New Understanding of Diagnosis, Treatment and Prevention of Endometriosis
Abstract
:1. Introduction
2. New Understanding of Pathophysiology
3. Clinical Consequences of Our New Understanding
3.1. Higher Risk of Initiating Endometriosis during Adolescence
3.2. Clinical Symptoms of Endometriosis
3.3. Diagnosis
3.4. Treatment
3.5. Prevention of Recurrences
4. Discussion of Changing Endometriosis Strategies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sampson, J.A. Perforating hemorrhagic (chocolate) cysts of the ovary. Their importance and especially their relation to pelvic adenomas of the endometrial type. Arch. Surg. 1921, 3, 245–323. [Google Scholar] [CrossRef] [Green Version]
- Cullen, T.S. Adeno-myoma uteri diffusum benignum. Johns Hopkins Hosp. Rep. 1897, 6, 133–157. [Google Scholar]
- Kempers, R.D.; Dockerty, M.B.; Hunt, A.B.; Symmonds, R.E. Significant postmenopausal endometriosis. Surg. Gynecol. Obstet. 1960, 111, 348–356. [Google Scholar] [PubMed]
- Jansen, R.P.S.; Russel, P. Nonpigmented endometriosis: Clinical, laparoscopic, and pathologic definition. Am. J. Obstet. Gynecol. 1986, 155, 1154–1159. [Google Scholar] [CrossRef]
- Cornillie, F.J.; Oosterlynck, D.; Lauweryns, J.M.; Koninckx, P.R. Deeply infiltrating pelvic endometriosis: Histology and clinical significance. Fertil. Steril. 1990, 53, 978–983. [Google Scholar] [CrossRef]
- Mignemi, G.; Facchini, C.; Raimondo, D.; Montanari, G.; Ferrini, G.; Seracchioli, R. A case report of nasal endometriosis in a patient affected by Behcet’s disease. J. Minim. Invasive Gynecol. 2012, 19, 514–516. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Martin, D.C. Deep endometriosis: A consequence of infiltration or retraction or possibly adenomyosis externa? Fertil. Steril. 1992, 58, 924–928. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Gomel, V.; Martin, D.C. Pathogenesis of endometriosis: The genetic/epigenetic theory. Fertil. Steril. 2019, 111, 327–339. [Google Scholar] [CrossRef] [Green Version]
- Bulun, S.E.; Yilmaz, B.D.; Sison, C.; Miyazaki, K.; Bernardi, L.; Liu, S.; Kohlmeier, A.; Yin, P.; Milad, M.; Wei, J. Endometriosis. Endocr. Rev. 2019, 40, 1048–1079. [Google Scholar] [CrossRef]
- Saha, R.; Pettersson, H.J.; Svedberg, P.; Olovsson, M.; Bergqvist, A.; Marions, L.; Tornvall, P.; Kuja-Halkola, R. The heritability of endometriosis. Fertil. Steril. 2015, 104, 947–952. [Google Scholar] [CrossRef] [Green Version]
- de Almeida Asencio, F.; Ribeiro, H.A.; Ribeiro, P.A.; Malzoni, M.; Adamyan, L.; Ussia, A.; Gomel, V.; Martin, D.C.; Koninckx, P.R. Symptomatic endometriosis developing several years after menopause in the absence of increased circulating estrogen concentrations: A systematic review and seven case reports. Gynecol. Surg. 2019, 16, 3. [Google Scholar] [CrossRef] [Green Version]
