The Association of Physical (in)Activity with Mental Health. Differences between Elder and Younger Populations: A Systematic Literature Review
Abstract
:1. Introduction
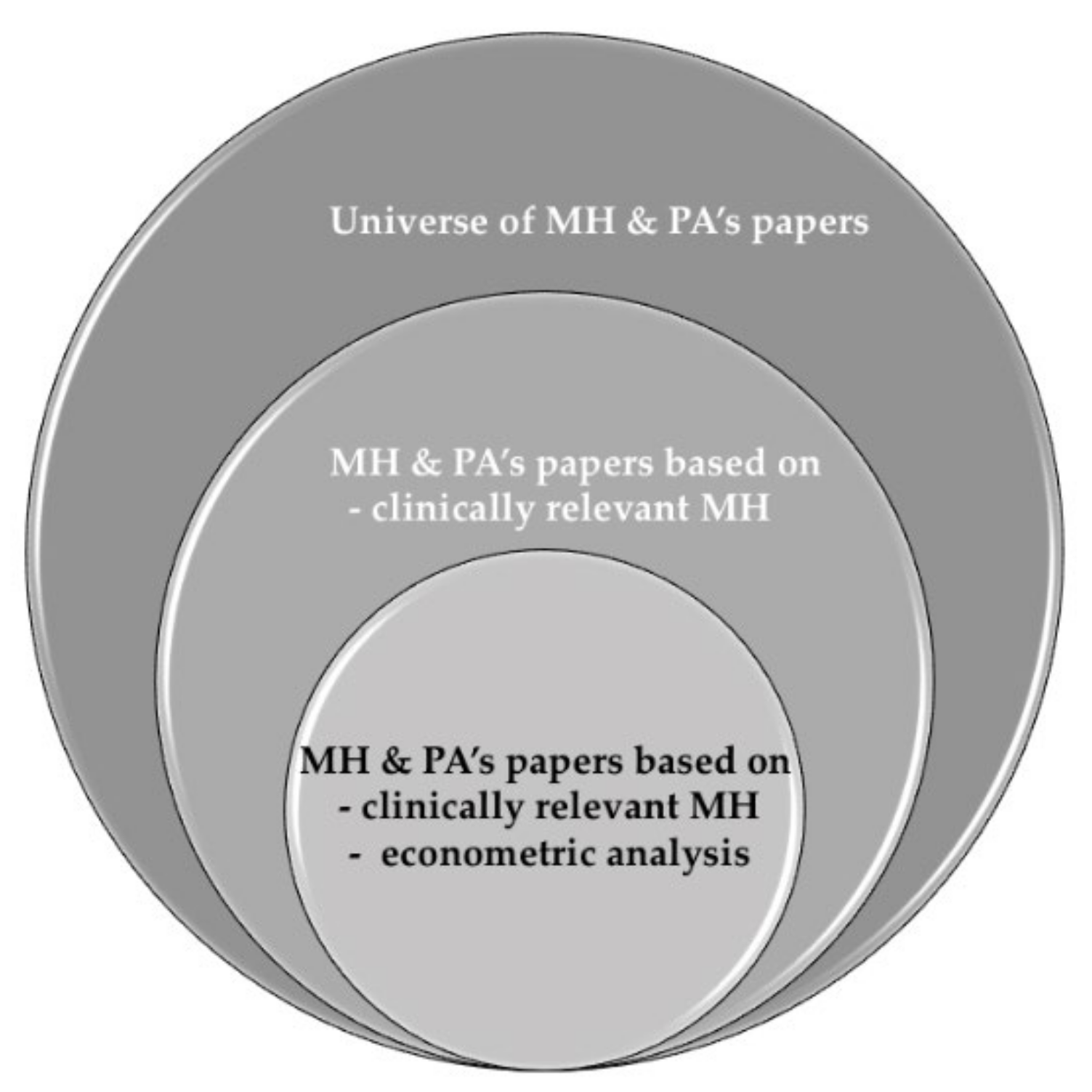
2. Material and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection and Data Extraction
2.4. Risk of Bias Assessment
2.5. Synthesis of Results
3. Results
3.1. Study Selection
3.2. Quality Assessment and the Risk of Bias
3.3. Main Results
3.3.1. Differences in the Association of PA with MH between Elder and Younger Populations
3.3.2. Differences in the Association of PA with MH between Self-Reported and Objective Types of MH
3.3.3. Differences in the Association of PA with MH for Self-Reported and Objective Types of PA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Steel, J.L.; Cheng, H.; Pathak, R.; Wang, Y.; Miceli, J.; Hecht, C.L.; Haggerty, D.; Peddada, S.; Geller, D.A.; Marsh, W.; et al. Psychosocial and Behavioral Pathways of Metabolic Syndrome in Cancer Caregivers. Psychooncology 2019, 28, 1735–1742. [Google Scholar] [CrossRef]
- Barbato, A.; Vallarino, M.; Rapisarda, F.; Lora, A.; Caldas de Almeida, J. Access to Mental Health Care in Europe—Scientific Paper; EU Compass for Action on Mental Health and Well-Being; Funded by the European Union in the frame of the 3rd EU Health Programme (2014–2020); Trimbos Institute: Utrecht, The Netherlands; NOVA University of Lisbon: Lisbon, Portugal; Finish Association for Mental Health: Helsinki, Finland, 2016. [Google Scholar]
- World Health Organization Regional Office for Europe. Mental Health; Fact Sheets on Sustainable Development Goals: Health Targets; WHO Regional Office for Europe: Copenhagen, Denmark, 2018. [Google Scholar]
- World Health Organization. WHO | Mental Health. Available online: http://www.who.int/research-observatory/analyses/mentalhealth/en/ (accessed on 19 February 2021).
- Organisation for Economic Co-operation and Development; World Health Organization; World Bank Group. Delivering Quality Health Services: A Global Imperative for Universal Health Coverage; OECD Publishing: Paris, France, 2018; ISBN 978-92-64-30030-9. [Google Scholar]
- Velten, J.; Bieda, A.; Scholten, S.; Wannemüller, A.; Margraf, J. Lifestyle Choices and Mental Health: A Longitudinal Survey with German and Chinese Students. BMC Public Health 2018, 18, 632. [Google Scholar] [CrossRef]
- Jacob, K.S. Social Context and Mental Health, Distress and Illness: Critical yet Disregarded by Psychiatric Diagnosis and Classification. Indian J. Psychiatry 2016, 32, 243–248. [Google Scholar] [CrossRef]
- Kim, Y.-M.; Cho, S. Socioeconomic Status, Work-Life Conflict, and Mental Health. Am. J. Ind. Med. 2020, 63, 703–712. [Google Scholar] [CrossRef]
- Appelqvist-Schmidlechner, K.; Tamminen, N.; Solin, P. Association between Positive Mental Health and Family Background among Young People in Finland. Eur. J. Public Health 2019, 29. [Google Scholar] [CrossRef]
- Jalayondeja, C.; Jalayondeja, W.; Suttiwong, J.; Sullivan, P.E.; Nilanthi, D.L. Physical Activity, Self-Esteem, and Quality of Life among People with Physical Disability. Southeast Asian J. Trop. Med. Public Health 2016, 47, 546–558. [Google Scholar] [PubMed]
- NCDs | Physical Inactivity: A Global Public Health Problem. Available online: http://www.who.int/ncds/prevention/physical-activity/inactivity-global-health-problem/en/ (accessed on 3 March 2021).
