Utilization of Postnatal Care Services among Thai Women during the COVID-19 Pandemic: Results of a Web-Based Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Variable Measures
2.3. Statistical Analyses
3. Results
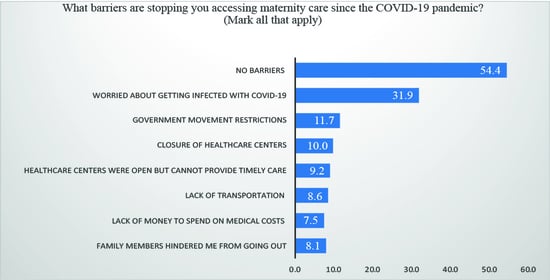
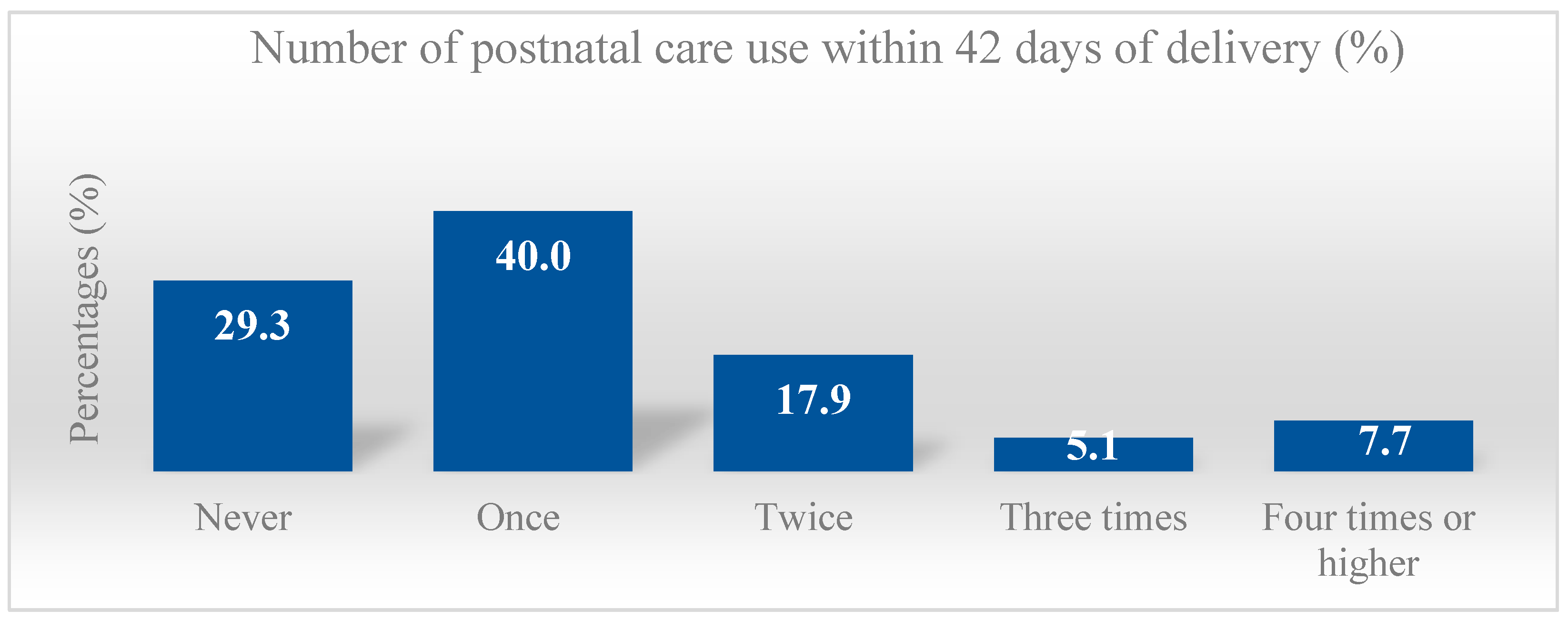
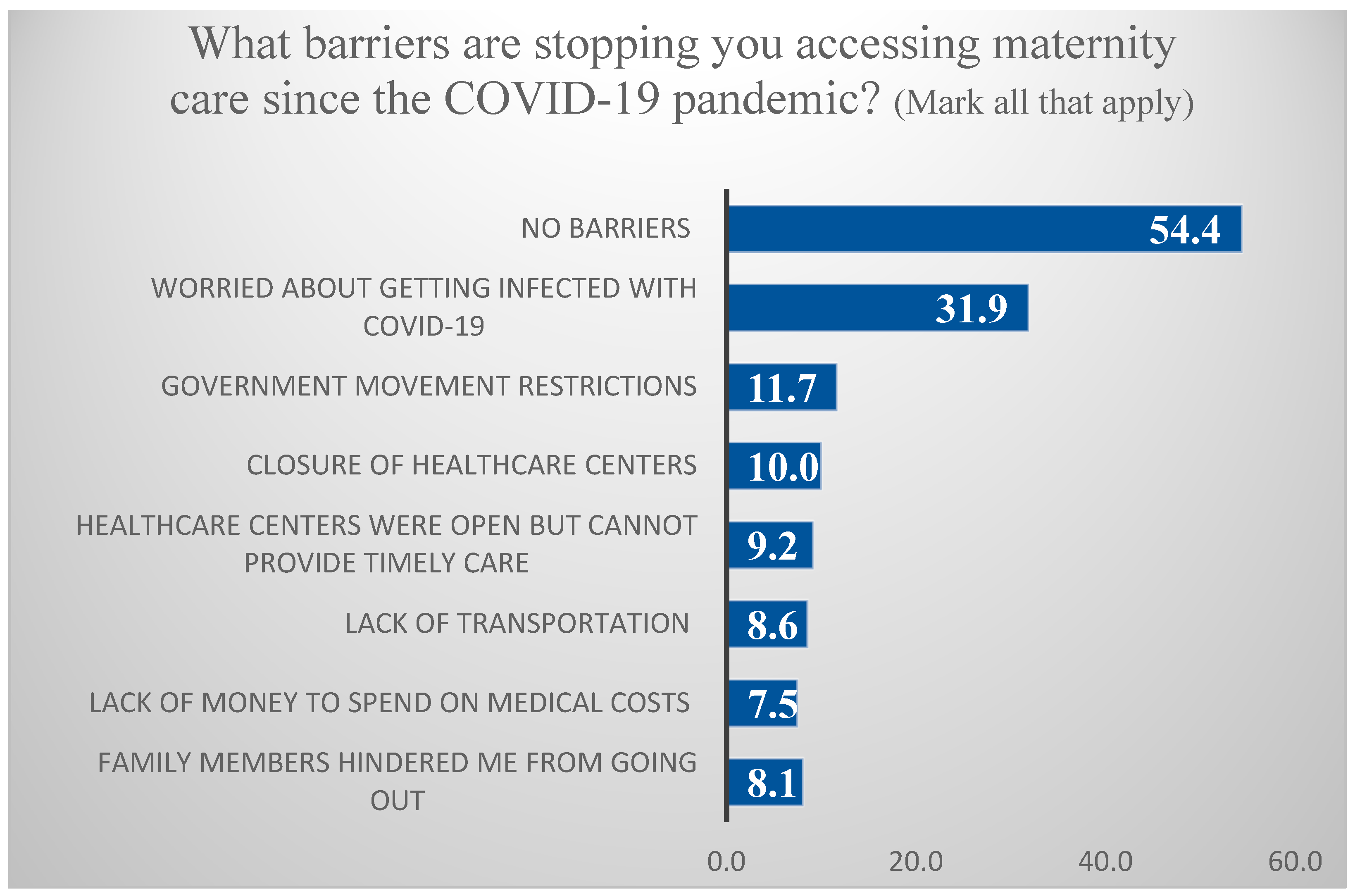
3.1. Percentage of Postnatal Care Uptake and Barriers to Accessing Postnatal Care Services
3.2. General Characteristics of the Study Subjects
3.3. Bivariate Associations between Independent Factors and Postnatal Care Uptake
3.4. Multivariate Association with Postnatal Care Uptake
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization; United Nations Children’s Fund; World Bank Group. Nurturing Care for Early Childhood Development: A Framework for Helping Children Survive and Thrive to Transform Health and Human Potential; World Health Organization: Geneva, Switzerland, 2018.
