Abstract
The aim of this study was to analyze the trends in diabetes in pregnancy in Belgrade, Serbia for the period of the past decade and forecast the number of women with pre-gestational diabetes for the years 2030 and 2050. The study included the data on all pregnant women with diabetes from the registry of the deliveries in Belgrade, by the City Institute of Public Health of Belgrade, Serbia for the period between 2010 and 2020 and the published data on the deliveries on the territory of Belgrade. During the examined period the total number of live births in Belgrade was 196,987, and the prevalence of diabetes in pregnancy was 3.4%, with the total prevalence of pre-gestational diabetes of 0.7% and overall prevalence of GDM of 2.7%. The average age of women in our study was significantly lower in 2010 compared to 2020. The forecasted prevalence of pre-gestational diabetes among all pregnant women for 2030 is 2% and 4% for 2050 in our cohort. Our study showed that the prevalence of pre-gestational diabetes has increased both among all pregnant women and among women with diabetes in pregnancy in the past decade in Belgrade, Serbia and that it is expected to increase further in the next decades and to further double by 2050.
1. Introduction
More than 20 million births per year worldwide are associated with diabetes in pregnancy. The diabetes in pregnancy can be classified in two large categories: pre-gestational diabetes that includes mainly type 1 diabetes mellitus (T1DM), and type 2 diabetes mellitus (T2DM), along with specific types of diabetes and on the gestational diabetes mellitus (GDM), diabetes first diagnosed during the late second or third trimesters of pregnancy [1].
Although it is well known that both gestational diabetes (GDM) and pre-gestational diabetes are associated with numerous pregnancy complications, large studies that examine the prevalence of pre-gestational diabetes in the population are generally lacking. The majority of studies examining the characteristics of pregnant women with pre-gestational diabetes are based in clinical settings, and population-wide studies are sparse [2].
The vast majority of women with diabetes in pregnancy have GDM: between 80% and 90%, while the remaining 15% are the pre-gestational diabetes [1]. In past decades, the prevalence of pre-gestational diabetes is increasing mainly due to the rise of the prevalence of T2DM in the general population of women of the reproductive age, as a consequence of the obesity epidemic [3]. Pre-gestational diabetes is associated with the higher likelihood for congenital anomalies, stillbirth and large for gestational age infants, preterm births, and operative deliveries [3,4,5]. It is expected that the prevalence of pre-gestational diabetes during pregnancy reflects the prevalence of diabetes in the general population, but the women with pre-gestational diabetes have decreased fertility and the prevalence of pre-gestational diabetes underestimates the prevalence of the DM in the general population [1]. The decrease in fertility among women with pre-gestational diabetes is associated with the microvascular and cardiovascular complications among women with T1DM and with the high prevalence of obesity and polycystic ovarian syndrome among women with T2DM [1].
It is expected that the prevalence of overweight and obesity among the pregnant women in the future will increase, along with the increase in the body mass index of children and adolescents. The prevalence of the pre-gestational DM will also increase. All this raises more concerns from a public health perspective and the perspective of the possible pregnancy associated complications and their costs [1].
The total number of individuals with diabetes is now expected to increase to almost 600 million in the world by 2030 and 700 million by 2050, which is the double of the expected number for 2030 forecasted back in 2004 [6,7]. The rise in the prevalence of T2DM among younger populations has also shown that these women have similar rates of diabetic nephropathy, commonly considered the significant predictor of the adverse pregnancy outcomes, in women with T1DM in pregnancy. This is despite the fact that the women with T1DM have significantly longer duration of illness prior to pregnancy [8].
The health care system must be able to provide the identification of women with pre-gestational diabetes and to provide the adequate counseling to achieve the best possible time for conception at the time of the best possible glycemic control, enable the adequate control during pregnancy and puerperium in order to maximize the benefits for the mothers and for the newborns [1]. This can be achieved through the adequate allocation of the recourses in the health care system. Both material and human recourses need to be directed towards the women with diabetes [1,9,10].
In order for the health care system to provide those services, adequate planning is necessary based on the predicted number of women in need. The aim of this study is to analyze the trends in the diabetes in pregnancy in Belgrade, Serbia for the period of the past decade and to forecast the number of women with pre-gestational diabetes for the years 2030 and 2050.
2. Materials and Methods
The study included the data on all pregnant women with diabetes from the registry of the deliveries in Belgrade, by the City Institute of Public Health of Belgrade, Serbia for the period between 2010 and 2020 and the published data on the deliveries on the territory of Belgrade [11].
The data in the registry are the data on the maternal age, the health care institution that delivery occurred in, the newborns’ birth weight, the newborns’ birth length, the gestational age at birth, the Apgar score, the type of delivery, and the presence of any chronic illness of pregnant women (chronic hypertension, preeclampsia, pregnancy induced hypertension, development of the HEELP syndrome, diabetes type).
For the purpose of this study, we analyzed the trends in the number of women with pre-gestational diabetes and used the forecast analysis to predict the number of women with pre-gestational diabetes in 2030 and in 2050. Based on the reported number of deliveries in Belgrade in each year, we calculated the prevalence of pre-gestational diabetes and GDM among all pregnant women who delivered in Belgrade in each year.
The Ethical committee of the Faculty of Medicine, University of Belgrade approved the study (No 1322/IX-80).