- Makiyan, Z. Endometriosis origin from primordial germ cells. Organogenesis 2017, 13, 95–102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrando, C.A.; Chapman, G.; Pollard, R. Preoperative Pain Symptoms and the Incidence of Endometriosis in Transgender Men Undergoing Hysterectomy for Gender Affirmation. J. Minim. Invasive Gynecol. 2021, 28, 1579–1584. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Ide, P.; Vandenbroucke, W.; Brosens, I.A. New aspects of the pathophysiology of endometriosis and associated infertility. J. Reprod. Med. 1980, 24, 257–260. [Google Scholar]
- Koninckx, P.R.; Ussia, A.; Tahlak, M.; Adamyan, L.; Wattiez, A.; Martin, D.C.; Gomel, V. Infection as a potential cofactor in the genetic-epigenetic pathophysiology of endometriosis: A systematic review. Facts Views Vis. ObGyn 2019, 11, 209–216. [Google Scholar] [PubMed]
- Leonardi, M.; Hicks, C.; El-Assaad, F.; El-Omar, E.; Condous, G. Endometriosis and the microbiome: A systematic review. BJOG 2020, 127, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Koppolu, A.; Maksym, R.B.; Paskal, W.; Machnicki, M.; Rak, B.; Pępek, M.; Garbicz, F.; Pełka, K.; Kuśmierczyk, Z.; Jacko, J.; et al. Epithelial Cells of Deep Infiltrating Endometriosis Harbor Mutations in Cancer Driver Genes. Cells 2021, 10, 749. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.W. Cancer driver mutations in endometriosis: Variations on the major theme of fibrogenesis. Reprod. Med. Biol. 2018, 17, 369–397. [Google Scholar] [CrossRef] [Green Version]
- Murakami, K.; Kanto, A.; Sakai, K.; Miyagawa, C.; Takaya, H.; Nakai, H.; Kotani, Y.; Nishio, K.; Matsumura, N. Frequent PIK3CA mutations in eutopic endometrium of patients with ovarian clear cell carcinoma. Mod. Pathol. 2021, 34, 2071–2079. [Google Scholar] [CrossRef]
- Bulun, S.E.; Monsivais, D.; Kakinuma, T.; Furukawa, Y.; Bernardi, L.; Pavone, M.E.; Dyson, M. Molecular biology of endometriosis: From aromatase to genomic abnormalities. Semin. Reprod. Med. 2015, 33, 220–224. [Google Scholar]
- Koninckx, P.R.; Ussia, A.; Mashiach, R.; Vilos, G.; Martin, D.C. Endometriosis Can Cause Pain at a Distance. J. Obstet. Gynaecol. Can. 2021, 43, 1035–1036. [Google Scholar] [CrossRef] [PubMed]
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Gomel, V.; Martin, D.C. Heterogeneity of endometriosis lesions requires individualisation of diagnosis and treatment and a different approach to research and evidence based medicine. Facts Views Vis. ObGyn 2020, 11, 263. [Google Scholar] [PubMed]
