trauma 1994, 37, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Tovar, J.A.; Vazquez, J.J. Management of chest trauma in children. Paediatr. Respir. Rev. 2013, 14, 86–91. [Google Scholar] [CrossRef]
- Black, T.L.; Snyder, C.L.; Miller, J.P.; Mann, C.M., Jr.; Copetas, A.C.; Ellis, D.G. Significance of chest trauma in children. South. Med. J. 1996, 89, 494–496. [Google Scholar] [CrossRef]
- Su, S.C.; Hua, K.F.; Lee, H.; Chao, L.K.; Tan, S.K.; Lee, H.; Yang, S.F.; Hsu, H.Y. LTA and LPS mediated activation of protein kinases in the regulation of inflammatory cytokines expression in macrophages. Clin. Chim. Acta Int. J. Clin. Chem. 2006, 374, 106–115. [Google Scholar] [CrossRef]
- Pearson, E.G.; Fitzgerald, C.A.; Santore, M.T. Pediatric thoracic trauma: Current trends. Semin. Pediatric Surg. 2017, 26, 36–42. [Google Scholar] [CrossRef]
- Simon, J.B.; Wickham, A.J. Blunt chest wall trauma: An overview. Br. J. Hosp. Med. 2019, 80, 711–715. [Google Scholar] [CrossRef]
- Cheng, C.W.; Chien, M.H.; Su, S.C.; Yang, S.F. New markers in pneumonia. Clin. Chim. Acta Int. J. Clin. Chem. 2013, 419, 19–25. [Google Scholar] [CrossRef]
- Chiang, T.Y.; Tsao, S.M.; Yeh, C.B.; Yang, S.F. Matrix metalloproteinases in pneumonia. Clin. Chim. Acta Int. J. Clin. Chem. 2014, 433, 272–277. [Google Scholar] [CrossRef]
- Shelat, V.G.; Eileen, S.; John, L.; Teo, L.T.; Vijayan, A.; Chiu, M.T. Chronic pain and its impact on quality of life following a traumatic rib fracture. Eur. J. Trauma Emerg. Surg. Off. Publ. Eur. Trauma Soc. 2012, 38, 451–455. [Google Scholar] [CrossRef]
- Daoust, R.; Emond, M.; Bergeron, E.; LeSage, N.; Camden, S.; Guimont, C.; Vanier, L.; Chauny, J.M. Risk factors of significant pain syndrome 90 days after minor thoracic injury: Trajectory analysis. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2013, 20, 1139–1145. [Google Scholar] [CrossRef]
- Marco, C.A.; Sorensen, D.; Hardman, C.; Bowers, B.; Holmes, J.; McCarthy, M.C. Risk factors for pneumonia following rib fractures. Am. J. Emerg. Med. 2020, 38, 610–612. [Google Scholar] [CrossRef]
- Bergeron, E.; Lavoie, A.; Clas, D.; Moore, L.; Ratte, S.; Tetreault, S.; Lemaire, J.; Martin, M. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J. Trauma 2003, 54, 478–485. [Google Scholar] [CrossRef]
- Kyu, H.H.; Pinho, C.; Wagner, J.A.; Brown, J.C.; Bertozzi-Villa, A.; Charlson, F.J.; Coffeng, L.E.; Dandona, L.; Erskine, H.E.; Ferrari, A.J.; et al. Global and National Burden of Diseases and Injuries Among Children and Adolescents Between 1990 and 2013: Findings From the Global Burden of Disease 2013 Study. JAMA Pediatrics 2016, 170, 267–287. [Google Scholar] [CrossRef] [Green Version]
- Ho, S.W.; Teng, Y.H.; Yang, S.F.; Yeh, H.W.; Wang, Y.H.; Chou, M.C.; Yeh, C.B. Risk of pneumonia in patients with isolated minor rib fractures: A nationwide cohort study. BMJ Open 2017, 7, e013029. [Google Scholar] [CrossRef] [Green Version]
- Miske, L.J.; Hickey, E.M.; Kolb, S.M.; Weiner, D.J.; Panitch, H.B. Use of the mechanical in-exsufflator in pediatric patients with neuromuscular disease and impaired cough. Chest 2004, 125, 1406–1412. [Google Scholar] [CrossRef] [Green Version]
