COVID-19 Medical Vulnerability Indicators: A Predictive, Local Data Model for Equity in Public Health Decision Making
Abstract
:1. Introduction
2. Materials and Methods
2.1. Geographic Unit of Analysis
2.2. Data Sources
2.2.1. AskCHIS Neighborhood Edition
2.2.2. American Community Survey
2.2.3. California Department of Parks and Recreation
2.3. Construction of the Indicators
2.3.1. Pre-Existing Health Vulnerability
- Heart disease, defined as any adult respondent over the age of 18 ever diagnosed with heart disease by a doctor. We included heart disease as a dimension in lieu of specific data on hypertension which has been identified as one of the most common comorbidities related to increased COVID-19 risk [17,21,23].
- Health status, defined has any adult respondents ages 18–64 with fair or poor health. We included health status as a measure of fair or poor health as a substitute for other pre-existing health conditions absent from our data sources.
- Mental health, defined as any adult respondent over the age of 18 who reported serious psychological distress in the past 12 months, constructed using the Kessler 6 series (K6 greater or equal to 13). People with severe mental health tend to have higher levels of pre-existing conditions, such as type 2 diabetes and heart disease, than the general population [45].
- Food insecurity, defined as any adult respondent over the age of 18 with income less than 200% below the federal poverty line who self-identified their ability to afford enough food [46]. We included this variable as a measure of poor nutrition. Poor nutrition is a leading factor in contributing to widespread instances of diabetes and obesity across the world [47].
2.3.2. Barriers to Accessing Health Care
- Non-U.S. citizens, defined as the share of immigrants who are not U.S. citizens. We include non-U.S. citizens because this population often faces cultural and legal barriers to accessing health care. Most of this group are from non-Western countries, and may risk being labeled a “public charge,” which could potentially jeopardize their immigrant status. A disproportionate number also have limited English language ability, and lack of health insurance, which are factors included separately in the indicator.
- English language barrier, defined as the share of the population aged 5 years or older that speak English “less than well”. Language barriers can often prevent people from accessing important information in a timely manner. Many organizations lack the resources necessary to provide documents in multiple languages. Even if organizations have enough resources, it takes time to provide all the necessary information in languages that are accessible to different communities. This delay in translation applies to information regarding COVID-19 risk and prevention.
- Lack of broadband access, defined as the share of households with a computer but without broadband internet access. Lack of broadband hinders access to important information distributed by local and federal health agencies regarding COVID-19, such as where to find the closest COVID-19 testing center.
- Lack of Health Insurance, defined as the share of individuals without health insurance. Despite the fact that the Coronavirus Aid, Relief, and Economic Security Act (CARES Act) reimburses the medical cost of those with COVID-19, lack of health care insurance may cause delays in accessing preventive care and seeking other health-related benefits. Moreover, many may not know about this provision in the CARES Act.
- Vehicles per person, defined as the inverted ratio of vehicles available per person. We inverted the ratio to indicate a higher level of vulnerability for households that have fewer cars per person. Depending on the number of cars available per person, having the availability to use a car for medical purposes might not be an option given that there might be other priorities such as getting to work or school that prevents people in the household from getting the health care they need. Moreover, some COVID-19 testing sites in Los Angeles require that people arrive in a motorized vehicle. For example, Dodger Stadium serves as LA County’s largest coronavirus drive-through testing site.