- Becker, C.M.; Gattrell, W.T.; Gude, K.; Singh, S.S. Reevaluating response and failure of medical treatment of endometriosis: A systematic review. Fertil. Steril. 2017, 108, 125–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vercellini, P.; Sergenti, G.; Buggio, L.; Frattaruolo, M.P.; Dridi, D.; Berlanda, N. Advances in the medical management of bowel endometriosis. Best Pract. Res. Clin. Obstet. Gynaecol. 2020, 71, 78–99. [Google Scholar] [CrossRef]
- Nirgianakis, K.; Ma, L.; McKinnon, B.; Mueller, M.D. Recurrence Patterns after Surgery in Patients with Different Endometriosis Subtypes: A Long-Term Hospital-Based Cohort Study. J. Clin. Med. 2020, 9, 496. [Google Scholar] [CrossRef] [Green Version]
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Gomel, V.; Martin, D.C. Peritoneal fluid progesterone and progesterone resistance in superficial endometriosis lesions. Hum. Reprod. 2022, 28, 209–219. [Google Scholar] [CrossRef]
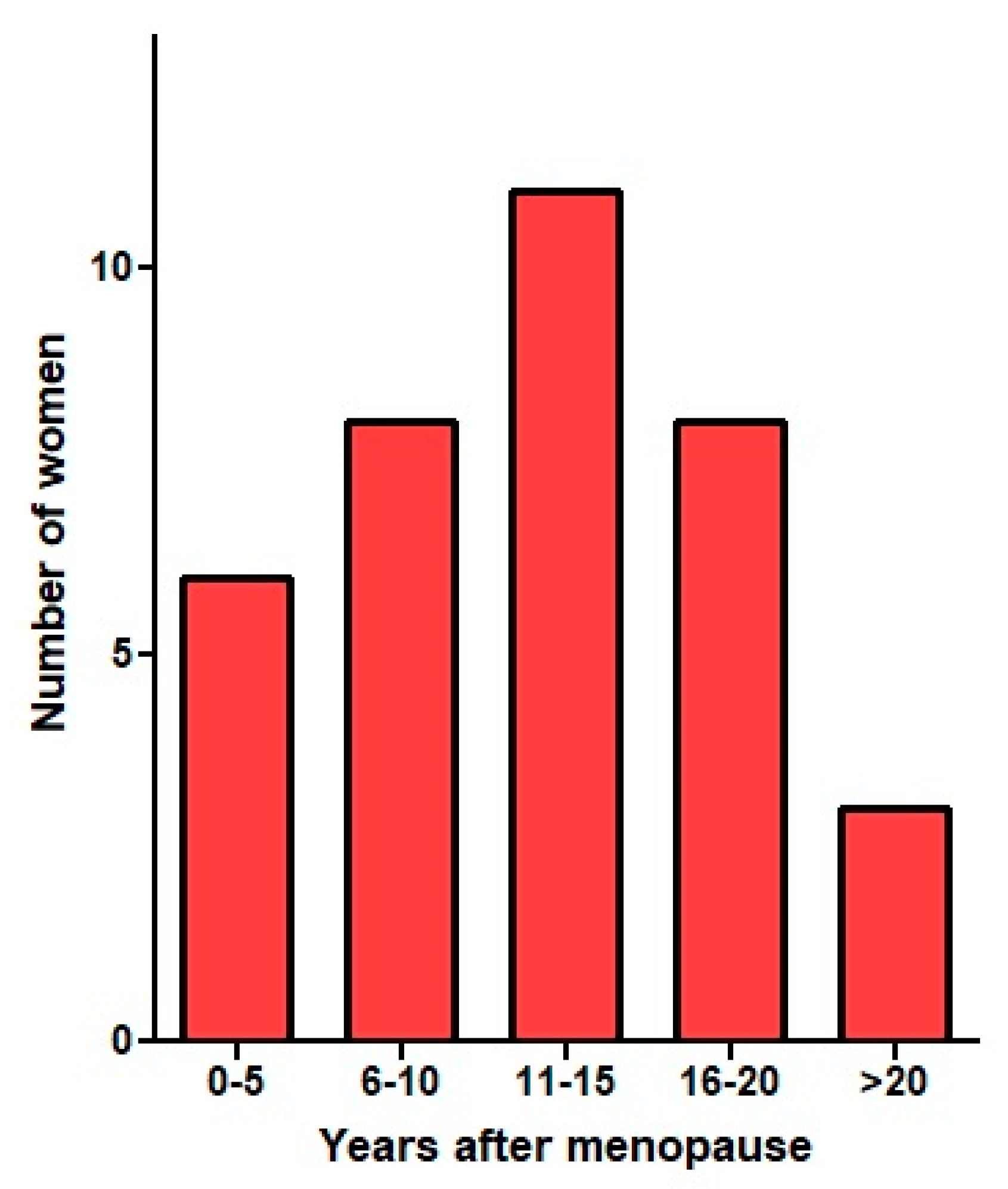
- Koninckx, P.R.; Ussia, A.; Wattiez, A.; Adamyan, L.; Martin, D.C.; Gordts, S. The severity and frequency distribution of endometriosis subtypes at different ages: A model to understand the natural history of endometriosis based on single centre/single surgeon data. Facts Views Vis. ObGyn 2021, 13, 211–221. [Google Scholar] [CrossRef]
- Samaneh, Y.; ShahidehJahanian, S.; Azadeh, M.; Anoshirvan, K. The association of food consumption and nutrient intake with endometriosis risk in Iranian women: A case-control study. Int. J. Reprod. Biomed. 2019, 17, 661–670. [Google Scholar] [CrossRef]
- Harris, H.R.; Chavarro, J.E.; Malspeis, S.; Willett, W.C.; Missmer, S.A. Dairy-food, calcium, magnesium, and vitamin D intake and endometriosis: A prospective cohort study. Am. J. Epidemiol. 2013, 177, 420–430. [Google Scholar] [CrossRef] [Green Version]
- Parazzini, F.; Chiaffarino, F.; Surace, M.; Chatenoud, L.; Cipriani, S.; Chiantera, V.; Benzi, G.; Fedele, L. Selected food intake and risk of endometriosis. Hum. Reprod. 2004, 19, 1755–1759. [Google Scholar] [CrossRef] [Green Version]
- Tennfjord, M.K.; Gabrielsen, R.; Tellum, T. Effect of physical activity and exercise on endometriosis-associated symptoms: A systematic review. BMC Womens Health 2021, 21, 355. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.; Sverrisdóttir, U.; Rudnicki, M. Impact of exercise on pain perception in women with endometriosis: A systematic review. Acta Obstet. Gynecol. Scand. 2021, 100, 1595–1601. [Google Scholar] [CrossRef] [PubMed]
- Poli-Neto, O.B.; Oliveira, A.M.Z.; Salata, M.C.; Cesar Rosa, E.S.J.; Machado, D.R.L.; Candido-Dos-Reis, F.J.; Nogueira, A.A. Strength Exercise Has Different Effects on Pressure Pain Thresholds in Women with Endometriosis-Related Symptoms and Healthy Controls: A Quasi-experimental Study. Pain Med. 2020, 21, 2280–2287. [Google Scholar] [CrossRef] [PubMed]