- Pavlova, I.; Vovkanych, L.; Vynogradskyi, B. Physical Activity of Elderly People. Physiotherapy 2014, 22, 78745660. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez-Ayllon, M.; Cadenas-Sánchez, C.; Estévez-López, F.; Muñoz, N.E.; Mora-Gonzalez, J.; Migueles, J.H.; Molina-García, P.; Henriksson, H.; Mena-Molina, A.; Martínez-Vizcaíno, V.; et al. Role of Physical Activity and Sedentary Behavior in the Mental Health of Preschoolers, Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. Auckl. N. Z. 2019, 49, 1383–1410. [Google Scholar] [CrossRef] [PubMed]
- Jack, K.; McLean, S.M.; Moffett, J.K.; Gardiner, E. Barriers to Treatment Adherence in Physiotherapy Outpatient Clinics: A Systematic Review. Man. Ther. 2010, 15, 220–228. [Google Scholar] [CrossRef]
- Garcia, D.; Archer, T. Positive Affect and Age as Predictors of Exercise Compliance. PeerJ 2014, 2, e694. [Google Scholar] [CrossRef] [Green Version]
- Lukács, A.; Mayer, K.; Juhász, E.; Varga, B.; Fodor, B.; Barkai, L. Reduced Physical Fitness in Children and Adolescents with Type 1 Diabetes: Reduced Physical Fitness in Youths with Type 1 Diabetes. Pediatr. Diabetes 2012, 13, 432–437. [Google Scholar] [CrossRef] [Green Version]
- Maggio, A.B.R.; Hofer, M.F.; Martin, X.E.; Marchand, L.M.; Beghetti, M.; Farpour-Lambert, N.J. Reduced Physical Activity Level and Cardiorespiratory Fitness in Children with Chronic Diseases. Eur. J. Pediatr. 2010, 169, 1187–1193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamer, M.; Biddle, S.J.H.; Stamatakis, E. Weekend Warrior Physical Activity Pattern and Common Mental Disorder: A Population Wide Study of 108,011 British Adults. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 96. [Google Scholar] [CrossRef] [Green Version]
- Spitzer, S.; Weber, D. Reporting Biases in Self-Assessed Physical and Cognitive Health Status of Older Europeans. PLoS ONE 2019, 14, e0223526. [Google Scholar] [CrossRef]
- Sagatun, Å.; Heyerdahl, S.; Wentzel-Larsen, T.; Lien, L. Medical Benefits in Young Adulthood: A Population-Based Longitudinal Study of Health Behaviour and Mental Health in Adolescence and Later Receipt of Medical Benefits. BMJ Open 2015, 5, e007139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baker, J.G.; Leddy, J.J.; Hinds, A.L.; Haider, M.N.; Shucard, J.; Sharma, T.; Hernandez, S.; Durinka, J.; Zivadinov, R.; Willer, B.S. An Exploratory Study of Mild Cognitive Impairment of Retired Professional Contact Sport Athletes. J. Head Trauma Rehabil. 2018, 33, E16–E23. [Google Scholar] [CrossRef] [PubMed]
- Asefa, A.; Nigussie, T.; Henok, A.; Mamo, Y. Prevalence of Sexual Dysfunction and Related Factors among Diabetes Mellitus Patients in Southwest Ethiopia. BMC Endocr. Disord. 2019, 19, 141. [Google Scholar] [CrossRef] [Green Version]
- Hallberg, I.; Bachrach-Lindström, M.; Hammerby, S.; Toss, G.; Ek, A.-C. Health-Related Quality of Life after Vertebral or Hip Fracture: A Seven-Year Follow-up Study. BMC Musculoskelet. Disord. 2009, 10, 135. [Google Scholar] [CrossRef] [Green Version]
- Ball, K.; Burton, N.W.; Brown, W.J. A Prospective Study of Overweight, Physical Activity, and Depressive Symptoms in Young Women. Obesity 2009, 17, 66–71. [Google Scholar] [CrossRef]
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for Depression in Well Older Adults: Evaluation of a Short Form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Sackett, D.L.; Strauss, S.E.; Richardson, W.S.; Rosenberg, W.; Haynes, R.B. Evidence-Based Medicine: How to Practice and Teach EBM, 2nd ed.; Elsevier: Philadelphia, PA, USA, 2000; Volume 16. [Google Scholar]
- Da Costa, D.; Zelkowitz, P.; Dasgupta, K.; Sewitch, M.; Lowensteyn, I.; Cruz, R.; Hennegan, K.; Khalifé, S. Dads Get Sad Too: Depressive Symptoms and Associated Factors in Expectant First-Time Fathers. Am. J. Mens Health 2017, 11, 1376–1384. [Google Scholar] [CrossRef] [Green Version]
- Parmar, D.; Stavropoulou, C.; Ioannidis, J.P.A. Health Outcomes during the 2008 Financial Crisis in Europe: Systematic Literature Review. BMJ 2016, 354, i4588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coll, C.d.V.N.; Domingues, M.R.; Stein, A.; da Silva, B.G.C.; Bassani, D.G.; Hartwig, F.P.; da Silva, I.C.M.; da Silveira, M.F.; da Silva, S.G.; Bertoldi, A.D. Efficacy of Regular Exercise During Pregnancy on the Prevention of Postpartum Depression: The PAMELA Randomized Clinical Trial. JAMA Netw. Open 2019, 2, e186861. [Google Scholar] [CrossRef]
- Underwood, M.; Lamb, S.E.; Eldridge, S.; Sheehan, B.; Slowther, A.-M.; Spencer, A.; Thorogood, M.; Atherton, N.; Bremner, S.A.; Devine, A.; et al. Exercise for Depression in Elderly Residents of Care Homes: A Cluster-Randomised Controlled Trial. Lancet Lond. Engl. 2013, 382, 41–49. [Google Scholar] [CrossRef] [Green Version]
- Shigdel, R.; Stubbs, B.; Sui, X.; Ernstsen, L. Cross-Sectional and Longitudinal Association of Non-Exercise Estimated Cardiorespiratory Fitness with Depression and Anxiety in the General Population: The HUNT Study. J. Affect. Disord. 2019, 252, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Annerstedt, M.; Ostergren, P.-O.; Björk, J.; Grahn, P.; Skärbäck, E.; Währborg, P. Green Qualities in the Neighbourhood and Mental Health—Results from a Longitudinal Cohort Study in Southern Sweden. BMC Public Health 2012, 12, 337. [Google Scholar] [CrossRef] [Green Version]
- Benedetti, T.R.B.; Borges, L.J.; Petroski, E.L.; Gonçalves, L.H.T. Physical Activity and Mental Health Status among Elderly People. Rev. Saúde Pública 2008, 42, 302–307. [Google Scholar] [CrossRef] [Green Version]
- Bishwajit, G.; O’Leary, D.P.; Ghosh, S.; Yaya, S.; Shangfeng, T.; Feng, Z. Physical Inactivity and Self-Reported Depression among Middle- and Older-Aged Population in South Asia: World Health Survey. BMC Geriatr. 2017, 17, 100. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Babyak, M.A.; O’Connor, C.; Keteyian, S.; Landzberg, J.; Howlett, J.; Kraus, W.; Gottlieb, S.; Blackburn, G.; Swank, A.; et al. Effects of Exercise Training on Depressive Symptoms in Patients with Chronic Heart Failure: The HF-ACTION Randomized Trial. JAMA 2012, 308, 465–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byeon, H. Relationship between Physical Activity Level and Depression of Elderly People Living Alone. Int. J. Environ. Res. Public Health 2019, 16, 4051. [Google Scholar] [CrossRef] [Green Version]