- Eckhardt, T.; Horst, K.; Störmann, P.; Bläsius, F.; Hofman, M.; Herren, C.; Kobbe, P.; Hildebrand, F.; Andruszkow, H. Impact of Chest Trauma and Overweight on Mortality and Outcome in Severely Injured Patients. J. Clin. Med. 2020, 9, 2752. [Google Scholar] [CrossRef]
- Button, B.; Goodell, H.P.; Atieh, E.; Chen, Y.C.; Williams, R.; Shenoy, S.; Lackey, E.; Shenkute, N.T.; Cai, L.H.; Dennis, R.G.; et al. Roles of mucus adhesion and cohesion in cough clearance. Proc. Natl. Acad. Sci. USA 2018, 115, 12501–12506. [Google Scholar] [CrossRef] [Green Version]
- Battle, C.; Hutchings, H.; Evans, P.A. Blunt chest wall trauma: A review. Trauma 2013, 15, 156–175. [Google Scholar] [CrossRef]
- Dongel, I.; Coskun, A.; Ozbay, S.; Bayram, M.; Atli, B. Management of thoracic trauma in emergency service: Analysis of 1139 cases. Pak. J. Med. Sci. 2013, 29, 58–63. [Google Scholar] [CrossRef]
- Galvagno, S.M., Jr.; Smith, C.E.; Varon, A.J.; Hasenboehler, E.A.; Sultan, S.; Shaefer, G.; To, K.B.; Fox, A.D.; Alley, D.E.; Ditillo, M.; et al. Pain management for blunt thoracic trauma: A joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J. Trauma Acute Care Surg. 2016, 81, 936–951. [Google Scholar] [CrossRef]
- Cicala, R.S.; Voeller, G.R.; Fox, T.; Fabian, T.C.; Kudsk, K.; Mangiante, E.C. Epidural analgesia in thoracic trauma: Effects of lumbar morphine and thoracic bupivacaine on pulmonary function. Crit. Care Med. 1990, 18, 229–231. [Google Scholar] [CrossRef]
- Karmakar, M.K.; Ho, A.M. Acute pain management of patients with multiple fractured ribs. J. Trauma 2003, 54, 615–625. [Google Scholar] [CrossRef]
- Bulger, E.M.; Arneson, M.A.; Mock, C.N.; Jurkovich, G.J. Rib fractures in the elderly. J. Trauma 2000, 48, 1040–1046, discussion 1046–1047. [Google Scholar] [CrossRef]
- Alexander, J.; Manno, M. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Ann. Emerg. Med. 2003, 41, 617–622. [Google Scholar] [CrossRef]
- Friedland, L.R.; Kulick, R.M. Emergency department analgesic use in pediatric trauma victims with fractures. Ann. Emerg. Med. 1994, 23, 203–207. [Google Scholar] [CrossRef]
- Friedland, L.R.; Pancioli, A.M.; Duncan, K.M. Pediatric emergency department analgesic practice. Pediatric Emerg. Care 1997, 13, 103–106. [Google Scholar] [CrossRef] [PubMed]
- Teepe, J.; Grigoryan, L.; Verheij, T.J. Determinants of community-acquired pneumonia in children and young adults in primary care. Eur. Respir. J. 2010, 35, 1113–1117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heiskanen-Kosma, T.; Korppi, M.; Jokinen, C.; Heinonen, K. Risk factors for community-acquired pneumonia in children: A population-based case-control study. Scand. J. Infect. Dis. 1997, 29, 281–285. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Young, J.B.; Schermer, C.R.; Utter, G.H. Use of ketorolac is associated with decreased pneumonia following rib fractures. Am. J. Surg. 2014, 207, 566–572. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antonelli, M.; Moro, M.L.; Capelli, O.; De Blasi, R.A.; D’Errico, R.R.; Conti, G.; Bufi, M.; Gasparetto, A. Risk factors for early onset pneumonia in trauma patients. Chest 1994, 105, 224–228. [Google Scholar] [CrossRef]

