Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Definition of Stroke
2.3. Indices for Abdominal Obesity
2.4. Covariates
2.5. Statistics
3. Results
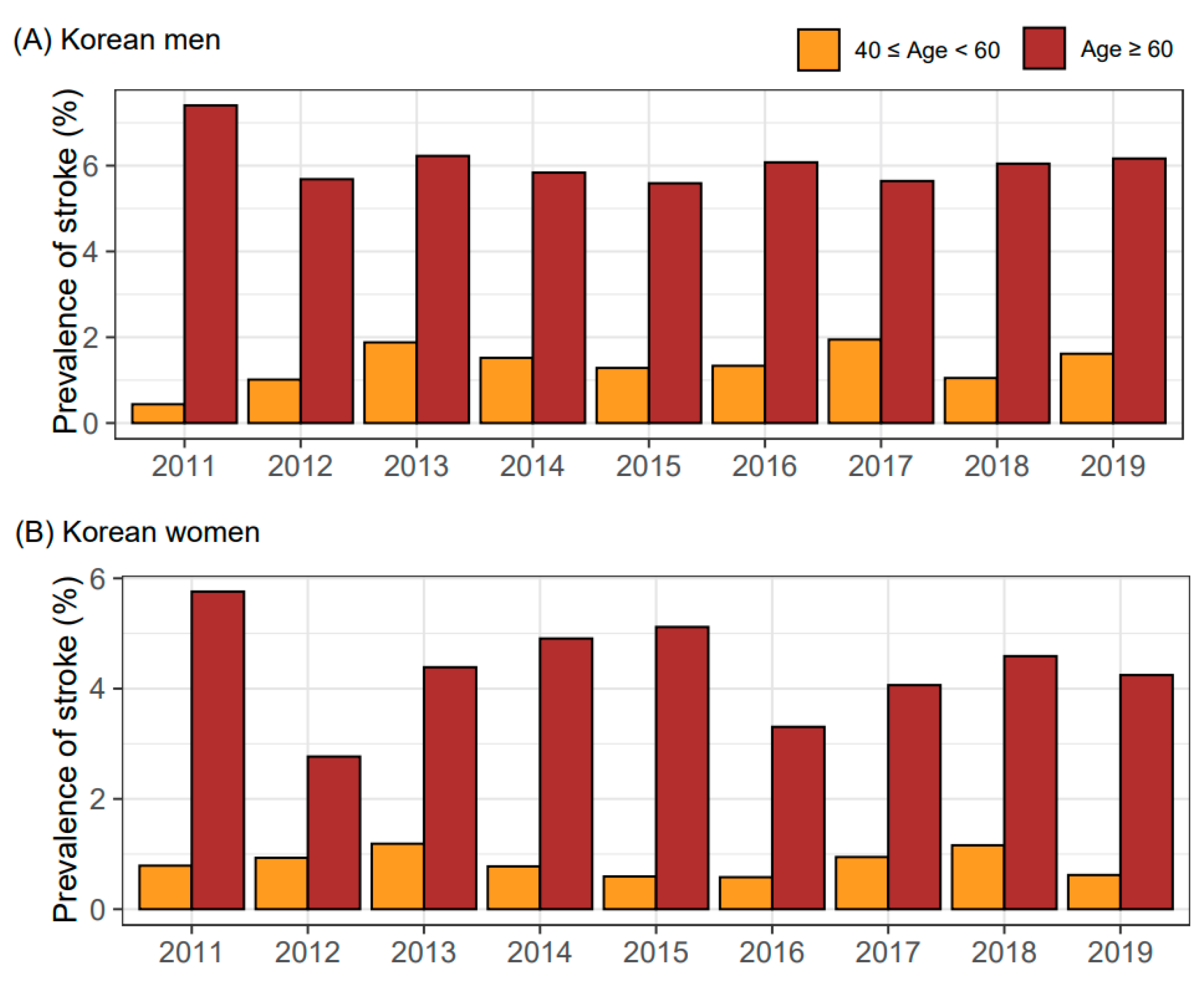
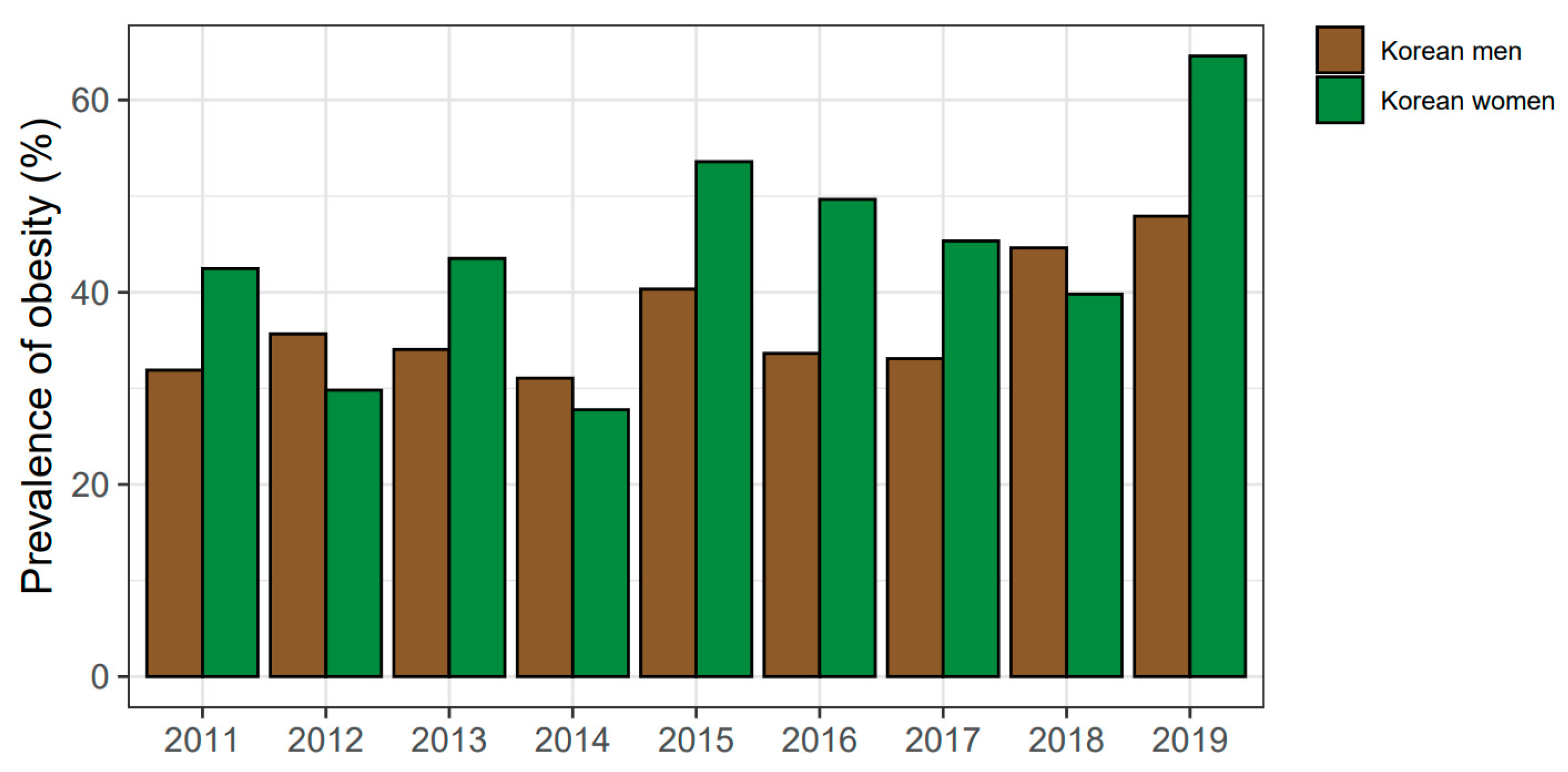
3.1. General Characteristics
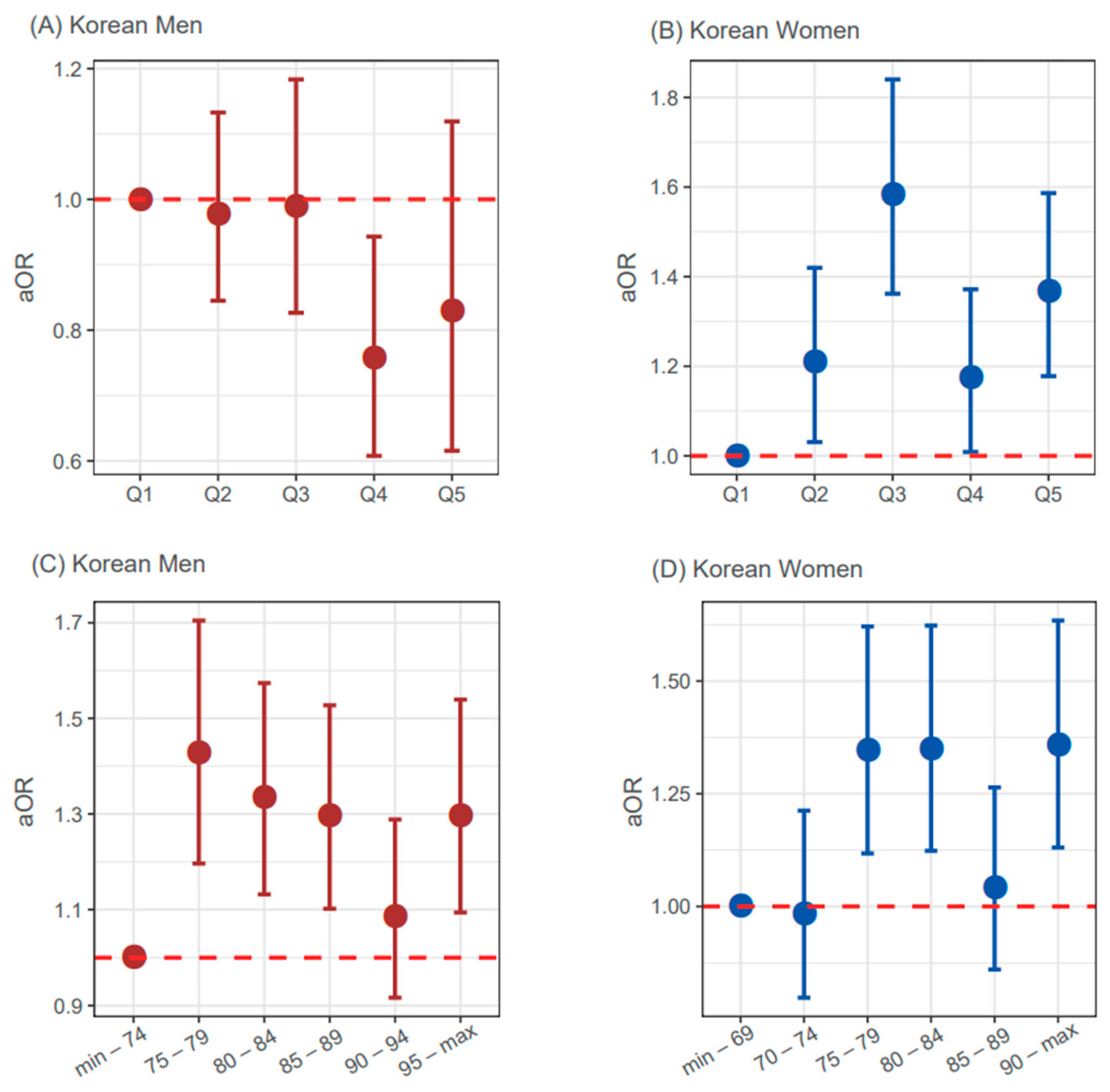
3.2. Relationship of the Continuous and Binary form of WC with the Risk of Stroke
3.3. Relationship of the Five Groups of WC with the Risk of Stroke
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roger, V.L.; Go, A.S.; Lloyd-Jones, D.M.; Adams, R.J.; Berry, J.D.; Brown, T.M.; Carnethon, M.R.; Dai, S.; De Simone, G.; Ford, E.S. Heart disease and stroke statistics—2011 update: A report from the American Heart Association. Circulation 2011, 123, e18–e209. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J. Heart disease and stroke statistics—2016 update: A report from the American Heart Association. Circulation 2015, 123, e18–e209. [Google Scholar] [CrossRef] [PubMed]
- Ovbiagele, B.; Goldstein, L.B.; Higashida, R.T.; Howard, V.J.; Johnston, S.C.; Khavjou, O.A.; Lackland, D.T.; Lichtman, J.H.; Mohl, S.; Sacco, R.L. Forecasting the future of stroke in the United States: A policy statement from the American Heart Association and American Stroke Association. Stroke 2013, 44, 2361–2375. [Google Scholar] [CrossRef] [PubMed]
- Pearson, T.A.; Palaniappan, L.P.; Artinian, N.T.; Carnethon, M.R.; Criqui, M.H.; Daniels, S.R.; Fonarow, G.C.; Fortmann, S.P.; Franklin, B.A.; Galloway, J.M. American Heart Association Guide for Improving Cardiovascular Health at the Community Level, 2013 update: A scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation 2013, 127, 1730–1753. [Google Scholar] [CrossRef] [PubMed]
- Hong, K.-S.; Bang, O.Y.; Kang, D.-W.; Yu, K.-H.; Bae, H.-J.; Lee, J.S.; Heo, J.H.; Kwon, S.U.; Oh, C.W.; Lee, B.-C. Stroke statistics in Korea: Part I. Epidemiology and risk factors: A report from the korean stroke society and clinical research center for stroke. J. Stroke 2013, 15, 2. [Google Scholar] [CrossRef]