Statistical analyses were done using the descriptive and analytical statistics. The differences between the groups on the numerical variables were examined using the univariate variance analysis (ANOVA). Time trends were analyzed creating the traditional forecasting models with the specification of the data of the final forecast of 2050. All statistical analyses were done using the SPSS for Windows 22.0.
3. Results
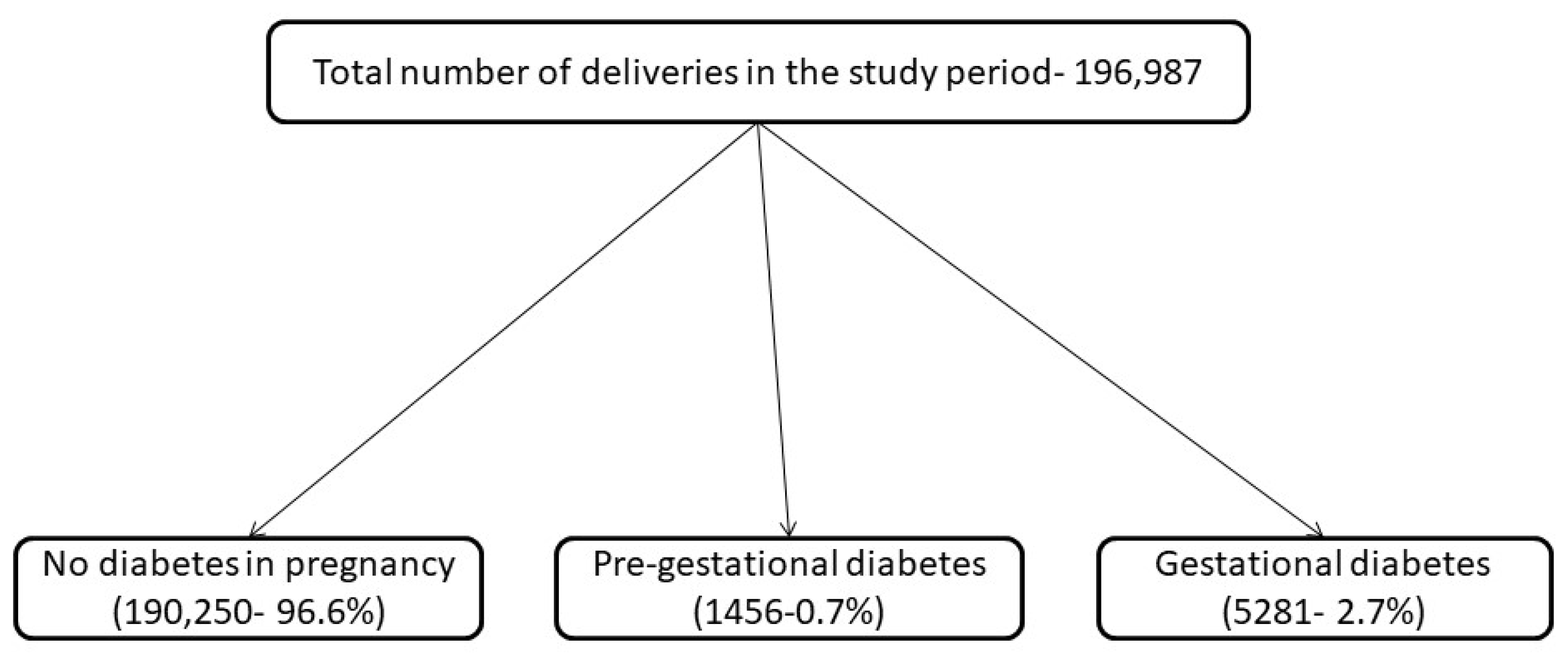
During the examined period, the total number of live births in Belgrade was 196,987, and the prevalence of diabetes in pregnancy was 3.4%, with the total prevalence of pre-gestational diabetes of 0.7% and overall prevalence of GDM of 2.7%. The prevalence of diabetes in pregnancy and factors associated with it are described elsewhere [12]. Almost four fifths of the women with diabetes had GDM (5281—78.4%), just under one fifth (1318—19.6%) had T1DM, while 138 women (2.0%) had T2DM. The total number of women with pre-gestational diabetes was 1456 (21.6%). The highest number of women treated with pre-gestational diabetes was in 2018 (261 women) and the highest prevalence of pre-gestational diabetes among women with diabetes was 71.5% in 2020. A flow diagram showing the study population is presented in Figure 1.
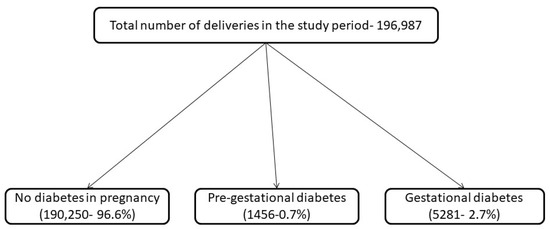
Figure 1.
Flow diagram representing the study population.
The total number of women with pre-gestational and GDM and the prevalence of pre-gestational and GDM in each year of the study are presented in Table 1.

Table 1.
The total number of women with pre-gestational diabetes and GDM and the prevalence of pre-gestational diabetes and GDM in each year of the study.
