Psychotherapists’ Reports regarding the Impact of the COVID-19 Pandemic on Their Patients: A Cross-National Descriptive Study Based on the Social-Ecological Model (SEM)
Abstract
:1. Introduction
2. Materials and Methods
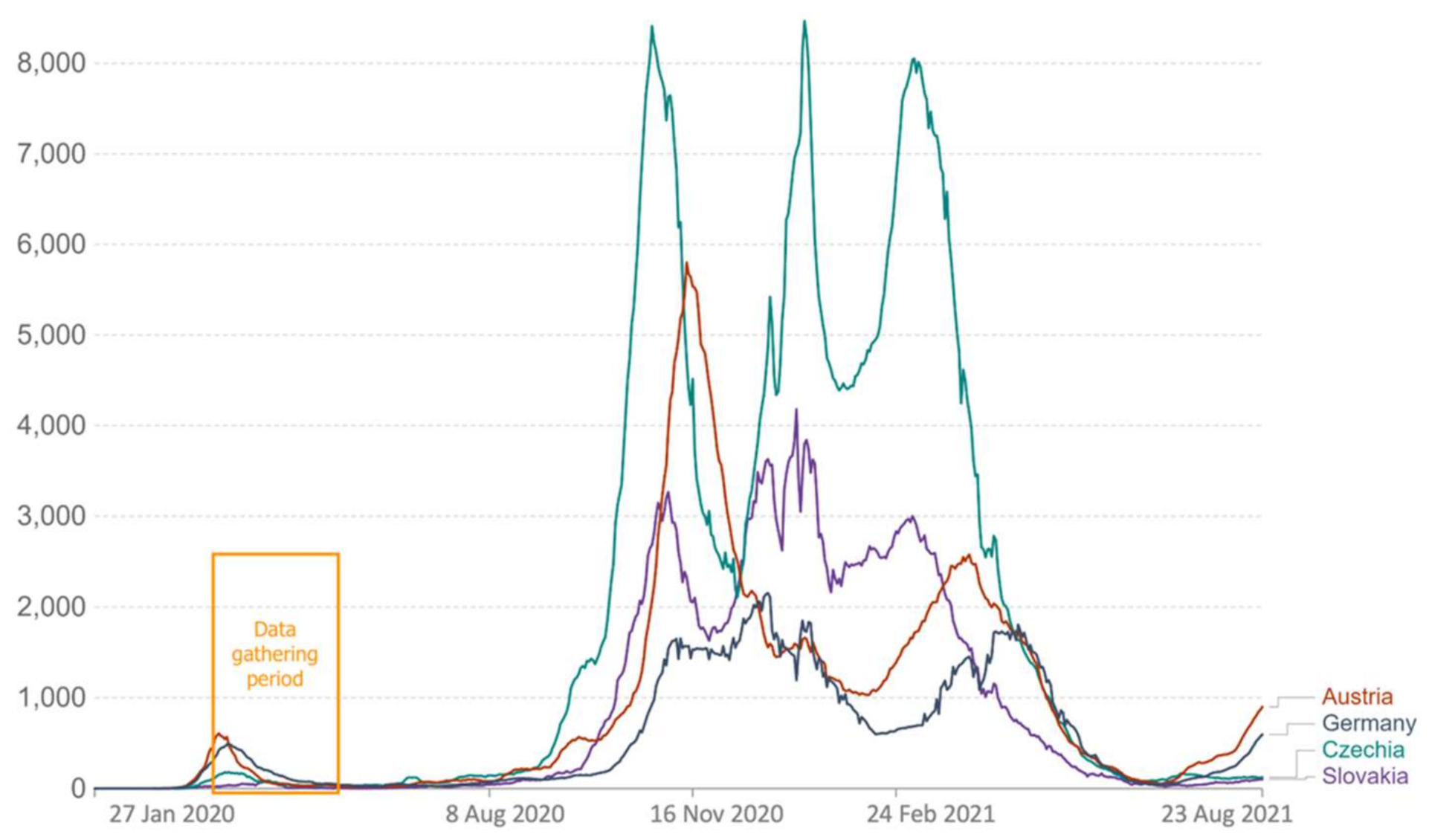
2.1. Study Design, Samples, and Data Collection
2.2. Sample Recruiting
2.3. Data Gathering Period
2.4. Analysis
2.5. Ethics
3. Results
3.1. Narrative Reports of Themes
3.1.1. Public Policy
3.1.2. Community and Societal Level
3.1.3. Interpersonal Level
3.1.4. Individual Level
3.2. Visualisation of Themes
3.3. The Most Frequent Word Stems Used according to Countries
4. Discussion
4.1. Stressful Environmental Conditions
4.2. Maladaptive and Adaptive Responses from the Public Policy to the Individual Level
4.3. Word Stem Analysis
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Serafini, G.; Parmigiani, B.; Amerio, A.; Aguglia, A.; Sher, L.; Amore, M. The psychological impact of COVID-19 on the mental health in the general population. QJM 2020, 113, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Shi, L.; Que, J.; Lu, Q.; Liu, L.; Lu, Z.; Xu, Y.; Liu, J.; Sun, Y.; Meng, S.; et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol. Psychiatry 2020, 26, 4813–4822. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological Impact of COVID-19 in Spain: Early Data Report. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 550–552. [Google Scholar] [CrossRef]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Marroquín, B.; Vine, V.; Morgan, R. Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Res. 2020, 293, 113419. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The Mental Health Consequences of COVID-19 and Physical Distancing The Need for Prevention and Early Intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef] [Green Version]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Bonsaksen, T.; Heir, T.; Schou-Bredal, I.; Ekeberg, Ø.; Skogstad, L.; Grimholt, T.K. Post-traumatic stress disorder and associated factors during the early stage of the covid-19 pandemic in Norway. Int. J. Environ. Res. Public Health 2020, 17, 9210. [Google Scholar] [CrossRef]
- Baral, S.; Logie, C.; Grosso, A.; Wirtz, A.L.; Beyrer, C. Modified Social Ecological Model: A tool to visually represent the risks and risk contexts of HIV epidemics. BMC Public Health 2013, 13, 482. [Google Scholar] [CrossRef] [Green Version]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Behav. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Nowak, B.; Brzóska, P.; Piotrowski, J.; Sedikides, C. Adaptive and maladaptive behavior during the COVID-19 pandemic: The roles of Dark Triad traits, collective narcissism, and health beliefs. Personal. Individ. Differ. 2020, 167, 110232. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.; Zielinski, M.J.; Thompson, R.G.; Willis, D.E.; Purvis, R.S.; McElfish, P.A. “This Pandemic Is Making Me More Anxious about My Welfare and the Welfare of Others:” COVID-19 Stressors and Mental Health. Int. J. Environ. Res. Public Health 2021, 18, 5680. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Taylor, S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020, 71, 102211. [Google Scholar] [CrossRef]