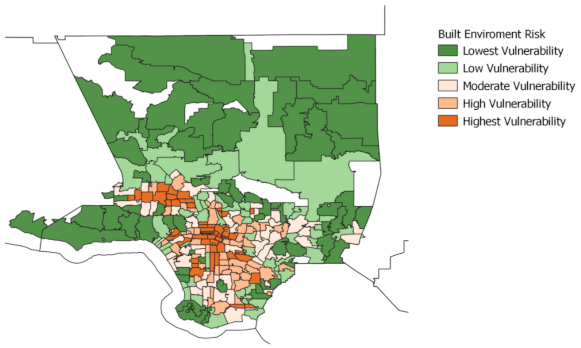
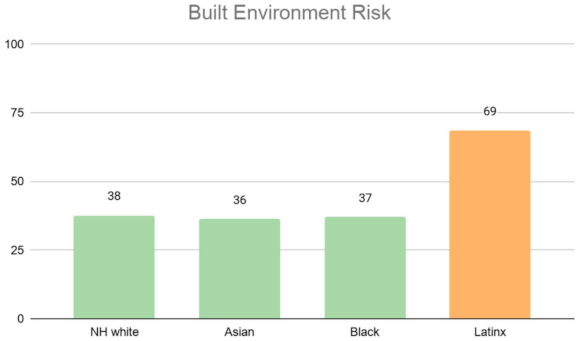
2.3.3. Built Environment Risk
- Population density, operationally defined as the total number of persons divided by the ZCTA’s land area in square miles. Counts of the population are derived from the 2014–2018 five-year ACS. Places that are densely populated increases the chances of encountering people, which limits the ability to maintain social distancing guidelines and increases the likelihood of encountering a COVID-19 carrier.
- Building structure density, operationally defined as housing structures with 10 or more units divided by the total housing stock (i.e., as a share of all housing units in the ZCTA). Similar to population density, building density also increases chances of encountering people which limits social distance guidelines and increases likelihood of encountering a COVID-19 carrier. We focus on 10 or more units because as opposed to including all multi-units (e.g., duplexes, triplexes), structures with 10 or more units are more likely to increase one odds of encountering people in common areas (e.g., lobby, hallways, mailrooms) and therefore increases the risk and COVID-19 contagion.
- In-unit housing crowding, operationally defined as having 1.01 or more persons per room. In-unit crowding can increase a person’s risk to COVID-19 infection. If someone in a household becomes infected with COVID-19 and there is not a room for them to quarantine in, the rest of the household has a higher risk of contracting the disease. A study recently found that areas with the highest number of COVID-19 cases faced three-times the level of overcrowding than areas with the lowest number of COVID-19 cases [48].
- Availability of parks and open space per 1000 residents. Areas with more parks and open space enable individuals to more easily keep physically and mentally fit through outdoor exercise or activity.
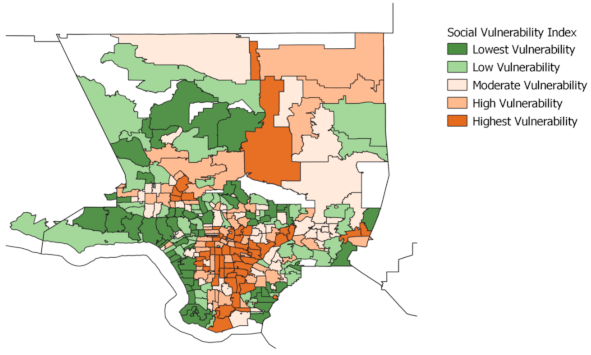
2.3.4. Social Vulnerability Index
- 1.
- Socioeconomic status
- Persons below poverty, defined as the share of persons with income below the federal poverty line;
- Unemployed, defined as the share of civilian labor force population (ages 16 and over) who are unemployed;
- Per capita income, a measure of the amount of income earned per person;
- No high school diploma, defined as share of persons age 25 and older with no high school diploma.
- 2.
- Household composition
- Persons aged 65 or older as a share of the total population;
- Persons aged 17 or younger as a share of the total population;
- Civilian non-institutionalized population with a disability, defined as any individuals age 5 years or older with a disability;
- Single-parent households with children under 18 as a share of total households.
- 3.
- Minority status and language
- Racial minority population, defined as the share of the population who are not non-Hispanic White (e.g., total population minus non-Hispanic White);
- Speaks English “less than well”, defined as the share of the population aged 5 years of older that speak English “less than well.”
- 4.
- Housing type and transportation
- Multi-unit structure, defined as the share of housing structures with 10 housing units or more;
- Mobile homes, defined as the share of mobile homes;
- In-unit housing crowding, defined as having 1.01 or more persons per room;
- No-vehicle households, defined as households with no vehicles available as a share of all households;
- Group quarters, defined as share of persons in institutionalized group quarters.