- Chang, A.H.; Lee, J.J.; Chmiel, J.S.; Almagor, O.; Song, J.; Sharma, L. Association of Long-Term Strenuous Physical Activity and Extensive Sitting With Incident Radiographic Knee Osteoarthritis. JAMA Netw. Open 2020, 3, e204049. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.; Snaedal, J.; Einarsson, B.; Bjornsson, S.; Saczynski, J.S.; Aspelund, T.; Garcia, M.; Gudnason, V.; Harris, T.B.; Launer, L.J.; et al. The Association Between Midlife Physical Activity and Depressive Symptoms in Late Life: Age Gene/Environment Susceptibility-Reykjavik Study. J. Gerontol. A. Biol. Sci. Med. Sci. 2016, 71, 502–507. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Lu, W.; Zheng, Y.; Gu, K.; Chen, Z.; Zheng, W.; Shu, X.O. Exercise, Tea Consumption, and Depression among Breast Cancer Survivors. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2010, 28, 991–998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, Q.; Zhang, Q.; Du, Y.; Ye, Y.; He, Q. Associations of Physical Activity, Screen Time with Depression, Anxiety and Sleep Quality among Chinese College Freshmen. PLoS ONE 2014, 9, e100914. [Google Scholar] [CrossRef] [Green Version]
- Griffiths, A.; Kouvonen, A.; Pentti, J.; Oksanen, T.; Virtanen, M.; Salo, P.; Väänänen, A.; Kivimäki, M.; Vahtera, J. Association of Physical Activity with Future Mental Health in Older, Mid-Life and Younger Women. Eur. J. Public Health 2014, 24, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Guddal, M.H.; Stensland, S.Ø.; Småstuen, M.C.; Johnsen, M.B.; Zwart, J.-A.; Storheim, K. Physical Activity and Sport Participation among Adolescents: Associations with Mental Health in Different Age Groups. Results from the Young-HUNT Study: A Cross-Sectional Survey. BMJ Open 2019, 9, e028555. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Coombs, N.; Stamatakis, E. Associations between Objectively Assessed and Self-Reported Sedentary Time with Mental Health in Adults: An Analysis of Data from the Health Survey for England. BMJ Open 2014, 4, e004580. [Google Scholar] [CrossRef]
- Kanamori, S.; Takamiya, T.; Inoue, S.; Kai, Y.; Tsuji, T.; Kondo, K. Frequency and Pattern of Exercise and Depression after Two Years in Older Japanese Adults: The JAGES Longitudinal Study. Sci. Rep. 2018, 8, 11224. [Google Scholar] [CrossRef] [Green Version]
- Karg, N.; Dorscht, L.; Kornhuber, J.; Luttenberger, K. Bouldering Psychotherapy Is More Effective in the Treatment of Depression than Physical Exercise Alone: Results of a Multicentre Randomised Controlled Intervention Study. BMC Psychiatry 2020, 20, 116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, W.C.; Kalarchian, M.A.; Steffen, K.J.; Wolfe, B.M.; Elder, K.A.; Mitchell, J.E. Associations between Physical Activity and Mental Health among Bariatric Surgical Candidates. J. Psychosom. Res. 2013, 74, 161–169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koo, K.-M.; Kim, K. Effects of Physical Activity on the Stress and Suicidal Ideation in Korean Adult Women with Depressive Disorder. Int. J. Environ. Res. Public Health 2020, 17, 3502. [Google Scholar] [CrossRef]
- Nam, J.Y.; Kim, J.; Cho, K.H.; Choi, J.; Shin, J.; Park, E.-C. The Impact of Sitting Time and Physical Activity on Major Depressive Disorder in South Korean Adults: A Cross-Sectional Study. BMC Psychiatry 2017, 17, 274. [Google Scholar] [CrossRef] [Green Version]
- Pengpid, S.; Peltzer, K. Leisure-Time Sedentary Behavior Is Associated with Psychological Distress and Substance Use among School-Going Adolescents in Five Southeast Asian Countries: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 2091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinmo, S.; Hagger-Johnson, G.; Shahab, L. Bidirectional Association between Mental Health and Physical Activity in Older Adults: Whitehall II Prospective Cohort Study. Prev. Med. 2014, 66, 74–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Gool, C.H.; Kempen, G.I.J.M.; Bosma, H.; van Boxtel, M.P.J.; Jolles, J.; van Eijk, J.T.M. Associations between Lifestyle and Depressed Mood: Longitudinal Results from the Maastricht Aging Study. Am. J. Public Health 2007, 97, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Vankim, N.A.; Nelson, T.F. Vigorous Physical Activity, Mental Health, Perceived Stress, and Socializing among College Students. Am. J. Health Promot. AJHP 2013, 28, 7–15. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Ting, R.Z.; Yang, W.; Jia, W.; Li, W.; Ji, L.; Guo, X.; Kong, A.P.; Wing, Y.-K.; Luk, A.O.; et al. Depression in Chinese Patients with Type 2 Diabetes: Associations with Hyperglycemia, Hypoglycemia, and Poor Treatment Adherence. J. Diabetes 2015, 7, 800–808. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, R.L.; Bennie, J.; Abbott, G.; Teychenne, M. Work-Related Physical Activity and Psychological Distress among Women in Different Occupations: A Cross-Sectional Study. BMC Public Health 2020, 20, 1007. [Google Scholar] [CrossRef]
- Jeong, J.-Y.; Lee, S.K.; Kang, Y.-W.; Jang, S.-N.; Choi, Y.J.; Kim, D.-H. Relationship between ED and Depression among Middle-Aged and Elderly Men in Korea: Hallym Aging Study. Int. J. Impot. Res. 2011, 23, 227–234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiely, K.M.; Butterworth, P. Validation of Four Measures of Mental Health against Depression and Generalized Anxiety in a Community Based Sample. Psychiatry Res. 2015, 225, 291–298. [Google Scholar] [CrossRef]
- Bernard, P.; Doré, I.; Romain, A.-J.; Hains-Monfette, G.; Kingsbury, C.; Sabiston, C. Dose Response Association of Objective Physical Activity with Mental Health in a Representative National Sample of Adults: A Cross-Sectional Study. PLoS ONE 2018, 13, e0204682. [Google Scholar] [CrossRef]
- Gautam, R.; Saito, T.; Kai, I. Leisure and Religious Activity Participation and Mental Health: Gender Analysis of Older Adults in Nepal. BMC Public Health 2007, 7, 299. [Google Scholar] [CrossRef] [Green Version]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in Physical Activity and Sedentary Behavior in Response to COVID-19 and Their Associations with Mental Health in 3052 US Adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef]
- Dunstan, D.A.; Scott, N. Clarification of the Cut-off Score for Zung’s Self-Rating Depression Scale. BMC Psychiatry 2019, 19, 177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Makowska, Z.; Merecz, D.; Mościcka, A.; Kolasa, W. The Validity of General Health Questionnaires, GHQ-12 and GHQ-28, in Mental Health Studies of Working People. Int. J. Occup. Med. Environ. Health 2002, 15, 353–362. [Google Scholar] [PubMed]
- Salinas-Rodríguez, A.; Manrique-Espinoza, B.; Acosta-Castillo, G.I.; Franco-Núñez, A.; Rosas-Carrasco, O.; Gutiérrez-Robledo, L.M.; Sosa-Ortiz, A.L. Validation of a cutoff point for the short version of the Depression Scale of the Center for Epidemiologic Studies in older Mexican adults. Salud Publica Mex. 2014, 56, 279–285. [Google Scholar] [CrossRef] [Green Version]