| Variables | Chest Trauma N = 3604 | Non-Chest Trauma N = 14,416 | p-Value † | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age on index date | 0.123 | ||||
| 0–5 | 412 | 11.4 | 1563 | 10.8 | |
| 6–11 | 1203 | 33.4 | 4626 | 32.1 | |
| 12–18 | 1989 | 55.2 | 8227 | 57.1 | |
| Mean ± SD | 12.03 ± 4.37 | 12.15 ± 4.34 | 0.141 | ||
| Gender | 0.798 | ||||
| Female | 1543 | 42.8 | 6138 | 42.6 | |
| Male | 2061 | 57.2 | 8278 | 57.4 | |
| Congenital anomalies | 44 | 1.2 | 223 | 1.5 | 0.147 |
| Cerebral palsy | 3 | 0.1 | 10 | 0.1 | 0.781 ¶ |
| Epilepsy | 15 | 0.4 | 38 | 0.3 | 0.130 |
| Asthma | 116 | 3.2 | 475 | 3.3 | 0.818 |
| Upper respiratory tract infection | 2929 | 81.3 | 11,619 | 80.6 | 0.360 |
| Atopic dermatitis | 100 | 2.8 | 468 | 3.2 | 0.147 |
| Allergic rhinitis | 937 | 26.0 | 3720 | 25.8 | 0.812 |
| NSAIDs | 2186 | 60.7 | 8563 | 59.4 | 0.169 |
| Track duration (years): mean ± SD | 0.98 ± 0.12 | 0.98 ± 0.11 | 0.012 | ||
| Variables | No. of Subjects | No. of Pneumonia Event | Crude HR | 95% C.I. | p-Value | Adjusted HR † | 95% C.I. | p-Value |
|---|---|---|---|---|---|---|---|---|
| Group | ||||||||
| Non-chest trauma | 14,416 | 437 | 1 | 1 | ||||
| Chest trauma | 3604 | 137 | 1.26 | 1.04–1.53 | 0.018 | 1.23 | 1.02–1.49 | 0.034 |
| Age on index date | ||||||||
| 0–5 | 1975 | 248 | 1 | 1 | ||||
| 6–11 | 5829 | 193 | 0.25 | 0.21–0.30 | <0.001 | 0.26 | 0.21–0.31 | <0.001 |
| 12–18 | 10,216 | 133 | 0.10 | 0.08–0.12 | <0.001 | 0.11 | 0.08–0.13 | <0.001 |
| Gender | ||||||||
| Female | 7681 | 254 | 1 | 1 | ||||
| Male | 10,339 | 320 | 0.94 | 0.79–1.10 | 0.436 | 1.04 | 0.88–1.23 | 0.622 |
| Congenital anomalies | 267 | 16 | 1.95 | 1.18–3.20 | 0.009 | 1.76 | 1.07–2.91 | 0.026 |
| Epilepsy | 53 | 6 | 3.73 | 1.67–8.33 | 0.001 | 4.95 | 2.21–11.10 | <0.001 |
| Asthma | 591 | 39 | 2.20 | 1.59–3.04 | <0.001 | 1.26 | 0.90–1.75 | 0.172 |
| Upper respiratory tract infection | 14,548 | 534 | 3.23 | 2.34–4.45 | <0.001 | 1.77 | 1.27–2.47 | <0.001 |
| Atopic dermatitis | 568 | 41 | 2.41 | 1.75–3.31 | <0.001 | 0.95 | 0.68–1.31 | 0.741 |
| Allergic rhinitis | 4657 | 159 | 1.10 | 0.92–1.32 | 0.299 | 1.31 | 1.08–1.59 | 0.005 |
| NSAIDs | 10,749 | 406 | 1.64 | 1.37–1.96 | <0.001 | 1.09 | 0.90–1.32 | 0.363 |
| Variables | Chest Trauma | Non-Chest Trauma | HR | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|
| N | No. of Pneumonia Event | N | No. of Pneumonia Event | ||||
| Age | |||||||
| 0–5 | 412 | 60 | 1563 | 188 | 1.24 | 0.93–1.66 | 0.149 |
| 6–11 | 1203 | 42 | 4626 | 151 | 1.07 | 0.76–1.51 | 0.690 |
| 12–18 | 1989 | 35 | 8227 | 98 | 1.48 | 1.01–2.18 | 0.046 |
| p for interaction = 0.468 | |||||||
| Gender | |||||||
| Female | 1543 | 65 | 6138 | 189 | 1.38 | 1.04–1.83 | 0.026 |
| Male | 2061 | 72 | 8278 | 248 | 1.17 | 0.90–1.52 | 0.238 |
| p for interaction = 0.409 | |||||||
| Congenital anomalies | |||||||
| No | 3560 | 135 | 14,193 | 423 | 1.28 | 1.05–1.55 | 0.013 |
