Prompts for the Future to Live Healthier: A Study of Cognition and Motivation for Healthy Behaviors
Abstract
1. Introduction
1.1. Definition of Health Promotion
1.2. Health Belief Model
1.3. Cognition of Health Promotion
2. Materials and Methods
2.1. Standard for Selection of Research Target
2.2. Research Procedure
- Social demography variables, including age, gender, present work situation, occupation, educational level, etc.
- Perceived health conditions: This was a self-report of the sample on their health status, including perceived health conditions, health level as compared to that of 3 years ago, prediction of self-health, and autonomous non-bedridden age.
- Living habit situation: After reminding the respondents of what unhealthy bedridden years were, the sample showed a stronger willingness to continue with behaviors that he/she had implemented, or increased behaviors that could be implemented presently. The contents included previous dieting methods, present dieting methods, previous physical activity, and present physical activity.
3. Results
- (1)
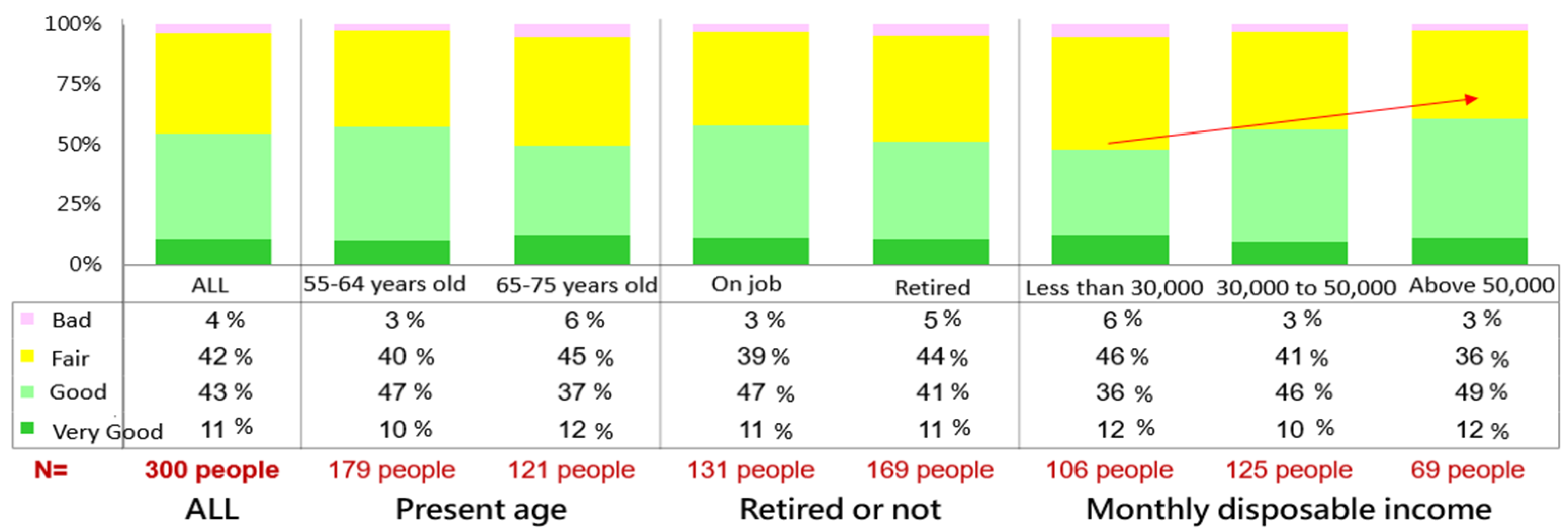
- Self-health situation
- (2)
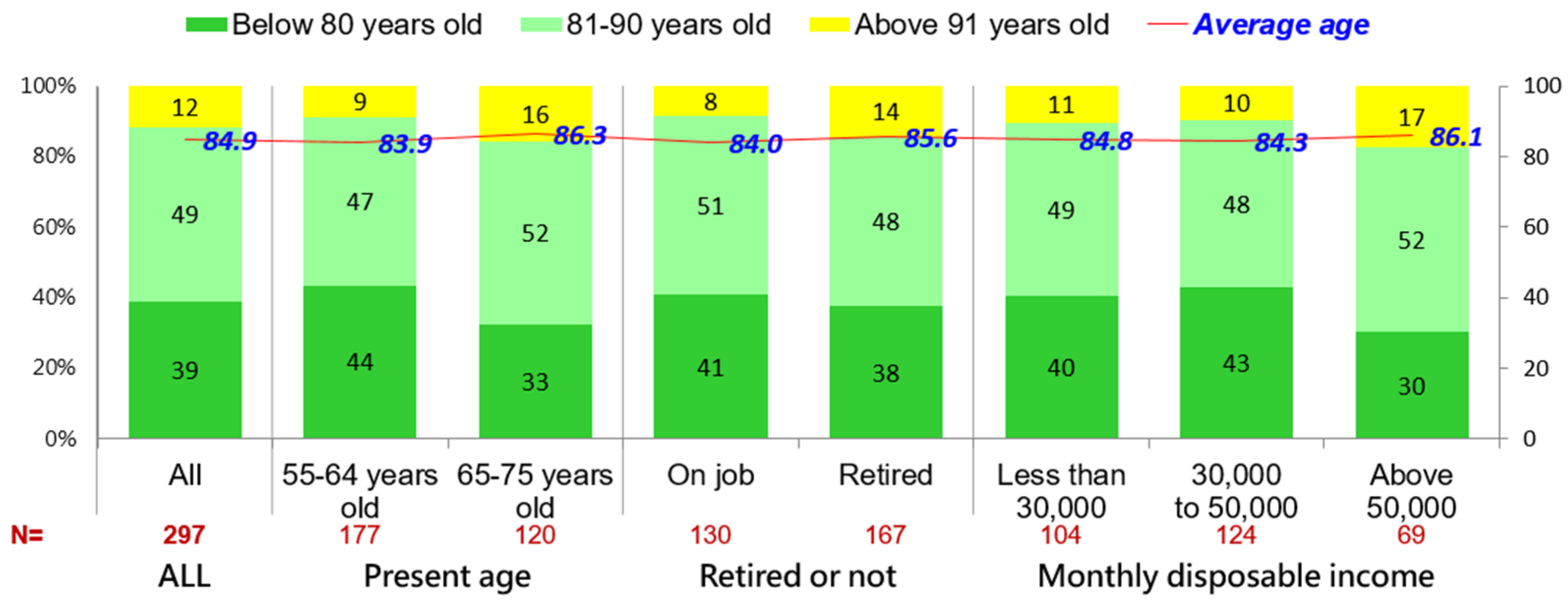
- Self-age prediction
- (3)
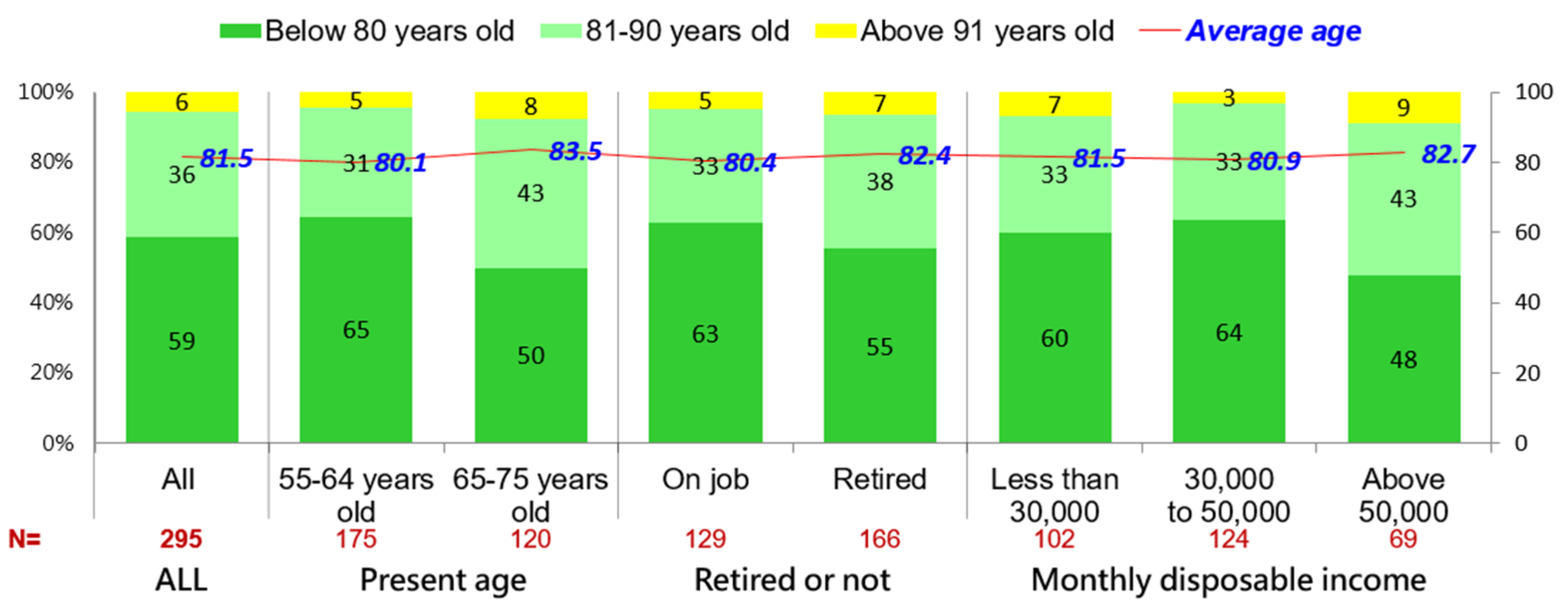
- Prediction of age of self-health and autonomous non-bedridden age
- (4)
- Health situation compared to that of three years ago
- (5)
- Previous dieting method
- (6)
- Previous physical activity
- (1)
- Present dieting methods
- (2)
- Present physical activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- “Unhealthy Life Expectancy” for Fellow Countrymen Had Reached 8.47 Years in 2019, Which Was a Historical Record High. 2021. Available online: https://www.ftvnews.com.tw/news/detail/2021809L06M1 (accessed on 9 August 2021).
- Green, L.; Kreuter, M. The precede–proceed model. In Health Promotion Planning: An Educational Approach, 3rd ed.; Mayfield Publishing Company: Mountain View, CA, USA, 1999; pp. 32–43. [Google Scholar]
- Bunton, R.; Macdonald, G.; Macdonald, G. Health promotion: Disciplinary developments. In Health Promotion: Disciplines and Diversity, 2nd ed.; Macdonald, G., Bunton, R., Eds.; Routledge: London, UK, 2003; pp. 23–42. [Google Scholar]