- Montenegro, M.L.; Bonocher, C.M.; Meola, J.; Portella, R.L.; Ribeiro-Silva, A.; Brunaldi, M.O.; Ferriani, R.A.; Rosa, E.S.J.C. Effect of Physical Exercise on Endometriosis Experimentally Induced in Rats. Reprod. Sci. 2018, 26, 785–793. [Google Scholar] [CrossRef]
- Bonocher, C.M.; Montenegro, M.L.; JC, R.e.S.; Ferriani, R.A.; Meola, J. Endometriosis and physical exercises: A systematic review. Reprod. Biol. Endocrinol. 2014, 12, 4. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Yang, Y.; Li, W.; Tian, X.; Cui, H.; Zhang, Q. Identification of small-molecule ligands that bind to MiR-21 as potential therapeutics for endometriosis by screening ZINC database and in-vitro assays. Gene 2018, 662, 46–53. [Google Scholar] [CrossRef]
- Messalli, E.M.; Schettino, M.T.; Mainini, G.; Ercolano, S.; Fuschillo, G.; Falcone, F.; Esposito, E.; Di Donna, M.C.; De Franciscis, P.; Torella, M. The possible role of zinc in the etiopathogenesis of endometriosis. Clin. Exp. Obstet. Gynecol. 2014, 41, 541–546. [Google Scholar] [CrossRef]
- Warowicka, A.; Qasem, B.; Dera-Szymanowska, A.; Wołuń-Cholewa, M.; Florczak, P.; Horst, N.; Napierała, M.; Szymanowski, K.; Popenda, Ł.; Bartkowiak, G.; et al. Effect of Protoberberine-Rich Fraction of Chelidonium majus L. on Endometriosis Regression. Pharmaceutics 2021, 13, 931. [Google Scholar] [CrossRef]
- Liu, L.; Luo, N.; Guo, J.; Xie, Y.; Chen, L.; Cheng, Z. Berberine inhibits growth and inflammatory invasive phenotypes of ectopic stromal cells: Imply the possible treatment of adenomyosis. J. Pharmacol. Sci. 2018, 137, 5–11. [Google Scholar] [CrossRef]
- Porpora, M.G.; Brunelli, R.; Costa, G.; Imperiale, L.; Krasnowska, E.K.; Lundeberg, T.; Nofroni, I.; Piccioni, M.G.; Pittaluga, E.; Ticino, A.; et al. A promise in the treatment of endometriosis: An observational cohort study on ovarian endometrioma reduction by N-acetylcysteine. Evid. Based Complement. Altern. Med. 2013, 2013, 240702. [Google Scholar] [CrossRef] [Green Version]
- Marziali, M.; Capozzolo, T. Role of Gluten-Free Diet in the Management of Chronic Pelvic Pain of Deep Infiltranting Endometriosis. J. Minim. Invasive Gynecol. 2015, 22, S51–S52. [Google Scholar] [CrossRef] [PubMed]
- Leyendecker, G.; Herbertz, M.; Kunz, G.; Mall, G. Endometriosis results from the dislocation of basal endometrium. Hum. Reprod. 2002, 17, 2725–2736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koninckx, P.R.; Heyns, W.; Verhoeven, G.; Van Baelen, H.; Lissens, W.D.; De Moor, P.; Brosens, I.A. Biochemical characterization of peritoneal fluid in women during the menstrual cycle. J. Clin. Endocrinol. Metab. 1980, 51, 1239–1244. [Google Scholar] [CrossRef] [PubMed]