2.4. Ranking Methodology
2.5. Method for Assessing Ethnoracial and Vulnerability Distributions
3. Results
3.1. Maps
3.2. Results for Analysis of Racial Distribution
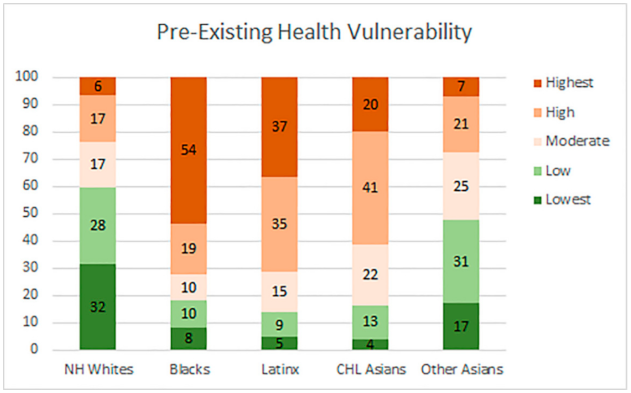
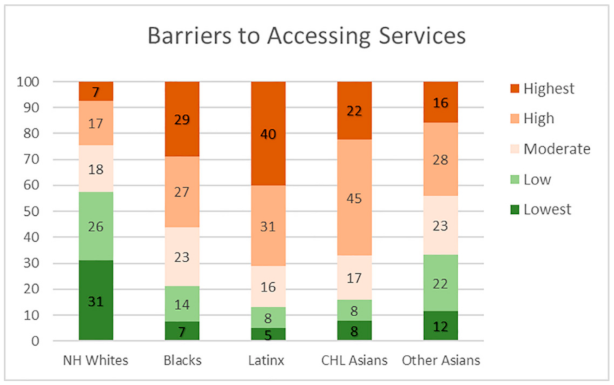
3.2.1. Distribution of Vulnerability within Ethnoracial Groups
3.2.2. Vulnerability Levels by Racial Majority Groups
3.2.3. Neighborhood Socio-Demographic Characteristics by Levels of Medical Vulnerability
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tracking the Coronavirus in Los Angeles County. Los Angeles Times. Available online: https://www.latimes.com/projects/california-coronavirus-cases-tracking-outbreak/los-angeles-county/ (accessed on 22 January 2021).
- Gravlee, C.C. Systemic racism, chronic health inequities, and COVID-19: A syndemic in the making? Am. J. Hum. Biol. 2020, 32, e23482. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.T.; Krieger, N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J. Public Health Manag. Pract. 2021, 27, S43–S56. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.H.; Moonesinghe, R.; Truman, B.I. COVID-19 hospitalization by race and ethnicity: Association with chronic conditions among medicare beneficiaries. J. Racial. Ethn. Health Disparities 2021, 8, 1–10. [Google Scholar] [CrossRef]
- Rader, B.; Scarpino, S.V.; Nande, A.; Hill, A.L.; Adlam, B.; Reiner, R.C.; Pigott, D.M.; Gutierrez, B.; Zarebski, A.E.; Shrestha, M.; et al. Crowding and the shape of COVID-19 epidemics. Nat. Med. 2020, 26, 1829–1834. [Google Scholar] [CrossRef] [PubMed]
- Ong, P.M.; Gonzalez, S.R. Uneven Urbanscape: Spatial Structures and Ethnoracial Inequality; Cambridge University Press: Cambridge, UK, 2019. [Google Scholar]
- Kolak, M.; Bhatt, J.; Park, Y.H.; Padron, N.A.; Molefe, A. Quantification of neighborhood-level social determinants of health in the continental United States. JAMA 2020, 1, e1919928. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N.; Kim, R.; Feldman, J.; Waterman, P.D. Using the index of concentration at the extremes at multiple geographical levels to monitor health inequities in an era of growing spatial social polarization: Massachusetts, USA (2010–14). Int. J. Epidemiol. 2018, 47, 788–819. [Google Scholar] [CrossRef]
- Alam, M.R.; Kabir, M.R.; Reza, S. Comorbidities might be a risk factor for the incidence of COVID-19: Evidence from a web-based survey. Prev. Med. Rep. 2021, 21, 101319. [Google Scholar] [CrossRef]
- Hooper, J.E.; Padera, R.F.; Dolhnikoff, M.; da Silva, L.F.F.; Duarte-Neto, A.N.; Kapp, M.E.; Lacy, J.M.; Mauad, T.; Saldiva, P.H.N.; Rapkiewicz, A.V.; et al. A post-mortem portrait of the Coronavirus Disease 2019 (COVID-19) pandemic: A large multi-institutional autopsy survey study. Arch. Pathol. Lab. Med. 2021. [Google Scholar] [CrossRef]
- Wei, Z.Y.; Qiao, R.; Chen, J.; Huang, J.; Wu, H.; Wang, W.J.; Yu, H.; Xu, J.; Wang, C.; Gu, C.H.; et al. The influence of pre-existing hypertension on coronavirus disease 2019 patients. Epidemiol. Infect. 2021, 149, e4. [Google Scholar] [CrossRef]