- Ahn, J.V.; Sera, F.; Cummins, S.; Flouri, E. Associations between Objectively Measured Physical Activity and Later Mental Health Outcomes in Children: Findings from the UK Millennium Cohort Study. J. Epidemiol. Community Health 2018, 72, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.W.; Chen, C.-Y.; Stein, M.B.; Klimentidis, Y.C.; Wang, M.-J.; Koenen, K.C.; Smoller, J.W. Major Depressive Disorder Working Group of the Psychiatric Genomics Consortium Assessment of Bidirectional Relationships Between Physical Activity and Depression Among Adults: A 2-Sample Mendelian Randomization Study. JAMA Psychiatry 2019, 76, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Frank, R.G.; Conti, R.M.; Goldman, H.H. Mental Health Policy and Psychotropic Drugs. Milbank Q. 2005, 83, 271–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zschucke, E.; Gaudlitz, K.; Ströhle, A. Exercise and Physical Activity in Mental Disorders: Clinical and Experimental Evidence. J. Prev. Med. Public Health 2013, 46, S12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lordan, G.; Pakrashi, D. Make Time for Physical Activity or You May Spend More Time Sick! Soc. Indic. Res. 2014, 119, 1379–1391. [Google Scholar] [CrossRef]

| Author (Year) Study Name (Reference) ACRONYM | Type of Study | Study Objectives | Sample Size (MH Sample, %) | Age Range, Mean (SD/IQ Range) | PA Measure (Self-Reported/Programme) | MH Problem(s) Assessed | MH PRO Measure (Objective/Self-Reported) Cut-Off for CRS | Results | Overall Effect (+/−, No) |
|---|---|---|---|---|---|---|---|---|---|
| Annerstedt et al. (2012) [33] Health survey ¥ | Cohort (follow-up) | Whether or not an inverse relationship exists between green qualities in the neighbourhood and development of mental disorder. | 8683 (1424, 16.4%) | 18–80 50.1 (unknown) | “How often are you physically active or perform exercise during your leisure time? (self-reported) Not validated measure | Poor Mental Health | GHQ—12 (self-reported) Reporting problems in 3 or more questions Validated measure | The risk of having poor mental health at follow-up decreased 80% if having access to space and being physically active and 70% if access to Space and physically active, compared to not having access to either of these qualities and being physically inactive. These effects were statistically significant for women, but not for men. However, the tendencies were the same for men. We have found that in interaction with physical activity the qualities Serene and Space have some risk-reducing effect on mental health disorders for women, an impact that seems to over shadow the mere amount of nature. | - (conditional) |
| Ball et al. (2009) [24] The Australian Longitudinal Study on Women’s Health/ALSWH ¥ | Cohort (follow-up) | To examine, in a population-based sample of young women, the prospective associations over 3 years between (i) BMI and PA, and depressive symptoms; and (ii) changes in BMI and PA, and depressive symptoms. | 6677 (1691, 26%) | 21–65 Mean not disclosed | Frequency and duration of walking (for recreation or transport), and of moderate- and vigorous-intensity activity in the last week. (self-reported) Not validated measure | Depression | CES-D (self-reported) Score ≥ 10 Validated measure | Adjusted odds of depressive symptoms in 2003 were lower among women who reported any level of PA, compared with women who reported none. After adjustment for sociodemographic variables and BMI, ORs for depressive symptoms in 2003 became nonsignificant for the very low category, but remained significantly lower among women who reported low, moderate (borderline significant or high levels of PA. Compared with women who maintained none or a very low level of PA, those who increased their PA level from none or very low to either a moderate or high level had significantly lower risk of depressive symptoms in 2003, which remained after adjustment for covariates and 2000 BMI, and also after adjustment for covariates and change in BMI (latter data not shown). | - |
| Benedetti et al. (2008) [34] Survey Θ, * | Cross-sectional | To evaluate the association between physical activity level and mental health status among elderly people. | 869 (291, 33.5%) | 60–101 71.6 (SD = 7.9) | International Physical Activity Questionnaire (IPAQ) (self-reported) Validated measure | Dementia and Depression | GMS scale (self-reported) Dementia: score ≥ 3 Depression: score ≥ 7 Validated measure | The present study found a significant relationship between the levels of physical activity and the state of mental health. That is, this association showed lower prevalence of indicators of depression and dementia among non-sedentary elderly people. The importance of keeping active was reaffirmed, along with the fact that physical activity influences how depressive syndrome is faced, through expanding sociability and corporal stimulation. It can be inferred that physical activity is able to reduce and/or delay the risks of dementia, although it cannot be stated that physical activity avoids dementia. | - |
| Bishwajit et al. (2017) [35] ¥ | Cross-sectional | To explore the pattern of physical activity across various demographic and socioeconomic groups in four countries, and to measure the association between PA and self-reported depression among the middle- and older-aged population | 6855 (2380, Prevalence of self-reported depression was respectively 47.7%, 40.3%, 40.4% and 11.4% in Bangladesh, India, Nepal and Sri Lanka respectively) | 50 and over Bangladesh [60.72 (SD = 9.6)]; India [59.94 (SD = 9.1)]; Nepal [60.5 (SD = 9)]; Sri Lanka [60 (SD = 9.08)] | Time dedicated to MPA and VPA (self-reported) Not validated measure | Depression | Clinical diagnosis (objective) | With regard to diagnosed depression, compared to those who reported engaging in MPA on daily basis, the odds of reporting depression were more than five times higher [AOR = 5.512; 95% CI = 1.159–26.21] for those who never took MPA in Bangladesh. In India, those never took VPA had 44% higher [AOR = 1.442; 95% CI = 1.046–1.987] odds of being diagnosed with depression compared those who never engaged in VPA. | - |
| Blumenthal et al. (2012) [36] HF-Action ¥ | RCT | To determine whether exercise training will result in greater improvements in depressive symptoms compared with usual care among patients with heart failure. | 2322 (653, 28,1%) | 19–91 56 (IQ range = 50–63) | Supervised & home-based aerobic exercise training sessions (programme) | Depression | BDI-II scale (self-reported) score ≥ 14 Validated measure | Exercise training may be effective in reducing depressive symptoms and by further documenting the prognostic significance of depression in patients with heart failure. In this ancillary study from the HFACTION trial, patients with heart failure who participate in exercise training, compared with usual care, had modest reductions in depressive symptoms at 12 months, although the clinical significance of these small improvements is unknown. | - |