- Tannahill, A. What is health promotion? Health Educ. J. 1985, 44, 167–168. [Google Scholar] [CrossRef] [PubMed]
- Beattie, A. 12 The health promoting school: From idea to action. In Health Promotion: Professional Perspectives; Scriven, A., Orme, J., Eds.; Macmillan Press: London, UK, 1996; pp. 129–143. [Google Scholar]
- MacDonald, T.H. Rethinking Health Promotion: A Global Approach; Routledge: London, UK, 2012. [Google Scholar]
- Smith, R.D. Promoting the health of people with physical disabilities: A discussion of the financing and organization of public health services in Australia. Health Promot. Int. 2000, 15, 79–86. [Google Scholar] [CrossRef][Green Version]
- Merzel, C.; D’Afflitti, J. Reconsidering community-based health promotion: Promise, performance, and potential. Am. J. Public Health 2003, 93, 557–574. [Google Scholar] [CrossRef] [PubMed]
- Duaso, M.J.; Cheung, P. Health promotion and lifestyle advice in a general practice: What do patients think? J. Adv. Nurs. 2002, 39, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Chiva, A.; Stears, D. Promoting the Health of Older People: The Next Step in Health Generation; Open University Press: Buckingham, UK, 2001. [Google Scholar]
- Rosenstock, I.M. Historical origins of the health belief model. Health Educ. Monogr. 1974, 2, 328–335. [Google Scholar] [CrossRef]
- Robins, P.R. Some explorations into the nature of anxieties relating to illness. Genet. Psychol. Monogr. 1962, 66, 91–141. [Google Scholar]
- Rosenstock, I.M. The health belief model and preventive health behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Huang, S.-C.; Yao, Y.-C. Study on health belief, diet-related self-efficacy and dieting behavior of students in universities. J. Natl. Taiwan Norm. Univ. Educ. Type 1999, 44, 43–53. [Google Scholar]
- Becker, M.H.; Maiman, B.A. Sociobehavioral determinants of compliance with health and medical care recommen-dations. Med. Care 1975, 13, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Wong, L.P.; Alias, H.; Wong, P.F.; Lee, H.Y.; AbuBakar, S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum. Vaccines Immunother. 2020, 16, 2204–2214. [Google Scholar] [CrossRef] [PubMed]
