Physical Activity and Perceived Physical Fitness during the COVID-19 Epidemic: A Population of 40- to 69-Year-Olds in Japan
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Assessment of PA
2.3. Assessment of Perceived Declining Physical Fitness
2.4. Demographic Variables
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carriedo, A.; Cecchini, J.A.; Fernandez-Rio, J.; Méndez-Giménez, A. COVID-19, Psychological Well-being and Physical Activity Levels in Older Adults during the Nationwide Lockdown in Spain. Am. J. Geriatr. Psychiatry 2020, 28, 1146–1155. [Google Scholar] [CrossRef]
- Al-Domi, H.; Al-Dalaeen, A.; Al-Rosan, S.; Batarseh, N.; Nawaiseh, H. Healthy nutritional behavior during COVID-19 lockdown: A cross-sectional study. Clin. Nutr. ESPEN 2021, 42, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, L.; Shaw, M.K.; Ko, J.; Deprez, D.; Chilibeck, P.D.; Zello, G.A. The impact of the coronavirus disease 2019 (COVID-19) pandemic on university students’ dietary intake, physical activity, and sedentary behaviour. Appl. Physiol. Nutr. Metab. 2021, 46, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Shaw, K.A.; Bertrand, L.; Deprez, D.; Ko, J.; Zello, G.A.; Chilibeck, P.D. The impact of the COVID-19 pandemic on diet, fitness, and sedentary behaviour of elite para-athletes. Disabil. Health J. 2021, 2021, 101091. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Henson, J.J.; Coull, N.A.; Edwardson, C.L.; Brady, E.; Hall, A.; Khunti, K.; Davies, M.; Yates, T. The impact of COVID-19 restrictions on accelerometer-assessed physical activity and sleep in individuals with type 2 diabetes. Diabet. Med. 2021, e14549. [Google Scholar] [CrossRef]
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef]
- Looi, M.-K. Covid-19: Japan prepares to extend state of emergency nationwide as “untraceable” cases soar. BMJ 2020, 369, m1543. [Google Scholar] [CrossRef]
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Effect of the COVID-19 Epidemic on Physical Activity in Community-Dwelling Older Adults in Japan: A Cross-Sectional Online Survey. J Nutr. Health Aging 2020, 24, 948–950. [Google Scholar] [CrossRef] [PubMed]
- Naseri, P.; Amiri, P.; Masihay-Akbar, H.; Jalali-Farahani, S.; Khalili, D.; Azizi, F. Long-term incidence of cardiovascular outcomes in the middle-aged and elderly with different patterns of physical activity: Tehran lipid and glucose study. BMC Public Health 2020, 20, 1654. [Google Scholar] [CrossRef]
- Lin, M.-S.; Yeh, M.-H.; Chen, M.-Y. Prevalence of and Factors Associated with Cardiometabolic Risks and Lung Function Impairment among Middle-Aged Women in Rural Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 8067. [Google Scholar] [CrossRef] [PubMed]