- Torales, J.; Higgins, M.O.; Castaldelli-maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riva, M.A.; Benedetti, M.; Cesana, G. Pandemic fear and literature: Observations from jack London’s the scarlet plague. Emerg. Infect. Dis. 2014, 20, 1753–1757. [Google Scholar] [CrossRef]
- Usher, K.; Durkin, J.; Bhullar, N. The COVID-19 pandemic and mental health impacts. Int. J. Ment. Health Nurs. 2020, 29, 315–318. [Google Scholar] [CrossRef] [Green Version]
- Qin, X.; Song, L. Addressing stigma in the context of the COVID-19 outbreak: A social-ecological approach. Infect. Control. Hosp. Epidemiol. 2020, 2019, 1433. [Google Scholar] [CrossRef]
- Fuentes, A. A (Bio)anthropological View of the COVID-19 Era Midstream: Beyond the Infection. Anthropol. Now 2020, 12, 24–32. [Google Scholar] [CrossRef]
- Nicomedes, C.J.C.; Avila, R.M.A. An analysis on the panic during COVID-19 pandemic through an online form. J. Affect. Disord. 2020, 276, 14–22. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Margraf, J. Predicting adaptive and maladaptive responses to the Coronavirus (COVID-19) outbreak: A prospective longitudinal study. Int. J. Clin. Health Psychol. 2020, 20, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Marshall, J.; Wiltshire, J.; Delva, J.; Bello, T.; Masys, A.J. Natural and Manmade Disasters: Vulnerable Populations. In Global Health Security Recognizing Vulnerabilities, Creating Opportunities; Masys, A.J., Ortiz, M.R., Izurieta, R., Eds.; Springer Nature: Cham, Switzerland, 2020; pp. 143–161. ISBN 9783030234904. [Google Scholar]
- Pieh, C.; Budimir, S.; Probst, T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J. Psychosom. Res. 2020, 136, 110186. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Chen, J.H.; Xu, Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 2020, 7, e21. [Google Scholar] [CrossRef]
- Murphy, L.; Markey, K.; O’ Donnell, C.; Moloney, M.; Doody, O. The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: A scoping review. Arch. Psychiatr. Nurs. 2021, 35, 375–394. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Stevens, C.; Conrad, R.C.; Hahm, H.C. Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID-19 pandemic among U.S. young adults with suspected and reported psychiatric diagnoses. Phychiatry Res. 2020, 292, 113345. [Google Scholar] [CrossRef]
- Richter, D.; Riedel-Heller, S.; Zuercher, S. Mental health problems in the general population during and after the first lockdown phase due to the SARS-Cov-2 pandemic: Rapid review of multi-wave studies. Epidemiol. Psychiatr. Sci. 2021, 30, e27. [Google Scholar] [CrossRef]
- Pinkham, A.E.; Ackerman, R.A.; Depp, C.A.; Harvey, P.D.; Moore, R.C. A Longitudinal Investigation of the Effects of the COVID-19 Pandemic on the Mental Health of Individuals with Pre-existing Severe Mental Illnesses. Psychiatry Res. 2020, 294, 113493. [Google Scholar] [CrossRef]