- Ronsmans, C.; Lancet Maternal Survival Series Steering Group. Maternal mortality: Who, when, where, and why. Lancet 2006, 368, 1189–1200. [Google Scholar] [CrossRef]
- Wudineh, K.G.; Nigusie, A.A.; Gesese, S.S.; Tesu, A.A.; Beyene, F.Y. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, Northwest Ethiopia: A community-based cross-sectional study. BioMec Cent. Pregnancy Childbirth 2018, 18, 508. [Google Scholar]
- Countdown Coverage Writing Group; Countdown to 2015 Core Group; Daelmans, B.; Dwivedi, A.; Fauveau, V.; Lawn, J.E.; Mason, E.; Newby, H.; Shankar, A.; Starrs, A.; et al. Countdown to 2015 for maternal, newborn, and child survival: The 2008 report on tracking coverage of interventions. Lancet 2008, 371, 1247–1258. [Google Scholar]
- Countdown to 2030 Collaboration. Countdown to 2030: Tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet 2018, 391, 1538–1548. [CrossRef]
- Sacks, E.; Langlois, E.V. Postnatal care: Increasing coverage, equity, and quality. Lancet Glob. Health 2016, 4, e442–e443. [Google Scholar] [CrossRef] [Green Version]
- Roberton, T.; Carter, E.D.; Chou, V.B.; Stegmuller, A.R.; Jackson, B.D.; Tam, Y.; Sawadogo-Lewis, T.; Walker, N. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: A modelling study. Lancet Glob. Health 2020, 8, e901–e908. [Google Scholar] [CrossRef]
- Townsend, R.; Chmielewska, B.; Barratt, I.; Kalafat, E.; van der Meulen, J.; Gurol-Urganci, I.; O’Brien, P.; Morris, E.; Draycott, T.; Thangaratinam, S.; et al. Global changes in maternity care provision during the COVID-19 pandemic: A systematic review and meta-analysis. eClinicalMedicine 2021, 37, 100947. [Google Scholar] [CrossRef]
- Cameron, E.S.; Ramos, H.; Aston, M.; Kuri, M.; Jackson, L. “COVID affected us all:” the birth and postnatal health experiences of resettled Syrian refugee women during COVID-19 in Canada. BioMed Cent. 2021, 18, 256. [Google Scholar]
- Ombere, S.O. Access to maternal health services during the COVID-19 pandemic: Experiences of indigent mothers and health care providers in Kilifi County, Kenya. Front. Sociol. 2021, 6, 613042. [Google Scholar] [CrossRef]
- Oluoch-Aridi, J.; Chelagat, T.; Nyikuri, M.M.; Onyango, J.; Guzman, D.; Makanga, C.; Miller-Graff, L.; Dowd, R. COVID-19 effect on access to maternal health services in Kenya. Front. Glob. Womens Health 2020, 1, 599267. [Google Scholar] [CrossRef]
- Irvine, I.C.; Chisnall, G.; Vindrola-Padros, C. The Impact of Maternity Service Restrictions Related to COVID-19 on Women’s Experiences of Giving Birth in England during the Pandemic: A Qualitative Study and Policy Review. Res. Square 2022. [Google Scholar] [CrossRef]
- Gebreegziabher, S.B.; Marrye, S.S.; Kumssa, T.H.; Merga, K.H.; Feleke, A.K.; Dare, D.J.; Hallstrom, I.K.; Yimer, S.A.; Shargie, M.B. Assessment of maternal and child health care services performance in the context of COVID-19 pandemic in Addis Ababa, Ethiopia: Evidence from routine service data. Reprod. Health 2022, 19, 42. [Google Scholar] [CrossRef] [PubMed]
- Mhajabin, S.; Hossain, A.T.; Nusrat, N.; Jabeen, S.; Ameen, S.; Banik, G.; Tahsina, T.; Ahmed, A.; Rahman, Q.S.; Gurley, E.S.; et al. Indirect effects of the early phase of the COVID-19 pandemic on the coverage of essential maternal and newborn health services in a rural subdistrict in Bangladesh: Results from a cross-sectional household survey. Br. Med. J. 2022, 12, e056951. [Google Scholar] [CrossRef]
- Jardine, J.; Relph, S.; Magee, L.A.; von Dadelszen, P.; Morris, E.; Ross-Davie, M.; Draycott, T.; Khalil, A. Maternity services in the UK during the coronavirus disease 2019 pandemic: A national survey of modifications to standard care. BJOG 2021, 128, 880–889. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. How a Strong Health System Fights a Pandemic; World Health Organization: Geneva, Switzerland, 2020.
- Oxford Policy Management. Social Impact Assessment of COVID-19 in Thailand; Oxford Policy Management: Oxford, UK, 2020. [Google Scholar]
- Thailand: Overview. Johns Hopkins University & Medicine. Available online: https://coronavirus.jhu.edu/region/thailand (accessed on 20 March 2022).