- Lim, S.-J.; Kim, H.-J.; Nam, C.-M.; Chang, H.-S.; Jang, Y.-H.; Kim, S.; Kang, H.-Y. Socioeconomic costs of stroke in Korea: Estimated from the Korea national health insurance claims database. J. Prev. Med. Public Health 2009, 42, 251–260. [Google Scholar] [CrossRef]
- Mitchell, A.B.; Cole, J.W.; McArdle, P.F.; Cheng, Y.-C.; Ryan, K.A.; Sparks, M.J.; Mitchell, B.D.; Kittner, S.J. Obesity increases risk of ischemic stroke in young adults. Stroke 2015, 46, 1690–1692. [Google Scholar] [CrossRef]
- Rexrode, K.M.; Hennekens, C.H.; Willett, W.C.; Colditz, G.A.; Stampfer, M.J.; Rich-Edwards, J.W.; Speizer, F.E.; Manson, J.E. A prospective study of body mass index, weight change, and risk of stroke in women. Jama 1997, 277, 1539–1545. [Google Scholar] [CrossRef]
- Ni Mhurchu, C.; Rodgers, A.; Pan, W.H.; Gu, D.F.; Woodward, M. Body mass index and cardiovascular disease in the Asia-Pacific Region: An overview of 33 cohorts involving 310 000 participants. Int. J. Epidemiol. 2004, 33, 751–758. [Google Scholar] [CrossRef]
- Kurth, T.; Gaziano, J.M.; Berger, K.; Kase, C.S.; Rexrode, K.M.; Cook, N.R.; Buring, J.E.; Manson, J.E. Body Mass Index and the Risk of Stroke in Men. Arch. Intern. Med. 2002, 162, 2557–2562. [Google Scholar] [CrossRef]
- Suk, S.H.; Sacco, R.L.; Boden-Albala, B.; Cheun, J.F.; Pittman, J.G.; Elkind, M.S.; Paik, M.C. Abdominal obesity and risk of ischemic stroke: The Northern Manhattan Stroke Study. Stroke 2003, 34, 1586–1592. [Google Scholar] [CrossRef] [PubMed]
- Strazzullo, P.; D’Elia, L.; Cairella, G.; Garbagnati, F.; Cappuccio, F.P.; Scalfi, L. Excess body weight and incidence of stroke: Meta-analysis of prospective studies with 2 million participants. Stroke 2010, 41, e418–e426. [Google Scholar] [CrossRef] [PubMed]
- Kernan, W.N.; Inzucchi, S.E.; Sawan, C.; Macko, R.F.; Furie, K.L. Obesity: A stubbornly obvious target for stroke prevention. Stroke 2013, 44, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Winter, Y.; Rohrmann, S.; Linseisen, J.; Lanczik, O.; Ringleb, P.A.; Hebebrand, J.; Back, T. Contribution of obesity and abdominal fat mass to risk of stroke and transient ischemic attacks. Stroke 2008, 39, 3145–3151. [Google Scholar] [CrossRef] [PubMed]