- Shmueli, L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health 2021, 21, 804. [Google Scholar] [CrossRef] [PubMed]
- Posner, M.I. Cognition: An Introduction; Scott Foresman: Brook, IL, USA, 1973. [Google Scholar]
- Rivera, E.; Corte, C.; Steffen, A.; DeVon, H.A.; Collins, E.G.; McCabe, P.J. Illness Representation and Self-Care Ability in Older Adults with Chronic Disease. Geriatrics 2018, 3, 45. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-L.; Chen, L.-S.; Chen, Y.T.; Gardenhire, D.S. The Association of Health-Related Factors with Leisure-Time Physical Activity among Adults with COPD: A Cross-Sectional Analysis. Healthcare 2022, 10, 249. [Google Scholar] [CrossRef] [PubMed]
- Bevan, A.L.; Maxfield, M.; Bultmann, M.N. The effects of age and death awareness on intentions for healthy behaviours. Psychol. Health 2014, 29, 405–421. [Google Scholar] [CrossRef] [PubMed]
- Pardasani, M.; Berman, J.; Powell, M. Age-Tastic! An Evaluation of an Evidence-Based Intervention for Older Adults. Healthcare 2018, 6, 142. [Google Scholar] [CrossRef] [PubMed]
- Klinker, C.D.; Aaby, A.; Ringgaard, L.W.; Hjort, A.V.; Hawkins, M.; Maindal, H.T. Health Literacy is Associated with Health Behaviors in Students from Vocational Education and Training Schools: A Danish Population-Based Survey. Int. J. Environ. Res. Public Health 2020, 17, 671. [Google Scholar] [CrossRef] [PubMed]
- Atallah, N.; Adjibade, M.; Lelong, H.; Hercberg, S.; Galan, P.; Assmann, K.E.; Kesse-Guyot, E. How Healthy Lifestyle Factors at Midlife Relate to Healthy Aging. Nutrients 2018, 10, 854. [Google Scholar] [CrossRef] [PubMed]
- Shih, W.-W. Study of Influential Factors for the Health Situations of Teachers in Colleges and Universities Using Health Belief Model. Master’s Thesis, National Sun Yat-sen University, Kaohsiung City, Taiwan, 2004. [Google Scholar]
| Basic Information | Top Item | Percentage |
|---|---|---|
| gender | female | 52% |
| age | in the range of 55–64 years old | 60% |
| religion | Buddhism | 41% |
| educational level | those above senior high/occupational senior high school | 77% |
| birth place | Islanders and Southern Fujian | 71% |
| occupational situation | retired | 56% |