- Kanchanachitra, C.; Kanchanachitra, M.; Apipornchaisakul, K. Thai Health 2017: Empowering Vulnerable Populations Creating an Inclusive Society; Institute for Population and Social Research, Mahidol University: Nakhon Pathom, Thailand, 2017. [Google Scholar]
- Topothai, C.; Chaweewan, T. Maternal and Child Health: Benefit Package under the Thai Universal Health Coverage; Department of Health, Ministry of Public Health: Nonthaburi, Thailand, 2018.
- National Statistical Office; United Nations Children’s Fund. Thailand Multiple Indicator Cluster Survey 2015–2016; NSO and UNICEF: Bangkok, Thailand, 2016. [Google Scholar]
- Lee, R.W.K.; Loy, S.L.; Yang, L.; Chan, J.K.Y.; Tan, L.K. Attitudes and precaution practices towards COVID-19 among pregnant women in Singapore: A cross-sectional survey. BMC Pregnancy Childbirth 2020, 20, 675. [Google Scholar] [CrossRef]
- Ayele, A.D.; Mihretie, G.N.; Belay, H.G.; Teffera, A.G.; Kassa, B.G.; Amsalu, B.T. Knowledge and Practice to Prevent against Corona Virus Disease (COVID-19) and Its Associated Factors among Pregnant Women in Debre Tabor Town Northwest Ethiopia: A Community Based Cross-Sectional Study. BMC Pregnancy Childbirth. 2021, 21, 397. [Google Scholar] [CrossRef]
- Anikwe, C.C.; Ogah, C.O.; Anikwe, I.H.; Okorochukwu, B.C.; Ikeoha, C.C. Coronavirus disease 2019: Knowledge, attitude, and practice of pregnant women in a tertiary hospital in Abakaliki, southeast Nigeria. Int. J. Gynecol. Obstet. 2020, 151, 197–202. [Google Scholar] [CrossRef]
- Bureau of Health Service System Development. Manual of Primary Health Care Unit Standard Evaluation and Quality Assurance; Department of Health Service Support, Ministry of Public Health: Nonthaburi, Thailand, 2003.
- Pothisiri, W. Postpartum Care in Thailand: Experience, Practice and Policy; Department of Social Policy, The London School of Economics and Political Science: London, UK, 2010. [Google Scholar]
- Ministry of Public Health; World Health Organization. Thailand Reproductive Health Profile; Department of Health, Ministry of Public Health: Nonthaburi, Thailand; Regional Office for Southeast Asia: New Delhi, India; The World Health Organization: Geneva, Switzerland, 2003.
- National Statistical Office. The Reproductive Health Survey 2009. National Statistical Office, Bangkok. 2010. Available online: http://www.nso.go.th/sites/2014en/Survey/social/health/reproductive/2009/6.%20Full%20Report.pdf (accessed on 20 March 2022).
- The Pandemic Has Pushed Women Out of Work. These Policies Can Help. Available online: https://blogs.adb.org/blog/pandemic-has-pushed-women-out-work-these-policies-can-help (accessed on 10 March 2022).
- Against the Odds: Stories from Women in Thailand during COVID-19. Available online: https://asiapacific.unwomen.org/en/news-and-events/stories/2020/06/against-the-odds-stories-from-women-in-thailand-during-covid19 (accessed on 15 February 2022).
- Thailand Launches “New Normal” Healthcare System to Build Back Better after COVID-19. Available online: https://www.who.int/thailand/news/feature-stories/detail/thailand-launches-new-normal-healthcare-system-to-build-back-better-after-covid-19 (accessed on 10 February 2022).
- Jongudomsuk, P.; Srithamrongsawat, S.; Patcharanarumol, W.; Limwattananon, S.; Pannarunothai, S.; Vapatanavong, P.; Sawaengdee, K.; Fahamnuaypol, P. The Kingdom of Thailand Health System Review; WHO Regional Office for the Western Pacific: Manila, Philippines, 2015. [Google Scholar]
- Sahoo, K.C.; Negi, S.; Patel, K.; Mishra, B.K.; Palo, S.K.; Pati, S. Challenges in Maternal and Child Health Services Delivery and Access during Pandemics or Public Health Disasters in Low-and Middle-Income Countries: A Systematic Review. Healthcare 2021, 9, 828. [Google Scholar] [CrossRef]
- Fort, A.L.; Kothari, M.T. Postpartum Care. Levels and Determinants in Developing Countries, MEASURE DHS (Demographic and Health Surveys); Macro International: Calverton, MD, USA, 2006. [Google Scholar]
- Impact of COVID-19 on Thailand’s Households—Insights from a Rapid Phone Survey. Available online: https://blogs.worldbank.org/eastasiapacific/impact-covid-19-thailands-households-insights-rapid-phone-survey (accessed on 7 March 2022).