- Cromeens, M.G.; Carey, E.T.; Robinson, W.R.; Knafl, K.; Thoyre, S. Timing, delays and pathways to diagnosis of endometriosis: A scoping review protocol. BMJ Open 2021, 11, e049390. [Google Scholar] [CrossRef] [PubMed]
- Surrey, E.; Soliman, A.M.; Trenz, H.; Blauer-Peterson, C.; Sluis, A. Impact of Endometriosis Diagnostic Delays on Healthcare Resource Utilization and Costs. Adv. Ther. 2020, 37, 1087–1099. [Google Scholar] [CrossRef] [Green Version]
- Stochino-Loi, E.; Millochau, J.C.; Angioni, S.; Touleimat, S.; Abo, C.; Chanavaz-Lacheray, I.; Hennetier, C.; Roman, H. Relationship between Patient Age and Disease Features in a Prospective Cohort of 1560 Women Affected by Endometriosis. J. Minim. Invasive Gynecol. 2020, 27, 1158–1166. [Google Scholar] [CrossRef]
- Missmer, S.A.; Hankinson, S.E.; Spiegelman, D.; Barbieri, R.L.; Marshall, L.M.; Hunter, D.J. Incidence of Laparoscopically Confirmed Endometriosis by Demographic, Anthropometric, and Lifestyle Factors. Am. J. Epidemiol. 2004, 160, 784–796. [Google Scholar] [CrossRef]
- Goodman, L.R.; Franasiak, J.M. Efforts to redefine endometriosis prevalence in low-risk patients. BJOG 2018, 125, 63. [Google Scholar] [CrossRef] [Green Version]
- Koninckx, P.R.; Renaer, M. Pain sensitivity of and pain radiation from the internal female genital organs. Hum. Reprod. 1997, 12, 1785–1788. [Google Scholar] [CrossRef] [Green Version]
- Nirgianakis, K.; Gasparri, M.L.; Radan, A.P.; Villiger, A.; McKinnon, B.; Mosimann, B.; Papadia, A.; Mueller, M.D. Obstetric complications after laparoscopic excision of posterior deep infiltrating endometriosis: A case-control study. Fertil. Steril. 2018, 110, 459–466. [Google Scholar] [CrossRef] [Green Version]
- Vijay, A.; Valdes, A.M. Role of the gut microbiome in chronic diseases: A narrative review. Eur. J. Clin. Nutr. 2021, 76, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Huang, T.; Debelius, J.W.; Fang, F. Gut microbiome and amyotrophic lateral sclerosis: A systematic review of current evidence. J. Intern. Med. 2021, 290, 758–788. [Google Scholar] [CrossRef]
- Sublette, M.E.; Cheung, S.; Lieberman, E.; Hu, S.; Mann, J.J.; Uhlemann, A.C.; Miller, J.M. Bipolar disorder and the gut microbiome: A systematic review. Bipolar. Disord. 2021, 23, 544–564. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Sharma, V.; Shahjouei, S.; Li, J.; Chaudhary, D.; Khan, A.; Wolk, D.M.; Zand, R.; Abedi, V. At the Intersection of Gut Microbiome and Stroke: A Systematic Review of the Literature. Front. Neurol. 2021, 12, 729399. [Google Scholar] [CrossRef] [PubMed]
