Motherhood and Treatment Outcome in Female Patients with Compulsive Buying–Shopping Disorder
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Treatment
2.2.1. Main Elements of the Treatment Program
2.2.2. Main Outcome Variables
2.3. Instruments
2.3.1. Diagnostic Criteria for CBSD
2.3.2. Symptom Checklist-Revised (SCL-90-R)
2.3.3. Other Sociodemographic and Clinical Variables
2.4. Procedure
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Comparison between the Groups at Baseline
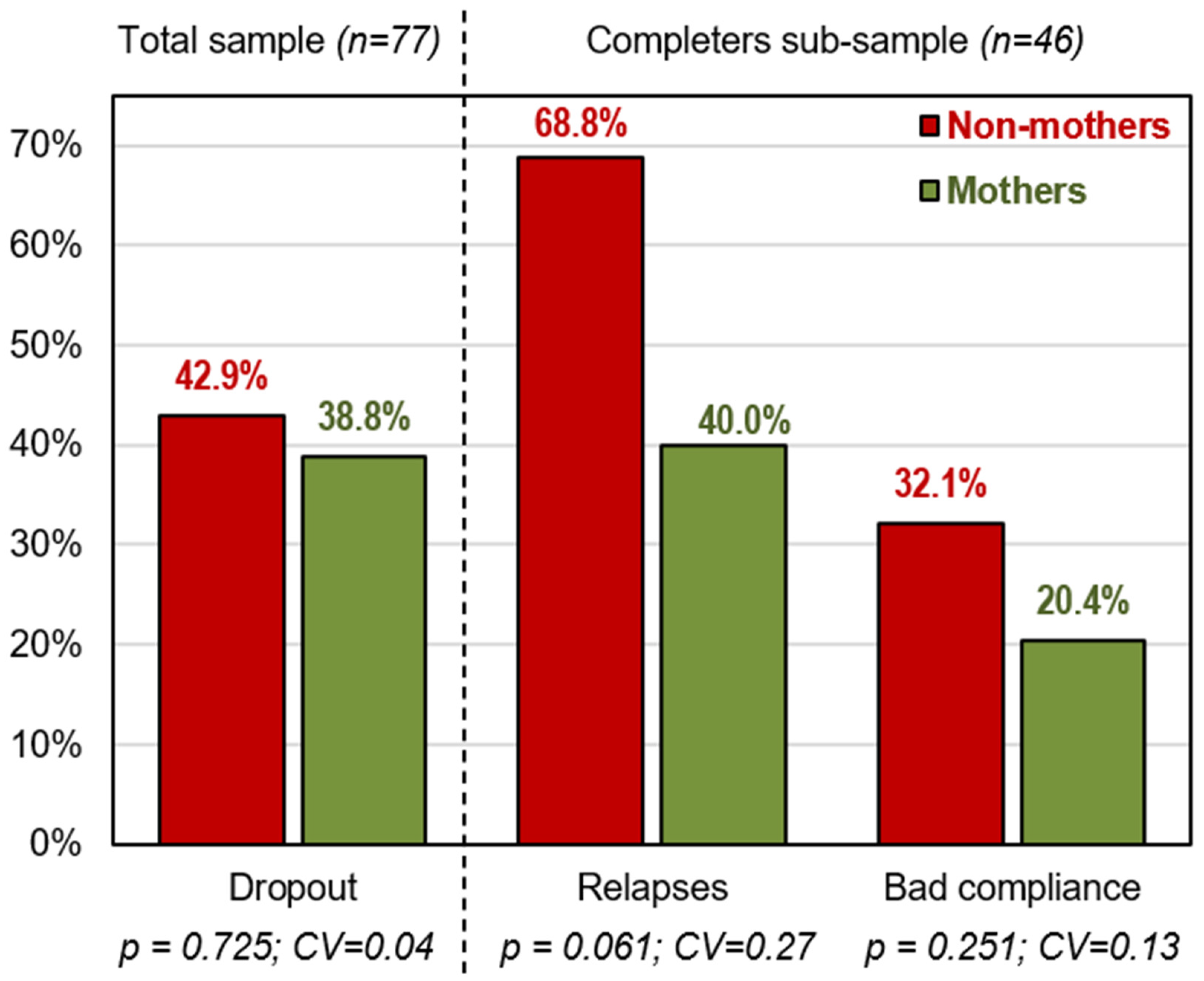
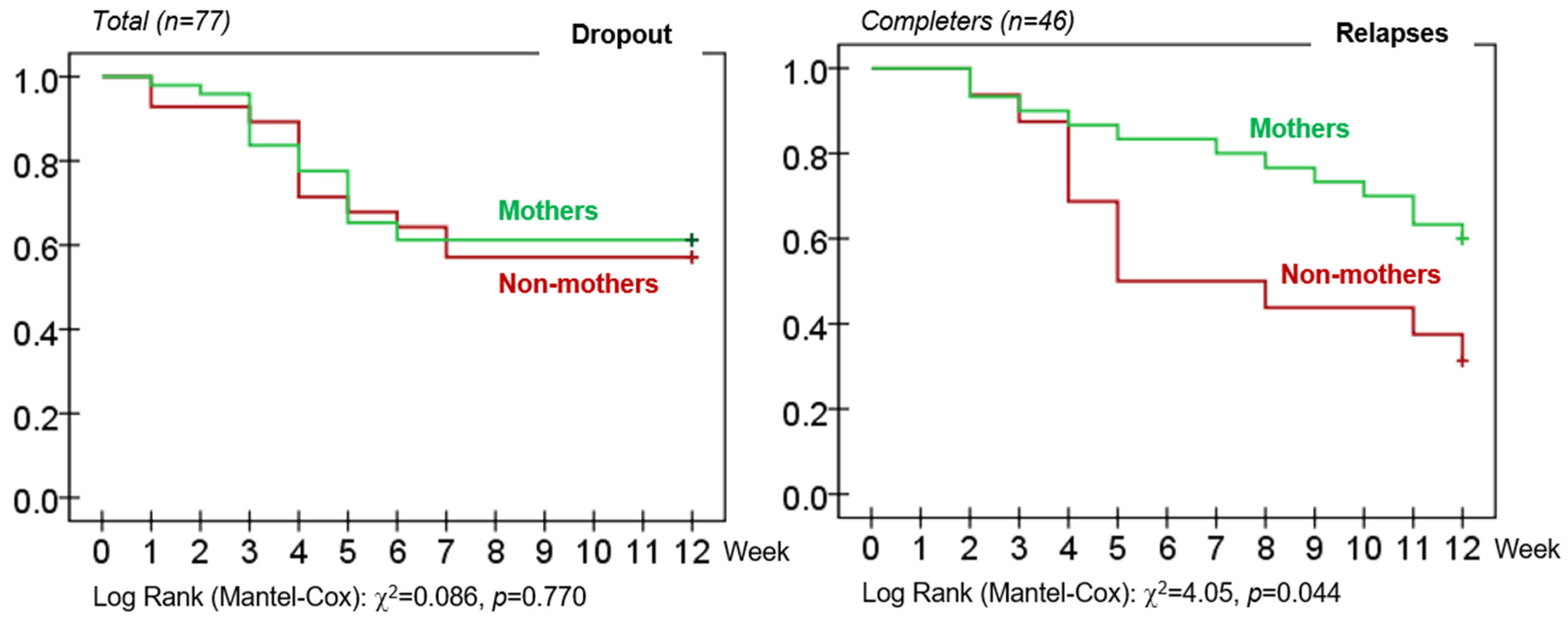
3.3. Comparison between the Groups for the CBT Outcomes during the Treatment
3.4. Survival Analysis
4. Discussion
4.1. Research and Clinical Implications
4.2. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barnett, E.R.; Knight, E.; Herman, R.J.; Amarakaran, K.; Jankowski, M.K. Difficult binds: A systematic review of facilitators and barriers to treatment among mothers with substance use disorders. J. Subst. Abus. Treat. 2021, 126, 108341. [Google Scholar] [CrossRef] [PubMed]
- Secco, L.; Letourneau, N.; Campbell, M.A.; Craig, S.; Colpitts, J. Stresses, strengths, and experiences of mothers engaged in methadone maintenance treatment. J. Addict. Nurs. 2014, 25, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Lander, L.; Howsare, J.; Byrne, M. The Impact of Substance Use Disorders on Families and Children: From Theory to Practice. Soc. Work Public Health 2013, 28, 194–205. [Google Scholar] [CrossRef]
- Marcellus, L. A Grounded Theory of Mothering in the Early Years for Women Recovering From Substance Use. J. Fam. Nurs. 2017, 23, 341–365. [Google Scholar] [CrossRef]
- Mackintosh, V.; Knight, T. The notion of self in the journey back from addiction. Qual. Health Res. 2012, 22, 1094–1101. [Google Scholar] [CrossRef] [PubMed]
- Hine, R.H.; Maybery, D.J.; Goodyear, M.J. Identity in recovery for mothers with a mental illness: A literature review. Psychiatr. Rehabil. J. Educ. Publ. Found. 2018, 41, 16. [Google Scholar] [CrossRef]
- Nicholson, J.; Henry, A.D. Achieving the goal of evidence-based psychiatric rehabilitation practices for mothers with mental illnesses. Psychiatr. Rehabil. J. 2003, 27, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Benoit, C.; Magnus, S.; Phillips, R.; Marcellus, L.; Charbonneau, S. Complicating the dominant morality discourse: Mothers and fathers’ constructions of substance use during pregnancy and early parenthood. Int. J. Equity Health 2015, 14, 72. [Google Scholar] [CrossRef]