- Zotcheva, E.; Bergh, S.; Selbæk, G.; Krokstad, S.; Håberg, A.K.; Strand, B.H.; Ernstsen, L. Midlife Physical Activity, Psychological Distress, and Dementia Risk: The HUNT Study. J. Alzheimer’s Dis. 2018, 66, 825–833. [Google Scholar] [CrossRef]
- Payn, T.; Pfeiffer, K.A.; Hutto, B.; Vena, J.E.; LaMonte, M.J.; Blair, S.N.; Hooker, S.P. Daily Steps in Midlife and Older Adults: Relationship With Demographic, Self-Rated Health, and Self-Reported Physical Activity. Res. Q. Exerc. Sport 2008, 79, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.S.H.; Kean, Y.M.; Slymen, D.J.; Liu, W.T.; Zhang, M.; Katzman, R. Self-perceived Health and 5-Year Mortality Risks among the Elderly in Shanghai, China. Am. J. Epidemiol. 1998, 147, 880–890. [Google Scholar] [CrossRef] [PubMed]
- Bond, J.; Dickinson, H.O.; Matthews, F.; Jagger, C.; Brayne, C.; Cfas, M. Self-rated health status as a predictor of death, functional and cognitive impairment: a longitudinal cohort study. Eur. J. Ageing 2006, 3, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Montlahuc, C.; Soumare, A.; Dufouil, C.; Berr, C.; Dartigues, J.-F.; Poncet, M.; Tzourio, C.; Alperovitch, A. Self-rated health and risk of incident dementia: A community-based elderly cohort, the 3C Study. Neurology 2011, 77, 1457–1464. [Google Scholar] [CrossRef]
- Hargreaves, E.A.; Lee, C.; Jenkins, M.; Calverley, J.R.; Hodge, K.; Mackenzie, S.H. Changes in Physical Activity Pre-, During and Post-lockdown COVID-19 Restrictions in New Zealand and the Explanatory Role of Daily Hassles. Front. Psychol. 2021, 12, 642954. [Google Scholar] [CrossRef]
- Makizako, H.; Nakai, Y.; Shiratsuchi, D.; Akanuma, T.; Yokoyama, K.; Matsuzaki-Kihara, Y.; Yoshida, H. Perceived declining physical and cognitive fitness during the COVID-19 state of emergency among community-dwelling Japanese old-old adults. Geriatr. Gerontol. Int. 2021, 21, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Caputo, E.L.; Reichert, F.F. Studies of Physical Activity and COVID-19 during the Pandemic: A Scoping Review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). 2005. Available online: http://www.IPAQ.ki.se (accessed on 22 April 2021).
- Yamada, M.; Kimura, Y.; Ishiyama, D.; Otobe, Y.; Suzuki, M.; Koyama, S.; Kikuchi, T.; Kusumi, H.; Arai, H. Recovery of Physical Activity Among Older Japanese Adults Since the First Wave of the COVID-19 Pandemic. J. Nutr. Health Aging 2020, 24, 1036–1037. [Google Scholar] [CrossRef]
- Li, X.; Zhang, W.; Zhang, W.; Tao, K.; Ni, W.; Wang, K.; Li, Z.; Liu, Q.; Lin, J. Level of physical activity among middle-aged and older Chinese people: evidence from the China health and retirement longitudinal study. BMC Public Health 2020, 20, 1682. [Google Scholar] [CrossRef]