| Yes | 44 | 2 | 223 | 14 | 0.71 | 0.16–3.14 | 0.654 |
| p for interaction= 0.448 | |||||||
| Epilepsy | |||||||
| No | 3589 | 136 | 14,378 | 432 | 1.27 | 1.05–1.54 | 0.016 |
| Yes | 15 | 1 | 38 | 5 | 0.48 | 0.06–4.11 | 0.503 |
| p for interaction = 0.375 | |||||||
| Asthma | |||||||
| No | 3488 | 132 | 13,941 | 403 | 1.32 | 1.08–1.60 | 0.006 |
| Yes | 116 | 5 | 475 | 34 | 0.59 | 0.23–1.52 | 0.276 |
| p for interaction = 0.103 | |||||||
| Upper respiratory tract infection | |||||||
| No | 675 | 9 | 2797 | 31 | 1.20 | 0.57–2.52 | 0.632 |
| Yes | 2929 | 128 | 11,619 | 406 | 1.26 | 1.03–1.54 | 0.023 |
| p for interaction = 0.900 | |||||||
| Atopic dermatitis | |||||||
| No | 3504 | 126 | 13,948 | 407 | 1.24 | 1.01–1.51 | 0.036 |
| Yes | 100 | 11 | 468 | 30 | 1.77 | 0.88–3.52 | 0.107 |
| p for interaction = 0.336 | |||||||
| Allergic rhinitis | |||||||
| No | 2667 | 93 | 10,696 | 322 | 1.16 | 0.92–1.47 | 0.197 |
| Yes | 937 | 44 | 3720 | 115 | 1.53 | 1.08–2.17 | 0.016 |
| p for interaction = 0.198 | |||||||
| NSAIDs | |||||||
| No | 1418 | 46 | 5853 | 122 | 1.57 | 1.12–2.20 | 0.009 |
| Yes | 2186 | 91 | 8563 | 315 | 1.14 | 0.90–1.43 | 0.285 |
| p for interaction = 0.123 | |||||||
| Variables | No. of Subjects | No. of Pneumonia Event | Crude HR | 95% C.I. | p-Value | Adjusted HR † | 95% C.I. | p-Value |
|---|---|---|---|---|---|---|---|---|
| Follow-up duration ≤1 months | ||||||||
| Group | ||||||||
| Non-chest trauma | 14,416 | 50 | 1 | 1 | ||||
| Chest trauma | 3604 | 12 | 0.96 | 0.51–1.80 | 0.900 | 0.92 | 0.49–1.73 | 0.801 |
| Follow-up duration ≤3 months | ||||||||
| Group | ||||||||
| Non-chest trauma | 14,416 | 118 | 1 | 1 | ||||
| Chest trauma | 3604 | 43 | 1.46 | 1.03–2.07 | 0.034 | 1.42 | 1.00–2.01 | 0.049 |
| Follow-up duration ≤6 months | ||||||||
| Group | ||||||||
| Non-chest trauma | 14,416 | 238 | 1 | 1 | ||||
| Chest trauma | 3604 | 80 | 1.35 | 1.05–1.74 | 0.020 | 1.33 | 1.03–1.71 | 0.028 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chou, Y.-H.; Tai, L.-H.; Chan, C.-H.; Liu, H.-Y.; Yeh, H.-W.; Wang, Y.-H.; Lin, C.-W.; Yang, S.-F.; Chen, Y.-C.; Yeh, C.-B. Risk of Pneumonia in Pediatric Patients Following Minor Chest Trauma: A Population-Based Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 4690. https://doi.org/10.3390/ijerph18094690
Chou Y-H, Tai L-H, Chan C-H, Liu H-Y, Yeh H-W, Wang Y-H, Lin C-W, Yang S-F, Chen Y-C, Yeh C-B. Risk of Pneumonia in Pediatric Patients Following Minor Chest Trauma: A Population-Based Retrospective Cohort Study. International Journal of Environmental Research and Public Health. 2021; 18(9):4690. https://doi.org/10.3390/ijerph18094690
Chicago/Turabian StyleChou, Ying-Hsiang, Li-Hsiu Tai, Chi-Ho Chan, Haw-Yu Liu, Han-Wei Yeh, Yu-Hsun Wang, Chiao-Wen Lin, Shun-Fa Yang, Ying-Cheng Chen, and Chao-Bin Yeh. 2021. "Risk of Pneumonia in Pediatric Patients Following Minor Chest Trauma: A Population-Based Retrospective Cohort Study" International Journal of Environmental Research and Public Health 18, no. 9: 4690. https://doi.org/10.3390/ijerph18094690