- Winter, Y.; Pieper, L.; Klotsche, J.; Riedel, O.; Wittchen, H.U. Obesity and Abdominal Fat Markers in Patients with a History of Stroke and Transient Ischemic Attacks. J Stroke Cerebrovasc. Dis. 2016, 25, 1141–1147. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Rhee, E.J.; Park, S.E.; Kwon, H.; Jung, J.H.; Han, K.D.; Park, Y.G.; Park, H.S.; Kim, Y.H.; Yoo, S.J.; et al. The Risk of Myocardial Infarction and Ischemic Stroke According to Waist Circumference in 21,749,261 Korean Adults: A Nationwide Population-Based Study. Diabetes Metab. J. 2019, 43, 206–221. [Google Scholar] [CrossRef] [PubMed]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y. The Korea National Health and Nutrition Examination Survey (KNHANES): Current status and challenges. Epidemiol. Health 2014, 36, e2014002. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kang, K.; Kang, J.; Koo, J.; Kim, D.H.; Kim, B.J.; Kim, W.J.; Kim, E.G.; Kim, J.G.; Kim, J.M.; et al. Executive Summary of Stroke Statistics in Korea 2018: A Report from the Epidemiology Research Council of the Korean Stroke Society. J. Stroke 2019, 21, 42–59. [Google Scholar] [CrossRef]
- Seo, M.H.; Lee, W.Y.; Kim, S.S.; Kang, J.H.; Kang, J.H.; Kim, K.K.; Kim, B.Y.; Kim, Y.H.; Kim, W.J.; Kim, E.M.; et al. 2018 Korean Society for the Study of Obesity Guideline for the Management of Obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 40–45. [Google Scholar] [CrossRef]
- Kim, B.-Y.; Kang, S.M.; Kang, J.-H.; Kang, S.Y.; Kim, K.K.; Kim, K.-B.; Kim, B.; Kim, S.J.; Kim, Y.-H.; Kim, J.-H.; et al. 2020 Korean Society for the Study of Obesity Guidelines for the Management of Obesity in Korea. JOMES 2021, 30, 81–92. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Goff, D.C., Jr.; Lloyd-Jones, D.M.; Bennett, G.; Coady, S.; D’Agostino, R.B.; Gibbons, R.; Greenland, P.; Lackland, D.T.; Levy, D.; O’Donnell, C.J.; et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S49–S73. [Google Scholar] [CrossRef] [PubMed]