- Tuchman, E. Women and addiction: The importance of gender issues in substance abuse research. J. Addict. Dis. 2010, 29, 127–138. [Google Scholar] [CrossRef]
- Brown, S. A Place Called Self: Women, Sobriety & Radical Transformation; Simon and Schuster: New York, NY, USA, 2009. [Google Scholar]
- Elms, N.; Link, K.; Newman, A.; Brogly, S.B. Need for women-centered treatment for substance use disorders: Results from focus group discussions. Harm Reduct. J. 2018, 15, 40. [Google Scholar] [CrossRef]
- Adams, Z.M.; Ginapp, C.M.; Price, C.R.; Qin, Y.; Madden, L.M.; Yonkers, K.; Meyer, J.P. “A good mother”: Impact of motherhood identity on women’s substance use and engagement in treatment across the lifespan. J. Subst. Abus. Treat. 2021, 130, 108474. [Google Scholar] [CrossRef] [PubMed]
- Gavriel-Fried, B.; Ajzenstadt, M. Pathological Women Gamblers: Gender-Related Aspects of Control. Sex Roles 2012, 66, 128–142. [Google Scholar] [CrossRef]
- Suchman, E.; Cindy, L.D.; Thomas, J.M.; Rachel, D.; Linda, C.; Mayes, J.B. Mothering from the Inside Out: Results of a second randomized clinical trial testing a mentalization-based intervention for mothers in addiction treatment. Dev. Psychopathol. 2017, 29, 617–636. [Google Scholar] [CrossRef] [PubMed]
- Lejoyeux, M.; Weinstein, A. Compulsive buying. Am. J. Drug Alcohol Abus. 2010, 36, 248–253. [Google Scholar] [CrossRef]
- Brand, M.; Rumpf, H.-J.; Demetrovics, Z.; MÜller, A.; Stark, R.; King, D.L.; Goudriaan, A.E.; Mann, K.; Trotzke, P.; Fineberg, N.A.; et al. Which conditions should be considered as disorders in the International Classification of Diseases (ICD-11) designation of “other specified disorders due to addictive behaviors”? J. Behav. Addict. 2020. [Google Scholar] [CrossRef]
- Müller, A.; Laskowski, N.M.; Trotzke, P.; Ali, K.; Fassnacht, D.B.; de Zwaan, M.; Brand, M.; Häder, M.; Kyrios, M. Proposed diagnostic criteria for compulsive buying-shopping disorder: A Delphi expert consensus study. J. Behav. Addict. 2021, 10, 208–222. [Google Scholar] [CrossRef]
- Hague, B.; Hall, J.; Kellett, S. Treatments for compulsive buying: A systematic review of the quality, effectiveness and progression of the outcome evidence. J. Behav. Addict. 2016, 5, 379–394. [Google Scholar] [CrossRef]