- Vijayan, T.; Shin, M.; Adamson, P.C.; Harris, C.; Seeman, T.; Norris, K.C.; Goodman-Meza, D. Beyond the 405 and the 5: Geographic variations and factors associated with SARS-CoV-2 positivity rates in Los Angeles County. Clin. Infect Dis. 2020, ciaa1692. [Google Scholar] [CrossRef]
- Dorn, A.V.; Cooney, R.E.; Sabin, M.L. COVID-19 exacerbating inequalities in the U.S. Lancet 2020, 395, 1243–1244. [Google Scholar] [CrossRef]
- Gross, C.P.; Essien, U.R.; Pasha, S.; Gross, J.R.; Wang, S.Y.; Nunez-Smith, M. Racial and ethnic disparities in population level COVID-19 mortality. MedRxiv 2020. [Google Scholar] [CrossRef]
- DiMaggio, C.; Klein, M.; Berry, C.; Frangos, S. Blacks/African American communities are at highest risk of COVID-19: Spatial modeling of New York City ZIP code-level testing results. Ann. Epidemiol. 2020, 51, 7–13. [Google Scholar] [CrossRef]
- Wiemers, E.E.; Abrahams, S.; AlFakhri, M.; Hotz, V.J.; Schoeni, R.F.; Seltzer, J.A. Disparities in vulnerability to severe complications from COVID-19 in the United States (No. w27294). MedRxiv 2020. [Google Scholar] [CrossRef]
- Myers, L.C.; Parodi, S.M.; Escobar, G.J.; Liu, V.X. Characteristics of hospitalized adults with COVID-19 in an integrated health care system in California. JAMA 2020, 323, 2195–2198. [Google Scholar] [CrossRef]
- Hajifathalian, K.; Kumar, S.; Newberry, C.; Shah, S.; Fortune, B.; Krisko, T.; Ortiz-Pujols, S.; Zhou, X.K.; Dannenberg, A.J.; Kumar, R.; et al. Obesity is associated with worse outcomes in COVID-19: Analysis of early data from New York City. Obesity 2020, 28, 1606–1612. [Google Scholar] [CrossRef]
- Yeheskel, A.; Rawal, S. Exploring the ‘patient experience’ of individuals with limited English proficiency: A scoping review. J. Immigr. Minor. Health 2019, 21, 853–878. [Google Scholar] [CrossRef]
- Wolfe, M.K.; Noreen, C.M.; Holmes, M.G. Transportation barriers to health care in the United States: Findings from the National Health Interview Survey, 1997–2017. Am. J. Public Health 2020, 110, 815–822. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; the Northwell COVID-19 Research Consortium; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef]
- Kalligeros, M.; Shehadeh, F.; Mylona, E.K.; Benitez, G.; Beckwith, C.G.; Chan, P.A.; Mylonakis, E. Association of obesity with disease severity among patients with COVID-19. Obesity 2020, 28, 1200–1204. [Google Scholar] [CrossRef]
- Argenziano, M.G.; Bruce, S.L.; Slater, C.L.; Tiao, J.R.; Baldwin, M.R.; Barr, R.G.; Chang, B.P.; Chau, K.H.; Choi, J.J.; Gavin, N.; et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: Retrospective case series. BMJ 2020, 369, m1996. [Google Scholar] [CrossRef] [PubMed]
- Chow, N.; Fleming-Dutra, K.; Gierke, R.; Hall, A.; Hughes, M.; Pilishvili, T.; Ritchey, M.; Roguski, K.; Skoff, T.; Ussery, E. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–March 28, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 382–386. Available online: https://www.cdc.gov/mmwr/volumes/69/wr/mm6913e2.htm (accessed on 28 April 2021).