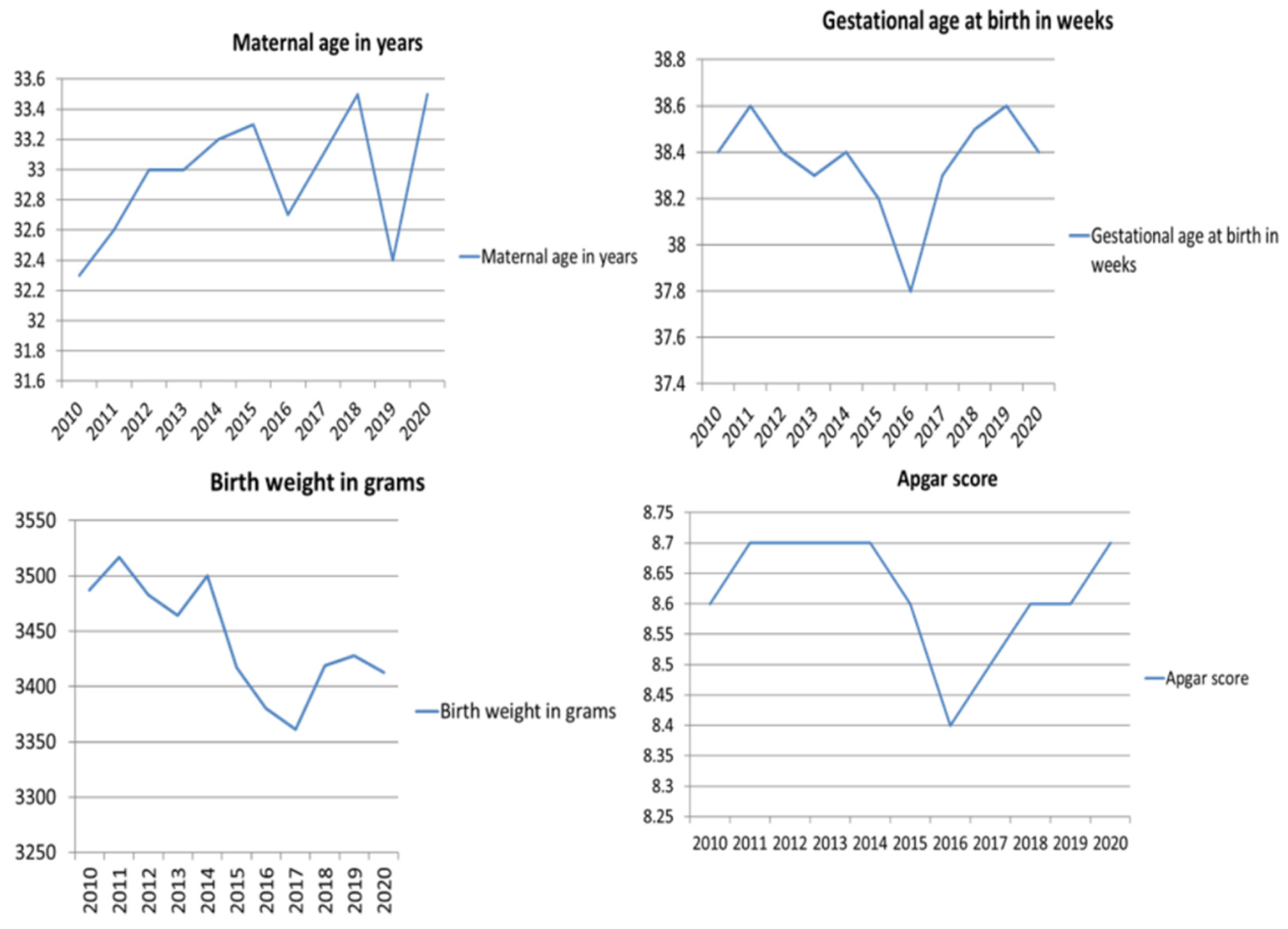
The average age of women with DM included in the study was 32.96 ± 5.22 years, the average gestational age at delivery was 38.4 ± 1.86 weeks, the average newborns’ birth weight was 3453.99 ± 611.11 g and the average Apgar score was 8.63 ± 1.21. Maternal age increased in this period from 32.3 ± 5.23 to 33.5 ± 5.30 years, gestational age at delivery was the same in 2010 and in 2020 (38.4 weeks) Apgar score remained the same (8.60 ± 1.2 in 2010 and 8.68 ± 1.09), except for the decrease in 2016 (8.44 ± 1.43). In 2016 there was the lowest average gestational age at delivery (37.80 ± 2.22 weeks), birth weight (3380.27 ± 627.84) and the lowest average Apgar score (8.44 ± 1.43). The average maternal age differed significantly between 2010 and 2020 (p = 0.035). The trends in the maternal age, the gestational age at delivery, the newborns’ birth weight and the Apgar scores in the study period are presented in Figure 2.
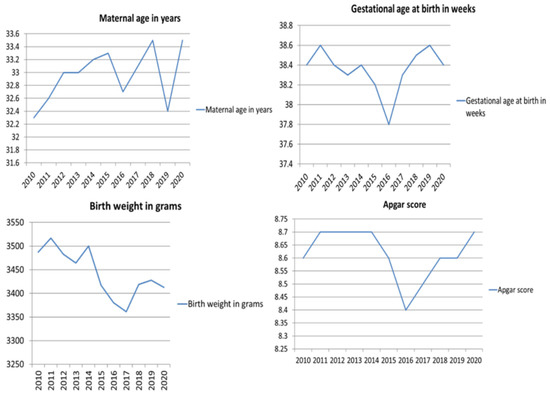
Figure 2.