| Byeon et al. (2019) [37] The Korea National Health and Nutrition Examination Survey (KNHANES) Θ | Cross-sectional | To investigate the relationship between physical activity and depression in the elderly living alone and to provide basic data for the prevention of depression in the elderly. | 256 (45, 19%) | 65 and over | Regular physical activities performed on average in a week were investigated using a self-care questionnaire. (self-reported) Not validated measure | Depression | PHQ-9 scale (self-reported) score ≥ 10 Validated measure | This study showed that regular flexibility exercises were independently related to depression prevention. The flexibility exercise of the elderly was independently associated with depression prevention. The results of this study implied that persistent flexibility exercise (e.g., stretching and freehand exercise) might be more effective to maintain a healthy mental status than muscular strength exercise. A longitudinal study is required to prove the causal relationship between physical activity and depression in old age. | - (some techniques more than others) |
| Chang et al. (2020) [38] Survey in Taiwan ¥ | Cross-sectional | To investigate the long-term association between midlife PA and late-life depressive symptoms, on average 25 years later, in a population free of clinical history of depression and diagnosis of dementia. | 1114 (MH sample not reported) | Range not disclosed 35.9 (SD = 15.16) | Exercise. Any activity they chose to do as their exercise (e.g., workouts at home, running outside, etc.). (self-reported) Not validated measure | Mood state | POMS (self-reported) At least 10 items answered Validated measure | There was a significant main effect of exercise frequency during the pandemic on mood states. Those who exercised four days or more had significantly higher mood states compared to those who exercised for 2–3 days (bduring3-2 = 0.14, p = 0.04), and those exercised for 2–3 days had significantly higher mood states compared to those who exercised one day or less per week during the pandemic (bduring2-1 = 0.29, p < 0.001). There was also a significant main effect of pre-pandemic exercise frequency on mood states. Specifically, those who exercised four days or more per week pre-pandemic had a significantly lower mood state during the pandemic, compared to those who exercised for 2–3 days per week pre-pandemic (bpre3-2 = 0.16, p = 0.03). However, there was a significant interaction effect on exercise frequency levels during the pandemic x pre-pandemic exercise frequency levels on mood (bpre x during = 0.48–0.42, p = 0.01–0.03). Meaning, the effects of pre-pandemic exercise frequency on mood were dependent on exercise frequency during the pandemic. | - |
| Chang et al. (2016) [39] Age Gene/Environment Susceptibility (AGES)—Reykjavik Study §, Θ | Cohort (follow-up) | To investigate the long-term association between midlife PA and late-life depressive symptoms, on average 25 years later, in a population free of clinical history of depression and diagnosis of dementia. | 4140 (216, 5.5%) | 65 and over Mean not disclosed | Regular participation in sports or exercise, and hours per week (self-reported) Not validated measure | Depression | GDS-15 (self-reported) score ≥ 6 Validated measure | This longitudinal study over a period of 25 years found a strong association between midlife PA and depressive symptoms in late life among community dwelling old people who did not have a history of depression. Compared with those who were inactive at midlife, those who were active at midlife had significantly less depressive symptoms 25 years later even after controlling for demographics, physiological markers, and various aspects of cognitive function. | - |
| Chen et al. (2010) [40] Questionnaire ¥ | Cohort (follow-up) | To examine the association of lifestyle factors and supplement use with depression among breast cancer survivors. | 1399 (176, 12.5%) | Adults, not specified 53.7 (SD = 9.8) | Exercise questionnaire (self-reported) Validated measure | Depression (self-reported) | CES-D scale (self-reported) score ≥ 16 Validated measure | Regular exercise participation may play an important role in the prevention of depression among breast cancer survivors. | - |
| Coll et al. (2019) [30] The Physical Activity for Mothers Enrolled in Longitudinal Analysis (PAMELA) study ¥ | RCT | To assess the efficacy of a 16-week exercise intervention during pregnancy on the prevention of postpartum depression using data from a large RCT. | 639 (579, 90.6%) | Young women, range unspecified 27.1 (SD = 5.1) | 16-week supervised exercise program including aerobic and resistance training delivered in 60-min sessions 3 times per week (programme) | Depression (postpartum) | EPDS (self-reported) score ≥ 12 Validated measure | There were no significant differences between study groups in the rates of postpartum depression (12 of 192 [6.3%] in the intervention group and 36 of 387 [9.3%] in the control group; OR, 0.65; 95%CI, 0.33–1.28). Sensitivity analysis using multiple imputation to deal with missing data yielded virtually identical results. | No |
| Feng et al. (2014) [41] Questionnaire §, ¥ | Cross-sectional | To investigate the independent and interactive associations of physical activity (PA) and screen time (ST) with depression, anxiety and sleep quality among Chinese college students. | 1106 (201, 18.2%) | 16–24 18.9 (SD = 0.9) | Frequency of physical activity (self-reported) Not validated measure | Depression and Anxiety | SDS and SAS (self-reported) Anxiety: score ≥ 50 Depression: score ≥ 53 Validated measure | The present study suggests an independent and interactive relationship of high PA and low ST with significantly reduced prevalence of mental health problems and favorable sleep quality among Chinese college freshmen. These results provide support for the notion that maintaining sufficient PA and reducing sedentary behaviors should be included in the planning of health promotion strategies. | - |
| Griffiths et al. (2014) [42] Survey data derived from the Finnish Public Sector Study (FPSS) ¥ | Cohort (follow-up) | To explore the relationship between physical activity and symptoms of mental ill-health in a large, well defined and heterogeneous sample of working women. | 26,913 (4666, 17%) | 18–69 45.6 (SD = 9.8) | Average time spent on physical activity (self-reported) Not validated measure | Mental ill-health | GHQ-12 (self-reported) score ≥ 4 Validated measure | The results of this study with a large cohort of Finnish working women showed that physical activity was associated with a reduced future risk of mental ill-health. These findings also demonstrated an inverse dose–response relationship between physical activity and likelihood of later symptoms of mental ill-health. In addition, our findings revealed that mid-life and older women who reported increased levels of physical activity were at significantly less risk of later mental ill-health than those who did not increase physical activity. No association was observed in the group of younger women | - |
