Experiences, Emotions, and Health Consequences among COVID-19 Survivors after Intensive Care Unit Hospitalization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Procedure
2.3. Instruments
2.4. Data Collection
2.5. Ethics
2.6. Data Analysis
3. Results
3.1. Demographic Characteristics
3.2. Themes Emerged from the Interviews
3.2.1. Theme 1: Emotion of Fear
Sub-Theme 1: Fear for One’s Own Life
ID7: “the greatest fear was when I got into the ambulance and I thought to my daughter who greeted me from the window saying “Hi dad, I love you”. It was the worst moment, the fear for not coming back home”.
ID9: “the fear for dying, and the fear for not being able to come back my house even for one day… I remember this fear as a daily fear”.
ID6: “the first day [of hospitalization] I thought I was going to die. I remembered my whole life and I thought «ok that’s what happened, I am 57 years old and I have already done many things in my life”.
ID15: “fear for failing, I also saw two people die next to me, so the fear of ending up the same was strong”.
ID11: “let’s face it, I saw as a coffin and someone waiting for me”.
ID14: “I remember the fear given by the breathing difficulty, fear and panic… and in the end, they [doctors] intubated me (…). After waking up it seemed that the worst was over, but for me, it was not really like this, I always continued to have anxiety and fear to die”.
ID4: “I was very scared, I immediately asked which possibilities I had [with endotracheal intubation]. I was really very afraid, and the greatest fear was to not being able to come back home to my loved ones, afraid to die and not waking up”.
ID15: “the head physician informed me that I needed to be intubated. I would say that I felt terror, I didn’t know what I was getting into (…)”.
Sub-Theme 2: Fear about Getting Sick Again and about the Risk of Contagion of Loved Ones
ID4: “one of the biggest fears that never left me was the fear of having transmitted the infection to someone at home”.
ID 11 “(…) Now that the numbers [of infections] are always growing I do not deny that it makes me worry, especially for my grandchildren and the people around me … and this fear I’m only having right now”.
ID8: “(…) to date I am also afraid to infect me again, just afraid of taking it back and reliving everything I have already been through”.
ID13 “(…) When you see such things the fear is still there, since I was discharged I have never had a great social life (…)”.
3.2.2. Theme 2: Isolation and Loneliness
ID3: (…) well, what could I say … that I was alone, that yes, I suffered loneliness”.
ID7: “I feared loneliness a lot and when a person is alone s/he knows s/he can’t do much, at that moment I raised my hands and said to myself «I know it’s done»”.
ID11: “loneliness seemed an insurmountable thing, thinking about it today I don’t know how I could do it (…). The loneliness was always there, but luckily it was dampened by those wonderful characters [the health care workers] who surrounded me”.
ID6: “There were a few moments where I felt anxious. For example, the lack of contact with people, we were many [hospitalized patients] but perhaps the isolation [from loved ones] made us feel even more alone”.
ID12: “Another thing that I experienced really badly was that we were alone because there were single rooms, it happened that there was not always someone inside, I always asked the nurses what time it was and when it was evening I couldn’t wait to asking for something to sleep, so I could spend some time without thinking I was alone”.
ID13: “I was afraid of being alone, of loneliness… just the fear for not being accompanied, for dying and not having anyone close to, none of the loved one I shared my life with”.
ID4: “(…) the greatest stress was loneliness, being alone when there were no nurses. It was very stressful to me being alone… we had no one close to”.
ID11: “I was alone, I had no company. I had no one, loneliness was the real stress. I wished someone who could stay with me longer, but I understood that it was not possible, I suffered from not having someone to chat with, I missed people, the contact, chatting…”.
ID12: “I remember as if it were yesterday, a day when I burst into tears [with a doctor] (…), but I immediately I said «doctor, it’s not the cure that making me a nervous wreck, because I feel that it [the cure] is going well, but I react like this because I am alone, the fact of not having company makes me very sad”.
3.2.3. Theme 3: Unawareness about the Gravity of the Situation as a Protective Factor
ID5: “(…) I couldn’t quantify how long I was wide-awake after the coma, perhaps this lack of perception, somehow, saved me”.
ID13: “(…) I don’t remember much of those days in ICU, maybe on the one hand it went better this way… I didn’t realize the gravity of the situation… I would have died of fear (…). On the other hand, I thank a bit the drugs and my freaking out that kept my thoughts away from reality.