- Temesgen, K.; Wakgari, N.; Debelo, B.T.; Tafa, B.; Alemu, G.; Wondimu, F.; Gudisa, T.; Gishile, T.; Daba, G.; Bulto, G.A.; et al. Maternal health care services utilization amidst the COVID-19 pandemic in West Shoa zone, Central Ethiopia. PLoS ONE 2021, 16, e0249214. [Google Scholar] [CrossRef]
- Banke-Thomas, A.; Semaan, A.; Amongin, D.; Babah, O.; Dioubate, N.; Kikula, A.; Nakubulwa, S.; Ogein, O.; Adroma, M.; Anzo Adiga, W.; et al. A mixed-methods study of maternal health care utilisation in six referral hospitals in four sub-Saharan African countries before and during the COVID-19 pandemic. BMJ Glob. Health 2022, 7, e008064. [Google Scholar] [CrossRef]
- Balogun, M.; Banke-Thomas, A.; Sekoni, A.; Boateng, G.O.; Yesufu, V.; Wright, O.; Ubani, O.; Abayomi, A.; Afolabi, B.B.; Ogunsola, F. Challenges in access and satisfaction with reproductive, maternal, newborn and child health services in Nigeria during the COVID-19 pandemic: A cross-sectional survey. PLoS ONE 2021, 16, e0251382. [Google Scholar] [CrossRef] [PubMed]
- Pant, S.; Koirala, S.; Subedi, M. Access to maternal health services during COVID-19. Eur. J. Med. Sci. 2020, 2, 46–50. [Google Scholar] [CrossRef]
- Bar-Zeev, S.; Breen-Kamkong, C. COVID-19 Technical Brief Package for Maternity Services Part 1: Delivery of Facility Based Maternity Services-Interim Guidance; UNFPA: New York, NY, USA, 2020. [Google Scholar]
- Bilimoria, K.Y.Z.T.; Durst, D.A.; Merkow, R.P.; Sama, P.R.; Bahaveolos, S.A.; Chrisman, H.B. Comparison of Patient Experience with Telehealth vs. In-Person Visits before and during the COVID-19 Pandemic. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 533–536. [Google Scholar] [CrossRef] [PubMed]
| Total | Number of Postnatal Care Uptakes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <2 | ≥2 | <3 | ≥3 | Never | 1 | 2 | 3 | ≥4 | ||||||
| n | (%) | % | % | p-Value | % | % | p-Value | % | % | % | % | % | p-Value | |
| Total number | 840 | (100) | 69.3 | 30.7 | 87.1 | 12.9 | 29.3 | 40.0 | 17.9 | 5.1 | 7.7 | |||
| Mother’s age (years) | ||||||||||||||
| 18–29 | 489 | (58.2) | 60.3 | 53.5 | 0.0645 | 58.6 | 55.6 | 0.5484 | 62.2 | 58.9 | 52.0 | 51.2 | 58.5 | 0.2940 |
| 30–49 | 351 | (41.8) | 39.7 | 46.5 | 41.4 | 44.4 | 37.8 | 41.1 | 48.0 | 48.8 | 41.5 | |||
| Education of mother (secondary school or lower) | 458 | (54.5) | 58.4 | 45.7 | 0.0007 | 55.1 | 50.9 | 0.4212 | 57.3 | 59.2 | 42.0 | 39.6 | 58.5 | 0.0015 |
| Marital status (married) | 759 | (90.4) | 89.7 | 91.9 | 0.3257 | 90.2 | 91.7 | 0.6214 | 91.5 | 88.4 | 92.0 | 93.0 | 90.8 | 0.6160 |
| Working status | ||||||||||||||
| Waged/employed | 252 | (30.0) | 29.9 | 30.2 | 0.0028 | 29.8 | 31.5 | 0.1086 | 28.1 | 31.3 | 29.3 | 27.9 | 33.9 | 0.0791 |
| Self-employed/family business | 105 | (12.5) | 10.0 | 18.2 | 11.7 | 17.6 | 9.8 | 10.1 | 18.7 | 23.3 | 13.9 | |||