- Macias, G.R.; Marcelin, J.R.; Zuniga-Blanco, B.; Marquez, C.; Mathew, T.; Piggott, D.A. COVID-19 pandemic: Disparate health impact on the Hispanic/Latinx population in the United States. J. Infect. Dis. 2020, 222, 1592–1595. [Google Scholar] [CrossRef] [PubMed]
- Yancy, C.W. COVID-19 and African Americans. JAMA 2020, 323, 1891–1892. [Google Scholar] [CrossRef] [Green Version]
- Kanter, G.P.; Segal, A.G.; Groeneveld, P.W. Income disparities in access to critical care services: Study examines disparities in community intensive care unit beds by US communities’ median household income. Health Aff. 2020, 39, 1362–1367. [Google Scholar] [CrossRef]
- Fortuna, L.R.; Tolou-Shams, M.; Robles-Ramamurthy, B.; Porche, M.V. Inequity and the disproportionate impact of COVID-19 on communities of color in the United States: The need for a trauma-informed social justice response. Psychol. Trauma 2020, 12, 442–445. [Google Scholar] [CrossRef]
- Chen, D.T.; Wang, Y.J. Inequality-related health and social factors and their impact on well-being during the COVID-19 pandemic: Findings from a national survey in the UK. Int. J. Environ. Res. Public Health 2021, 18, 1014. [Google Scholar] [CrossRef]
- Weinstein, B.; da Silva, A.R.; Kouzoukas, D.E.; Bose, T.; Kim, G.J.; Correa, P.A.; Pondugula, S.; Lee, Y.; Kim, J.; Carpenter, D.O. Precision mapping of COVID-19 vulnerable locales by epidemiological and socioeconomic risk factors, developed using South Korean data. Int. J. Environ. Res. Public Health 2021, 18, 604. [Google Scholar] [CrossRef]
- Islam, N.; Lacey, B.; Shabnam, S.; Erzurumluoglu, A.M.; Dambha-Miller, H.; Chowell, G.; Kawachi, I.; Marmot, M. Social inequality and the syndemic of chronic disease and COVID-19: County-level analysis in the USA. J. Epidemiol. Community Health 2021. [Google Scholar] [CrossRef]
- Azar, K.M.; Shen, Z.; Romanelli, R.J.; Lockhart, S.H.; Smits, K.; Robinson, S.; Brown, S.; Pressman, A.R. Disparities in outcomes among COVID-19 patients in a large health care system in California: Study examines disparities in access and outcomes for COVID-19 patients who are members of racial and ethnic minorities and socioeconomically disadvantaged groups. Health Aff. 2020, 39. [Google Scholar] [CrossRef]
- Tai, D.B.G.; Shah, A.; Doubeni, C.A.; Sia, I.G.; Wieland, M.L. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin. Infect. Dis. 2020, 72, 703–706. [Google Scholar] [CrossRef]
- Davis, J.B. Stratification economics and identity economics. Camb. J. Econ. 2015, 39, 1215–1229. [Google Scholar] [CrossRef] [Green Version]
- Devine, D.; Gaskell, J.; Jennings, W.; Stoker, G. Trust and the Coronavirus pandemic: What are the consequences of and for trust? An early review of the literature. Political Stud. Rev. 2020. [Google Scholar] [CrossRef]
- Raine, L.; Perrin, A. The State of Americans’ Trust in Each Other Amid the COVID-19 Pandemic. Available online: https://www.pewresearch.org/fact-tank/2020/04/06/the-state-of-americans-trust-in-each-other-amid-the-covid-19-pandemic/ (accessed on 31 January 2021).