ID11: “It seems like as I didn’t have an inkling of what happened to me. I had an inkling that something wasn’t right, but it was as if I had my ears plugged towards what was happening”.
ID1: “I didn’t know what was going on (…), I didn’t think I was going to die (…), I was never afraid of dying”.
ID7: “(…) there were some days, like those after the coma, where I had no conscience, and maybe that helped me to don’t let me go to bad emotions and feelings”.
ID6: “Everything was so fast and maybe I didn’t become aware of the gravity of what was happening to me. I don’t think I was afraid at that moment [before endotracheal intubation]”.
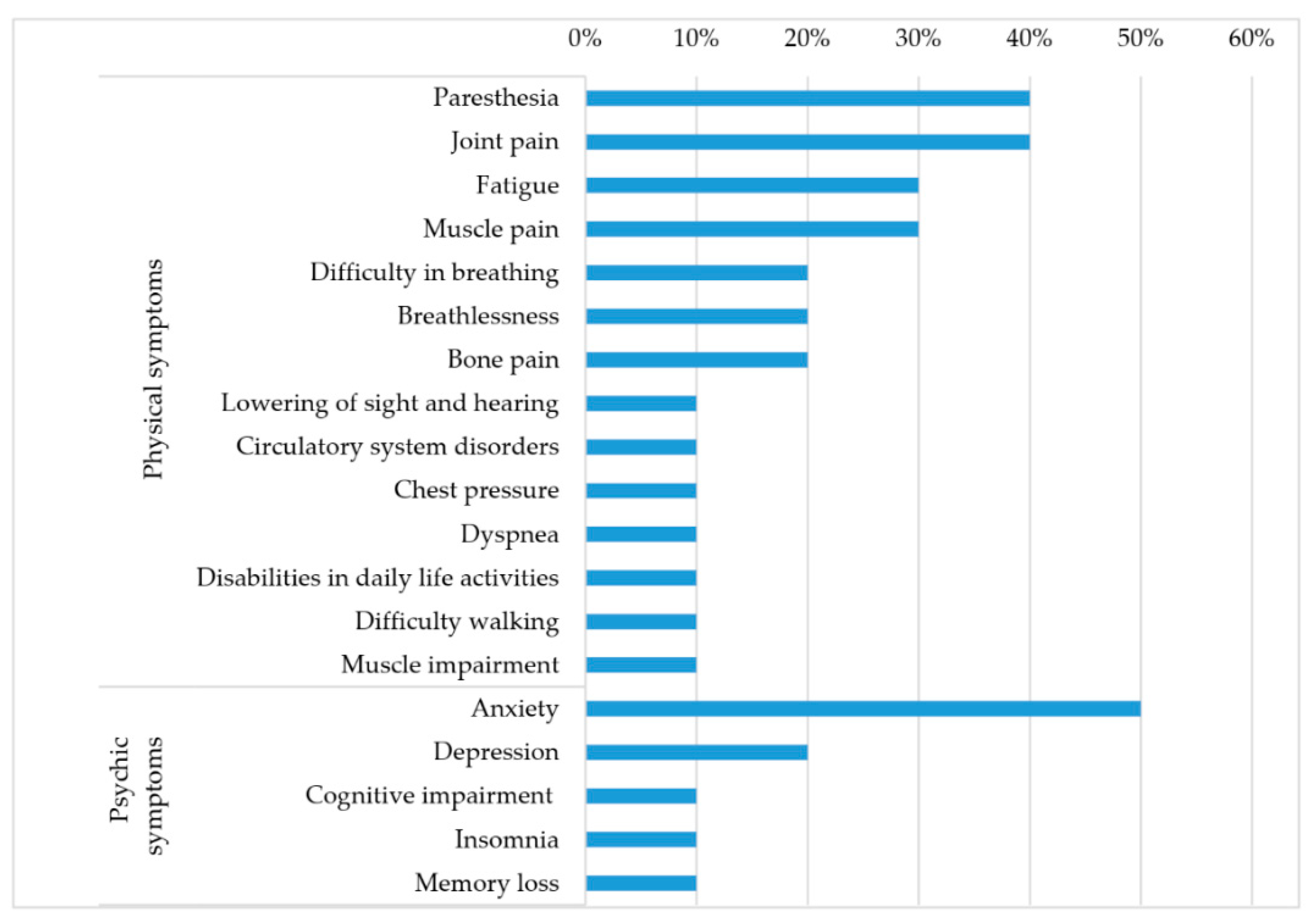
3.2.4. Theme 4: “Long COVID”: Consequences of the Disease on Health
ID5: “today I am certainly fine compared to before, but I have problems with my ankles, toes, fingers, and mainly at the bone level (…)”.