| On maternity leave | 171 | (20.4) | 20.1 | 20.9 | 19.9 | 23.1 | 22.8 | 18.2 | 19.3 | 20.9 | 24.6 | |||
| Housewife/unemployed | 312 | (37.1) | 40.0 | 30.6 | 38.5 | 27.8 | 39.4 | 40.5 | 32.7 | 27.9 | 27.7 | |||
| Region | ||||||||||||||
| Central (incl. Bangkok) | 308 | (36.7) | 34.9 | 40.7 | 0.1280 | 36.5 | 38.0 | 0.5515 | 35.0 | 34.8 | 42.7 | 41.9 | 35.4 | 0.0685 |
| North/Northeast | 105 | (12.5) | 13.8 | 9.7 | 13.0 | 9.3 | 9.4 | 17.0 | 10.0 | 4.7 | 12.3 | |||
| South | 427 | (50.8) | 51.4 | 49.6 | 50.5 | 52.8 | 55.7 | 48.2 | 47.3 | 53.5 | 52.3 | |||
| Residence (urban) | 382 | (45.5) | 42.4 | 52.3 | 0.0079 | 43.6 | 58.3 | 0.0040 | 45.5 | 40.2 | 48.0 | 65.1 | 53.9 | 0.0128 |
| Intended pregnancy (yes) | 705 | (83.9) | 83.5 | 84.9 | 0.6158 | 83.6 | 86.1 | 0.5082 | 85.8 | 81.9 | 84.0 | 86.1 | 86.2 | 0.7204 |
| Number of children (one child) | 495 | (58.9) | 59.6 | 57.4 | 0.5400 | 58.3 | 63.0 | 0.9906 | 61.8 | 58.0 | 53.3 | 69.8 | 58.5 | 0.2898 |
| Birth interval | ||||||||||||||
| No sibling | 436 | (51.9) | 52.6 | 50.4 | 0.3113 | 51.9 | 51.9 | 0.1330 | 52.4 | 52.7 | 49.3 | 58.1 | 47.7 | 0.3010 |
| Less than three years | 102 | (12.1) | 11.0 | 14.7 | 11.3 | 17.6 | 13.0 | 9.5 | 12.7 | 20.9 | 15.4 | |||
| Three years or higher | 302 | (36.0) | 36.4 | 34.9 | 36.7 | 30.6 | 34.6 | 37.8 | 38.0 | 20.9 | 36.9 | |||
| Delivery mode (Caesarean section) | 351 | (41.8) | 37.1 | 52.3 | <0.0001 | 41.0 | 47.2 | 0.2198 | 35.4 | 38.4 | 56.0 | 32.6 | 56.9 | <0.0001 |
| Preterm delivery (less than 37 weeks) | 173 | (20.6) | 21.3 | 19.0 | 0.4443 | 20.8 | 19.4 | 0.7514 | 24.8 | 18.8 | 18.7 | 16.3 | 21.5 | 0.3769 |
| Low birth weight (<2.5 kg) | 81 | (9.6) | 9.8 | 9.3 | 0.8238 | 9.6 | 10.2 | 0.8379 | 10.6 | 9.2 | 8.7 | 4.65 | 13.85 | 0.5543 |
| Health problems during delivery (yes) | 98 | (11.7) | 10.5 | 14.3 | 0.1079 | 10.8 | 17.6 | 0.0399 | 12.2 | 9.2 | 12.0 | 14.0 | 20.0 | 0.1572 |
| Health problems during postpartum (yes) | 73 | (8.7) | 8.8 | 8.5 | 0.9109 | 8.7 | 8.3 | 0.8878 | 11.0 | 7.1 | 8.7 | 7.0 | 9.2 | 0.5890 |
| Total | Number of Postnatal Care Uptakes | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <2 | ≥2 | <3 | ≥3 | Never | 1 | 2 | 3 | ≥4 | ||||||
| n | (%) | (%) | (%) | p-Value | (%) | (%) | p-Value | (%) | (%) | (%) | (%) | (%) | p-Value | |
| COVID-19-related factors | ||||||||||||||
| Family income during the COVID-19 pandemic | ||||||||||||||
| 1st tertile (low) | 278 | (33.3) | 34.8 | 29.8 | 0.0200 | 34.3 | 26.2 | 0.1200 | 41.1 | 30.2 | 32.4 | 23.8 | 27.7 | 0.0171 |
| 2nd tertile | 309 | (37.0) | 38.4 | 33.7 | 37.0 | 36.4 | 32.9 | 42.4 | 31.8 | 33.3 | 38.5 | |||
| 3rd tertile (high) | 249 | (29.8) | 26.9 | 36.5 | 28.7 | 37.4 | 26.0 | 27.5 | 35.8 | 42.9 | 33.9 | |||
