The Effects of COVID-19 Lockdown on the Perception of Physical Activity and on the Perception of Musculoskeletal Symptoms in Computer Workers: Comparative Longitudinal Study Design
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Procedures
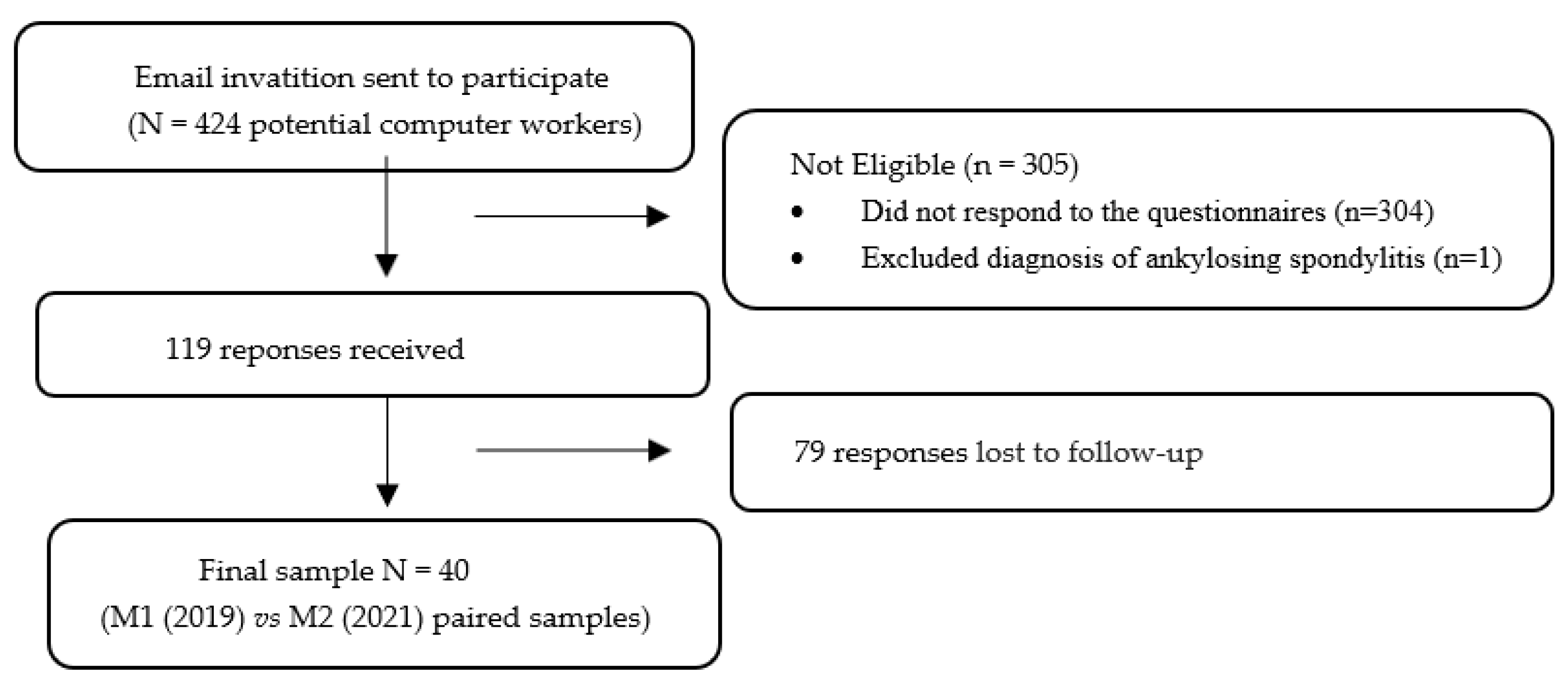
2.3. Sample Recruitment and Elegibility Criteria
2.4. Questionnaire for Collecting Data
2.5. Instruments
2.5.1. Sociodemographic Questionnaire
2.5.2. Nordic Musculoskeletal Questionnaire (NMQ-vPt)
2.5.3. International Physical Activity Questionnaire (IPAQ)–Short Version
- Walking METs = 3.3 × minutes’ walk × number of days walking
- Moderate METs = 4.0 × minutes of moderate activity × number of days doing moderate activity
- Vigorous METs = 8.0 × minutes of vigorous activity × number of days doing vigorous activity
- Total METs = METs walking
- METs of moderate activity + METs of vigorous activity.