- Fontanet, A.; Cauchemez, S. COVID-19 herd immunity: Where are we? Nat. Rev. Immunol. 2020, 20, 583–584. [Google Scholar] [CrossRef]
- Kwok, K.O.; Lai, F.; Wei, W.I.; Wong, S.Y.S. Herd immunity–estimating the level required to halt the COVID-19 epidemics in affected countries. J. Infect. Dis. 2020, 80, e32–e33. [Google Scholar] [CrossRef]
- Patel, J.A.; Nielsen, F.B.H.; Badiani, A.A.; Assi, S. Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health 2020, 183, 110–111. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry/Geospatial Research, Analysis, and Services Program. Social Vulnerability Index 2018 Documentation. CDC 2018. Available online: https://svi.cdc.gov/Documents/Data/2018_SVI_Data/SVI2018Documentation-508.pdf (accessed on 28 April 2021).
- U.S. Census Bureau. ZIP Code Tabulation Areas (ZCTAs). 2020. Available online: https://www.census.gov/programs-surveys/geography/guidance/geo-areas/zctas.html (accessed on 28 April 2021).
- AskCHIS Neighborhood Edition. Available online: https://askchisne.ucla.edu/ask/_layouts/ne/dashboard.aspx (accessed on 30 September 2020).
- About the American Community Survey. United States Census Bureau. Available online: https://www.census.gov/programs-surveys/acs (accessed on 30 September 2020).
- Parks for California. Available online: https://www.parksforcalifornia.org/methods (accessed on 30 September 2020).
- Kavoor, A.R. COVID-19 in people with mental illness: Challenges and vulnerabilities. Asian J. Psychiatr. 2020, 51, 102051. [Google Scholar] [CrossRef]
- AskCHIS NE Indicator Definitions. Available online: http://healthpolicy.ucla.edu/Lists/AskCHIS%20NE%20Indicator%20Definitions/AllItems.aspx (accessed on 30 September 2020).
- Butler, M.J.; Barrientos, R.M. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav. Immun. 2020, 87, 53–54. [Google Scholar] [CrossRef]
- Botts, J. California Divide: How We Analyzed the Link between COVID-19 and Crowded Housing in California. CalMatters. 2020. Available online: https://calmatters.org/projects/california-coronavirus-overcrowded-housing-data-analysis/ (accessed on 30 September 2020).
- Rozenfeld, Y.; Beam, J.; Maier, H.; Haggerson, W.; Boudreau, K.; Carlson, J.; Medows, R. A model of disparities: Risk factors associated with COVID-19 infection. Int. J. Equity Health 2020, 19, 126. [Google Scholar] [CrossRef]
- Suarez-Lopez, J.R.; Cairns, M.R.; Sripada, K.; Quiro-Alcala, L.; Mielke, H.W.; Eskenazi, B.; Etzel, R.A.; Kordas, K.; on behalf of the International Society for Children’s Health and the Environment. COVID-19 and children’s health in the United States: Consideration of physical and social environments during the pandemic. Environ. Res. 2021, 11, 111160. [Google Scholar] [CrossRef]
- Scannell, C.A.; Oronce, C.I.A.; Tsugawa, Y. Association between county-level racial and ethnic characteristics and COVID-19 cases and deaths in the USA. J. Gen. Intern. Med. 2020, 35, 3126–3128. [Google Scholar] [CrossRef] [PubMed]
- Zalla, L.C.; Martin, C.L.; Edwards, J.K.; Gartner, D.R.; Noppert, G.A. A geography of risk: Structural racism and COVID-19 mortality in the United States. Am. J. Epidemiol. 2021, 12, kwab059. [Google Scholar] [CrossRef] [PubMed]
