Health Literacy Level and Comprehension of Prescription and Nonprescription Drug Information
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Survey Instrument and Data Collection
2.3. Measurements of Health Literacy
2.4. Measuring Amounts of Reading Information on OTC Drug Labels
2.5. Statistical Analysis
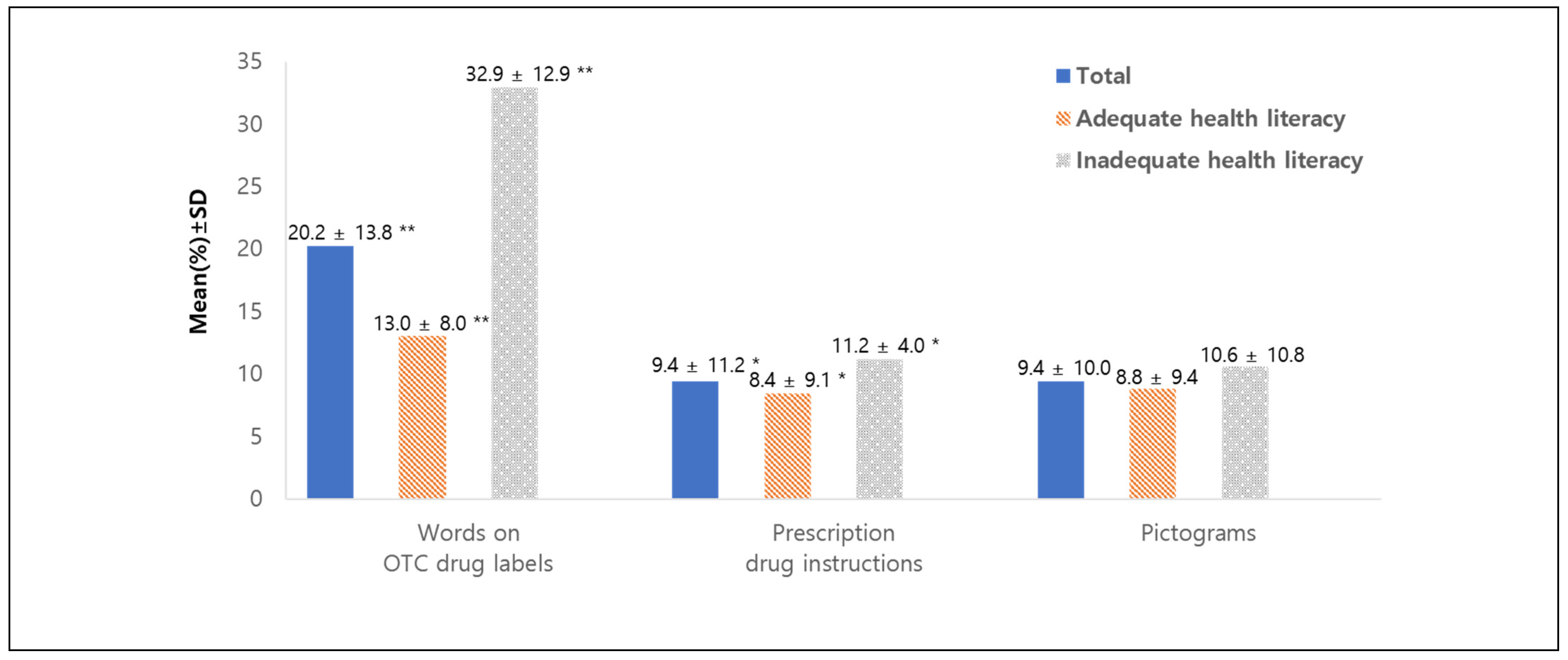
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mullen, R.J.; Curtis, L.M.; O’Conor, R.; Serper, M.; McCarthy, D.; Bailey, S.C.; Parker, R.M.; Wolf, M.S. Visual acuity, literacy, and unintentional misuse of nonprescription medications. Am. J. Health Syst. Pharm. 2018, 75, e213–e220. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.; Conn, K.M.; Zak, M. Evaluation of over-the-counter medication knowledge and literacy in adolescent students. Acad. Pediatrics 2018, 18, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Whittaker, C.F.; Tom, S.E.; Bivens, A.; Klein-Schwartz, W. Evaluation of an educational intervention on knowledge and awareness of medication safety in older adults with low health literacy. Am. J. Health Ed. 2017, 48, 100–107. [Google Scholar] [CrossRef]
- Chun, S.Y.; Park, H.K.; Han, K.T.; Kim, W.; Lee, H.J.; Park, E.C. Deregulation of sale of over-the-counter drugs outside of pharmacies in the Republic of Korea: Interrupted-time-series analysis of outpatient visits before and after the policy. BMC Health Serv. Res. 2017, 17, 478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- AbuAlreesh, A.; Alburikan, K.A. Health literacy among patients with poor understanding of prescription drug label instructions in Saudi Arabia. Saudi Pharm. J. 2019, 27, 900–905. [Google Scholar] [CrossRef]
- Huang, Y.M.; Chen, L.J.; Hsieh, L.L.; Chan, H.Y.; Chen-Liu, K.C.S.; Ho, Y.F. Evaluation of use, comprehensibility and clarity of over-the-counter medicine labels: Consumers’ perspectives and needs in Taiwan. Health Soc. Care Community 2022, 30, 753–761. [Google Scholar] [CrossRef]
- Formica, D.; Sultana, J.; Cutroneo, P.M.; Lucchesi, S.; Angelica, R.; Crisafulli, S.; Ingrasciotta, Y.; Salvo, F.; Spina, E.; Trifirò, G. The economic burden of preventable adverse drug reactions: A systematic review of observational studies. Expert Opin. Drug Saf. 2018, 17, 681–695. [Google Scholar] [CrossRef]
- Potlog Shchory, M.; Goldstein, L.H.; Arcavi, L.; Shihmanter, R.; Berkovitch, M.; Levy, A. Increasing adverse drug reaction reporting-How can we do better? PLoS ONE 2020, 15, e0235591. [Google Scholar] [CrossRef]
- Xie, Y.; Ma, M.; Zhang, Y.; Tan, X. Factors associated with health literacy in rural areas of Central China: Structural equation model. BMC Health Serv. Res. 2019, 19, 300. [Google Scholar] [CrossRef]