2.6. Statistics
3. Results
3.1. Sample Profile
3.2. Musculoskeletal Symptomatology
3.3. Physical Activity and Sitting Time
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eurostat, E.C. Health and Safety at Work in Europe (1999–2007); A Statistical Portrait; Publications Office of the European Union: Luxembourg, 2010. [Google Scholar]
- Akodu, A.; Akinfeleye, A. Work-related musculoskeletal disorders of the upper extremity with reference to working posture of secretaries. S. Afr. J. Occup. Ther. 2015, 45, 16–22. [Google Scholar] [CrossRef] [Green Version]
- Eijckelhof, B.H.; Bruno Garza, J.L.; Huysmans, M.A.; Blatter, B.M.; Johnson, P.W.; van Dieen, J.H.; van der Beek, A.J.; Dennerlein, J.T. The effect of overcommitment and reward on muscle activity, posture, and forces in the arm-wrist-hand region—A field study among computer workers. Scand. J. Work Environ. Health 2013, 39, 379–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hugue, T.D.; Júnior, A.A.P. Prevalência de dor Osteomuscular Entre os Funcionários Administrativos da UNIFEBE. Revista da UNIFEBE 2011. Available online: https://periodicos.unifebe.edu.br/index.php/RevistaUnifebe/article/view/54 (accessed on 19 July 2019).
- Waongenngarm, P.; van der Beek, A.J.; Akkarakittichoke, N.; Janwantanakul, P. Perceived musculoskeletal discomfort and its association with postural shifts during 4-h prolonged sitting in office workers. Appl. Ergon. 2020, 89, 103225. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Ijmker, S.; Blatter, B.M.; van der Beek, A.J.; van Mechelen, W.; Bongers, P.M. Prospective research on musculoskeletal disorders in office workers (PROMO): Study protocol. BMC Musculoskelet. Disord. 2006, 7, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baker, R.; Coenen, P.; Howie, E.; Williamson, A.; Straker, L. The Short Term Musculoskeletal and Cognitive Effects of Prolonged Sitting During Office Computer Work. Int. J. Environ. Res. Public Health 2018, 15, 1678. [Google Scholar] [CrossRef] [Green Version]
- Chambers, A.J.; Robertson, M.M.; Baker, N.A. The effect of sit-stand desks on office worker behavioral and health outcomes: A scoping review. Appl. Ergon. 2019, 78, 37–53. [Google Scholar] [CrossRef]
- Arslan, S.S.; Alemdaroğlu, İ.; Karaduman, A.A.; Yilmaz, Ö.T. The effects of physical activity on sleep quality, job satisfaction, and quality of life in office workers. Work 2019, 63, 3–7. [Google Scholar] [CrossRef]
- Hu, F.B.; Li, T.Y.; Colditz, G.A.; Willett, W.C.; Manson, J.E. Television Watching and Other Sedentary Behaviors in Relation to Risk of Obesity and Type 2 Diabetes Mellitus in Women. JAMA 2003, 289, 1785–1791. [Google Scholar] [CrossRef] [Green Version]
- Juul-Kristensen, B.; Søgaard, K.; Støyer, J.; Jensen, C. Computer users’ risk factors for developing shoulder, elbow and back symptoms. Scand. J. Work. Environ. Health 2004, 30, 390–398. [Google Scholar] [CrossRef] [Green Version]
- Gonzalez, L.R.; Lucca, S.R.; Kitamura, S.; Oliveira, J.I.; Lido, A.V.; Manzano, L.F.; Soares, A.L. Contribuições para a investigação de lesões por esforços repetitivos—Distúrbios ósteomusculares relacionados com o trabalho em membros superiores. Rev. Soc. Bras. Clín. Méd 2008, 6, 72–78. [Google Scholar]