| occupation | commerce section | 30% |
| marital situation | married or cohabiting | 82% |
| present living situation | living with partner/spouse | 78% |
| experience taking care of parents | had experience taking care of parents | 70% |
| % | All | Age | Retired or Not | Monthly Disposable Income | ||||
|---|---|---|---|---|---|---|---|---|
| 55–64 Years Old | 65–75 Years Old | On Job | Retired | Less Than 30,000 NTD | 30,000–50,000 NTD | Above 50,000 NTD | ||
| n = | 300 | 179 | 121 | 131 | 169 | 106 | 125 | 69 |
| Memory was worse than before | 69% | 69% | 70% | 71% | 68% | 68% | 66% | 78% |
| Physical strength was worse than before | 59% | 60% | 59% | 62% | 57% | 60% | 59% | 58% |
| Not knowing the reason for waist and back pain | 31% | 35% | 26% | 37% | 26% | 35% | 31% | 25% |
| Red letter shown in health test report | 27% | 28% | 25% | 30% | 24% | 28% | 27% | 23% |
| Catching cold more | 7% | 7% | 7% | 6% | 8% | 6% | 10% | 6% |
| frequently | 8% | 8% | 7% | 8% | 8% | 8% | 7% | 9% |
| % | All | Age | Retired or Not | Monthly Disposable Income | ||||
|---|---|---|---|---|---|---|---|---|
| 55–64 Years Old | 65–75 Years Old | Employed | Retired | Less Than 30,000 NTD | 30,000–50,000 NTD | Above 50,000 NTD | ||
| n = | 300 | 179 | 121 | 131 | 169 | 106 | 125 | 69 |
| Maintaining a positive mood | 83% | 79% | 88% | 76% | 88% | 80% | 83% | 86% |
| Sleeping more than six hours each day | 79% | 81% | 77% | 79% | 79% | 79% | 79% | 80% |
| Having autonomous exercise habits | 54% | 50% | 60% | 47% | 59% | 45% | 62% | 52% |
| Sitting less than 90 min at a time | 43% | 38% | 50% | 37% | 47% | 41% | 46% | 42% |
| Waling more than 6000 steps a day | 40% | 36% | 45% | 38% | 41% | 39% | 41% | 41% |
| Participating in a sports club | 27% | 23% | 31% | 21% | 31% | 25% | 26% | 30% |
| Item | Dieting Methods That Were Done Previously | Dieting Methods Done Presently | Number of People Who Were Willing to Pay More Attention to Diet after This Survey | Percentage |
|---|---|---|---|---|
| Try to have fixed times and quantities for three daily meals | 72 persons | 86 persons | +14 persons | 29% |
| Try to have less or reduced sugar | 76 persons | 85 persons | +9 persons | 28% |