- Henry, A.T.; Jacobs, T.; Sabbs, D.; Holden, K.; Braithwaite, R.; Johnson, L.N.; Dawes, D.; Hoffman, L. Community engagement of African Americans in the era of COVID-19: Considerations, challenges, implications, and recommendations for public health. Prev. Chronic Dis. 2020, 17, E83. [Google Scholar] [CrossRef]
- Abuelgasim, E.; Saw, L.J.; Shirke, M.; Zeinah, M.; Harky, A. COVID-19: Unique public health issues facing Black, Asian and minority ethnic communities. Curr. Probl. Cardiol. 2020, 45, 100621. [Google Scholar] [CrossRef]
- Krieger, N.; Waterman, P.D.; Chen, J.T. COVID-19 and overall mortality inequities in the surge in death rates by zip code characteristics: Massachusetts, January 1 to May 19, 2020. Am. J. Public Health 2020, 110, 1850–1852. [Google Scholar] [CrossRef]
- Whittle, R.S.; Diaz-Artiles, A. An ecological study of socioeconomic predictors in detection of COVID-19 cases across neighborhoods in New York City. BMC Med. 2020, 18, 271. [Google Scholar] [CrossRef]
- Rosenbaum, S.; Handley, M.; Morris, R.; Casoni, M. How the Trump administration’s pandemic health care response failed racial health equity: Case studies of structural racism and a call for equity mindfulness in federal health policymaking. J. Health Polit. Policy Law 2021. [Google Scholar] [CrossRef]
- Maani, N.; Van Schalkwyk, M.C.; Petticrew, M.; Galea, S. The commercial determinants of three contemporary national crises: How corporate practices intersect with the COVID-19 pandemic, economic shutdown, and racial inequity. Milbank Q. 2021. [Google Scholar] [CrossRef]
- Ingraham, N.E.; Purcell, L.N.; Karam, B.S.; Dudley, R.A.; Usher, M.G.; Warlick, C.A.; Allen, M.L.; Melton, G.B.; Charles, A.; Tignanelli, C.J. Racial/ethnic disparities in hospital admissions from COVID-19 and determining the impact of neighborhood deprivation and primary language. MedRxiv 2020. [Google Scholar] [CrossRef]
- Millett, G.A.; Honermann, B.; Jones, A.; Lankiewicz, E.; Sherwood, J.; Blumenthal, S.; Sayas, A. White counties stand apart: The primacy of residential segregation in COVID-19 and HIV diagnoses. AID Patient Care STDS 2020. [Google Scholar] [CrossRef]
- Chin, T.; Kahn, R.; Li, R.; Chen, J.T.; Krieger, N.; Buckee, C.O.; Balsari, S.; Kiang, M.V. US-county level variation in intersecting individual, household and community characteristics relevant to COVID-19 and planning an equitable response: A cross-sectional analysis. BMJ Open 2020, 10, e039886. [Google Scholar] [CrossRef]
- Wang, M.L.; Behrman, P.; Dulin, A.; Baskin, M.L.; Buscemi, J.; Alcaraz, K.I.; Goldstein, C.M.; Carson, T.L.; Shen, M.; Fitzgibbon, M. Addressing inequities in COVID-19 morbidity and mortality: Research and policy recommendations. Transl. Behav. Med. 2020, 10, 516–519. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Shang, T.; Ahn, D.; Chen, K.; Coté, G.; Espinoza, J.; Mendez, C.E.; Spanakis, E.K.; Thompson, B.; Wallia, A.; et al. How to best protect people with diabetes from the impact of SARS-CoV-2: Report of the International COVID-19 and Diabetes Summit. J. Diabetes Sci. Technol. 2021, 15, 478–514. [Google Scholar] [CrossRef]









| Pre-Existing Health Vulnerability | |||||
|---|---|---|---|---|---|
| Lowest Vulnerable Quintile | Second Lowest Vulnerable Quintile | Middle Vulnerable Quintile | Second Highest Vulnerable Quintile | Highest Vulnerable Quintile | |
| Distribution by race | |||||
| % NH White | 60% | 42% | 31% | 19% | 7% |
| % Black | 5% | 6% | 5% | 6% | 19% |
