Acute Kidney Failure among Brazilian Agricultural Workers: A Death-Certificate Case-Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Studied Area
2.2. Data Collection
2.3. Trends in AKF Mortality Sample
2.4. Death-Certificate-Based Case-Control Sample
2.5. Statistical Analyses
2.5.1. AKF Mortality Time Trend Analysis
2.5.2. Case-Control Analysis
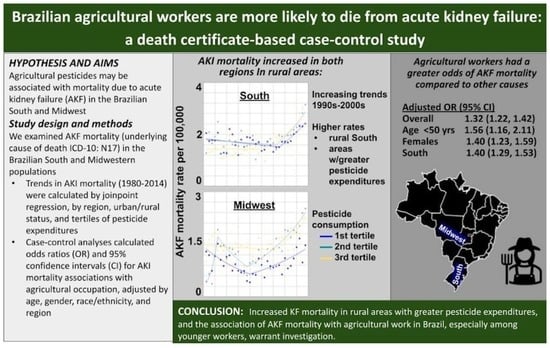
3. Results
3.1. Mortality Trends
3.2. Agricultural Work and AKF
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bellomo, R.; Kellum, J.A.; Ronco, C. Acute Kidney Injury. Lancet 2012, 380, 756–766. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron. Clin. Pract. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Soares, D.M.; Pessanha, J.F.; Sharma, A.; Brocca, A.; Ronco, C. Delayed Nephrology Consultation and High Mortality on Acute Kidney Injury: A Meta-Analysis. Blood Purif. 2017, 43, 57–67. [Google Scholar] [CrossRef] [PubMed]
- Susantitaphong, P.; Cruz, D.N.; Cerda, J.; Abulfaraj, M.; Alqahtani, F.; Koulouridis, I.; Jaber, B.L. Acute Kidney Injury Advisory Group of the American Society of Nephrology World Incidence of AKI: A Meta-Analysis. Clin. J. Am. Soc. Nephrol. 2013, 8, 1482–1493. [Google Scholar] [CrossRef] [Green Version]
- Cerdá, J.; Bagga, A.; Kher, V.; Chakravarthi, R.M. The Contrasting Characteristics of Acute Kidney Injury in Developed and Developing Countries. Nat. Clin. Pract. Nephrol. 2008, 4, 138–153. [Google Scholar] [CrossRef]
- Hoste, E.A.; Kellum, J.A.; Selby, N.M.; Zarbock, A.; Palevsky, P.M.; Bagshaw, S.M.; Goldstein, S.L.; Cerdá, J.; Chawla, L.S. Global Epidemiology and Outcomes of Acute Kidney Injury. Nat. Rev. Nephrol. 2018, 14, 607–625. [Google Scholar] [CrossRef]
- Grams, M.E.; Matsushita, K.; Sang, Y.; Estrella, M.M.; Foster, M.C.; Tin, A.; Kao, W.L.; Coresh, J. Explaining the Racial Difference in AKI Incidence. J. Am. Soc. Nephrol. 2014, 25, 1834–1841. [Google Scholar] [CrossRef] [Green Version]
- Xue, J.L.; Daniels, F.; Star, R.A.; Kimmel, P.L.; Eggers, P.W.; Molitoris, B.A.; Himmelfarb, J.; Collins, A.J. Incidence and Mortality of Acute Renal Failure in Medicare Beneficiaries, 1992 to 2001. J. Am. Soc. Nephrol. 2006, 17, 1135–1142. [Google Scholar] [CrossRef]
- Hsu, C.-Y.; McCulloch, C.; Fan, D.; Ordonez, J.; Chertow, G.; Go, A. Community-Based Incidence of Acute Renal Failure. Kidney Int. 2007, 72, 208–212. [Google Scholar] [CrossRef] [Green Version]
- Cerdá, J.; Lameire, N.; Eggers, P.; Pannu, N.; Uchino, S.; Wang, H.; Bagga, A.; Levin, A. Epidemiology of Acute Kidney Injury. Clin. J. Am. Soc. Nephrol. 2008, 3, 881–886. [Google Scholar] [CrossRef] [Green Version]
- Ponce, D.; Balbi, A. Acute Kidney Injury: Risk Factors and Management Challenges in Developing Countries. Int. J. Nephrol. Renov. Dis. 2016, 9, 193–200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rewa, O.; Bagshaw, S.M. Acute Kidney Injury-Epidemiology, Outcomes and Economics. Nat. Rev. Nephrol. 2014, 10, 193–207. [Google Scholar] [CrossRef] [PubMed]