- Agarwal, P.; Lin, J.; Muellers, K.; O’Conor, R.; Wolf, M.; Federman, A.D.; Wisnivesky, J.P. A structural equation model of relationships of health literacy, illness and medication beliefs with medication adherence among patients with chronic obstructive pulmonary disease. Patient Educ. Couns. 2021, 104, 1445–1450. [Google Scholar] [CrossRef]
- Berthenet, M.; Vaillancourt, R.; Pouliot, A. Evaluation, modification, and validation of pictograms depicting medication instructions in the elderly. J. Health Commun. 2016, 21, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Muflih, S.M.; Bashir, H.N.; Khader, Y.S.; Karasneh, R.A. The impact of health literacy on self-medication: A cross-sectional outpatient study. J. Public Health 2022, 44, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Koster, E.S.; Blom, L.; Winters, N.A.; van Hulten, R.P.; Bouvy, M.L. Interpretation of drug label instructions: A study among four immigrants groups in the Netherlands. Int. J. Clin. Pharm. 2014, 36, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Bazargan, M.; Smith, J.; Yazdanshenas, H.; Movassaghi, M.; Martins, D.; Orum, G. Non-adherence to medication regimens among older African-American adults. BMC Geriatr. 2017, 17, 163. [Google Scholar] [CrossRef]
- Boudewyns, V.; O’Donoghue, A.C.; Kelly, B.; West, S.L.; Oguntimein, O.; Bann, C.M.; McCormack, L.A. Influence of patient medication information format on comprehension and application of medication information: A randomized, controlled experiment. Patient Educ. Couns. 2015, 98, 1592–1599. [Google Scholar] [CrossRef]
- Andrews, J.C.; Kees, J.; Paul, K.L.; Davis, T.C.; Wolf, M.S. Factors to consider in improving prescription drug pharmacy leaflets. Int. J. Advert. 2015, 34, 765–788. [Google Scholar] [CrossRef]
- Saqlain, M.; Riaz, A.; Malik, M.N.; Khan, S.; Ahmed, A.; Kamran, S.; Ali, H. Medication adherence and its association with health literacy and performance in activities of daily livings among elderly hypertensive patients in Islamabad, Pakistan. Medicina 2019, 55, 163. [Google Scholar] [CrossRef] [Green Version]
- Tong, V.; Raynor, D.K.; Aslani, P. Design and comprehensibility of over-the-counter product labels and leaflets: A narrative review. Int. J. Clin. Pharm. 2014, 36, 865–872. [Google Scholar] [CrossRef]
- Wolf, M.S.; Davis, T.C.; Curtis, L.M.; Bailey, S.C.; Knox, J.P.; Bergeron, A.; Abbet, M.; Shrank, W.H.; Parker, R.M.; Wood, A.J. A patient-centered prescription drug label to promote appropriate medication use and adherence. J. Gen. Intern. Med. 2016, 31, 1482–1489. [Google Scholar] [CrossRef]
- Lee, M.; Whitehill King, K.; Reid, L.N. Factors influencing consumers’ attitudinal and behavioral responses to direct-to-consumer and over-the-counter drug advertising. J. Health Commun. 2015, 20, 431–444. [Google Scholar] [CrossRef]
- Korean Statistical Information Service. Population Statistics Based on Resident Registration. Available online: https://kosis.kr/eng/ (accessed on 15 January 2021).