ID9: “COVID has left me with pathologies, mainly to my bones and muscles (…)”.
ID11: “(…) I can’t close my hands (…). I can no longer handle the big toe of my right foot; I cannot drive for a year. I have mobility problems, I’ve ruined my hips, when someone sees me walking s/he understands, it’s really hard walking for me”.
ID7: “I’m fine now, but COVID has left me with respiratory problems, dyspnea and I feel pressure on my chest (…)”
ID5: “fatigue is always latent and I’m realizing that I no longer have the strength of before (…), I struggle to sing, I’ve never recovered my diaphragmatic breathing”.
ID15: “(…) if I go up the stairs I am a bit out of breath, or maybe when I have to manage bad days, when I feel profound tiredness”.
ID6: “I have a deficit in the external popliteal sciatic nerve to both feet, a nerve injury and the left thigh still looks like it is under anesthesia”.
ID9: “(…) a circulation problem has arisen in the lower limbs (…). I have a sense of paresis in my feet and legs, my limbs are always cold and I feel electric discharges, as if needles”.
ID14: “(…) neurological problems in the lower limbs, I feel as if they are passing inside the shocks, it seems to feel the electric current”.
ID14: “What I am left is definitely anxiety (…)”.
ID13: “I have problems (…) with my head. Besides anxiety I have many memory lapses, holes, and difficulties in remembering some things that happened a few hours before”.
ID12: “I’m fine now but mostly on a psychological level I have problems. I always take the sleeping pill and also the psyche pills”.
ID15: “I am not as I was before the hospitalization, but thanks to psychotherapy I am learning to look back as well as forward (…)”.
3.3. Emotional and Mental Disorders
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Coronavirus Disease (COVID-19). Available online: https://www.who.int/health-topics/coronavirus#tab=tab_1 (accessed on 12 October 2021).
- Liang, W.; Liang, H.; Ou, L.; Chen, B.; Chen, A.; Li, C.; Li, Y.; Guan, W.; Sang, L.; Lu, J.; et al. Development and validation of a clinical risk score to predict the onset of critical illness in hospitalized patients with COVID-19. JAMA Intern. Med. 2020, 180, 1081–1089. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Deiana, G.; Azara, A.; Dettori, M.; Delogu, F.; Vargiu, G.; Gessa, I.; Stroscio, F.; Tidore, M.; Steri, G.; Castiglia, P. Deaths in SARS-CoV-2 Positive Patients in Italy: The Influence of Underlying Health Conditions on Lethality. Int. J. Environ. Res. Public Health 2020, 17, 4450. [Google Scholar] [CrossRef] [PubMed]
- Yun, K.; Lee, J.S.; Kim, E.Y.; Chandra, H.; Oh, B.L.; Oh, J. Severe COVID-19 Illness: Risk Factors and Its Burden on Critical Care Resources. Front. Med. 2020, 7, 583060. [Google Scholar] [CrossRef]
- WHO. A Clinical Case Definition of the Post COVID-19 Condition from a Delphi Consensus. 6 October 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed on 12 October 2021).
- Worldometers. Available online: https://www.worldometers.info/coronavirus/ (accessed on 8 August 2021).