- Rossaint, J.; Zarbock, A. Acute Kidney Injury: Definition, Diagnosis and Epidemiology. Minerva Urol. Nefrol. 2016, 68, 49–57. [Google Scholar] [PubMed]
- Lebov, J.F.; Engel, L.S.; Richardson, D.; Hogan, S.L.; Sandler, D.P.; Hoppin, J.A. Pesticide Exposure and End-Stage Renal Disease Risk among Wives of Pesticide Applicators in the Agricultural Health Study. Environ. Res. 2015, 143, 198–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lebov, J.F.; Engel, L.S.; Richardson, D.; Hogan, S.L.; Hoppin, J.A.; Sandler, D.P. Pesticide Use and Risk of End-Stage Renal Disease among Licensed Pesticide Applicators in the Agricultural Health Study. Occup. Environ. Med. 2016, 73, 3–12. [Google Scholar] [CrossRef] [Green Version]
- Petejova, N.; Martinek, A.; Zadrazil, J.; Teplan, V. Acute Toxic Kidney Injury. Renal. Fail. 2019, 41, 576–594. [Google Scholar] [CrossRef] [Green Version]
- Agostini, M.; Bianchin, A. Acute Renal Failure from Organophospate Poisoning: A Case of Success with Haemofiltration. Hum. Exp. Toxicol. 2003, 22, 165–167. [Google Scholar] [CrossRef]
- Rubio, C.R.; Felipe Fernández, C.; Manzanedo Bueno, R.; Del Pozo, B.A.; García, J.M. Acute Renal Failure Due to the Inhalation of Organophosphates: Successful Treatment with Haemodialysis. Clin. Kidney J. 2012, 5, 582–583. [Google Scholar] [CrossRef] [Green Version]
- Lee, F.-Y.; Chen, W.-K.; Lin, C.-L.; Lai, C.-Y.; Wu, Y.-S.; Lin, I.-C.; Kao, C.-H. Organophosphate Poisoning and Subsequent Acute Kidney Injury Risk: A Nationwide Population-Based Cohort Study. Medicine 2015, 94, e2107. [Google Scholar] [CrossRef]
- Dinis-Oliveira, R.J.; Duarte, J.A.; Remiao, F.; Sanchez-Navarro, A.; Bastos, M.L.; Carvalho, F. Single high dose dexamethasone treatment decreases the pathological score and increases the survival rate of paraquat-intoxicated rats. Toxicology 2006, 227, 73–85. [Google Scholar] [CrossRef]
- Tayeb, W.; Nakbi, A.; Trabelsi, M.; Miled, A.; Hammami, M. Biochemical and histological evaluation of kidney damage after sub-acute exposure to 2,4-dichlorophenoxyacetic herbicide in rats: Involvement of oxidative stress. Toxicol. Mech. Methods 2012, 22, 696–704. [Google Scholar] [CrossRef] [PubMed]
- Wunnapuk, K.; Liu, X.; Peake, P.; Gobe, G.; Endre, Z.; Grice, J.E.; Roberts, M.S.; Buckley, N.A. Renal biomarkers predict nephrotoxicity after paraquat. Toxicol. Lett. 2013, 222, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Parsons, P.P. Mammalian Toxicokinetics and Toxicity of Chlorothalonil. In Hayes’ Handbook of Pesticide Toxicology; Academic Press: Cambridge, MA, USA, 2010; pp. 1951–1966. [Google Scholar] [CrossRef]
- Ziada, R.M.; Abdulrhman, S.M.; Nahas, A.A. Hepato-nephro-toxicity Induced by Premium Fungicide and Protective Effect of Sesame Oil. Egypt. J. Hosp. Med. 2020, 81, 2445–2450. [Google Scholar] [CrossRef]
- Zhang, W. Global Pesticide Use: Profile, Trend, Cost/Benefit and More. Proc. Int. Acad. Ecol. Environ. Sci. 2018, 8, 1–27. [Google Scholar]
- Pignati, W.A.; Lima, F.A.; Correa, M.L.M.; Barbosa, J.R.; Leão, L.H.; Pignatti, M.G. Spatial distribution of pesticide use in Brazil: A strategy for Health Surveillance. Cienc. Saude Colet. 2017, 22, 3281–3293. [Google Scholar] [CrossRef]