- Nichani, V.; Vena, J.E.; Friedenreich, C.M.; Christie, C.; McCormack, G.R. A population-based study of the associations between neighbourhood walkability and different types of physical activity in Canadian men and women. Prev. Med. 2019, 129, 105864. [Google Scholar] [CrossRef]
- Yu, L.; Liang, Q.; Zhou, W.; Huang, X.; Hu, L.; You, C.; Li, J.; Wu, Y.; Li, P.; Wu, Q.; et al. Association between physical activity and stroke in a middle-aged and elderly Chinese population. Medicine 2018, 97, e13568. [Google Scholar] [CrossRef]
- McDowell, C.; Dishman, R.; Hallgren, M.; MacDonncha, C.; Herring, M. Associations of physical activity and depression: Results from the Irish Longitudinal Study on Ageing. Exp. Gerontol. 2018, 112, 68–75. [Google Scholar] [CrossRef]
- Gross, A.L.; Lu, H.; Meoni, L.; Gallo, J.J.; Schrack, J.A.; Sharrett, A.R. Physical Activity in Midlife is not Associated with Cognitive Health in Later Life Among Cognitively Normal Older Adults. J. Alzheimer’s Dis. 2017, 59, 1349–1358. [Google Scholar] [CrossRef]
- Gjaka, M.; Feka, K.; Bianco, A.; Tishukaj, F.; Giustino, V.; Parroco, A.; Palma, A.; Battaglia, G. The Effect of COVID-19 Lockdown Measures on Physical Activity Levels and Sedentary Behaviour in a Relatively Young Population Living in Kosovo. J. Clin. Med. 2021, 10, 763. [Google Scholar] [CrossRef] [PubMed]
- An, H.-Y.; Chen, W.; Wang, C.-W.; Yang, H.-F.; Huang, W.-T.; Fan, S.-Y. The Relationships between Physical Activity and Life Satisfaction and Happiness among Young, Middle-Aged, and Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 4817. [Google Scholar] [CrossRef]
- Vogelsang, E.M.; Raymo, J.M.; Liang, J.; Kobayashi, E.; Fukaya, T. Population Aging and Health Trajectories at Older Ages. J. Gerontol. Ser. B 2017, 72, 1111–1112. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, A.B.S.; Siersma, V.; Kreiner, S.; Hiort, L.C.; Drivsholm, T.; Eplov, L.F.; Hollnagel, H. The impact of changes in self-rated general health on 28-year mortality among middle-aged Danes. Scand. J. Prim. Health Care 2009, 27, 160–166. [Google Scholar] [CrossRef][Green Version]
- Zaninotto, P.; Steptoe, A. Association Between Subjective Well-being and Living Longer Without Disability or Illness. JAMA Netw. Open 2019, 2, e196870. [Google Scholar] [CrossRef] [PubMed]
- Solomon, A.; Borodulin, K.; Ngandu, T.; Kivipelto, M.; Laatikainen, T.; Kulmala, J. Self-rated physical fitness and estimated maximal oxygen uptake in relation to all-cause and cause-specific mortality. Scand. J. Med. Sci. Sports 2017, 28, 532–540. [Google Scholar] [CrossRef] [PubMed]