- Jimenez-Murcia, S.; Aymamı-Sanroma, N.; Gomez-Peña, M.; Alvarez-Moya, E.; Vallejo, J. Protocols de Tractament Cognitivoconductual pel joc Patològic i d’altres Addiccions no Tòxiques Departamen; Hospital Universitari de Bellvitge: Barcelona, Spain, 2006. [Google Scholar]
- Jiménez-Murcia, S.; Granero, R.; Fernández-Aranda, F.; Arcelus, J.; Aymamí, M.N.; Gomez-Peña, M.; Tárrega, S.; Moragas, L.; Del Pino-Gutiérrez, A.; Sauchelli, S.; et al. Predictors of outcome among pathological gamblers receiving cognitive behavioral group therapy. Eur. Addict. Res. 2015, 21, 169–178. [Google Scholar] [CrossRef]
- Black, D.W. Compulsive buying disorder: A review of the evidence. CNS Spectr. 2007, 12, 124–132. [Google Scholar] [CrossRef]
- Granero, R.; Fernandez-Aranda, F.; Mestre-Bach, G.; Steward, T.; Baño, M.; Agüera, Z.; Mallorquí-Bagué, N.; Aymamí, N.; Gomez-Peña, M.; Sancho, M.; et al. Cognitive behavioral therapy for compulsive buying behavior: Predictors of treatment outcome. Eur. Psychiatry 2017, 39, 57–65. [Google Scholar] [CrossRef]
- Jimenez-Murcia, S.; Aymamí, N.; Gómez-Peña, M.; Santamaría, J.J.; Álvarez-Moya, E.; Fernández-Aranda, F.; Granero, R.; Penelo, E.; Bueno, B.; Moragas, L.; et al. Does exposure and response prevention improve the results of group cognitive-behavioural therapy for male slot machine pathological gamblers? Br. J. Clin. Psychol. 2012, 51, 54–71. [Google Scholar] [CrossRef] [PubMed]
- McElroy, S.L.; Keck, P.E.; Pope, H.G.; Smith, J.M.; Strakowski, S.M. Compulsive buying: A report of 20 cases. J. Clin. Psychiatry 1994, 55, 242–248. [Google Scholar] [PubMed]
- Tavares, H.; Lobo, D.S.S.; Fuentes, D.; Black, D.W. Compulsive buying disorder:a review and a case vignette. Braz. J. Psychiatry 2008, 30, S16–S23. [Google Scholar] [CrossRef] [PubMed]
- APA. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 11th ed.; World Health Organization: Geneva, Switzerland, 2019.
- Müller, A.; Mitchell, J.E.; de Zwaan, M. Compulsive buying. Am. J. Addict. 2015, 24, 132–137. [Google Scholar] [CrossRef]
- Derogatis, L. Administration, Scoring and Procedures Manual. Baltimore: Clinical Psychometric Research; SCL-90-R; Clinical Psychometric Research: Towson, MD, USA, 1990. [Google Scholar]
- Derogatis, L.R. SCL-90-R. Cuestionario de 90 Síntomas-Manual; TEA Editorial: Madrid, Spain, 2002. [Google Scholar]
- Hollingshead, A.B. Four factor index of social status. Ale J. Sociol. 2011, 8, 21–51. [Google Scholar]
- Stata-Corp. Stata Statistical Software: Release 17; College Station TSPP, Ed.; StataCorp LLC: College Station, TX, USA, 2021. [Google Scholar]