- Yadlowsky, S.; Hayward, R.A.; Sussman, J.B.; McClelland, R.L.; Min, Y.I.; Basu, S. Clinical Implications of Revised Pooled Cohort Equations for Estimating Atherosclerotic Cardiovascular Disease Risk. Ann. Intern. Med. 2018, 169, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Association, A.D. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014, 37, S81–S90. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2013. [Google Scholar]
- Park, H.; Park, C.; Oh, S.; Yoo, H. Prevalence of obesity and metabolic syndrome in Korean adults. Obes. Rev. 2008, 9, 104–107. [Google Scholar] [CrossRef]
- Lee, S.Y.; Park, H.S.; Kim, D.J.; Han, J.H.; Kim, S.M.; Cho, G.J.; Kim, D.Y.; Kwon, H.S.; Kim, S.R.; Lee, C.B. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res. Clin. Pract. 2007, 75, 72–80. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. The metabolic syndrome--a new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Balkau, B.; Charles, M.A. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet. Med. 1999, 16, 442–443. [Google Scholar] [CrossRef]
- Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). Jama 2001, 285, 2486–2497. [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abedi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Bembenek, J.P.; Karlinski, M.; Niewada, M.; Kurkowska-Jastrzębska, I.; Członkowska, A. Measurement of Nutritional Status Using Body Mass Index, Waist-to-Hip Ratio, and Waist Circumference to Predict Treatment Outcome in Females and Males with Acute First-Ever Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2018, 27, 132–139. [Google Scholar] [CrossRef]
- Zhang, P.; Sun, X.; Jin, H.; Zhang, F.L.; Guo, Z.N.; Yang, Y. Comparison of the Four Anthropometric Indexes and Their Association With Stroke: A Population-Based Cross-Sectional Study in Jilin Province, China. Front. Neurol. 2019, 10, 1304. [Google Scholar] [CrossRef]
- Cong, X.; Liu, S.; Wang, W.; Ma, J.; Li, J. Combined consideration of body mass index and waist circumference identifies obesity patterns associated with risk of stroke in a Chinese prospective cohort study. BMC Public Health 2022, 22, 347. [Google Scholar] [CrossRef]