The trends in the maternal age, gestational age at delivery, newborns’ birth weight and Apgar scores in the study period.
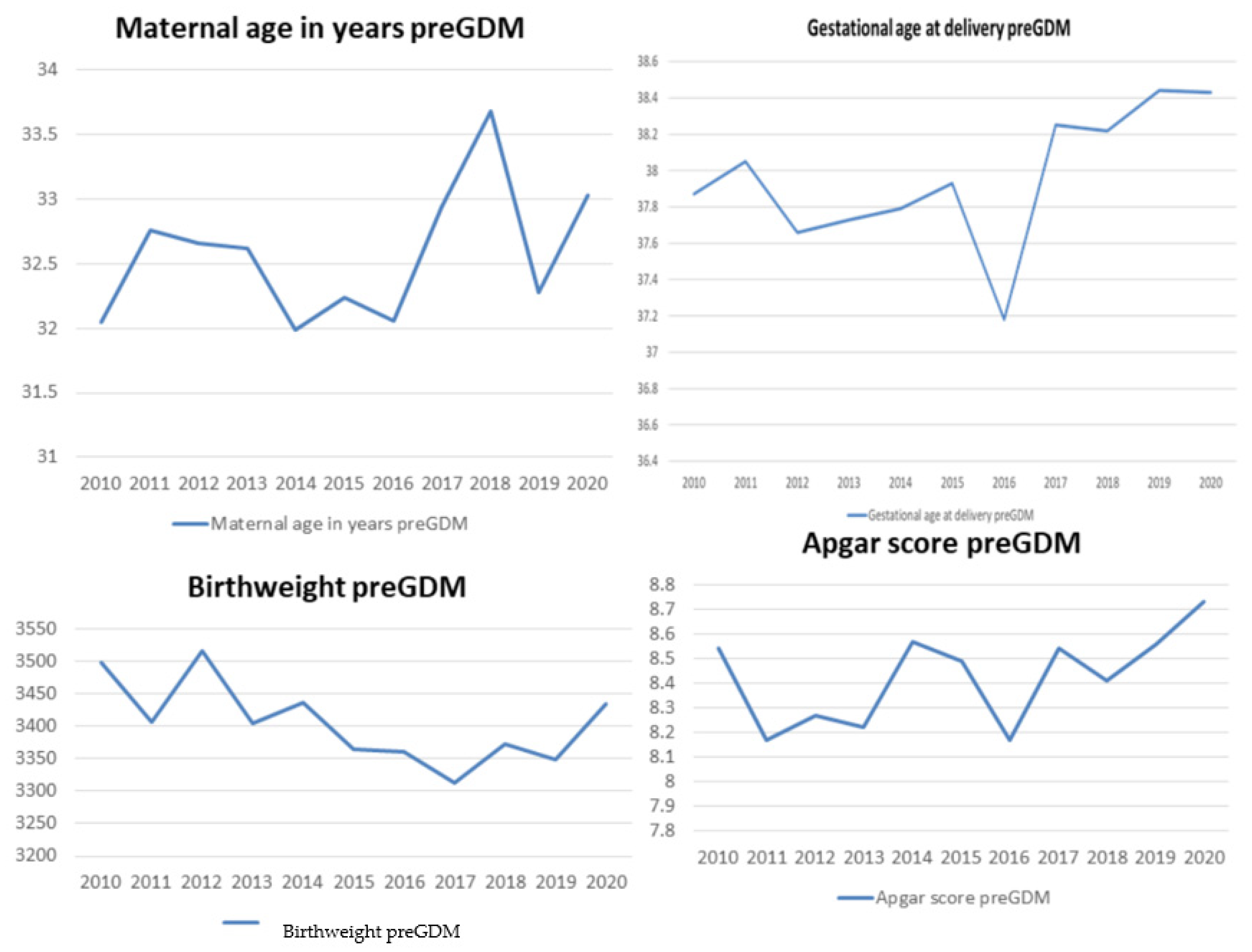
There were no significant differences in the average maternal age, the average gestational age at birth, the average birth weight, or the average Apgar scores between the different years in our examined period among the women with pre-gestational diabetes. Trends in the average maternal age, the gestational age at delivery, the newborns’ birth weight and the average Apgar scores among women with pre-gestational diabetes are presented in Figure 3.
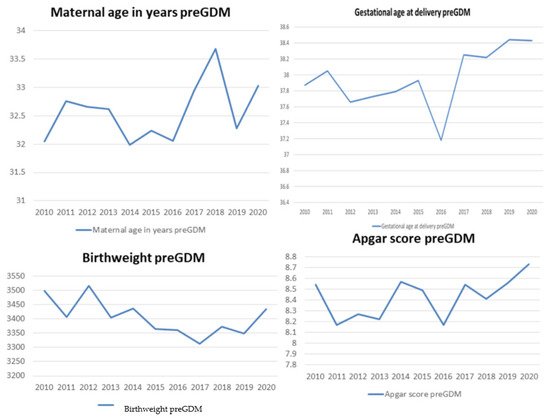
Figure 3.
Trends in average maternal age, gestational age at delivery, newborns’ birth weight and average Apgar scores among women with pre-gestational diabetes.