| Guddal et al. (2019) [43] Young HUNT3 study ¥ | Cross-sectional | To describe PA levels and sport participation in a population-based sample of adolescents, and to explore how they relate to mental health in different age groups. | 7619 (933, 12.2%) | 13–19 15.8 (SD = 1.7) | Leisure time PA and type and frequency of sport participation (self-reported) Validated measure | Psychological distress | SCL-5 (self-reported) score ≥ 2 Validated measure | In this population-based sample of adolescents, PA levels and participation rates in sports were lower among girls, and lower among senior high school students compared with junior high school students. These results showed that higher levels of PA were favorably associated with self-esteem and life satisfaction throughout adolescence, as well as with reduced likelihood of psychological distress in senior high school students. Team sport participation was associated with mental health benefits, especially for girls. | - |
| Hamer et al. (2017) [18] The Health Survey for England (HSE) and the Scottish Health Survey (SHS) ¥ | Cross-sectional | To compare associations between objectively assessed and self-reported sedentary time with mental health in adults. | 108,011 (15,661, 14.5%) | Adults, range not specified 47 (SD = 17) | Questionnaire to enquire about frequency, duration and pace of walking and participation in sports and exercises including cycling, swimming, running, football, rugby, tennis and squash (self-reported) Validated measure | Psychological distress | GHQ-12 (self-reported) Score > 3 Validated measure | The pattern of results was essentially the same in men and women and across different age categories. Slightly stronger associations were observed in participants >60 yrs. of age. Significant interaction (p < 0.05) by longstanding illness was observed. Results suggest that presence of chronic illness is an important factor in modifying associations between PA and mental health; among participants reporting longstanding health conditions, reduced odds of psychological distress below the PA guidelines were observed, from as little as one to two sessions per week of MVPA. Given that just under half (~44%) of this general population sample of adults reported a longstanding health condition, this is an important factor in potentially modifying associations between PA and mental health. | - (specially for the aged >60 or with chronic conditions) |
| Hamer et al. (2014) [44] HSE ¥ | Cross-sectional | To explore if mental health benefits can be optimized by accumulating PA in certain patterns. | 11,658 (1486, 12.7%) | 16–95 50 (SD unknown) | Uniaxial accelerometer that records movement on the vertical axis, the Actigraph GT1M (Actigraph, Pensacola, Florida, USA), during waking hours for seven consecutive days. (programme) | Psychological distress | GHQ-12 (self-reported) score ≥ 4 Validated measure | Sedentary time is associated with adverse mental health. Sedentary time (<200 CPM) was directly associated with psychological distress after adjustment for all covariables including MVPA, although this was more apparent in the highest tertile (OR = 1.74, 95% CI 1.07 to 2.83). Light activity (200–2018 CPM) was inversely associated with risk for psychological distress, although the association was not linear. MVPA, however, was not associated with psychological distress in any models. MVPA was inversely associated with risk of psychological distress in a dose–response manner (p<0.001 for all models). | + |
| Kanamori et al. (2018) [45] The JAGES longitudinal study Θ | Cohort (follow-up) | To examine (1) the relationship between frequency of exercise at baseline and later depression in older Japanese adults and (2) the relationship between exercise patterns at baseline (non-exercisers, exercising alone only, or exercising with others) and later depression, and (3) the relationship between combinations of frequency of exercise and exercise patterns at baseline with later depression. | 1422 (MH subsample not specified) | 65 and over 72.5 (SD = 4.9) | Total frequency/pattern of exercise (self-reported) Not validated measure | Depression | GDS-15 (self-reported) score ≥ 5 Validated measure | The results of the present study suggest that exercising two or more times a week and/or exercising with others can lower the risk of depression in older Japanese adults. When promoting exercise to older adults to prevent depression, social aspects should be considered in addition to frequency | - |
| Karg et al. (2020) [46] The StudyKuS §, ¥ | Cohort (follow-up) | To investigate the effectiveness of a manualised bouldering psychotherapy (BPT), compared with exercise alone, in a large nationwide sample of outpatients with depression. | 133 (133, 100%) | 18 and over 42 (SD = 12.5) | Bouldering psychotherapy &home-based exercise programmes. (programme) | Depression | MADRS (Diagnosis) | The results of the current study provide support for previous findings in suggesting positive effects of physical activity and particularly bouldering in depressed individuals. Moreover, it is evident that our bouldering psychotherapy is not only efficacious in reducing depressive symptoms but even goes beyond the benefits of mere physical exercise. | - |
| King et al. (2013) [47] The Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) §, ¥ | Cross-sectional | To examine associations between physical activity (PA) and mental health among adults undergoing bariatric surgery. | 850 (735, 86.4%) | 36–53 Mean not disclosed | Preoperative PA was assessed in one half of LABS-2 participants with the StepWatch™ 3 Activity Monitor (programme) | Depression | MCS and BDI (self-reported) Mild severe: score 10–18 Moderate-severe: score ≥19 Validated measure | This study revealed an inverse association between rather modest levels of PA and depressive symptoms and recent treatment for depression or anxiety, in a large cohort of adults with class 2 and 3 obesity undergoing bariatric surgery at one of 10 hospitals throughout the U.S. Although causality cannot be established, our findings are encouraging and should leverage further investigation of the role of PA in prevention and treatment of depression and anxiety in adults with class 2 and 3 obesity, as PA may prove to be a comparatively safe and cost-effective treatment option. | - |