| % Latinx | 15% | 25% | 41% | 61% | 68% |
| % Asian | 16% | 24% | 20% | 12% | 4% |
| % Speaks English “less than well” | 4% | 8% | 12% | 16% | 16% |
| Per capita income | $67.4 k | $40.6 k | $31.9 k | $23.9 k | $19.6 k |
| N (ZCTAs) | 51 | 52 | 52 | 53 | 52 |
| Social Vulnerability | |||||
|---|---|---|---|---|---|
| Lowest Vulnerable Quintile | Second Lowest Vulnerable Quintile | Middle Vulnerable Quintile | Second Highest Vulnerable Quintile | Highest Vulnerable Quintile | |
| Distribution by race | |||||
| % NH White | 60% | 48% | 31% | 21% | 8% |
| % Black | 4% | 5% | 7% | 11% | 13% |
| % Latinx | 15% | 26% | 40% | 52% | 70% |
| % Asian | 16% | 18% | 19% | 14% | 9% |
| % Speaks English “less than well” | 3% | 6% | 10% | 15% | 20% |
| Per capita income | $63.9 k | $49.0 | $33.3 k | $26.5 | $18.6 |
| N (ZCTAs) | 55 | 56 | 55 | 56 | 55 |
| Barriers to Access Vulnerability | |||||
|---|---|---|---|---|---|
| Lowest Vulnerable Quintile | Second Lowest Vulnerable Quintile | Middle Vulnerable Quintile | Second Highest Vulnerable Quintile | Highest Vulnerable Quintile | |
| Distribution by race | |||||
| % NH White | 62% | 47% | 29% | 20% | 10% |
| % Black | 5% | 7% | 9% | 9% | 9% |
| % Latinx | 17% | 24% | 41% | 52% | 70% |
| % Asian | 12% | 18% | 18% | 18% | 10% |
| % Speaks English “less than well” | 2% | 5% | 9% | 15% | 23% |
| Per capita income | $66.0 k | $48.4 k | $31.7 k | $26.3 k | $19.0 k |
| N (ZCTAs) | 55 | 56 | 55 | 56 | 55 |
| Built Environment Vulnerability | |||||
|---|---|---|---|---|---|
| Lowest Vulnerable Quintile | Second Lowest Vulnerable Quintile | Middle Vulnerable Quintile | Second Highest Vulnerable Quintile | Highest Vulnerable Quintile | |
| Distribution by race | |||||
| % NH White | 49% | 40% | 30% | 25% | 23% |
| % Black | 8% | 6% | 7% | 9% | 9% |
| % Latinx | 23% | 37% | 41% | 50% | 51% |
| % Asian | 16% | 14% | 19% | 13% | 14% |
| % Speaks English “less than well” | 4% | 7% | 11% | 14% | 18% |
| Per capita income | $51.4 k | $43.6 k | $36.3 k | $31.5 k | $28.5 k |
| N (ZCTAs) | 55 | 56 | 55 | 56 | 55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ong, P.M.; Pech, C.; Gutierrez, N.R.; Mays, V.M. COVID-19 Medical Vulnerability Indicators: A Predictive, Local Data Model for Equity in Public Health Decision Making. Int. J. Environ. Res. Public Health 2021, 18, 4829. https://doi.org/10.3390/ijerph18094829
Ong PM, Pech C, Gutierrez NR, Mays VM. COVID-19 Medical Vulnerability Indicators: A Predictive, Local Data Model for Equity in Public Health Decision Making. International Journal of Environmental Research and Public Health. 2021; 18(9):4829. https://doi.org/10.3390/ijerph18094829
Chicago/Turabian StyleOng, Paul M., Chhandara Pech, Nataly Rios Gutierrez, and Vickie M. Mays. 2021. "COVID-19 Medical Vulnerability Indicators: A Predictive, Local Data Model for Equity in Public Health Decision Making" International Journal of Environmental Research and Public Health 18, no. 9: 4829. https://doi.org/10.3390/ijerph18094829
APA StyleOng, P. M., Pech, C., Gutierrez, N. R., & Mays, V. M. (2021). COVID-19 Medical Vulnerability Indicators: A Predictive, Local Data Model for Equity in Public Health Decision Making. International Journal of Environmental Research and Public Health, 18(9), 4829. https://doi.org/10.3390/ijerph18094829