- Davis, T.C.; Long, S.W.; Jackson, R.H.; Mayeaux, E.J.; George, R.B.; Murphy, P.W.; Crouch, M.A. Rapid estimate of adult literacy in medicine: A shortened screening instrument. Fam. Med. 1993, 25, 391–395. [Google Scholar] [PubMed]
- Lee, S.H.; Choi, E.H.R.; Je, M.J.; Han, H.S.; Park, B.K.; Kim, S.S. Comparison of two versions of KHLAT for improvement strategies. Korean J. Health Ed. Promot. 2011, 28, 57–65. [Google Scholar]
- Kim, S.S.; Kim, S.H.; Lee, S.Y. Health literacy: Development of a Korean health literacy assessment tool. Korean J. Health Educ. Promot. 2005, 22, 215–227. [Google Scholar]
- Hazra, A.; Gogtay, N. Biostatistics series module 4: Comparing groups—Categorical variables. Indian J. Dermatol. 2016, 61, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Fay, M.; Proschan, M. Wilcoxon–Mann–Whitney or t-test? On assumptions for hypothesis test and multiple interpretations of decision rules. Stat. Surv. 2010, 4, 1–39. [Google Scholar] [CrossRef]
- Harman, H.H. Modern Factor Analysis, 3rd ed.; University of Chicago Press: Chicago, IL, USA, 1976. [Google Scholar]
- Rababah, J.A.; Al-Hammouri, M.M.; Drew, B.L. The impact of health literacy on college students’ psychological disturbances and quality of life: A structural equation modeling analysis. Health Qual. Life Outcomes 2020, 18, 292. [Google Scholar] [CrossRef]
- Gutierrez, K.M.; Cohn, L.D. Medication competence, numeracy, and health literacy. Health Lit. Res. Pract. 2019, 3, e181–e186. [Google Scholar] [CrossRef] [Green Version]
- Lee, Y.M.; Yu, H.Y.; You, M.A.; Son, Y.J. Impact of health literacy on medication adherence in older people with chronic diseases. Collegian 2017, 24, 11–18. [Google Scholar] [CrossRef]
- Kim, L.Y.; Lee, I.-H. Readibility of the product labelling of information of over-the-counter pharmaceuticals in convenient store. Korean J. Clin. Phamacol. 2015, 25, 27–33. [Google Scholar]
- Jin, H.K.; Kim, Y.H.; Rhie, S.J. Factors affecting medication adherence in elderly people. Patient Prefer. Adherence 2016, 10, 2117–2125. [Google Scholar] [CrossRef] [Green Version]
- Wilson, K.M.; Singh, P.; Blumkin, A.K.; Dallas, L.; Klein, J.D. Knowledge gaps and misconceptions about over-the-counter analgesics among adolescents attending a hospital-based clinic. Acad. Pediatrics 2010, 10, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Rahman, F.I.; Aziz, F.; Huque, S.; Ether, S.A. Medication understanding and health literacy among patients with multiple chronic conditions: A study conducted in Bangladesh. J. Public Health Res. 2020, 9, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Koops van‘t Jagt, R.; Hoeks, J.C.J.; Jansen, C.J.M.; Winter, A.F.d.; Reijneveld, S.A. Comprehensibility of health-related documents for older adults with different levels of health literacy: A systematic review. J. Health Commun. 2016, 21, 159–177. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.S.; Davis, T.C.; Curtis, L.M.; Webb, J.A.; Bailey, S.C.; Shrank, W.H.; Lindquist, L.; Ruo, B.; Bocchini, M.V.; Parker, R.M.; et al. Effect of standardized, patient-centered label instructions to improve comprehension of prescription drug use. Med. Care 2011, 49, 96–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, T.C.; Federman, A.D.; Bass, P.F.; Jackson, R.H.; Middlebrooks, M.; Parker, R.M.; Wolf, M.S. Improving patient understanding of prescription drug label instructions. J. Gen. Intern. Med. 2009, 24, 57–62. [Google Scholar] [CrossRef] [Green Version]