- Sahoo, S.; Mehra, A.; Dua, D.; Suri, V.; Malhotra, P.; Yaddanapudi, L.N.; Puri, G.D.; Grover, S. Psychological experience of patients admitted with SARS-CoV-2 infection. Asian J. Psychiatr. 2020, 54, 102355. [Google Scholar] [CrossRef] [PubMed]
- Tomasoni, D.; Bai, F.; Castoldi, R.; Barbanotti, D.; Falcinella, C.; Mulè, G.; Mondatore, D.; Tavelli, A.; Vegni, E.; Marchetti, G.; et al. Anxiety and depression symptoms after virological clearance of COVID-19: A cross-sectional study in Milan, Italy. J. Med. Virol. 2021, 93, 1175–1179. [Google Scholar] [CrossRef] [PubMed]
- Bonazza, F.; Borghi, L.; di San Marco, E.C.; Piscopo, K.; Bai, F.; Monforte, A.D.A.; Vegni, E. Psychological outcomes after hospitalization for COVID-19: Data from a multidisciplinary follow-up screening program for recovered patients. Res. Psychother. 2021, 23, 491. [Google Scholar] [CrossRef]
- Chen, W.; Ju, Y.; Liu, B.; Huang, M.; Yang, A.; Zhou, Y.; Wang, M.; Liao, M.; Shu, K.; Liu, J.; et al. Negative Appraisals of the COVID-19 Social Impact Associated with the Improvement of Depression and Anxiety in Patients After COVID-19 Recovery. Front. Psychiatry 2021, 12, 585537. [Google Scholar] [CrossRef]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Hao, F.; Tam, W.; Hu, X.; Tan, W.; Jiang, L.; Jiang, X.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; et al. A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID-19 inpatients in isolation facilities. Transl. Psychiatry 2020, 10, 355. [Google Scholar] [CrossRef]
- Dong, F.; Liu, H.L.; Dai, N.; Yang, M.; Liu, J.P. A living systematic review of the psychological problems in people suffering from COVID-19. J. Affect. Disord. 2021, 292, 172–188. [Google Scholar] [CrossRef] [PubMed]
- Sun, N.; Wei, L.; Wang, H.; Wang, X.; Gao, M.; Hu, X.; Shi, S. Qualitative study of the psychological experience of COVID-19 patients during hospitalization. J. Affect. Disord. 2021, 278, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Chung, G.K.; Strong, C.; Chan, Y.H.; Chung, R.Y.; Chen, J.S.; Lin, Y.H.; Huang, R.Y.; Lin, C.Y.; Ko, N.Y. Psychological Distress and Protective Behaviors during the COVID-19 Pandemic among Different Populations: Hong Kong General Population, Taiwan Healthcare Workers, and Taiwan Outpatients. Front. Med. 2022, 9, 800962. [Google Scholar] [CrossRef] [PubMed]
- Bo, H.X.; Li, W.; Yang, Y.; Wang, Y.; Zhang, Q.; Cheung, T.; Wu, X.; Xiang, Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2021, 51, 1052–1053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abate, S.M.; Checkol, Y.A.; Mantefardo, B. Global prevalence and determinants of mortality among patients with COVID-19: A systematic review and meta-analysis. Ann. Med. Surg. 2021, 64, 102204. [Google Scholar] [CrossRef] [PubMed]
- Tingey, J.L.; Bentley, J.A.; Hosey, M.M. COVID-19: Understanding and mitigating trauma in ICU survivors. Psychol. Trauma 2020, 12, S100–S104. [Google Scholar] [CrossRef]
- Sahoo, S.; Mehra, A.; Suri, V.; Malhotra, P.; Yaddanapudi, L.N.; Puri, G.D.; Grover, S. Lived Experiences of COVID-19 Intensive Care Unit Survivors. Indian J. Psychol. Med. 2020, 42, 387–390. [Google Scholar] [CrossRef]
- Kürtüncü, M.; Kurt, A.; Arslan, N. The Experiences of COVID-19 Patients in Intensive Care Units: A Qualitative Study. Omega J. Death Dying 2021, in press. [CrossRef]
- Aiyegbusi, O.L.; Hughes, S.E.; Turner, G.; Rivera, S.C.; McMullan, C.; Chandan, J.S.; Haroon, S.; Price, G.; Davies, E.H.; Nirantharakumar, K.; et al. Symptoms, complications and management of long COVID: A review. J. R. Soc. Med. 2021, 114, 428–442. [Google Scholar] [CrossRef]