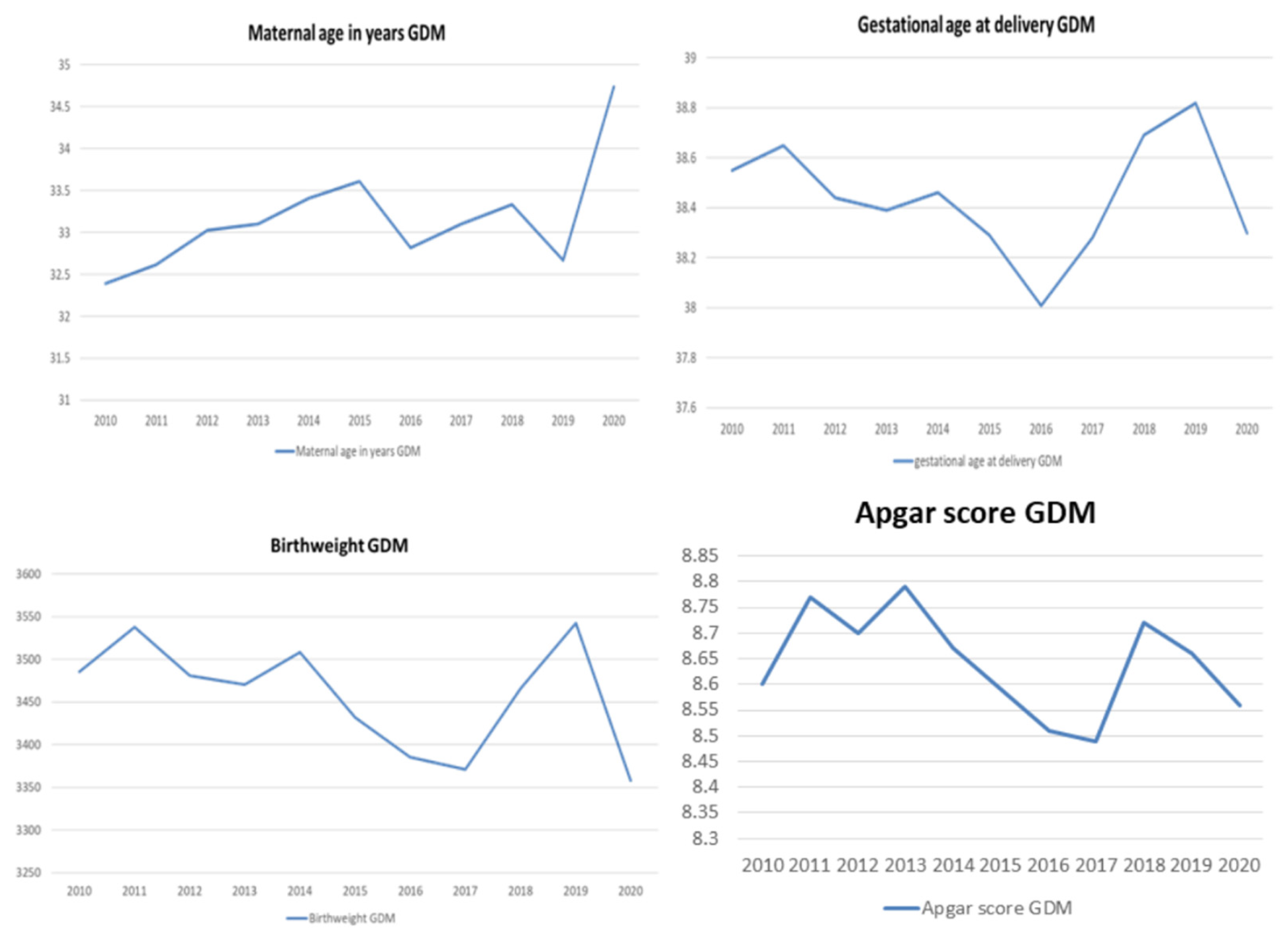
Women with GDM were significantly older in 2020 compared to women in 2010 and 2011 (33.74 ± 5.24 years in 2020, compared to 32.39 ± 5.18 in 2010, and 32.62 ± 5.09 in 2011, p = 0.003 and p = 0.013, respectively). Gestational age at delivery was the lowest in 2016, with significant differences between 2016 and 2010, 2011, 2012, 2013, 2014, 2018 and 2019. The trends in average maternal age, the gestational age at delivery, the newborns’ birth weight and the average Apgar scores among women with GDM are presented in Figure 4.
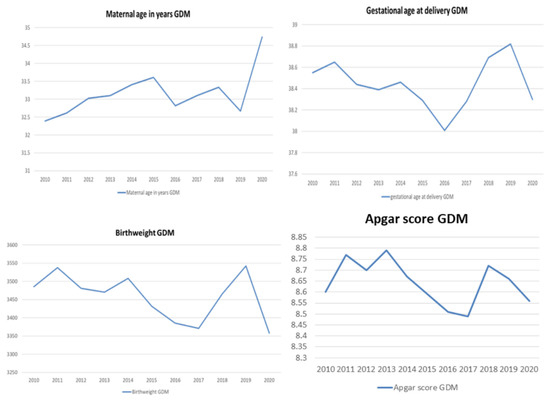
Figure 4.
The trends in average maternal age, gestational age at delivery, newborns’ birth weight and average Apgar scores among women with GDM.