- Pan, K.; Kok, A.A.L.; Eikelenboom, M.; Horsfall, M.; Jörg, F.; Luteijn, R.A.; Rhebergen, D.; Van Oppen, P.; Giltay, E.J. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 2021, 8, 121–129. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Brewin, C.R.; Kaniasty, K.; La Greca, A.M. Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychol. Sci. Public Interest 2010, 11, 1–49. [Google Scholar] [CrossRef] [Green Version]
- Brewer, G.; Centifanti, L.; Caicedo, J.C.; Huxley, G.; Peddie, C.; Stratton, K.; Lyons, M. Experiences of Mental Distress during COVID-19: Thematic Analysis of Discussion Forum Posts for Anxiety, Depression, and Obsessive-Compulsive Disorder. Illn. Crisis Loss 2021. [Google Scholar] [CrossRef]
- Sheridan, L.; Sonia, R.; Barnett, P.; Steare, T.; Needle, J.J.; Carr, S.; Lever, B.; Francesca, T.; Julian, B.; Childs, E.; et al. Early impacts of the COVID - 19 pandemic on mental health care and on people with mental health conditions: Framework synthesis of international experiences and responses. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 56, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Burton, A.; McKinlay, A.; Aughterson, H.; Fancourt, D. Impact of the Covid-19 pandemic on the mental health and wellbeing of adults with mental health conditions in the UK: A qualitative interview study. J. Ment. Health 2021, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gillard, S.; Dare, C.; Hardy, J.; Nyikavaranda, P.; Rowan Olive, R.; Shah, P.; Birken, M.; Foye, U.; Ocloo, J.; Pearce, E.; et al. Experiences of living with mental health problems during the COVID-19 pandemic in the UK: A coproduced, participatory qualitative interview study. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1447–1457. [Google Scholar] [CrossRef] [PubMed]
- Vos, J. The Psychology of COVID-19: Building Resilience for Future Pandemics; Sage Swifts: Los Angeles, LA, USA, 2021; ISBN 9780415475976. [Google Scholar]
- Cowan, E.; Khan, M.R.; Shastry, S.; Edelman, E.J. Conceptualizing the effects of the COVID-19 pandemic on people with opioid use disorder: An application of the social ecological model. Addict. Sci. Clin. Pract. 2021, 16, 4. [Google Scholar] [CrossRef]
- Bronfenbrenner, U. The Ecology of Human Development. Experiments by Nature and Design; Harvard University Press: Cambridge, UK, 1979; Volume 148, ISBN 0674224566. [Google Scholar]
- Colorafi, K.J.; Evans, B. Qualitative Descriptive Methods in Health Science Research. HERD Health Environ. Res. Des. J. 2016, 9, 16–25. [Google Scholar] [CrossRef]
- Mayring, P. Qualitative Forschungsdesigns in der Psychologie. Handb. Qual. Forsch. Der Psychol. 2018, 1–15. [Google Scholar] [CrossRef]
- Doyle, L.; McCabe, C.; Keogh, B.; Brady, A.; McCann, M. An overview of the qualitative descriptive design within nursing research. J. Res. Nurs. 2020, 25, 443–455. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; Neal, L.O.; Mcleod, L.; Delacqua, G.; Delacqua, F.; Duda, S.N.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Probst, T.; Stippl, P.; Pieh, C. Changes in provision of psychotherapy in the early weeks of the COVID-19 lockdown in Austria. Int. J. Environ. Res. Public Health 2020, 17, 3815. [Google Scholar] [CrossRef]