- Michelen, M.; Manoharan, L.; Elkheir, N.; Cheng, V.; Dagens, A.; Hastie, C.; O’Hara, M.; Suett, J.; Dahmash, D.; Bugaeva, P.; et al. Characterising long COVID: A living systematic review. BMJ Glob. Health 2021, 6, e005427. [Google Scholar] [CrossRef]
- Ceban, F.; Ling, S.; Lui, L.; Lee, Y.; Gill, H.; Teopiz, K.M.; Rodrigues, N.B.; Subramaniapillai, M.; Di Vincenzo, J.D.; Cao, B.; et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav. Immun. 2022, 101, 93–135. [Google Scholar] [CrossRef] [PubMed]
- Mongodi, S.; Salve, G.; Tavazzi, G.; Politi, P.; Mojoli, F. COVID-19 Post-ICU team; COVID-19 Pavia Crisis Unit. High prevalence of acute stress disorder and persisting symptoms in ICU survivors after COVID-19. Intensiv. Care Med. 2021, 47, 616–618. [Google Scholar] [CrossRef] [PubMed]
- Venturas, M.; Prats, J.; Querol, E.; Zabalegui, A.; Fabrellas, N.; Rivera, P.; Casafont, C.; Cuzco, C.; Frías, C.E.; Olivé, M.C.; et al. Lived Experiences of Hospitalized COVID-19 Patients: A Qualitative Study. Int. J. Environ. Res. Public Health 2021, 18, 10958. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.; Carvalho, P.; Lima, I.; Nunes, J.; Saraiva, J.S.; de Souza, R.I.; da Silva, C.; Neto, M. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020, 287, 112915. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatr. 2020, 33, e100213. [Google Scholar] [CrossRef] [Green Version]
- Colaizzi, P.F. Psychological Research as the Phenomenologist Sees It. In Existential-Phenomenological Alternatives for Psychology; Oxford University Press: New York, NY, USA, 1978; pp. 48–71. [Google Scholar]
- Kroenke, K.; Spitzer, R.; Williams, J.W.; Löwe, B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ-4. Psychosomatics 2009, 50, 613–621. [Google Scholar]
- Merriam, S.B. Qualitative Research and Case Study Applications in Education; Jossey-Bass Publishing House: San Francisco, CA, USA, 1998. [Google Scholar]
- Pei, H.; Wu, Q.; Xie, Y.; Deng, J.; Jiang, L.; Gan, X. A Qualitative Investigation of the Psychological Experiences of COVID-19 Patients Receiving Inpatient Care in Isolation. Clin. Nurs. Res. 2021, 30, 1113–1120. [Google Scholar] [CrossRef]
- Norouzadeh, R.; Abbasinia, M.; Tayebi, Z.; Sharifipour, E.; Koohpaei, A.; Aghaie, B.; Asgarpour, H. Experiences of Patients With COVID-19 Admitted to the Intensive Care Units: A Qualitative Study. J. Patient Exp. 2021, 8, 23743735211007359. [Google Scholar] [CrossRef]
- Shaban, R.Z.; Nahidi, S.; Sotomayor-Castillo, C.; Li, C.; Gilroy, N.; O’Sullivan, M.V.N.; Sorrell, T.C.; White, E.; Hackett, K.; Bag, S. SARS-CoV-2 infection and COVID-19: The lived experience and perceptions of patients in isolation and care in an Australian healthcare setting. Am. J. Infect. Control 2020, 48, 1445–1450. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef]
- Gomez, J.M.D.; Du-Fay-de-Lavallaz, J.M.; Fugar, S.; Sarau, A.; Simmons, J.A.; Clark, B.; Sanghani, R.M.; Aggarwal, N.T.; Williams, K.A.; Doukky, R.; et al. Sex Differences in COVID-19 Hospitalization and Mortality. J. Womens Health 2021, 30, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Higher Institute of Health. ISS COVID-19 Report No. 1/2021. The Mortality Rate of SARS-CoV-2 Infection at Regional Level and across the Different Phases of the Epidemic in Italy. Available online: https://www.iss.it/rapporti-covid-19/-/asset_publisher/btw1J82wtYzH/content/rapporto-isscovid-19-il-case-fatality-rate-dell-infezione-sars-cov-2-a-livello-regionale-e-attraverso-le-differenti-fasi-dell-epidemia-in-italia.-versione-del-20-gennaio-2021 (accessed on 8 October 2021).