| Koo and Kim (2020) [48] The KNHANES study ¥ | Cross-sectional | To investigate the effects of physical activity (PA) on the stress and suicidal ideation of Korean adult women with depressive disorder. | 1315 (1315, 100%) | 19–65 Mean not disclosed | International Physical Activity Questionnaire (IPAQ), which is a standardized questionnaire designed to measure and compare the level of PA of various populations (aged 16–65) around the world (self-reported) Validated measure | Depression | Clinical diagnosis for depression + The perception of stress, which is a dependent variable, was asked as “How much stress do you usually feel in your daily life?” (self-reported) Low: Score = 1 High: Score = 2 Not validated measure | In this study, flexibility exercises played an important role in reducing and preventing stress and suicidal ideation in Korean adult women with depressive disorder. However, strength exercises and walking did not have significant effects on stress and suicidal ideation in Korean adult women with depressive disorder. Future studies need to consider determining which exercises aside from strength exercises, flexibility exercises, and walking are effective to reduce stress and suicidal ideation in women with depressive disorder. | - |
| Nam et al. (2017) [49] The KNHANES study ¥ | Cross-sectional | To examine the relationship between sitting-time and MDD and estimate the effects of sitting-time and PA on MDD in a representative South Korean population. | 4145 (424, 10.2%) | 20 and over | Overall daily sitting time & IPAQ questionnaire (self-reported) Validated measure | Major Depressive Disorder | PHQ-9 (self-reported) score ≥ 8 Validated measure | This study showed that sitting for long periods was associated with greater risk of MDD in South Korean adults. The findings accentuated the importance of reducing overall sitting time and increasing PA and suggested that policymakers should develop strategies involving PA, to decrease sitting time and alleviate the burden of depression in terms of fiscal health premiums and social problems. | + |
| Pengpid and Peltzer (2019) [50] Cross-sectional data from the Global School-Based Student Health Survey (GSHS) of five Southeast Asian countries ¥ | Cross-sectional | To investigate the associations of leisure-time sedentary behavior with psychological distress and with substance use among school-going adolescents in five Southeast Asian countries. | 32,696 (7585, 23.1%) | 11 and over (adolescents) Mean not reported Median = 14 years (IQ range = 2) | Leisure time & days per week on physical activities (self-reported) Not validated measure | Psychological distress | The psychological distress items (no, single and multiple). (self-reported) Single: score = 1 Multiple: score ≥ 2 Not validated measure | Students who spent three or more hours engaged in leisure-time sedentary behavior were more likely to have single and multiple psychological distress. | + |
| Shigdel et al. (2019) [32] The HUNT study ¥ | Cohort (follow-up) | To examine the relationship between estimated Cardio Respiratory Fitness (eCRF) with depression and anxiety cross-sectionally and longitudinally in a representative population of middle-aged and older adults from Norway. | Cross-sectional: 26,615 (7141, 26.8%) Longitudinal: 14,020 (1847, 13.1%) | 19–90 55.7 (11.4) | Two PA question on weekly duration of hard PA (being sweat and breathless) and light PA (not being sweat and breathless) from HUNT 2 (self-reported) Validated measure | Anxiety and depression | HADS-D and HADS-A (self-reported) scores ≥ 8 Validated measure | In this large cohort study, medium and high levels of eCRF were associated with a lower risk of depression as compared to those with low eCRF level, even after adjustment for well-known risk factors in both cross-sectional and longitudinal analyses. Specifically, we found 11% and 8% lower risk of depression for each unit increase in MET in cross-sectional and longitudinal data respectively. However, our data do not support a statistically significant association of MET with anxiety neither in cross-sectional analysis nor in longitudinal analysis. | - with Depression; No with Anxiety. |
| Steinmo et al. (2014) [51] The Whitehall II study ¥ | Cohort (follow-up) | To investigate longitudinal and bidirectional associations between mental health and physical activity from midlife into old age. | 6909 (1041, 15.1%) | 45–69, 50–74 and 55–80 54.2 (5.7) | Total weekly hours of physical activity were converted into standardised Metabolic Equivalent of Task (MET) values (self-reported) | Probable depression & poor mental health | SF-36 MCS and GHQ (self-reported) MCS score of ≤42 GHQ ≥ 5 | From midlife to old age, greater physical activity is associated with better mental health and vice versa. These findings suggest persistent longitudinal and bidirectional associations between physical activity and mental health. | - |
| Underwood et al. (2013) [31] RCT, no name §, Θ | Cohort (follow-up) | To test the hypothesis that a moderate intensity exercise programme would reduce the burden of depressive symptoms in residents of care homes. | 765 (595, 77.7%) | 65 and over Mean no disclosed | Exercise classes to provide a moderate intensity strength and aerobic training stimulus (programme) | Depression | GDS-15 (self-reported) score ≥ 15 Validated measure | This moderately intense exercise programme did not reduce depressive symptoms in residents of care homes. In this frail population, alternative strategies to manage psychological symptoms are required. | No |
| Van Gool et al. (2006) [52] The longitudinal Maastricht survey ¥ | Cohort (follow-up) | To determine whether healthy lifestyles are associated, over time, with absence of depressed mood in the general population. | 1169 (164, 14%) | 21–48 48.9 (SD = 14.17) | Mean numbers of minutes spent daily on physical exercise at baseline and follow-up (self-reported) Not validated measure | Depression | CES-D (self-reported) score > 16 Validated measure | Significant longitudinal protective effect of baseline physical exercise (at recommended levels) on subsequent depressed mood. | - |