- Humer, E.; Pieh, C.; Kuska, M.; Barke, A.; Doering, B.K.; Gossmann, K.; Trnka, R.; Meier, Z.; Kascakova, N.; Tavel, P.; et al. Provision of Psychotherapy during the COVID-19 Pandemic among Czech, German and Slovak Psychotherapists. Int. J. Environ. Res. Public Health 2020, 17, 4811. [Google Scholar] [CrossRef]
- Hsieh, H.-F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Chalovich, J.M.; Eisenberg, E. Psychological Stress and the Human Immune System: A Meta- Analytic Study of 30 Years of Inquiry Suzanne. Magn Reson. Imaging 2013, 31, 477–479. [Google Scholar]
- Seiler, A.; Fagundes, C.P.; Christian, L.M. The impact of everyday stressors on the immune system and health. In Stress Challenges and Immunity in Space; Choukèr, A., Ed.; Springer: Cham, Switzerland, 2019; pp. 71–92. ISBN 9783030169961. [Google Scholar]
- Cacioppo, J.T.; Hawkley, L.C.; Norman, G.J.; Berntson, G.G. Social Isolation. Ann. N. Y. Acad. Sci. 2011, 1231, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Garbarino, S.; Lanteri, P.; Bragazzi, N.L.; Magnavita, N.; Scoditti, E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun. Biol. 2021, 4, 1304. [Google Scholar] [CrossRef] [PubMed]
- Salton, G. Automatic text analysis. J. Am. Soc. Inf. Sci. 1979, 30, 109–127. [Google Scholar] [CrossRef]
- Romsdorfer, H.; Pfister, B. Text analysis and language identification for polyglot text-to-speech synthesis. Speech Commun. 2007, 49, 697–724. [Google Scholar] [CrossRef] [Green Version]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A nationwide survey of psychological distress among italian people during the covid-19 pandemic: Immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Presti, G.; McHugh, L.; Gloster, A.; Karekla, M.; Hayes, S.C. The dynamics of fear at the time of COVID-19: A contextual behavioral science perspective. Clin. Neuropsychiatry 2020, 17, 65–71. [Google Scholar] [CrossRef]
- Abadi, D.; Arnaldo, I.; Fischer, A. Anxious and Angry: Emotional Responses to the COVID-19 Threat. Front. Psychol. 2021, 12, 3516. [Google Scholar] [CrossRef]
- Hills, S.; Eraso, Y. Factors associated with non-adherence to social distancing rules during the COVID-19 pandemic: A logistic regression analysis. BMC Public Health 2021, 21, 352. [Google Scholar] [CrossRef]
- Volk, S. Political Performances of Control During COVID-19: Controlling and Contesting Democracy in Germany. Front. Political Sci. 2021, 3, 38. [Google Scholar] [CrossRef]
- Nachtwey, O.; Schäfer, R.; Frei, N. Political Sociology of the Corona Protests; University of Basel: Basel, Switzerland, 2020. [Google Scholar]
- European Union Agceny for Fundamental Rights (FRA). Coronavirus COVID-19 Outbreak in the EU. Fundamental Rights Implications; European Union Agceny for Fundamental Rights (FRA): Bratislava, Slovakia, 2020. [Google Scholar]