- Shrank, W.; Avorn, J.; Rolon, C.; Shekelle, P. Effect of content and format of prescription drug labels on readability, understanding, and medication use: A systematic review. Ann. Pharmacother. 2007, 41, 783–801. [Google Scholar] [CrossRef]
- Nutbeam, D.; McGill, B.; Premkumar, P. Improving health literacy in community populations: A review of progress. Health Promot. Int. 2018, 33, 901–911. [Google Scholar] [CrossRef]
- Visscher, B.B.; Steunenberg, B.; Heerdink, E.R.; Rademakers, J. Medication self-management support for people with diabetes and low health literacy: A needs assessment. PLoS ONE. 2020, 15, e0232022. [Google Scholar] [CrossRef]
- Mayo-Gamble, T.L.; Mouton, C. Examining the association between health literacy and medication adherence among older adults. Health Commun. 2018, 33, 1124–1130. [Google Scholar] [CrossRef]
- Merks, P.; Świeczkowski, D.; Balcerzak, M.; Drelich, E.; Białoszewska, K.; Cwalina, N.; Krysinski, J.; Jaguszewski, M.; Pouliot, A.; Vaillancourt, R. The evaluation of pharmaceutical pictograms among elderly patients in community pharmacy settings—A multicenter pilot study. Patient Prefer. Adherence 2018, 12, 257–266. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.J.; Yang, Y.-M.; Choi, E.J. Use patterns of over-the-counter (OTC) medications and perspectives on OTC medications among Korean adult patients with chronic diseases: Gender and age differences. Patient Prefer. Adherence 2018, 12, 1597–1606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, A.H.S.; Chan, K.W.L. Effects of prospective-user factors and sign design features on guessability of pharmaceutical pictograms. Patient Educ. Couns. 2013, 90, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Han, S.H.; Han, H.S.; Sohn, H.S. Conversion of professional terminology used in written medication instruction to plain terminology to improve health literacy. Yakhak Hoeji 2021, 65, 87–97. [Google Scholar] [CrossRef]
- Krypel, L.L. Constructing a self-care curriculum. Am. J. Pharm. Educ. 2006, 70, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coskun, S.; Bagcivan, G. Associated factors with treatment adherence of patients diagnosed with chronic disease: Relationship with health literacy. Appl. Nurs. Res. 2020, 57, 151368. [Google Scholar] [CrossRef]
- Setia, M.S. Methodology series module 3: Cross-sectional studies. Indian J. Dermatol. 2016, 61, 261–264. [Google Scholar] [CrossRef]