| Van Kim & Nelson (2013) [53] Web-based questionnaire ¥ | Cross-sectional | To examine cross-sectional associations between vigorous physical activity, mental health, perceived stress, and socializing among 4-year college students. | 14,706 (1145, 7.7%) | 18 and over (adults) Mean no disclosed | Question from the Youth Behavior Risk survey to assess vigorous PA (self-reported) Validated measure | Poor mental health & perceived stress | The five-item mental health scale from the Short Form–36 (SF-36) health scale (self-reported) Poor MH: score <40 Perceived stress: score 9 to 16 Validated measure | In conclusion, there appears to be an inverse association between vigorous PA in college and both poor mental health and perceived stress. This relationship remained after accounting for socializing. However, additional research using longitudinal data is needed to more accurately assess the influence of PA on mental health and perceived stress from high school to college. Among college students in particular, peer support interventions aimed at either increasing or maintaining PA levels could help improve mental health and reduce perceived stress as well as maintain physical health. In addition, mental health and stress management interventions could potentially include PA components combined with social support. | - |
| Zhang & Yen (2015) [54] U.S. Behavioral Risk Factor Surveillance System (BRFSS) questionnaire ¥ | Cross-sectional | To investigate the roles of physical activity (exercise) and sociodemographic factors in depressive symptoms among men and women in the United States. | 11,560 (1056, 9.13%) | 18–99 54 (16) | The measurement for PA is drawn from BRFSS questionnaire item “How many times per week or per month did you take part in this activity during the past month?” (self-reported) Not validated measure | Depression | PHQ-8 (self-reported) Severe Depression: score = 4 Validated measure | The primary finding is that regular PA ameliorates DS, decreasing the probability of moderate DS among men, and the probabilities of mild, moderate, and moderately severe DS among women. Mildly and moderately depressed women will benefit the most from regular PA. These results echo findings in previous studies, mostly with small and sectorial samples, that PA can reduce symptoms of mild to moderate depression. The use of a switching probability model allows quantification of these effects of PA and, more important, the segmented sample analysis uncovers important differences between men and women in the effects of PA on the probabilities of DS. | - |
| Study | Selection Bias | Ecological Fallacy | Confounding Bias | Reporting Bias | Time Bias | Measurement Error in Exposure (PA) Variable | Measurement Error in (Mental) Health Outcome | Overall bias Check Assessment |
|---|---|---|---|---|---|---|---|---|
| Annerstedt (2012) [33] | Moderate | Strong | Strong | Strong | Weak Time of data collection 2005 | Moderate | Strong | Moderate |
| Ball et al. (2009) [24] | Moderate | Strong | Strong | Strong | Weak Time of data collection 2000–2003 | Strong | Strong | Moderate |
| Benedetti et al. (2008) [34] | Moderate | Strong | Moderate | Moderate | Moderate | Moderate | Strong | Strong |
| Bishwajit et al. (2017) [35] | Strong | Strong | Moderate | Strong | Weak Time of data collection 2002–2004 | Moderate | Strong | Moderate |
| Blumenthal et al. (2012)* [36] | Strong | Strong | Moderate | Moderate | Strong | Strong | Strong | Strong |
| Byeon et al. (2019) [37] | Moderate | Strong | Strong | Strong | Strong | Moderate | Moderate | Strong |
| Chang et al. (2020) [38] | Weak No statistical method used to predetermine sample size | Strong | Moderate | Strong | Strong | Strong | Strong | Moderate |
| Chang et al. (2016) [39] | Strong | Strong | Strong | Strong | Moderate | Moderate | Moderate | Strong |
| Chen et al. (2010) [40] | Strong | Strong | Moderate | Strong | Moderate | Strong | Strong | Strong |
| Coll et al. (2019)* [30] | Strong | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Feng et al. (2014) [41] | Strong | Strong | Strong | Strong | Strong | Moderate | Moderate | Strong |
| Griffiths et al. (2014) [42] | Strong | Strong | Strong | Moderate | Moderate | Moderate | Moderate | Strong |
| Guddal et al. (2019) [43] | Moderate | Strong | Strong | Strong | Weak Time of data collection 2006–2008 | Strong | Strong | Moderate |
| Hamer et al. (2017) [18] | Strong | Strong | Moderate | Strong | Weak Time of data collection 1994–2004 | Strong | Strong | Moderate |
| Hamer et al. (2014) [44] | Strong | Strong | Strong | Strong | Moderate | Strong | Moderate | Strong |
| Kanamori et al. (2018) [45] | Weak Not representative sample | Strong | Moderate | Strong | Moderate | Moderate | Strong | Moderate |
| Karg et al. (2020) [46] | Strong | Strong | Strong | Strong | Strong | Strong | Strong | Strong |
| King et al. (2013) [47] | Strong | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Koo and Kim (2020) [48] | Strong | Strong | Moderate | Strong | Moderate | Strong | Weak Not validated scale | Moderate |
| Nam et al. (2017) [49] | Strong | Strong | Moderate | Strong | Moderate | Strong | Strong | Strong |
| Pengpid and Peltzer (2019) [50] | Strong | Strong | Strong | Weak Inaccurate reporting some aspects of the study | Moderate | Moderate | Moderate | Moderate |
| Shigdel et al. (2019) [32] | Strong | Strong | Strong | Strong | Moderate | Strong | Moderate | Strong |
| Steinmo et al. (2014) [51] | Weak | Strong | Moderate | Strong | Moderate | Moderate | Moderate | Moderate |
| Underwood et al. (2013) [31] | Strong | Strong | Strong | Strong | Moderate | Moderate | Moderate | Strong |
| Van Gool et al. (2007) [52] | Moderate | Strong | Moderate | Strong | Weak | Strong | Strong | Moderate |
| VanKim & Nelson (2013) [53] | Strong | Strong | Moderate | Weak Inaccurate reporting some aspects of the study | Moderate | Strong | Strong | Moderate |
| Zhang & Yen (2015) [54] | Moderate | Strong | Strong | Strong | Strong | Moderate | Strong | Strong |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maynou, L.; Hernández-Pizarro, H.M.; Errea Rodríguez, M. The Association of Physical (in)Activity with Mental Health. Differences between Elder and Younger Populations: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 4771. https://doi.org/10.3390/ijerph18094771
Maynou L, Hernández-Pizarro HM, Errea Rodríguez M. The Association of Physical (in)Activity with Mental Health. Differences between Elder and Younger Populations: A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2021; 18(9):4771. https://doi.org/10.3390/ijerph18094771
Chicago/Turabian StyleMaynou, Laia, Helena M. Hernández-Pizarro, and María Errea Rodríguez. 2021. "The Association of Physical (in)Activity with Mental Health. Differences between Elder and Younger Populations: A Systematic Literature Review" International Journal of Environmental Research and Public Health 18, no. 9: 4771. https://doi.org/10.3390/ijerph18094771
APA StyleMaynou, L., Hernández-Pizarro, H. M., & Errea Rodríguez, M. (2021). The Association of Physical (in)Activity with Mental Health. Differences between Elder and Younger Populations: A Systematic Literature Review. International Journal of Environmental Research and Public Health, 18(9), 4771. https://doi.org/10.3390/ijerph18094771