- Jamili, S.; Ebrahimipour, H.; Adel, A.; Badiee Aval, S.; Hoseini, S.J.; Vejdani, M.; Ebnehoseini, Z. Experience of patients hospitalized with COVID-19: A qualitative study of a pandemic disease in Iran. Health Expect. 2022, 25, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Y.T.; Yang, Y.; Li, W.; Zhang, L.; Zhang, Q.; Cheung, T.; Ng, C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020, 7, 228–229. [Google Scholar] [CrossRef] [Green Version]
- Banzett, R.B.B.; Sheridan, A.R.; Baker, K.M.; Lansing, R.W.; Stevens, J.P. ‘Scared to death’ dyspnoea from the hospitalised patient’s perspective. BMJ Open Respir. Res. 2020, 7, e000493. [Google Scholar] [CrossRef] [Green Version]
- Shih, F.J.; Chu, S.H. Comparisons of American-Chinese and Taiwanese patients’ perceptions of dyspnea and helpful nursing actions during the intensive care unit transition from cardiac surgery. Heart Lung 1999, 28, 41–54. [Google Scholar] [CrossRef]
- Purssell, E.; Gould, D.; Chudleigh, J. Impact of isolation on hospitalised patients who are infectious: Systematic review with meta-analysis. BMJ Open 2020, 10, e030371. [Google Scholar] [CrossRef]
- Arnold, D.T.; Hamilton, F.W.; Milne, A.; Morley, A.J.; Viner, J.; Attwood, M.; Noel, A.; Gunning, S.; Hatrick, J.; Hamilton, S.; et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: Results from a prospective UK cohort. Thorax 2021, 76, 399–401. [Google Scholar] [CrossRef]
- Carfì, A.; Bernabei, R.; Landi, F.; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef]
- Mandal, S.; Barnett, J.; Brill, S.E.; Brown, J.S.; Denneny, E.K.; Hare, S.S.; Heightman, M.; Hillman, T.E.; Jacob, J.; Jarvis, H.C.; et al. ‘Long-COVID’: A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 2021, 76, 396–398. [Google Scholar] [CrossRef]
- Crook, H.; Raza, S.; Nowell, J.; Young, M.; Edison, P. Long COVID—Mechanisms, risk factors, and management. BMJ 2021, 2021, n1648. [Google Scholar] [CrossRef]
- Sigfrid, L.; Drake, T.M.; Pauley, E.; Jesudason, E.C.; Olliaro, P.; Lim, W.S.; Gillesen, A.; Berry, C.; Lowe, D.J.; McPeake, J.; et al. Long COVID in adults discharged from UK hospitals after COVID-19: A prospective, multicenter cohort study using the ISARIC WHO Clinical Characterisation Protocol. Lancet Reg. Health 2021, 8, 100186. [Google Scholar] [CrossRef] [PubMed]
- Naidu, S.B.; Shah, A.J.; Saigal, A.; Smith, C.; Brill, S.E.; Goldring, J.; Hurst, J.R.; Jarvis, H.; Lipman, M.; Mandal, S. The high mental health burden of “Long COVID” and its association with on-going physical and respiratory symptoms in all adults discharged from hospital. Eur. Respir. J. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
| Questions |
|---|
| 1. How did you feel when you realized (or were told) that you were hospitalized in ICU? |
| 2. What was your main worry/stressor during ICU hospitalization? |
| 3. How is your health now (any consequences)? |
| 4. What was your feeling about becoming seriously ill during this pandemic? |
| Participant ID | Gender | Age | Respiratory Support in ICU | ICU LoS (Days) | Total LoS (Days) |
|---|---|---|---|---|---|
| 1 | M | 41 | TI | 18 | 21 |
| 2 | M | 57 | TI + tracheostomy | 98 | 159 |
| 3 | M | 61 | TI | 29 | 65 |
| 4 | M | 38 | TI | 10 | 45 |
| 5 | M | 48 | TI + tracheostomy | 45 | 90 |
| 6 | M | 49 | TI | 34 | 90 |
| 7 | M | 57 | TI + tracheostomy | 19 | 41 |