- De Castro, C.N. Agriculture in Brazil’s Midwest Region: Limitations and Future Challenges to Development; Texto Para Discussão: Brasília, Brazil, 2014. [Google Scholar]
- Meyer, A.; Chrisman, J.; Moreira, J.C.; Koifman, S. Cancer Mortality among Agricultural Workers from Serrana Region, State of Rio de Janeiro, Brazil. Environ. Res. 2003, 93, 264–271. [Google Scholar] [CrossRef]
- Meyer, A.; Koifman, S.; Koifman, R.J.; Moreira, J.C.; de Rezende Chrisman, J.; Abreu-Villaca, Y. Mood Disorders Hospitalizations, Suicide Attempts, and Suicide Mortality among Agricultural Workers and Residents in an Area with Intensive Use of Pesticides in Brazil. J. Toxicol. Environ. Health A 2010, 73, 866–877. [Google Scholar] [CrossRef]
- Santana, V.S.; Moura, M.C.P.; Ferreira e Nogueira, F. Occupational pesticide poisoning mortality, 2000-2009, Brazil. Rev. Saude Publica 2013, 47, 598–606. [Google Scholar] [CrossRef] [Green Version]
- Krawczyk, N.; de Souza Espíndola Santos, A.; Lima, J.; Meyer, A. Revisiting Cancer 15 Years Later: Exploring Mortality among Agricultural and Non-agricultural Workers in the Serrana Region of Rio de Janeiro. Am. J. Ind. Med. 2017, 60, 77–86. [Google Scholar] [CrossRef]
- de Boccolini, P.M.M.; Boccolini, C.S.; de Chrisman, J.R.; Koifman, R.J.; Meyer, A. Non-Hodgkin Lymphoma among Brazilian Agricultural Workers: A Death Certificate Case-Control Study. Arch. Environ. Occup. Health 2017, 72, 139–144. [Google Scholar] [CrossRef]
- Nunes, E.P.; da Costa Côrtes, S.; Bivar, W.S.B.; Fortes, L.P.S.; Simões, P.C.M.; Tai, D.W.; Quintslr, M.M.M.; Lima, U.T.; Gadelha, P.; Instituto Brasileiro de Geografia e Estatística-IBGE. Atlas do Espaço Rural Brasileiro, 2nd ed.; IBGE: Rio de Janeiro, Brazil, 2020. Available online: https://biblioteca.ibge.gov.br/visualizacao/livros/liv101773_pre_textual.pdf (accessed on 6 April 2022).
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation Tests for Joinpoint Regression with Applications to Cancer Rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- De Lima, E.E.C.; Queiroz, B.L. Evolution of the Deaths Registry System in Brazil: Associations with Changes in the Mortality Profile, under-Registration of Death Counts, and Ill-Defined Causes of Death. Cad. Saude Publica 2014, 30, 1721–1730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bashir, B.; Sharma, S.G.; Stein, H.D.; Sirota, R.A.; D’Agati, V.D. Acute Kidney Injury Secondary to Exposure to Insecticides Used for Bedbug (Cimex Lectularis) Control. Am. J. Kidney Dis. 2013, 62, 974–977. [Google Scholar] [CrossRef]
- Mohamed, F.; Endre, Z.H.; Buckley, N.A. Role of Biomarkers of Nephrotoxic Acute Kidney Injury in Deliberate Poisoning and Envenomation in Less Developed Countries. Br. J. Clin. Pharmacol. 2015, 80, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Cerdas, M. Chronic Kidney Disease in Costa Rica. Kidney Int. 2005, 68, S31–S33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orantes Navarro, C.M.; Herrera Valdés, R.; López, M.A.; Calero, D.J.; Fuentes de Morales, J.; Alvarado Ascencio, N.P.; Vela Parada, X.F.; Zelaya Quezada, S.M.; Granados Castro, D.V.; Orellana de Figueroa, P. Epidemiological Characteristics of Chronic Kidney Disease of Non-Traditional Causes in Women of Agricultural Communities of El Salvador. Clin. Nephrol. 