- Schütz, F.; Figueiredo-Braga, M.; Barata, P.; Cruz-Martins, N. Obesity and gut microbiome: Review of potential role of probiotics. Porto Biomed. J. 2021, 6, e111. [Google Scholar] [CrossRef]
- Sánchez Romero, E.A.; Meléndez Oliva, E.; Alonso Pérez, J.L.; Martín Pérez, S.; Turroni, S.; Marchese, L.; Villafañe, J.H. Relationship between the Gut Microbiome and Osteoarthritis Pain: Review of the Literature. Nutrients 2021, 13, 716. [Google Scholar] [CrossRef]
- Pinart, M.; Dötsch, A.; Schlicht, K.; Laudes, M.; Bouwman, J.; Forslund, S.K.; Pischon, T.; Nimptsch, K. Gut Microbiome Composition in Obese and Non-Obese Persons: A Systematic Review and Meta-Analysis. Nutrients 2021, 14, 12. [Google Scholar] [CrossRef]
- Chisari, E.; Wouthuyzen-Bakker, M.; Friedrich, A.W.; Parvizi, J. The relation between the gut microbiome and osteoarthritis: A systematic review of literature. PLoS ONE 2021, 16, e0261353. [Google Scholar] [CrossRef]
- Bu, Y.; Chan, Y.K.; Wong, H.L.; Poon, S.H.; Lo, A.C.; Shih, K.C.; Tong, L. A Review of the Impact of Alterations in Gut Microbiome on the Immunopathogenesis of Ocular Diseases. J. Clin. Med. 2021, 10, 4694. [Google Scholar] [CrossRef]
- Aldars-García, L.; Chaparro, M.; Gisbert, J.P. Systematic Review: The Gut Microbiome and Its Potential Clinical Application in Inflammatory Bowel Disease. Microorganisms 2021, 9, 977. [Google Scholar] [CrossRef]
- Yang, X.; Xu, X.; Lin, L.; Xu, K.; Xu, M.; Ye, J.; Shen, X. Sexual function in patients with endometriosis: A prospective case–control study in China. J. Int. Med. Res. 2021, 49, 030006052110043. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Zamora, M.-A.; Coloma, J.L.; Gracia, M.; Rius, M.; Castelo-Branco, C.; Carmona, F. Long-term Follow-up of Sexual Quality of Life after Laparoscopic Surgery in Patients with Deep Infiltrating Endometriosis. J. Minim. Invasive Gynecol. 2021, 28, 1912–1919. [Google Scholar] [CrossRef] [PubMed]
- Youseflu, S.; Jahanian Sadatmahalleh, S.; Bahri Khomami, M.; Nasiri, M. Influential factors on sexual function in infertile women with endometriosis: A path analysis. BMC Womens Health 2020, 20, 92. [Google Scholar] [CrossRef] [PubMed]
- Van Poll, M.; Van Barneveld, E.; Aerts, L.; Maas, J.W.M.; Lim, A.C.; De Greef, B.T.A.; Bongers, M.Y.; Van Hanegem, N. Endometriosis and Sexual Quality of Life. Sex. Med. 2020, 8, 532–544. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Meuleman, C.; Oosterlynck, D.; Cornillie, F.J. Diagnosis of deep endometriosis by clinical examination during menstruation and plasma CA-125 concentration. Fertil. Steril. 1996, 65, 280–287. [Google Scholar] [CrossRef]