| 8 | F | 63 | NIV/mask ventilation | 13 | 27 |
| 9 | F | 75 | NIV/mask ventilation | 42 | 90 |
| 10 | F | 65 | NIV/mask ventilation | 45 | 84 |
| 11 | M | 70 | TI + tracheostomy | 54 | 120 |
| 12 | M | 66 | NIV/mask ventilation | 40 | 55 |
| 13 | M | 65 | TI | 22 | 40 |
| 14 | M | 43 | TI + tracheostomy | 48 | 108 |
| 15 | M | 48 | TI | 21 | 38 |
| N. | Main Themes | Interviewees from Who the Themes Were Emerged |
|---|---|---|
| i | Emotion of fear | ID4, ID6, ID7, ID8, ID9, ID11, ID13, ID14, ID15 |
| ID4, ID6, ID7, ID9, ID11, ID14, ID15, | |
| ID4, ID8, ID11, ID13 | |
| ii | Isolation and loneliness | ID2, ID3, ID4, ID6, ID7, ID10, ID11, ID12, ID13 |
| iii | Unawareness about the gravity of the situation as a protective factor | ID1, ID5, ID6, ID7, ID11, ID13 |
| iv | “Long COVID”: consequences of the disease on health | ID5, ID6, ID7, ID8, ID9, ID11, ID12, ID13, ID14, ID15 |
| PHQ Referred to the Hospitalization Time | ||
| Score/Value | Participant (n) | % |
| 0–2 (normal) | 5 | 33.3% |
| 3–5 (mild) | 9 | 60% |
| 6–8 (moderate) | 1 | 6.7% |
| 9–12 (severe) | 0 | 0 |
| Total | 15 | 100% |
| PHQ Referred to the Time of the Interview | ||
| Score/Value | Participant (n) | % |
| 0–2 (normal) | 13 | 86.7% |
| 3–5 (mild) | 2 | 13.3% |
| 6–8 (moderate) | 0 | 0 |
| 9–12 (severe) | 0 | 0 |
| Total | 15 | 100% |
| ID Participant | PHQ Value during the Hospitalization (Sum) | PHQ Value at the Time of Interview (Sum) | ||
|---|---|---|---|---|
| 1 | 5 | (mild) | 0 | (normal) |
| 2 | 2 | (normal) | 1 | (normal) |
| 3 | 0 | (normal) | 0 | (normal) |
| 4 | 3 | (mild) | 2 | (normal) |
| 5 | 1 | (normal) | 0 | (normal) |
| 6 | 1 | (normal) | 0 | (normal) |
| 7 | 4 | (mild) | 1 | (normal) |
| 8 | 5 | (mild) | 3 | (mild) |
| 9 | 1 | (normal) | 1 | (normal) |
| 10 | 4 | (mild) | 0 | (normal) |
| 11 | 5 | (mild) | 1 | (normal) |
| 12 | 3 | (mild) | 1 | (normal) |
| 13 | 4 | (mild) | 1 | (normal) |
| 14 | 7 | (moderate) | 3 | (mild) |
| 15 | 5 | (mild) | 2 | (normal) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piras, I.; Piazza, M.F.; Piccolo, C.; Azara, A.; Piana, A.; Finco, G.; Galletta, M. Experiences, Emotions, and Health Consequences among COVID-19 Survivors after Intensive Care Unit Hospitalization. Int. J. Environ. Res. Public Health 2022, 19, 6263. https://doi.org/10.3390/ijerph19106263
Piras I, Piazza MF, Piccolo C, Azara A, Piana A, Finco G, Galletta M. Experiences, Emotions, and Health Consequences among COVID-19 Survivors after Intensive Care Unit Hospitalization. International Journal of Environmental Research and Public Health. 2022; 19(10):6263. https://doi.org/10.3390/ijerph19106263
Chicago/Turabian StylePiras, Ilenia, Maria Francesca Piazza, Cristina Piccolo, Antonio Azara, Andrea Piana, Gabriele Finco, and Maura Galletta. 2022. "Experiences, Emotions, and Health Consequences among COVID-19 Survivors after Intensive Care Unit Hospitalization" International Journal of Environmental Research and Public Health 19, no. 10: 6263. https://doi.org/10.3390/ijerph19106263
APA StylePiras, I., Piazza, M. F., Piccolo, C., Azara, A., Piana, A., Finco, G., & Galletta, M. (2022). Experiences, Emotions, and Health Consequences among COVID-19 Survivors after Intensive Care Unit Hospitalization. International Journal of Environmental Research and Public Health, 19(10), 6263. https://doi.org/10.3390/ijerph19106263