- van der Linde, R.M.; Mavaddat, N.; Luben, R.; Brayne, C.; Simmons, R.K.; Khaw, K.T.; Kinmonth, A.L. Self-rated health and cardiovascular disease incidence: results from a longitudinal population-based cohort in Norfolk, UK. PLoS ONE. 2013, 8, e65290. [Google Scholar] [CrossRef] [PubMed]
- Wicker, P.; Frick, B. Intensity of physical activity and subjective well-being: an empirical analysis of the WHO recommendations. J. Public Health 2016, 39, e19–e26. [Google Scholar] [CrossRef] [PubMed]
- Sjogren, T.; Nissinen, K.J.; Järvenpää, S.K.; Ojanen, M.T.; Vanharanta, H.; Mälkiä, E.A. Effects of a physical exercise intervention on subjective physical well-being, psychosocial functioning and general well-being among office workers: A cluster randomized-controlled cross-over design. Scand. J. Med. Sci. Sports 2006, 16, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Niemelä, M.S.; Kangas, M.; Ahola, R.J.; Auvinen, J.P.; Leinonen, A.-M.; Tammelin, T.H.; Vaaramo, E.S.; Keinänen-Kiukaanniemi, S.M.; Korpelainen, R.I.; Jämsä, T.J. Dose-response relation of self-reported and accelerometer-measured physical activity to perceived health in middle age—The Northern Finland Birth Cohort 1966 Study. BMC Public Health 2019, 19, 21. [Google Scholar] [CrossRef]
- Breen, L.; Stokes, K.A.; Churchward-Venne, T.A.; Moore, D.R.; Baker, S.K.; Smith, K.; Atherton, P.J.; Phillips, S.M. Two Weeks of Reduced Activity Decreases Leg Lean Mass and Induces “Anabolic Resistance” of Myofibrillar Protein Synthesis in Healthy Elderly. J. Clin. Endocrinol. Metab. 2013, 98, 2604–2612. [Google Scholar] [CrossRef]
- Hagstromer, M.; Ainsworth, B.E.; Oja, P.; Sjostrom, M. Comparison of a Subjective and an Objective Measure of Physical Activity in a Population Sample. J. Phys. Act. Health 2010, 7, 541–550. [Google Scholar] [CrossRef]
| Overall (n = 1986) | 40–49 Years (n = 1046) | 50–59 Years (n = 712) | 60–69 Years (n = 228) | |
|---|---|---|---|---|
| Age, years | 50.1 ± 6.9 | 44.8 ± 2.8 | 55.7 ± 2.8 | 63.4 ± 2.9 |
| Women, n (%) | 773 (38.9%) | 453 (43.3%) | 256 (36.0%) | 64 (28.1%) |
| Education, n (%) | ||||
| Master/doctorate degree | 110 (5.5%) | 55 (5.3%) | 38 (5.3%) | 17 (7.5%) |
| Bachelor’s degree | 1011 (50.9%) | 535 (51.1%) | 345 (48.5%) | 131 (57.5%) |
| Professional degree | 311 (15.7%) | 180 (17.2%) | 105 (14.7%) | 26 (11.4%) |
| High school graduate | 465 (23.4%) | 232 (22.2%) | 185 (26.0%) | 48 (21.1%) |
| Others | 89 (4.5%) | 44 (4.2%) | 29 (4.1%) | 6 (2.6%) |
| Living alone, n (%) | 368 (18.5%) | 201 (19.2%) | 129 (18.1%) | 38 (16.7%) |
| Living area, n (%) | ||||
| Special precaution areas due to COVID-19 pandemic | 1415 (71.2%) | 731 (69.9%) | 532 (74.7%) | 152 (66.7%) |