| Food insecurity before and during COVID-19 | ||||||||||||||
| No change (insecure–insecure) | 236 | (28.1) | 29.2 | 25.6 | 0.2720 | 28.8 | 23.1 | 0.3624 | 29.3 | 29.2 | 27.3 | 20.9 | 24.6 | 0.8660 |
| Worse (secure–insecure) | 180 | (21.4) | 22.2 | 19.8 | 21.6 | 20.4 | 23.2 | 21.4 | 19.3 | 18.6 | 21.5 | |||
| Better or no change (secure–secure) | 424 | (50.5) | 48.6 | 54.7 | 49.6 | 56.5 | 47.6 | 49.4 | 53.3 | 60.5 | 53.9 | |||
| Worried about COVID-19 infection | ||||||||||||||
| A little worried/Not at all | 299 | (35.6) | 34.2 | 38.8 | 0.0070 | 34.4 | 43.5 | 0.1452 | 28.5 | 38.4 | 35.3 | 48.8 | 40.0 | 0.0077 |
| Moderately worried | 199 | (23.7) | 21.6 | 28.3 | 23.8 | 23.1 | 24.8 | 19.4 | 32.0 | 18.6 | 26.2 | |||
| Very worried/Extremely worried | 342 | (40.7) | 44.2 | 32.9 | 41.8 | 33.3 | 46.8 | 42.3 | 32.7 | 32.6 | 33.9 | |||
| Ever diagnosed as COVID-19 positive (yes) | 143 | (17.0) | 47.0 | 18.2 | 0.5401 | 17.1 | 16.7 | 0.9158 | 18.7 | 14.9 | 19.3 | 11.6 | 20.0 | 0.4869 |
| Ever taken a COVID-19 vaccine (yes) | 469 | (55.8) | 52.9 | 62.4 | 0.0107 | 54.8 | 63.0 | 0.1100 | 50.0 | 55.1 | 62.0 | 74.4 | 55.4 | 0.0188 |
| COVID-19-related KAP | ||||||||||||||
| COVID-19-related knowledge | ||||||||||||||
| 1st tertile (low) | 321 | (38.2) | 40.9 | 32.2 | 0.0270 | 39.1 | 32.4 | 0.0060 | 43.5 | 39.0 | 32.0 | 23.3 | 38.5 | 0.0117 |
| 2nd tertile | 166 | (19.8) | 19.9 | 19.4 | 20.9 | 12.0 | 17.1 | 22.0 | 24.7 | 14.0 | 10.8 | |||
| 3rd tertile (high) | 353 | (42.0) | 39.2 | 48.4 | 40.0 | 55.6 | 39.4 | 39.0 | 43.3 | 62.8 | 50.8 | |||
| COVID-19-related attitude | ||||||||||||||
| 1st tertile (low) | 236 | (28.1) | 28.4 | 27.5 | 0.3710 | 29.4 | 19.4 | 0.0281 | 28.9 | 28.0 | 33.3 | 16.3 | 21.5 | 0.1881 |
| 2nd tertile | 364 | (43.3) | 44.5 | 40.7 | 43.4 | 42.6 | 46.8 | 42.9 | 39.3 | 41.9 | 43.1 | |||
| 3rd tertile (high) | 240 | (28.6) | 27.1 | 31.8 | 27.2 | 38.0 | 24.4 | 29.2 | 27.3 | 41.9 | 35.4 | |||
| COVID-19-related practice | ||||||||||||||
| 1st tertile (low) | 275 | (32.7) | 35.2 | 27.1 | 0.0590 | 33.3 | 28.7 | 0.5590 | 37.4 | 33.6 | 26.0 | 32.6 | 26.2 | 0.4095 |
| 2nd tertile | 279 | (33.2) | 31.4 | 37.2 | 32.7 | 37.0 | 32.1 | 31.0 | 37.3 | 37.2 | 36.9 | |||
| 3rd tertile (high) | 286 | (34.0) | 33.3 | 35.7 | 34.0 | 34.3 | 30.5 | 35.4 | 36.7 | 30.2 | 36.9 | |||
| Binary (≥2) | Binary (≥3) | Ordinal | ||||
|---|---|---|---|---|---|---|
| AOR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) | |
| Maternal age (18–29 vs. 30–49 years) | 1.00 | (0.71–1.40) | ||||
| Education of mother (secondary school or lower) | 0.81 | (0.56–1.16) | 0.98 | (0.73–1.32) | ||
| Working status | ||||||
| Waged/employed vs. unemployed | 1.01 | (0.67–1.52) | 1.06 | (0.76–1.47) | ||
| Self-employed/family business vs. unemployed | 1.96 | (1.20–3.20) | 1.58 | (1.04–2.39) | ||