| Have two types of fruits daily | 58 persons | 80 persons | +22 persons | 27% |
| Have three dishes of vegetable daily | 51 persons | 73 persons | +22 persons | 24% |
| Try to eat a lot of husked rice and cereals | 46 persons | 65 persons | +19 persons | 22% |
| Take daily vitamins or other health foods | 53 persons | 63 persons | +10 persons | 21% |
| Item | Physical Activities That Were Done Previously | Physical Activities That Were Done Presently | Number of People Who Were Willing to Engage in More Physical Activity after This Survey | Percentage |
|---|---|---|---|---|
| Maintaining a positive mood | 83 persons | 89 persons | +6 persons | 30% |
| Sleeping for more than six hours each day | 79 persons | 85 persons | +6 persons | 28% |
| Having autonomous exercise habits | 54 persons | 72 persons | +18 persons | 24% |
| Walking 6000 steps each day | 40 persons | 62 persons | +22 persons | 21% |
| Sitting for less than 90 min at a time | 43 persons | 60 persons | +17 persons | 20% |
| Participating in a sports club | 27 persons | 37 persons | +10 persons | 12% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-C.; Yu, P.-H.; Lin, J.-K. Prompts for the Future to Live Healthier: A Study of Cognition and Motivation for Healthy Behaviors. Int. J. Environ. Res. Public Health 2022, 19, 6682. https://doi.org/10.3390/ijerph19116682
Lin C-C, Yu P-H, Lin J-K. Prompts for the Future to Live Healthier: A Study of Cognition and Motivation for Healthy Behaviors. International Journal of Environmental Research and Public Health. 2022; 19(11):6682. https://doi.org/10.3390/ijerph19116682
Chicago/Turabian StyleLin, Chung-Chih, Pang-Hsiang Yu, and Jin-Kwan Lin. 2022. "Prompts for the Future to Live Healthier: A Study of Cognition and Motivation for Healthy Behaviors" International Journal of Environmental Research and Public Health 19, no. 11: 6682. https://doi.org/10.3390/ijerph19116682
APA StyleLin, C.-C., Yu, P.-H., & Lin, J.-K. (2022). Prompts for the Future to Live Healthier: A Study of Cognition and Motivation for Healthy Behaviors. International Journal of Environmental Research and Public Health, 19(11), 6682. https://doi.org/10.3390/ijerph19116682