- Friis, K.; Aaby, A.; Lasgaard, M.; Pedersen, M.H.; Osborne, R.H.; Maindal, H.T. Low health literacy and mortality in individuals with cardiovascular disease, chronic obstructive pulmonary disease, diabetes, and mental illness: A 6-year population-based follow-up study. Int. J. Environ. Res. Public Health 2020, 17, 9399. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, K.L.; Wingard, R.L.; Hakim, R.M.; Eden, S.; Shintani, A.; Wallston, K.A.; Huizinga, M.M.; Elasy, T.A.; Russell, L.; Rothman Ikizler, T.A. Low health literacy associates with increased mortality in ESRD. J. Am. Soc. Nephrol. 2010, 21, 1979–1985. [Google Scholar] [CrossRef] [Green Version]
| Variables | Total (n = 375) n (%) | Adequate Health Literacy (n = 240) n (%) | Inadequate Health Literacy (n = 135) n (%) | p-Value * |
|---|---|---|---|---|
| Gender | ||||
| Women | 203 (54.1) | 128 (53.3) | 75 (55.6) | 0.679 |
| Men | 172 (45.9) | 112 (46.7) | 60 (44.4) | |
| Age (Mean ± SD) | (42.4 ± 13.2) | (43.8 ± 13.7) | (39.9 ± 12.0) | 0.005 |
| 20–40 | 185 (49.3) | 117 (48.8) | 68 (50.4) | 0.104 |
| 41–54 | 113 (30.1) | 80 (33.3) | 33 (24.4) | |
| ≥55 | 77 (20.5) | 43 (17.9) | 34 (25.2) | |
| Employment status | ||||
| Full time | 160 (42.7) | 116 (48.3) | 44 (32.6) | <0.001 |
| Part time | 30 (8.0) | 12 (5.0) | 18 (13.3) | |
| Housewife | 107 (28.5) | 79 (32.9) | 28 (20.7) | |
| Student | 40 (10.7) | 18 (7.5) | 22 (16.3) | |
| Others | 38 (10.1) | 15 (6.3) | 23 (17.0) | |
| Education | ||||
| <High school | 63 (16.8) | 25 (10.4) | 38 (28.1) | <0.001 |
| High school | 45 (12.0) | 19 (7.9) | 26 (19.3) | |
| >College | 267 (71.2) | 196 (81.6) | 71 (52.6) | |
| Chronic diseases | ||||
| No | 268 (71.5) | 177 (73.8) | 91 (67.4) | 0.193 |
| Yes | 107 (28.5) | 63 (26.3) | 44 (32.6) |
| Items | Total (n = 375) (%) | Adequate Health Literacy (n = 240) (%) | Inadequate Health Literacy (n = 135) (%) | p-Value * |
|---|---|---|---|---|
| Overall reading amounts of information on OTC drug labels | ||||
| Mean ± SD | 58.8 ± 20.8 | 61.8 ± 21.2 | 53.4 ± 19.0 | <0.001 |
| Median (IR) | 58.0 (44–74) | 61.5 (47–77) | 52 (40–69) | <0.001 |
| Reading amounts of information on each section of OTC drug label | ||||
| Uses and dosage | ||||
| Mean ± SD | 84.3 ± 16.7 | 86.5 ± 15.8 | 80.3 ± 17.6 | 0.001 |
| Median (IR) | 87.5 (75–100) | 91.6 (79.1–100) | 83.3 (70.8–95.8) | <0.001 |
| Cautions and warnings | ||||
| Mean ± SD | 53.7 ± 25.8 | 56.8 ± 26.4 | 48.3 ± 23.7 | 0.002 |
| Median (IR) | 55 (35–73.3) | 56.6 (38.3–76.6) | 48.3 (30–66.6) | 0.002 |
| Active ingredients and dosage form | ||||
| Mean ± SD | 39.5 ± 28.9 | 43.7 ± 29.3 | 31.9 ± 26.5 | <0.001 |
| Median (IR) | 37.5 (12.5–62.5) | 37.5 (18.7–68.7) | 25 (6.2–50.0) | <0.001 |
| Therapeutic Class of Medications Listed in a Prescription | Instructions for Medications Listed in a Prescription | Total (n = 375) n (%) | Adequate Health Literacy (n = 240) n (%) | Inadequate Health Literacy (n = 135) n (%) | p-Value * |
|---|---|---|---|---|---|
| Fever and aches | 1 medication | 44 (11.7) | 20 (8.3) | 24 (17.7) | 0.001 |
| Diabetes and hypertension | 5 medications with same dosage | 73 (19.4) | 37 (15.4) | 36 (26.6) | 0.002 |
| Asthma | 5 medications with different dosages | 81 (21.6) | 47 (19.5) | 34 (25.1) | 0.060 |