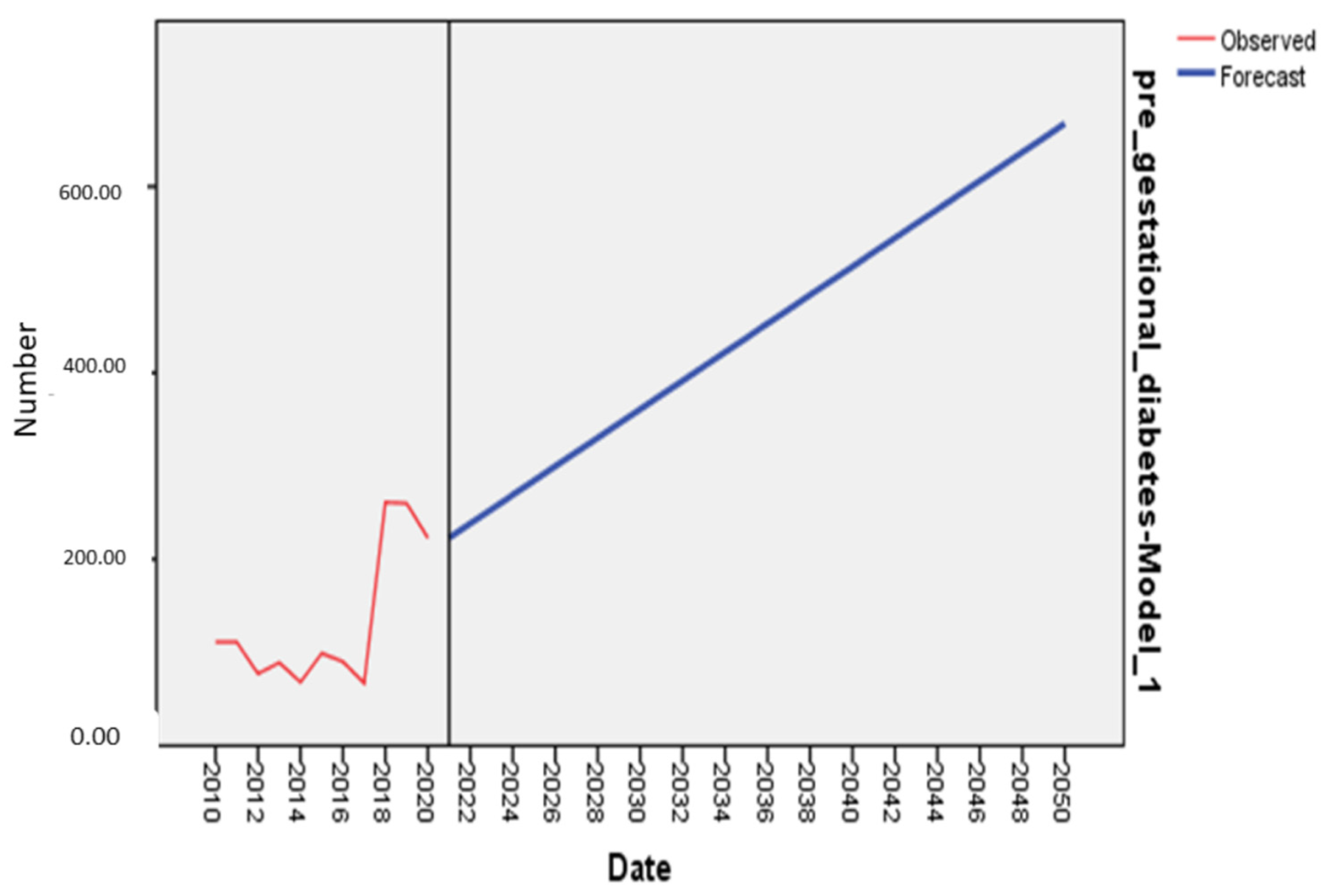
The forecasted number of women with GDM for 2030 is 180 (95% CI: −1290–1650). The forecasted number of women with pre-gestational diabetes for 2030 is 361 (95% CI: 225–497) and is 668 (95% CI: 532–803) for 2050 and the forecasted prevalence of pre-gestational diabetes among all pregnant women for 2030 is 2% and 4% for 2050. The forecast for pre-gestational diabetes is presented on Figure 5.
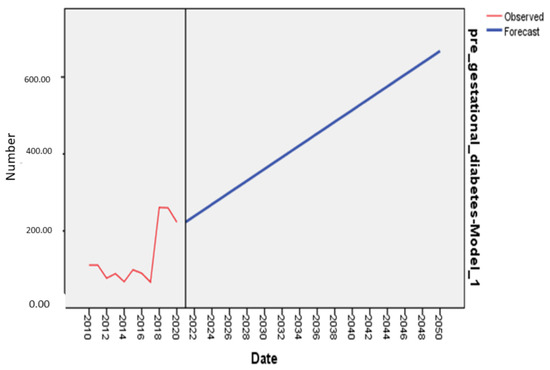
Figure 5.
The forecast of the total number of women with pre-gestational diabetes in 2030 and 2050.
The model was assessed using the simulation performance parameters, the root mean square error (RMSE) was 60.04, mean absolute percentage error (MAPE) was 43.94, mean absolute error (MAE) was 46.86.
The forecasted number of live births for both 2030 and 2050 is 17908 (95% CI: 16,241–19,575) making the forecasted prevalence of pre-gestational diabetes 2% for 2030 and 3.7% for 2050.