- Quiñones-Ossa, G.A.; Lobo, C.; Garcia-Ballestas, E.; Florez, W.A.; Moscote-Salazar, L.R.; Agrawal, A. Obesity and Stroke: Does the Paradox Apply for Stroke? Neurointervention 2021, 16, 9–19. [Google Scholar] [CrossRef]
- Lee, T.; Lee, H.; The Alzheimer’s Disease Neuroimaging, I. Identification of Disease-Related Genes That Are Common between Alzheimer’s and Cardiovascular Disease Using Blood Genome-Wide Transcriptome Analysis. Biomedicines 2021, 9, 1525. [Google Scholar] [CrossRef]
- Stanek, A.; Fazeli, B.; Bartuś, S.; Sutkowska, E. The Role of Endothelium in Physiological and Pathological States: New Data. BioMed Res. Int. 2018, 2018, 1098039. [Google Scholar] [CrossRef]
- Rigotti, N.A.; Clair, C. Managing tobacco use: The neglected cardiovascular disease risk factor. Eur. Heart J. 2013, 34, 3259–3267. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Jang, H.; Kim, J.; Min, S. Development of a suicide index model in general adolescents using the South Korea 2012–2016 national representative survey data. Sci. Rep. 2019, 9, 1846. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-O.; Bae, E.M.; Lee, Y.-N.; Son, J.S. Association between Consumption of Sugar-Sweetened Beverages and Risk of Cardiovascular Disease in Korean Men: Analysis Based on the Korea National Health and Nutrition Examination Survey 2014-2016. Korean J. Fam. Med. 2021, 42, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.J.; Kim, H.S.; Jung, D.H.; Kim, J.K. Cluster analysis of nutritional factors associated with low muscle mass index in middle-aged and older adults. Clin. Nutr. 2020, 39, 3369–3376. [Google Scholar] [CrossRef]
- Park, M.B.; Kim, C.B.; Nam, E.W.; Hong, K.S. Does South Korea have hidden female smokers: Discrepancies in smoking rates between self-reports and urinary cotinine level. BMC Womens Health 2014, 14, 156. [Google Scholar] [CrossRef]
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef]