| Perceived declining physical fitness (yes), n (%) | 671 (33.8%) | 364 (34.8%) | 227 (31.9%) | 80 (35.1%) |
| PA time, minutes | ||||
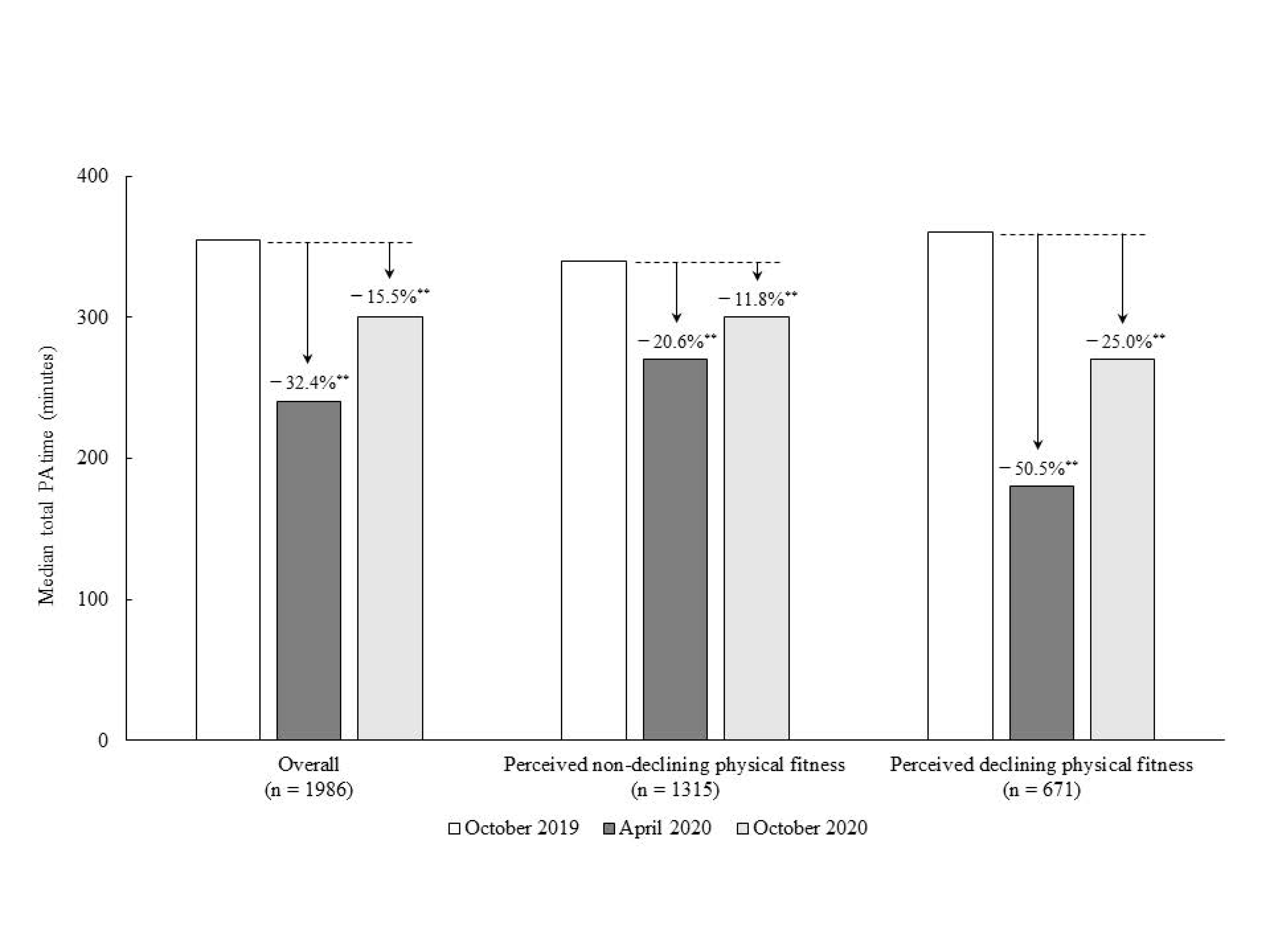
| October-2019, median (IQR) | 355 (150–660) | 343 (150–700) | 335 (150–630) | 360 (161–685) |
| April-2020, median (IQR) | 240 (80–540) | 240 (60–560) | 233 (80–490) | 300 (120–600) |
| October-2020, median (IQR) | 300 (120–600) | 300 (100–600) | 298 (120–600) | 300 (120–630) |
| No Perceived Decline in Physical Fitness (n = 1315) | Perceived Decline in Physical Fitness (n = 671) | p | |
|---|---|---|---|
| Age, years | 50.2 ± 6.9 | 50.0 ± 6.9 | 0.57 |
| Women, n (%) | 469 (35.7%) | 304 (45.3%) | <0.01 |
| Education (Bachelor/master/doctorate degree), n (%) | 587 (44.6%) | 278 (41.4%) | 0.17 |
| Living alone, n (%) | 237 (18.0%) | 131 (19.5%) | 0.42 |
| Living area, n (%) | |||
| Special precaution areas due to COVID-19 pandemic | 913 (69.4%) | 502 (74.8%) | 0.01 |
| PA time, minutes | |||
| October 2019, median (IQR) | 340 (140–660) | 360 (150–700) | 0.43 |
| April 2020, median (IQR) | 270 (100–600) | 180 (60–480) | <0.01 |
| October 2020, median (IQR) | 300 (120–620) | 270 (90–580) | 0.48 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makizako, H.; Akaida, S.; Shono, S.; Shiiba, R.; Taniguchi, Y.; Shiratsuchi, D.; Nakai, Y. Physical Activity and Perceived Physical Fitness during the COVID-19 Epidemic: A Population of 40- to 69-Year-Olds in Japan. Int. J. Environ. Res. Public Health 2021, 18, 4832. https://doi.org/10.3390/ijerph18094832
Makizako H, Akaida S, Shono S, Shiiba R, Taniguchi Y, Shiratsuchi D, Nakai Y. Physical Activity and Perceived Physical Fitness during the COVID-19 Epidemic: A Population of 40- to 69-Year-Olds in Japan. International Journal of Environmental Research and Public Health. 2021; 18(9):4832. https://doi.org/10.3390/ijerph18094832
Chicago/Turabian StyleMakizako, Hyuma, Shoma Akaida, Saki Shono, Ryuhei Shiiba, Yoshiaki Taniguchi, Daijo Shiratsuchi, and Yuki Nakai. 2021. "Physical Activity and Perceived Physical Fitness during the COVID-19 Epidemic: A Population of 40- to 69-Year-Olds in Japan" International Journal of Environmental Research and Public Health 18, no. 9: 4832. https://doi.org/10.3390/ijerph18094832
APA StyleMakizako, H., Akaida, S., Shono, S., Shiiba, R., Taniguchi, Y., Shiratsuchi, D., & Nakai, Y. (2021). Physical Activity and Perceived Physical Fitness during the COVID-19 Epidemic: A Population of 40- to 69-Year-Olds in Japan. International Journal of Environmental Research and Public Health, 18(9), 4832. https://doi.org/10.3390/ijerph18094832