- Oosterlynck, D.J.; Meuleman, C.; Waer, M.; Koninckx, P.R. CO2-laser excision of endometriosis does not improve the decreased natural killer activity. Acta Obstet. Gynecol. Scand. 1994, 73, 333–337. [Google Scholar] [CrossRef]
- Gordts, S.; Campo, R. Modern approaches to surgical management of endometrioma. Best Pract. Res Clin Obs. Gynaecol. 2019, 59, 48–55. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Donnez, J. Deep endometriosis: Definition, diagnosis, and treatment. Fertil. Steril. 2012, 98, 564–571. [Google Scholar] [CrossRef]
- Afrin, S.; AlAshqar, A.; El Sabeh, M.; Miyashita-Ishiwata, M.; Reschke, L.; Brennan, J.T.; Fader, A.; Borahay, M.A. Diet and Nutrition in Gynecological Disorders: A Focus on Clinical Studies. Nutrients 2021, 13, 1747. [Google Scholar] [CrossRef]
- Harris, H.R.; Eke, A.C.; Chavarro, J.E.; Missmer, S.A. Fruit and vegetable consumption and risk of endometriosis. Hum. Reprod. 2018, 33, 715–727. [Google Scholar] [CrossRef]
- Halpern, G.; Schor, E.; Kopelman, A. Nutritional aspects related to endometriosis. Rev. Da Assoc. Médica Bras. 2015, 61, 519–523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schindler, L.; Schindler, S.; Ussia, A.; Gordts, S.; Wattiez, A.; Koninckx, P.R. Cystic ovarian endometriosis and infertility: Arguments for an early but less aggressive surgical treatment. Obs. Gyn. Int. J. 2020, 11, 122–125. [Google Scholar]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amro, B.; Ramirez Aristondo, M.E.; Alsuwaidi, S.; Almaamari, B.; Hakim, Z.; Tahlak, M.; Wattiez, A.; Koninckx, P.R. New Understanding of Diagnosis, Treatment and Prevention of Endometriosis. Int. J. Environ. Res. Public Health 2022, 19, 6725. https://doi.org/10.3390/ijerph19116725
Amro B, Ramirez Aristondo ME, Alsuwaidi S, Almaamari B, Hakim Z, Tahlak M, Wattiez A, Koninckx PR. New Understanding of Diagnosis, Treatment and Prevention of Endometriosis. International Journal of Environmental Research and Public Health. 2022; 19(11):6725. https://doi.org/10.3390/ijerph19116725
Chicago/Turabian StyleAmro, Bedayah, Maria Eugenia Ramirez Aristondo, Shaima Alsuwaidi, Basma Almaamari, Zeinab Hakim, Muna Tahlak, Arnaud Wattiez, and Philippe R. Koninckx. 2022. "New Understanding of Diagnosis, Treatment and Prevention of Endometriosis" International Journal of Environmental Research and Public Health 19, no. 11: 6725. https://doi.org/10.3390/ijerph19116725
APA StyleAmro, B., Ramirez Aristondo, M. E., Alsuwaidi, S., Almaamari, B., Hakim, Z., Tahlak, M., Wattiez, A., & Koninckx, P. R. (2022). New Understanding of Diagnosis, Treatment and Prevention of Endometriosis. International Journal of Environmental Research and Public Health, 19(11), 6725. https://doi.org/10.3390/ijerph19116725