4. Discussion
The aim of this study was to examine the trends and to forecast the number of women with pre-gestational diabetes using the registry data for the period of 11 years at the territory of the City of Belgrade, Serbia. Our study has shown that the prevalence of pre-gestational diabetes among the women with diabetes in Belgrade, Serbia increased in the past decade, as did the prevalence of pre-gestational diabetes among all pregnant women. Further, according to our results, the prevalence of pre-gestational diabetes among all pregnant women is expected to increase in the next decades to 2% in 2030 and almost 4% in 2050.
The increase in the prevalence of pre-gestational diabetes is in line with the increase in the prevalence of DM in all age groups in both sexes, including the increase among women of the reproductive age [6]. This increase is largely associated with the increase in the prevalence of obesity worldwide and as this increase is not expected to slow down in the next decades, the forecasted increase in the prevalence of pre-gestational diabetes is fitting to these expectations [13].
As pre-gestational diabetes is associated with the decreased fertility rates, the increase in the number of women in the reproductive age with diabetes may lead to increase in the needs for the assisted reproductive technologies, its costs and the burden of pregnancy risks associated with them [1]. Further, the pregnancies with diabetes significantly burden the healthcare system through the necessities for the strict control, for diagnosis and treatment of the pregnancy associated complications and for the various adverse pregnancy outcomes for both mothers and newborns [14].
Increase in the prevalence of pre-gestational diabetes is expected to lead to the increase in the prevalence of all associated pregnancy complications affecting the mothers and the newborns, such as miscarriages, Caesarean deliveries, lacerations during vaginal deliveries, venous thromboembolism, congenital malformations, perinatal asphyxia and an overall higher perinatal mortality [15,16,17]. All of these complications are associated with the higher likelihood for increase in the length of hospital stay and the increase in the health care required for each women and the newborn [18].
The health care systems must work toward being able to provide best possible pre-conception and pre-natal care for women with pre-gestational diabetes. In order to achieve that, there is a highlighted need for strengthening the surveillance system for diabetes in pregnancy, mainly through the improvement of existing data sources, improvement of data quality and diabetes screening. With this the researchers, public health professionals, clinicians and all stakeholders in the health care system can have better insight in the actual burden of diabetes in pregnancy and all of its complications.
The average age of women in our study was significantly lower in 2010 compared to 2020, which is in line with the increasing maternal age worldwide [19,20]. However, these differences were not present when the group of pregnant women with pre-gestational diabetes only was analyzed, and were present among women with GDM. The increasing maternal age is the risk factor for the development of GDM, while the women with pre-gestational diabetes may be more prone not to postpone the pregnancy, and to get pregnant at the point with the shorter duration of illness.
Limitations
Our predictions are based on the citywide registry data and may not reflect the country level population. However, the majority of women with diabetes in pregnancy are referred to Belgrade for delivery from other regions in Serbia. Moreover, as shown previously, the analyses of the trends in the prevalence of diabetes in the general population and the forecasts based on these trends tend to underestimate the actual prevalence of the disease and the increase in diabetes prevalence is more than a double compared to the forecasted prevalence. This can significantly influence the clinicians working with the pregnant women with the pre-gestational diabetes and burden the healthcare system even further. We did not include the changes in the prevalence of the possible risk factors for diabetes in pregnancy in the forecasting analysis, and therefore did not account for the possible changes in those factors as well.
5. Conclusions
Our study showed that the prevalence of pre-gestational diabetes has increased both among all pregnant women and among women with diabetes in pregnancy in the past decade in Belgrade, Serbia and that it is expected to increase further in the next decades to 2% in 2030 and to further double by 2050 to 4%. As all types of hyperglycemia in pregnancy have significant intergenerational effect, expecting to influence the global prevalence of diabetes, as well, the forecasted increase in the prevalence of pre-gestational diabetes places high responsibility on the clinicians working with the women with diabetes in pregnancy as the adequate glycemic control not only influences the proximal outcomes related directly to the pregnancy and the childbirth, but also distal outcomes relating mostly to the risk for the diabetic complications in the women with pre-gestational diabetes.
Author Contributions
Conceptualization, S.D. (Stefan Dugalic), M.P., J.T., D.S. and M.G.; methodology, S.D. (Stefan Dugalic) and D.S.; software, D.S.; formal analysis, J.T., D.S. and B.V.; investigation, S.D. (Stefan Dugalic), M.P., A.J., L.L., T.M., N.L., K.L., M.S., T.S., A.S., K.S., S.V.-P. and M.M.; resources, S.D. (Stefan Dugalic), M.P., M.G., S.V.-P., A.S., K.S., M.M. and R.C.; data curation S.D. (Stefan Dugalic), M.P., A.J., L.L., T.M., N.L., K.L., M.S., A.S., K.S., S.V.-P., M.M., R.C., S.B. and S.P.-K.; writing—original draft preparation, S.D. (Stefan Dugalic), B.V., J.T., D.S., L.L., Z.T.-S., P.P., I.P., S.D. (Sinisa Djurasevic), M.M., M.J., S.B. and M.G.; writing—review and editing, S.D. (Stefan Dugalic), D.S., J.T., L.L., Z.T.-S., P.P., M.J., S.P.-K. and M.G.; visualization, D.S., J.T., T.S. and M.J.; supervision, M.P., B.V., N.L., K.L., A.S., K.S. and M.G.; project administration, S.D. (Stefan Dugalic) and M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Ethical committee of the Faculty of Medicine, University of Belgrade approved the study (No 1322/IX-80).
Informed Consent Statement
The study used registry data.