- Singer, J.D.; Willett, J.B.; Willett, J.B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Kelley, K.; Preacher, K.J. On effect size. Psychol. Methods 2012, 17, 137–152. [Google Scholar] [CrossRef]
- Ferguson, C.J. An Effect Size Primer: A Guide for Clinicians and Researchers. In Methodological Issues and Strategies in Clinical Research; Kazdin, A.E., Ed.; American Psychological Association: Washington, DC, USA, 2009; pp. 532–538. [Google Scholar]
- Finner, H.; Roters, M. On the false discovery rate and expected type I errors. Biom. J. Wiley Online Libr. 2001, 43, 985–1005. [Google Scholar] [CrossRef]
- Gunn, A.; Samuels, G.M. Promoting Recovery Identities Among Mothers with Histories of Addiction: Strategies of Family Engagement. Fam. Process. 2020, 59, 94–110. [Google Scholar] [CrossRef]
- Lin, C.; Wu, Z.; Detels, R. Family support, quality of life and concurrent substance use among methadone maintenance therapy clients in China. Public Health 2011, 125, 269–274. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3624763/pdf/nihms412728.pdf (accessed on 14 September 2021). [CrossRef]
- Ellis, B.; Bernichon, T.; Yu, P.; Roberts, T.; Herrell, J.M. Effect of social support on substance abuse relapse in a residential treatment setting for women. Eval. Program. Plann. 2004, 27, 213–221. [Google Scholar] [CrossRef]
- Patricia, J.K.; Beth Blacksin, E. Factors Affecting Substance Abuse Treatment Completion for Women. Issues Ment. Health Nurs. 2001, 22, 287–304. [Google Scholar] [CrossRef]
- Hser, Y.-I.; Evans, E.; Huang, D.; Messina, N. Long-term outcomes among drug-dependent mothers treated in women-only versus mixed-gender programs. J. Subst. Abus. Treat. 2011, 41, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, S.F.; Brooks, A.J.; Gordon, S.M.; Green, C.; Kropp, F.; McHugh, R.K.; Lincoln, M.; Hien, D.; Miele, G.M. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug Alcohol Depend. 2007, 86, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Mitrani, V.B.; Feaster, D.J.; Mccabe, B.E. Malaise, motivation and motherhood:predictors of engagement in behavioural interventions. Aids Behav. 2011, 15, 396–406. [Google Scholar] [CrossRef]
- Villegas, N.A.; Chodhury, S.M.; Mitrani, V.B.; Guerra, J. Mothers in substance abuse recovery: Perspectives on motivators, challenges and family involvement. Int. J. High. Risk Behav. Addict. 2017, 6, e32558. [Google Scholar] [CrossRef]