- European Union Agency for Fundamental Rights (FRA). Coronavirus Pandemic in the EU—Fundamental Rights Implications; European Union Agency for Fundamental Rights (FRA): Prague, Czech Republic, 2020. [Google Scholar]
- Leiblfinger, M.; Prieler, V.; Rogoz, M.; Sekulová, M. Confronted with COVID-19: Migrant live-in care during the pandemic. Glob. Soc. Policy 2021, 21, 490–507. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, E.; Renzetti, S.; Volta, M.; Donato, F.; Calza, S.; Placidi, D.; Lucchini, R.G.; Rota, M. COVID-19 incidence and mortality in Lombardy, Italy: An ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environ. Res. 2021, 195, 110777. [Google Scholar] [CrossRef] [PubMed]
- Allington, D.; Duffy, B.; Wessely, S.; Dhavan, N.; Rubin, J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol. Med. 2021, 51, 1763–1769. [Google Scholar] [CrossRef] [PubMed]
- OECD. Tackling the Mental Health Impact of the COVID-19 Crisis: An Integrated, Whole-of-Society Response; OECD: Paris, France, 2021; pp. 1–16. [Google Scholar]
- Law, P.C.F.; Too, L.S.; Butterworth, P.; Witt, K.; Reavley, N.; Milner, A.J. A systematic review on the effect of work-related stressors on mental health of young workers. Int. Arch. Occup. Environ. Health 2020, 93, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Thorell, L.B.; Skoglund, C.; de la Peña, A.G.; Baeyens, D.; Fuermaier, A.B.M.; Groom, M.J.; Mammarella, I.C.; van der Oord, S.; van den Hoofdakker, B.J.; Luman, M.; et al. Parental experiences of homeschooling during the COVID-19 pandemic: Differences between seven European countries and between children with and without mental health conditions. Eur. Child. Adolesc. Psychiatry 2021, 31, 649–661. [Google Scholar] [CrossRef]
- He, X.; Zhang, Y.; Chen, M.; Zhang, J.; Zou, W.; Luo, Y. Media Exposure to COVID-19 Predicted Acute Stress: A Moderated Mediation Model of Intolerance of Uncertainty and Perceived Social Support. Front. Psychiatry 2021, 11, 1552. [Google Scholar] [CrossRef]
- Thompson, R.R.; Jones, N.M.; Holman, E.A.; Silver, R.C. Media exposure to mass violence events can fuel a cycle of distress. Sci. Adv. 2019, 5, eaav3502. [Google Scholar] [CrossRef] [Green Version]
- Holman, E.A.; Garfin, D.R.; Lubens, P.; Silver, R.C. Media Exposure to Collective Trauma, Mental Health, and Functioning: Does It Matter What You See? Clin. Psychol. Sci. 2020, 8, 111–124. [Google Scholar] [CrossRef]
- Trnka, R.; Lorencova, R. Fear, Anger, and Media-Induced Trauma During the Outbreak of COVID-19 in the Czech Republic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 546–549. [Google Scholar] [CrossRef]
- Kato, T.A.; Sartorius, N.; Shinfuku, N. Forced social isolation due to COVID-19 and consequent mental health problems: Lessons from hikikomori. Psychiatry Clin. Neurosci. 2020, 74, 506–507. [Google Scholar] [CrossRef] [PubMed]