2015, 83, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Pearce, N.; Caplin, B. Let’s Take the Heat out of the CKDu Debate: More Evidence Is Needed. Occup. Environ. Med. 2019, 76, 357–359. [Google Scholar] [CrossRef] [Green Version]
- Jayatilake, N.; Mendis, S.; Maheepala, P.; Mehta, F.R. Chronic Kidney Disease of Uncertain Aetiology: Prevalence and Causative Factors in a Developing Country. BMC Nephrol. 2013, 14, 180. [Google Scholar] [CrossRef] [Green Version]
- Jayasumana, C.; Paranagama, P.; Agampodi, S.; Wijewardane, C.; Gunatilake, S.; Siribaddana, S. Drinking Well Water and Occupational Exposure to Herbicides Is Associated with Chronic Kidney Disease, in Padavi-Sripura, Sri Lanka. Environ. Health 2015, 14, 6. [Google Scholar] [CrossRef] [Green Version]
- Brandão, A.S.P.; de Rezende, G.C.; da Marques, R.W.C. Crescimento Agrícola No Período 1999/2004: A Explosão Da Soja e Da Pecuária Bovina e Seu Impacto Sobre o Meio Ambiente. Econ. Apl. 2006, 10, 249–266. [Google Scholar] [CrossRef] [Green Version]
- Raina, S.; Hamid, S. Histopathological Effects of Pesticide-Cholopyrifos on Kidney in Albino Rats. Int. J. Res. Med. Sci. 2013, 1, 465–475. [Google Scholar]
- Liu, W.; Du, Y.; Liu, J.; Wang, H.; Sun, D.; Liang, D.; Zhao, L.; Shang, J. Effects of Atrazine on the Oxidative Damage of Kidney in Wister Rats. Int. J. Clin. Exp. Med. 2014, 7, 3235–3243. [Google Scholar] [PubMed]
- Fuentes-Delgado, V.H.; Martínez-Saldaña, M.C.; Rodríguez-Vázquez, M.L.; Reyes-Romero, M.A.; Reyes-Sánchez, J.L.; Jaramillo-Juárez, F. Renal Damage Induced by the Pesticide Methyl Parathion in Male Wistar Rats. J. Toxicol. Environ. Health Part A 2018, 81, 130–141. [Google Scholar] [CrossRef] [PubMed]
- Moyce, S.; Joseph, J.; Tancredi, D.; Mitchell, D.; Schenker, M. Cumulative Incidence of Acute Kidney Injury in California’s Agricultural Workers. J. Occup. Environ. Med. 2016, 58, 391–397. [Google Scholar] [CrossRef] [PubMed]
- García-Trabanino, R.; Jarquín, E.; Wesseling, C.; Johnson, R.J.; González-Quiroz, M.; Weiss, I.; Glaser, J.; Vindell, J.J.; Stockfelt, L.; Roncal, C. Heat Stress, Dehydration, and Kidney Function in Sugarcane Cutters in El Salvador–a Cross-Shift Study of Workers at Risk of Mesoamerican Nephropathy. Environ. Res. 2015, 142, 746–755. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Correa-Rotter, R.; Wesseling, C.; Johnson, R.J. CKD of Unknown Origin in Central America: The Case for a Mesoamerican Nephropathy. Am. J. Kidney Dis. 2014, 63, 506–520. [Google Scholar] [CrossRef]
- Gunatilake, S.; Seneff, S.; Orlando, L. Glyphosate’s Synergistic Toxicity in Combination with Other Factors as a Cause of Chronic Kidney Disease of Unknown Origin. Int. J. Environ. Res. Public Health 2019, 16, 2734. [Google Scholar] [CrossRef] [Green Version]