| Total (n = 77) | Non-Mothers (n = 28) | Mothers (n = 49) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p | C-V | ||
| Education level | Primary | 29 | 37.7% | 6 | 21.4% | 23 | 46.9% | 0.077 | 0.26 † |
| Secondary | 29 | 37.7% | 14 | 50.0% | 15 | 30.6% | |||
| University | 19 | 24.7% | 8 | 28.6% | 11 | 22.4% | |||
| Civil status | Single | 27 | 35.1% | 21 | 75.0% | 6 | 12.2% | <0.001 * | 0.64 † |
| Married-in couple | 40 | 51.9% | 5 | 17.9% | 35 | 71.4% | |||
| Divorced-separated | 10 | 13.0% | 2 | 7.1% | 8 | 16.3% | |||
| Social index | Mean-high or high | 17 | 22.1% | 6 | 21.4% | 11 | 22.4% | <0.017 | 0.37 † |
| Mean | 7 | 9.1% | 5 | 17.9% | 2 | 4.1% | |||
| Mean-low | 24 | 31.2% | 12 | 42.9% | 12 | 24.5% | |||
| Low | 29 | 37.7% | 5 | 17.9% | 24 | 49.0% | |||
| Employment | Unemployed | 35 | 45.5% | 12 | 42.9% | 23 | 46.9% | 0.729 | 0.04 |
| Employed | 42 | 54.5% | 16 | 57.1% | 26 | 53.1% | |||
| Mean | SD | Mean | SD | Mean | SD | p | |d| | ||
| Age (years-old) | 43.03 | 10.59 | 38.04 | 9.31 | 45.88 | 10.30 | 0.001 * | 0.80 † | |
| Non-Mothers (n = 28) | Mothers (n = 49) | ||||||
|---|---|---|---|---|---|---|---|
| Psychopathology (SCL-90-R) | α | Mean | SD | Mean | SD | p | |d| |
| Somatization | 0.907 | 1.64 | 1.17 | 1.75 | 1.09 | 0.685 | 0.10 |
| Obsessive/compulsive | 0.898 | 2.12 | 1.09 | 1.83 | 1.04 | 0.267 | 0.28 |
| Interpersonal sensitive | 0.871 | 1.77 | 1.05 | 1.53 | 1.00 | 0.356 | 0.23 |
| Depressive | 0.914 | 2.38 | 1.12 | 2.28 | 1.07 | 0.711 | 0.09 |
| Anxiety | 0.908 | 1.76 | 1.06 | 1.70 | 1.20 | 0.841 | 0.05 |
| Hostility | 0.860 | 1.56 | 1.25 | 1.23 | 0.92 | 0.212 | 0.30 |
| Phobic anxiety | 0.844 | 1.09 | 1.15 | 0.97 | 1.03 | 0.638 | 0.12 |
| Paranoid Ideation | 0.808 | 1.60 | 1.04 | 1.33 | 0.94 | 0.275 | 0.27 |
| Psychotic | 0.831 | 1.29 | 0.95 | 1.24 | 0.97 | 0.828 | 0.05 |
| GSI score | 0.981 | 1.75 | 0.92 | 1.65 | 0.91 | 0.655 | 0.11 |
| PST score | 0.981 | 60.32 | 21.19 | 57.04 | 21.47 | 0.541 | 0.15 |
| PSDI score | 0.981 | 2.41 | 0.76 | 2.43 | 0.66 | 0.923 | 0.02 |
| Onset-duration buying problems | Mean | SD | Mean | SD | p | |d| | |
| Age of onset of buying problems | 28.53 | 10.74 | 37.94 | 12.22 | 0.001 * | 0.82 † | |
| Duration of buying problems | 7.18 | 6.90 | 8.38 | 8.19 | 0.517 | 0.16 | |
| Buying related variables | n | % | n | % | p | C-V | |
| Max. money spent/episode | Less 50 € | 10 | 35.7% | 27 | 55.1% | 0.235 | 0.23 † |
| 50 to 100 € | 1 | 3.6% | 0 | 0.0% | |||