- Kofman, Y.B.; Garfin, D.R. Home is not always a haven: The domestic violence crisis amid the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S199–S201. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.L.; Wasileski, G. The Struggle to Address Woman Battering in Slovakia: Stories From Service Providers. Violence Against Women 2015, 21, 734–757. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, M.; Lionetti, F.; Setti, A.; Fasolo, M. Parenting Stress During the COVID-19 Outbreak: Socioeconomic and Environmental Risk Factors and Implications for Children Emotion Regulation. Fam. Process 2021, 60, 639–653. [Google Scholar] [CrossRef]
- Clemens, V.; Köhler-Dauner, F.; Ziegenhain, U.; Fegert, J.M. Predictors of Parental Coping During the Covid-19 Pandemic: A Survey in Germany. Front. Psychol. 2021, 12, 3830. [Google Scholar] [CrossRef]
- El-Osta, A.; El-Osta, A.; Alaa, A.; Webber, I.; Riboli Sasco, E.; Bagkeris, E.; Millar, H.; Vidal-Hall, C.; Majeed, A. How is the COVID-19 lockdown impacting the mental health of parents of school-age children in the UK? A cross-sectional online survey. BMJ Open 2021, 11, e043397. [Google Scholar] [CrossRef]
- Morelli, M.; Cattelino, E.; Baiocco, R.; Trumello, C.; Babore, A.; Candelori, C.; Chirumbolo, A. Parents and Children During the COVID-19 Lockdown: The Influence of Parenting Distress and Parenting Self-Efficacy on Children’s Emotional Well-Being. Front. Psychol. 2020, 11, 2584. [Google Scholar] [CrossRef]
- Whitehead, B.R.; Torossian, E.; Arbor, A. Older Adults’ Experience of the COVID-19 Pandemic: A Mixed-Methods Analysis of Stresses and Joys. Gerontologist 2020, 61, 36–47. [Google Scholar] [CrossRef]
- McKinlay, A.; Fancourt, D.; Burton, A. “It makes you realise your own mortality.” A qualitative study on mental health of older adults in the UK during COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Gonçalves Júnior, J.; Moreira, M.M.; Rolim Neto, M.L. Silent Cries, Intensify the Pain of the Life That Is Ending: The COVID-19 Is Robbing Families of the Chance to Say a Final Goodbye. Front. Psychiatry 2020, 11, 10–12. [Google Scholar] [CrossRef]
- Moore, K.A.; March, E. Socially Connected during COVID-19: Online social connections mediate the relationship between loneliness and positive coping strategies. J. Stress Trauma Anxiety Resil. (J-STAR) 2022, 1, 1–20. [Google Scholar] [CrossRef]
- Schaffler, Y.; Gächter, A.; Dale, R.; Jesser, A.; Probst, T.; Pieh, C. Concerns and Support after One Year of COVID-19 in Austria: A Qualitative Study Using Content Analysis with 1505 Participants. Int. J. Environ. Res. Public Health 2021, 18, 8218. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, K.M.; Drawve, G.; Harris, C. Facing new fears during the COVID-19 pandemic: The State of America’s mental health. J. Anxiety Disord. 2020, 75, 102291. [Google Scholar] [CrossRef] [PubMed]
- Levkovich, I.; Shinan-Altman, S. Impact of the COVID-19 pandemic on stress and emotional reactions in Israel: A mixed-methods study. Int. Health 2021, 13, 358–366. [Google Scholar] [CrossRef] [PubMed]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Dailey, N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020, 290, 113117. [Google Scholar] [CrossRef] [PubMed]