- Hu, G.; Tuomilehto, J.; Silventoinen, K.; Sarti, C.; Männistö, S.; Jousilahti, P. Body mass index, waist circumference, and waist-hip ratio on the risk of total and type-specific stroke. Arch. Intern. Med. 2007, 167, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-J.; Choi, E.Y.; Park, E.W.; Cheong, Y.S.; Lee, H.-Y.; Kim, J.H. The Utility of HbA1c as a Diagnostic Criterion of Diabetes. Korean J. Fam. Med. 2011, 32, 383–389. [Google Scholar] [CrossRef]
- Yoo, B.; Nam, H.; Hwang, I.C.; Park, Y. Correlation of Cardiovascular Risk Factors with Central Obesity and Multiple Body Mass Index in Korea. Korean J. Fam. Med. 2017, 38, 338–345. [Google Scholar] [CrossRef][Green Version]
| Korean Men | Korean Women | |||||
|---|---|---|---|---|---|---|
| Variable | Non-Stroke | Stroke | p-Value | Non-Stroke | Stroke | p-Value |
| Unweighted subjects, n | 12,622 | 507 | 17,905 | 456 | ||
| Age, years | 59.4 ± 0.1 | 67.6 ± 0.41 | <0.001 | 58.8 ± 0.09 | 68.4 ± 0.46 | <0.001 |
| WC, cm | 86.3 ± 0.08 | 87.7 ± 0.37 | <0.001 | 80.9 ± 0.07 | 85 ± 0.47 | <0.001 |
| <75 (women: 70) | 1171 (9.3) | 31 (6.1) | 0.001 | 2028 (11.3) | 26 (5.7) | <0.001 |
| 75 (70)–84 (79) | 4232 (33.5) | 159 (31.4) | 6540 (36.5) | 116 (25.4) | ||
| 85 (80)–94 (89) | 5384 (42.7) | 214 (42.2) | 6408 (35.8) | 178 (39) | ||
| ≥95 (90) | 1835 (14.5) | 103 (20.3) | 2929 (16.4) | 136 (29.8) | ||
| Abd obesity, n | 4137 (32.8) | 195 (38.5) | <0.001 | 5699 (31.8) | 213 (46.7) | <0.001 |
| Systolic BP, mmHg | 123.2 ± 0.14 | 126.8 ± 0.8 | <0.001 | 121.4 ± 0.13 | 130 ± 0.88 | <0.001 |
| <130 | 8634 (68.4) | 301 (59.4) | <0.001 | 12,497 (69.8) | 235 (51.5) | <0.001 |
| 130–139 | 2141 (17) | 104 (20.5) | 2580 (14.4) | 92 (20.2) | ||
| 140–149 | 1100 (8.7) | 58 (11.4) | 1575 (8.8) | 76 (16.7) | ||
| ≥150 | 747 (5.9) | 44 (8.7) | 1253 (7) | 53 (11.6) | ||
| Current smoking, n | 4050 (32.1) | 124 (24.5) | <0.001 | 676 (3.8) | 19 (4.2) | 0.758 |
| Antihypertensive medication, n | 3727 (29.5) | 330 (65.1) | <0.001 | 5109 (28.5) | 313 (68.6) | <0.001 |
| Diabetes, n | 2406 (19.1) | 187 (36.9) | <0.001 | 2403 (13.4) | 149 (32.7) | <0.001 |
| TC, mg/dL | 189 ± 0.33 | 166.4 ± 1.72 | <0.001 | 197.2 ± 0.28 | 181.2 ± 1.76 | <0.001 |