Data Availability Statement
Not applicable. The data used in this study is the data owned by the City Institute of Public Health of Belgrade, Serbia.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Egan, A.M.; Dunne, F.P. Epidemiology of Gestational and Pregestational Diabetes Mellitus. In Gestational Diabetes; Karger Publishers: Basel, Switzerland, 2019; Volume 28, pp. 1–10. [Google Scholar]
- Gualdani, E.; Di Cianni, G.; Seghieri, M.; Francesconi, P.; Seghieri, G. Pregnancy outcomes and maternal characteristics in women with pregestational and gestational diabetes: A retrospective study on 206,917 singleton live births. Acta Diabetol. 2021, 58, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Khalifeh, A.; Breathnach, F.; Coulter-Smith, S.; Robson, M.; Fitzpatrick, C.; Malone, F. Changing trends in diabetes mellitus in pregnancy. J. Obstet. Gynaecol. 2014, 34, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Xodo, S.; Londero, A.P.; D’agostin, M.; Novak, A.; Galasso, S.; Pittini, C.; Baccarini, G.; Grimaldi, F.; Driul, L. Is glycated hemoglobin a1c level associated with adverse pregnancy outcomes of women affected by pre-gestational diabetes? Medicina 2021, 57, 461. [Google Scholar] [CrossRef] [PubMed]
- Mackin, S.T.; Nelson, S.M.; Kerssens, J.J.; Wood, R.; Wild, S.; Colhoun, H.M.; Leese, G.P.; Philip, S.; Lindsay, R.S. Diabetes and pregnancy: National trends over a 15 year period. Diabetologia 2018, 61, 1081–1088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wild, S.; Roglic, G.; Green, A.; Sicree, R.; King, H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004, 27, 1047–1053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maahs, D.M.; Snively, B.M.; Bell, R.A.; Dolan, L.; Hirsch, I.; Imperatore, G.; Linder, B.; Marcovina, S.M.; Mayer-Davis, E.J.; Pettitt, D.J.; et al. Higher prevalence of elevated albumin excretion in youth with type 2 than type 1 diabetes: The SEARCH for Diabetes in Youth study. Diabetes Care 2007, 30, 2593–2598. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morampudi, S.; Balasubramanian, G.; Gowda, A.; Zomorodi, B.; Patil, A.S. The challenges and recommendations for gestational diabetes mellitus care in India: A review. Front. Endocrinol. 2017, 8, 56. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, K.K.; De Courten, M.; Kapur, A. Health system and societal barriers for gestational diabetes mellitus (GDM) services—Lessons from World Diabetes Foundation supported GDM projects. BMC Int. Health Hum. Rights 2012, 12, 1. [Google Scholar] [CrossRef] [Green Version]
- City Institute of Public Health Belgrade. City Institute of Public Health of Belgrade Statistical Report of Health Care in Belgrade for 2020; City Institute of Public Health of Belgrade: Belgrade, Serbia, 2021. [Google Scholar]
- Gojnic, M.; Todorovic, J.; Stanisavljevic, D.; Jotic, A.; Lukic, L.; Milicic, T.; Dugalic, S. Maternal and Fetal Outcomes among Pregnant Women with Diabetes. Int. J. Environ. Res. Public Health 2022, 19, 3684. [Google Scholar] [CrossRef]
- Pineda, E.; Sanchez-Romero, L.M.; Brown, M.; Jaccard, A.; Jewell, J.; Galea, G.; Webber, L.; Breda, J. Forecasting Future Trends in Obesity across Europe: The Value of Improving Surveillance. Obes. Facts 2018, 11, 360–371. [Google Scholar] [CrossRef]
- Dall, T.M.; Yang, W.; Gillespie, K.; Mocarski, M.; Byrne, E.; Cintina, I.; Beronja, K.; Semilla, A.P.; Iacobucci, W.; Hogan, P.F. The economic burden of elevated blood glucose levels in 2017: Diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care 2019, 42, 1661–1668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coton, S.J.; Nazareth, I.; Petersen, I. A cohort study of trends in the prevalence of pregestational diabetes in pregnancy recorded in UK general practice between 1995 and 2012. BMJ Open 2016, 6, e009494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yefet, E.; Jeda, E.; Tzur, A.; Nachum, Z. Markers for undiagnosed type 2 diabetes mellitus during pregnancy—A population-based retrospective cohort study. J. Diabetes 2020, 12, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Isabey, E.P.; Pylypjuk, C.L. The Relationship between Fetal Abdominal Wall Thickness and Intrapartum Complications amongst Mothers with Pregestational Type 2 Diabetes. J. Diabetes Res. 2021, 2021, 5544599. [Google Scholar] [CrossRef] [PubMed]
- Van Otterloo, L.; Connelly, C.; Gould, J.; Abreo, A.; Main, E. Mothers at Risk: Factors Affecting Maternal Postpartum Length of Stay. J. Perinat. Neonatal Nurs. 2018, 32, 303–314. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.N.; Choi, D.W.; Kim, D.S.; Park, E.C.; Kwon, J.Y. Maternal age and risk of early neonatal mortality: A national cohort study. Sci. Rep. 2021, 11, 814. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ren, X.; He, L.; Li, J.; Zhang, S.; Chen, W. Maternal age and the risk of gestational diabetes mellitus: A systematic review and meta-analysis of over 120 million participants. Diabetes Res. Clin. Pract. 2020, 162, 108044. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).