- Gu, S.; He, Z.; Sun, L.; Jiang, Y.; Xu, M.; Feng, G.; Ma, X.; Wang, F.; Huang, J.H. Effects of Coronavirus-19 Induced Loneliness on Mental Health: Sleep Quality and Intolerance for Uncertainty as Mediators. Front. Psychiatry 2021, 12, 1606. [Google Scholar] [CrossRef]
- Imbrogno, S. Family policy in the Soviet Union. Int. J. Sociol. Fam. 1986, 16, 165–180. [Google Scholar]
- Puterman, E.; Delongis, A.; Lee-Baggley, D.; Greenglass, E. Coping and health behaviours in times of global health crises: Lessons from SARS and West Nile. Glob. Public Health 2009, 4, 69–81. [Google Scholar] [CrossRef]
- Taylor, S. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease; Cambridge Scholars Publishing: Newcastle upon Tyne, UK, 2019; ISBN 9780415475976. [Google Scholar]




| % | ||||
|---|---|---|---|---|
| English Equivalent to Local Word Stem | Austria | Germany | Czechia | Slovakia |
| Fear/anxiety (anxieties, anxious…) * | 28.5 | 41.7 | 24.0 24.0 | 24.7 23.6 |
| worry, worries | 20.5 | 19.2 | 36.5 | 20.2 |
| restriction(s), limitation(s), -ing | 12.7 | 25.0 | 18.3 | 16.9 |
| uncertainty, -ies | 8.9 | 6.7 | 20.2 | 16.9 |
| family, -ar, -ies, inkl. parent(s) | 5.8 | 6.7 | 19.2 | 19.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schaffler, Y.; Kuska, M.; Barke, A.; Doering, B.K.; Gossmann, K.; Meier, Z.; Kascakova, N.; Tavel, P.; Humer, E.; Pieh, C.; et al. Psychotherapists’ Reports regarding the Impact of the COVID-19 Pandemic on Their Patients: A Cross-National Descriptive Study Based on the Social-Ecological Model (SEM). Int. J. Environ. Res. Public Health 2022, 19, 6825. https://doi.org/10.3390/ijerph19116825
Schaffler Y, Kuska M, Barke A, Doering BK, Gossmann K, Meier Z, Kascakova N, Tavel P, Humer E, Pieh C, et al. Psychotherapists’ Reports regarding the Impact of the COVID-19 Pandemic on Their Patients: A Cross-National Descriptive Study Based on the Social-Ecological Model (SEM). International Journal of Environmental Research and Public Health. 2022; 19(11):6825. https://doi.org/10.3390/ijerph19116825
Chicago/Turabian StyleSchaffler, Yvonne, Martin Kuska, Antonia Barke, Bettina K. Doering, Katharina Gossmann, Zdenek Meier, Natalia Kascakova, Peter Tavel, Elke Humer, Christoph Pieh, and et al. 2022. "Psychotherapists’ Reports regarding the Impact of the COVID-19 Pandemic on Their Patients: A Cross-National Descriptive Study Based on the Social-Ecological Model (SEM)" International Journal of Environmental Research and Public Health 19, no. 11: 6825. https://doi.org/10.3390/ijerph19116825
APA StyleSchaffler, Y., Kuska, M., Barke, A., Doering, B. K., Gossmann, K., Meier, Z., Kascakova, N., Tavel, P., Humer, E., Pieh, C., Stippl, P., Schimböck, W., Haid, B., & Probst, T. (2022). Psychotherapists’ Reports regarding the Impact of the COVID-19 Pandemic on Their Patients: A Cross-National Descriptive Study Based on the Social-Ecological Model (SEM). International Journal of Environmental Research and Public Health, 19(11), 6825. https://doi.org/10.3390/ijerph19116825