| 100 to 300 € | 6 | 21.4% | 7 | 14.3% | |||
| More than 300 € | 11 | 39.3% | 15 | 30.6% | |||
| Mean money spent/episode | Less 50 € | 21 | 75.0% | 39 | 79.6% | 0.580 | 0.16 |
| 50 to 100 € | 4 | 14.3% | 3 | 6.1% | |||
| 100 to 300 € | 2 | 7.1% | 6 | 12.2% | |||
| More 300 € | 1 | 3.6% | 1 | 2.0% | |||
| Debts due to buying behaviors | No | 18 | 64.3% | 22 | 44.9% | 0.101 | 0.19 |
| Yes | 10 | 35.7% | 27 | 55.1% | |||
| Family support | No | 3 | 10.7% | 3 | 6.1% | 0.082 | 0.24 † |
| Partial | 2 | 7.1% | 13 | 26.5% | |||
| Complete | 23 | 82.1% | 33 | 67.3% | |||
| Prevalence substances use/abuse | n | % | n | % | p | C-V | |
| Tobacco | 12 | 42.9% | 14 | 28.6% | 0.202 | 0.15 | |
| Alcohol | 2 | 7.1% | 0 | 0.0% | 0.042 * | 0.22 † | |
| Other illegal drugs | 1 | 3.6% | 1 | 2.0% | 0.690 | 0.05 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mestre-Bach, G.; Granero, R.; Casalé-Salayet, G.; Fernández-Aranda, F.; Müller, A.; Brand, M.; Gómez-Peña, M.; Moragas, L.; Sánchez, I.; Camacho-Barcia, L.; et al. Motherhood and Treatment Outcome in Female Patients with Compulsive Buying–Shopping Disorder. Int. J. Environ. Res. Public Health 2022, 19, 7075. https://doi.org/10.3390/ijerph19127075
Mestre-Bach G, Granero R, Casalé-Salayet G, Fernández-Aranda F, Müller A, Brand M, Gómez-Peña M, Moragas L, Sánchez I, Camacho-Barcia L, et al. Motherhood and Treatment Outcome in Female Patients with Compulsive Buying–Shopping Disorder. International Journal of Environmental Research and Public Health. 2022; 19(12):7075. https://doi.org/10.3390/ijerph19127075
Chicago/Turabian StyleMestre-Bach, Gemma, Roser Granero, Gemma Casalé-Salayet, Fernando Fernández-Aranda, Astrid Müller, Matthias Brand, Mónica Gómez-Peña, Laura Moragas, Isabel Sánchez, Lucía Camacho-Barcia, and et al. 2022. "Motherhood and Treatment Outcome in Female Patients with Compulsive Buying–Shopping Disorder" International Journal of Environmental Research and Public Health 19, no. 12: 7075. https://doi.org/10.3390/ijerph19127075
APA StyleMestre-Bach, G., Granero, R., Casalé-Salayet, G., Fernández-Aranda, F., Müller, A., Brand, M., Gómez-Peña, M., Moragas, L., Sánchez, I., Camacho-Barcia, L., Villena, A., Lara-Huallipe, M. L., & Jiménez-Murcia, S. (2022). Motherhood and Treatment Outcome in Female Patients with Compulsive Buying–Shopping Disorder. International Journal of Environmental Research and Public Health, 19(12), 7075. https://doi.org/10.3390/ijerph19127075