| Cases | Controls | OR * (95% CI) | OR ** (95% CI) | |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Sex | ||||
| Male | 3215 (53.2) | 1,155,237 (57.5) | 1.00 | 1.00 |
| Female | 2826 (46.8) | 855,142 (42.5) | 1.19 (1.13–1.25) | 1.05 (0.99–1.11) |
| Age at death | ||||
| ≤50 | 539 (8.9) | 409,646 (20.4) | 1.00 | 1.00 |
| 51–70 | 1656 (27.4) | 660,093 (32.8) | 1.91 (1.73–2.10) | 1.90 (1.70–2.13) |
| >70 | 3846 (63.7) | 941,090 (46.8) | 3.11 (2.84–3.40) | 3.07 (2.76–3.42) |
| Region of residence | ||||
| South | 4236 (70.1) | 1,509,866 (75.1) | 1.00 | 1.00 |
| Midwest | 1805 (29.9) | 500,963 (24.9) | 1.28 (1.22–1.36) | 1.37 (1.28–1.47) |
| Race/Ethnicity | ||||
| Non-white | 1416 (23.4) | 502,380 (25.0) | 1.00 | 1.00 |
| White | 4625 (76.6) | 1,508,449 (75.0) | 1.09 (1.03–1.16) | 1.21 (1.11–1.30) |
| Education | ||||
| More than high school | 166 (3.6) | 81,147 (5.3) | 1.00 | 1.00 |
| High school or less | 4413 (96.4) | 1,438,597 (94.7) | 1.50 (1.28–1.75) | 1.30 (1.11–1.52) |
| Occupation *** | ||||
| Non-agricultural workers | 4030 (79.2) | 1,436,019 (83.9) | 1.00 | 1.00 |
| Agricultural workers | 1057 (20.8) | 274,834 (16.1) | 1.37 (1.28–1.47) | 1.32 (1.22–1.42) |
| Cases | Controls | OR * (95% CI) | OR ** (95% CI) | |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Sex | ||||
| Male | ||||
| Non-agricultural workers | 1909 (72.1) | 758,357 (78.9) | 1.00 | 1.00 |
| Agricultural workers | 739 (27.9) | 202,515 (21.1) | 1.45 (1.33–1.58) | 1.27 (1.15–1.39) |
| Female | ||||
| Non-agricultural workers | 2121 (87.0) | 677,551 (90.4) | 1.00 | 1.00 |
| Agricultural workers | 318 (13.0) | 72,307 (9.6) | 1.41 (1.25–1.58) | 1.40 (1.23–1.59) |
| Age at death | ||||
| ≤50 | ||||
| Non-agricultural workers | 369 (86.4) | 296,921 (89.2) | 1.00 | 1.00 |
| Agricultural workers | 58 (13.6) | 35,774 (10.8) | 1.31 (0.99–1.72) | 1.56 (1.16–2.11) |
| 51–70 | ||||
| Non-agricultural workers | 1147(83.4) | 474,278 (84.7) | 1.00 | 1.00 |
| Agricultural workers | 229 (16.6) | 85,743 (15.3) | 1.10 (0.96–1.27) | 1.13 (0.97–1.32) |
| >70 | ||||
| Non-agricultural workers | 2514 (76.6) | 664,820 (81.3) | 1.00 | 1.00 |
| Agricultural workers | 770 (23.4) | 153,317 (18.7) | 1.33 (1.23–1.44) | 1.36 (1.25–1.49) |
| Region of residence | ||||
| South | ||||
| Non-agricultural workers | 2851 (77.4) | 1,098,465 (83.7) | 1.00 | 1.00 |
| Agricultural workers | 831 (22.6) | 214,252 (16.3) | 1.49 (1.38–1.62) | 1.40 (1.29–1.53) |
| Midwest | ||||
| Non-agricultural workers | 1179 (83.9) | 337,554 (84.8) | 1.00 | 1.00 |
| Agricultural workers | 226 (16.1) | 60,582 (15.2) | 1.07 (0.93–1.23) | 1.06 (0.90–1.25) |
| Race/Ethnicity | ||||
| Non-white | ||||
| Non-agricultural workers | 908 (82.7) | 342,478 (84.4) | 1.00 | 1.00 |
| Agricultural workers | 190 (17.3) | 63,539 (15.6) | 1.13 (0.96–1.32) | 1.12 (0.94–1.34) |
| White | ||||
| Non-agricultural workers | 3122 (78.3) | 1,093,541 (83.8) | 1.00 | 1.00 |
| Agricultural workers | 867 (21.7) | 211,295 (16.2) | 1.44 (1.33–1.55) | 1.37 (1.26–1.49) |
| Education *** | ||||
| More than high school | ||||
| Non-agricultural workers | 146 (96.7) | 71,879 (98.1) | 1.00 | 1.00 |