| On maternity leave vs. unemployed | 0.88 | (0.55–1.41) | 0.83 | (0.57–1.21) | ||
| Region | ||||||
| North/Northeast vs. Central | 1.09 | (0.82–1.47) | ||||
| South vs. Central | 1.02 | (0.68–1.53) | ||||
| Health problems during delivery (yes vs. no) | 1.67 | (0.95–2.92) | ||||
| Residence (urban vs. rural) | 1.45 | (1.06–2.00) | 1.69 | (1.12–2.57) | 1.21 | (0.93–1.58) |
| Delivery mode (Caesarean section vs. vaginal) | 1.86 | (1.34–2.57) | 1.59 | (1.22–2.08) | ||
| COVID-19-related factors | ||||||
| Family income during the COVID-19 pandemic | ||||||
| Middle vs. Low | 0.85 | (0.57–1.25) | 1.20 | (0.87–1.64) | ||
| High vs. low | 1.08 | (0.70–1.69) | 1.30 | (0.89–1.90) | ||
| Worried about COVID-19 infection | ||||||
| Not at all/A little vs. very/extremely worried | 1.66 | (1.15–2.39) | 1.74 | (1.30–2.33) | ||
| Moderately vs. very/extremely worried | 1.64 | (1.10–2.45) | 1.32 | (0.96–1.83) | ||
| Ever taken a COVID-19 vaccine (yes vs. no) | 0.79 | (0.56–1.10) | 0.80 | (0.61–1.04) | ||
| COVID-19-related KAP | ||||||
| COVID-19-related knowledge | ||||||
| Middle vs. Low | 1.29 | (0.83–2.01) | 0.63 | (0.32–1.23) | 1.42 | (1.00–2.01) |
| High vs. low | 1.23 | (0.85–1.78) | 1.42 | (0.89–2.25) | 1.30 | (0.97–1.75) |
| COVID-19-related attitude | ||||||
| Middle vs. Low | 1.35 | (0.77–2.34) | ||||
| High vs. low | 1.90 | (1.07–3.39) | ||||
| COVID-19-related practice | ||||||
| Middle vs. Low | 1.30 | (0.88–1.93) | ||||
| High vs. low | 1.20 | (0.81–1.78) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aye, Y.M.; Kim, S.J.; Suriyawongpaisal, W.; Hong, S.A.; Chang, Y.-S. Utilization of Postnatal Care Services among Thai Women during the COVID-19 Pandemic: Results of a Web-Based Survey. Int. J. Environ. Res. Public Health 2022, 19, 6536. https://doi.org/10.3390/ijerph19116536
Aye YM, Kim SJ, Suriyawongpaisal W, Hong SA, Chang Y-S. Utilization of Postnatal Care Services among Thai Women during the COVID-19 Pandemic: Results of a Web-Based Survey. International Journal of Environmental Research and Public Health. 2022; 19(11):6536. https://doi.org/10.3390/ijerph19116536
Chicago/Turabian StyleAye, Yin Min, Soo Jung Kim, Wichukorn Suriyawongpaisal, Seo Ah Hong, and Yan-Shing Chang. 2022. "Utilization of Postnatal Care Services among Thai Women during the COVID-19 Pandemic: Results of a Web-Based Survey" International Journal of Environmental Research and Public Health 19, no. 11: 6536. https://doi.org/10.3390/ijerph19116536
APA StyleAye, Y. M., Kim, S. J., Suriyawongpaisal, W., Hong, S. A., & Chang, Y.-S. (2022). Utilization of Postnatal Care Services among Thai Women during the COVID-19 Pandemic: Results of a Web-Based Survey. International Journal of Environmental Research and Public Health, 19(11), 6536. https://doi.org/10.3390/ijerph19116536