| HDL-C, mg/dL | 46.9 ± 0.1 | 44.4 ± 0.51 | <0.001 | 52.7 ± 0.09 | 48.5 ± 0.54 | <0.001 |
| Men, WC (Continuous Variable, cm) | Women, WC (Continuous Variable, cm) | ||||
|---|---|---|---|---|---|
| Model | ORs (95% CI) | p | Model | ORs (95% CI) | p |
| Univariate model | 1.015 (1.011–1.02) | <0.001 | Univariate model | 1.044 (1.041–1.048) | <0.001 |
| Model 1 | 1.015 (1.011–1.019) | <0.001 | Model 1 | 1.024 (1.02–1.028) | <0.001 |
| Model 2 | 0.994 (0.99–0.998) | 0.004 | Model 2 | 1.009 (1.005–1.013) | <0.001 |
| Model 3 | 0.996 (0.992–1.001) | 0.089 | Model 3 | 1.009 (1.005–1.014) | <0.001 |
| Men, Abdominal Obesity (WC ≥ 90) | Women, Abdominal Obesity (WC ≥ 85) | ||||
| Model | ORs (95% CI) | p | Model | ORs (95% CI) | p |
| Univariate model | 1.238 (1.153–1.33) | <0.001 | Univariate model | 1.892 (1.788–2.002) | <0.001 |
| Model 1 | 1.187 (1.104–1.276) | <0.001 | Model 1 | 1.242 (1.172–1.317) | <0.001 |
| Model 2 | 0.886 (0.822–0.955) | 0.002 | Model 2 | 0.968 (0.912–1.028) | 0.288 |
| Model 3 | 0.912 (0.846–0.985) | 0.018 | Model 3 | 0.968 (0.911–1.028) | 0.290 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.Y.; Cho, S.M.; Yoo, Y.; Lee, T.; Kim, J.K. Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019. Int. J. Environ. Res. Public Health 2022, 19, 6140. https://doi.org/10.3390/ijerph19106140
Kim JY, Cho SM, Yoo Y, Lee T, Kim JK. Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019. International Journal of Environmental Research and Public Health. 2022; 19(10):6140. https://doi.org/10.3390/ijerph19106140
Chicago/Turabian StyleKim, Jong Yeon, Sung Min Cho, Youngmin Yoo, Taesic Lee, and Jong Koo Kim. 2022. "Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019" International Journal of Environmental Research and Public Health 19, no. 10: 6140. https://doi.org/10.3390/ijerph19106140
APA StyleKim, J. Y., Cho, S. M., Yoo, Y., Lee, T., & Kim, J. K. (2022). Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019. International Journal of Environmental Research and Public Health, 19(10), 6140. https://doi.org/10.3390/ijerph19106140