| Pictogram | Meaning | Total (n = 375) n (%) | Adequate Health Literacy (n = 240) n (%) | Inadequate Health Literacy (n = 135) n (%) |
|---|---|---|---|---|
| Pictograms with high misunderstanding | ||||
 | May cause bleeding | 183 (48.8) | 112 (46.6) | 71 (52.5) |
 | Take in the morning | 46 (12.2) | 33 (13.7) | 13 (9.6) |
 | May cause stomach problems | 42 (11.2) | 23 (9.5) | 19 (14.0) |
 | Do not take with other medicines | 32 (8.5) | 22 (9.1) | 10 (7.4) |
| Pictograms with low misunderstanding | ||||
 | Do not take if pregnant or planning pregnancy | 1 (0.2) | 0 (0) | 1 (0.7) |
 | Insert into your rectum | 2 (0.5) | 0 (0) | 2 (1.4) |
 | Do not break or crush | 13 (3.4) | 8 (3.3) | 5 (3.7) |
 | Shake it before use | 14 (3.7) | 7 (2.9) | 7 (5.1) |
| Variables | Misunderstanding Words on OTC Drug Labels | Misunderstanding Prescription Drug Instructions | Misunderstanding Pictograms | Overall Reading Amount of Information on OTC Drug Labels |
|---|---|---|---|---|
| Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | Coefficient (95% CI) | |
| Health literacy | ||||
| Inadequate | Ref | Ref | Ref | Ref |
| Adequate | −18.11 (−20.28, −15.95) ** | −1.26 (−3.58, 1.05) | −0.26 (−2.36, 1.83) | 9.27 (4.36, 14.17) ** |
| Age | ||||
| 20–40 | Ref | Ref | Ref | Ref |
| 41–54 | −0.86 (−3.30, 1.57) | 1.73 (−0.88, 4.34) | 2.53 (0.16, 4.90) * | 9.44 (3.91, 14.98) ** |
| ≥55 | −1.48 (−4.59, 1.63) | 8.81 (5.47, 12.14) ** | 5.26 (2.23, 8.28) ** | 12.49 (5.42, 19.55) ** |
| Gender | ||||
| Women | Ref | Ref | Ref | Ref |
| Men | 3.74 (1.72, 5.76) ** | 0.38 (−1.78, 2.54) | −0.05 (−2.01, 1.91) | −1.83 (−6.41, 2.74) |
| Education level | ||||
| <High school | Ref | Ref | Ref | Ref |
| High school | −1.53 (−5.77, 2.70) | −3.34 (−7.88, 1.19) | −1.49 (−5.61, 2.62) | 3.68 (−5.93, 13.29) |
| >College | −6.83 (−9.92, −3.74) ** | −5.05 (−8.36, −1.74) ** | −5.25 (−8.25, −2.25) ** | −0.57 (−7.57, 6.42) |
| Chronic disease | ||||
| No | Ref | Ref | Ref | Ref |
| Yes | 0.33 (−2.06, 2.74) | −0.28 (−2.86, 2.28) | 1.21 (−1.11, 3.55) | 7.49 (2.04, 12.94) ** |
| Model summary | ||||
| Adjusted R2 | 0.51 | 0.14 | 0.11 | 0.10 |
| F statistics | 56.834 | 10.137 | 7.692 | 7.562 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.; Suh, D.; Barone, J.A.; Jung, S.-Y.; Wu, W.; Suh, D.-C. Health Literacy Level and Comprehension of Prescription and Nonprescription Drug Information. Int. J. Environ. Res. Public Health 2022, 19, 6665. https://doi.org/10.3390/ijerph19116665
Kim M, Suh D, Barone JA, Jung S-Y, Wu W, Suh D-C. Health Literacy Level and Comprehension of Prescription and Nonprescription Drug Information. International Journal of Environmental Research and Public Health. 2022; 19(11):6665. https://doi.org/10.3390/ijerph19116665
Chicago/Turabian StyleKim, Meehoh, David Suh, Joseph A. Barone, Sun-Young Jung, Wenchen Wu, and Dong-Churl Suh. 2022. "Health Literacy Level and Comprehension of Prescription and Nonprescription Drug Information" International Journal of Environmental Research and Public Health 19, no. 11: 6665. https://doi.org/10.3390/ijerph19116665