| Agricultural workers | 5 (3.3) | 1390 (1.9) | 1.77 (0.73–4.33) | 1.82 (0.74–4.46) |
| High school or less | ||||
| Non-agricultural workers | 3036 (76.3) | 1,051,486 (81.6) | 1.00 | 1.00 |
| Agricultural workers | 941 (23.7) | 237,012 (18.4) | 1.38 (1.28–1.48) | 1.32 (1.22–1.42) |
| Cases | Controls | OR * (95% CI) | OR ** (95% CI) | |
|---|---|---|---|---|
| N (%) | N (%) | |||
| Age | ||||
| 20–29 | ||||
| Non-agricultural workers | 50 (83.3) | 72,588 (92.3) | 1.00 | 1.00 |
| Agricultural workers | 10 (16.7) | 6024 (7.7) | 2.41 (1.22–4.75) | 3.07 (1.71–6.26) |
| 30–39 | ||||
| Non-agricultural workers | 92 (82.5) | 81,309 (89.7) | 1.00 | 1.00 |
| Agricultural workers | 16 (14.8) | 9349 (10.3) | 1.51 (0.89–2.57) | 1.57 (0.84–2.91) |
| 40–49 | ||||
| Non-agricultural workers | 196 (87.9) | 126,365 (87.6) | 1.00 | 1.00 |
| Agricultural workers | 27 (12.1) | 17,886 (12.4) | 0.97 (0.65–1.46) | 1.25 (0.81–1.93) |
| 50–59 | ||||
| Non-agricultural workers | 430 (86.7) | 196,179 (85.9) | ||
| Agricultural workers | 66 (13.3) | 32,237 (14.1) | 0.93 (0.72–1.21) | 0.95 (0.71–1.26) |
| 60–69 | ||||
| Non-agricultural workers | 671 (82.4) | 264,325 (84.2) | 1.00 | 1.00 |
| Agricultural workers | 143 (17.6) | 49,687 (15.8) | 1.13 (0.95–1.36) | 1.16 (0.95–1.41) |
| 70–79 | ||||
| Non-agricultural workers | 1049 (76.1) | 326,149 (81.7) | 1.00 | 1.00 |
| Agricultural workers | 329 (23.9) | 72,913 (18.3) | 1.40 (1.24–1.59) | 1.42 (1.24–1.63) |
| 80+ | ||||
| Non-agricultural workers | 1542 (76.8) | 369,104 (81.0) | 1.00 | 1.00 |
| Agricultural workers | 466 (23.2) | 86,738 (19.0) | 1.29 (1.16–1.43) | 1.31 (1.17–1.47) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meyer, A.; Santos, A.S.E.; Asmus, C.I.R.F.; Camara, V.M.; Costa, A.J.L.; Sandler, D.P.; Parks, C.G. Acute Kidney Failure among Brazilian Agricultural Workers: A Death-Certificate Case-Control Study. Int. J. Environ. Res. Public Health 2022, 19, 6519. https://doi.org/10.3390/ijerph19116519
Meyer A, Santos ASE, Asmus CIRF, Camara VM, Costa AJL, Sandler DP, Parks CG. Acute Kidney Failure among Brazilian Agricultural Workers: A Death-Certificate Case-Control Study. International Journal of Environmental Research and Public Health. 2022; 19(11):6519. https://doi.org/10.3390/ijerph19116519
Chicago/Turabian StyleMeyer, Armando, Aline Souza Espindola Santos, Carmen Ildes Rodrigues Froes Asmus, Volney Magalhaes Camara, Antônio José Leal Costa, Dale P. Sandler, and Christine Gibson Parks. 2022. "Acute Kidney Failure among Brazilian Agricultural Workers: A Death-Certificate Case-Control Study" International Journal of Environmental Research and Public Health 19, no. 11: 6519. https://doi.org/10.3390/ijerph19116519
APA StyleMeyer, A., Santos, A. S. E., Asmus, C. I. R. F., Camara, V. M., Costa, A. J. L., Sandler, D. P., & Parks, C. G. (2022). Acute Kidney Failure among Brazilian Agricultural Workers: A Death-Certificate Case-Control Study. International Journal of Environmental Research and Public Health, 19(11), 6519. https://doi.org/10.3390/ijerph19116519