- Paksaichol, A.; Janwantanakul, P.; Purepong, N.; Pensri, P.; van der Beek, A.J. Office workers’ risk factors for the development of non-specific neck pain: A systematic review of prospective cohort studies. Occup. Environ. Med. 2012, 69, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.D.; Kwan, C.S.J.; Zhang, S.; Wheeler, J.; Sewell, T.; Johnston, V. The Influence of Using a Footstool during a Prolonged Standing Task on Low Back Pain in Office Workers. Int. J. Environ. Res. Public Health 2019, 16, 1405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, S.; Jing, Q.; Wei, C.; Lu, J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: A cross-sectional study. BMJ Open 2017, 7, e014914. [Google Scholar] [CrossRef] [Green Version]
- Eltayeb, S.; Staal, J.B.; Kennes, J.; Lamberts, P.H.; de Bie, R.A. Prevalence of complaints of arm, neck and shoulder among computer office workers and psychometric evaluation of a risk factor questionnaire. BMC Musculoskelet. Disord. 2007, 8, 68. [Google Scholar] [CrossRef] [Green Version]
- Kaliniene, G.; Ustinaviciene, R.; Skemiene, L.; Januskevicius, V. Associations between neck musculoskeletal complaints and work related factors among public service computer workers in Kaunas. Int. J. Occup. Med. Environ. Health 2013, 26, 670–681. [Google Scholar] [CrossRef]
- Valipour Noroozi, M.; Hajibabaei, M.; Saki, A.; Memari, Z. Prevalence of Musculoskeletal Disorders Among Office Workers. Jundishapur J. Health Sci. 2015, 7, e27157. [Google Scholar] [CrossRef] [Green Version]
- Holzgreve, F.; Maltry, L.; Lampe, J.; Schmidt, H.; Bader, A.; Rey, J.; Groneberg, D.A.; van Mark, A.; Ohlendorf, D. The office work and stretch training (OST) study: An individualized and standardized approach for reducing musculoskeletal disorders in office workers. J. Occup. Med. Toxicol. 2018, 13, 37. [Google Scholar] [CrossRef] [Green Version]
- Gerr, F.; Marcus, M.; Ensor, C.; Kleinbaum, D.; Cohen, S.; Edwards, A.; Gentry, E.; Ortiz, D.J.; Monteilh, C. A prospective study of computer users: I. Study design and incidence of musculoskeletal symptoms and disorders. Am. J. Ind. Med. 2002, 41, 221–235. [Google Scholar] [CrossRef]
- Gobbo, S.; Bullo, V.; Bergamo, M.; Duregon, F.; Vendramin, B.; Battista, F.; Roma, E.; Bocalini, D.S.; Rica, R.L.; Alberton, C.L.; et al. Physical Exercise Is Confirmed to Reduce Low Back Pain Symptoms in Office Workers: A Systematic Review of the Evidence to Improve Best Practices in the Workplace. J. Funct. Morphol. Kinesiol. 2019, 4, 43. [Google Scholar] [CrossRef] [Green Version]
- Shariat, A.; Alizadeh, R.; Moradi, V.; Afsharnia, E.; Hakakzadeh, A.; Ansari, N.N.; Ingle, L.; Shaw, B.S.; Shaw, I. The impact of modified exercise and relaxation therapy on chronic lower back pain in office workers: A randomized clinical trial. J. Exerc. Rehabil. 2019, 15, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.O.; Pereira, B.F.; Pereira Gomes, M.V.; Marcondes, L.P.; de Campos Gomes, F.; de Melo-Neto, J.S. Preventive factors against work-related musculoskeletal disorders: Narrative review. Rev. Bras. Med. Trab. 2019, 17, 415–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vitta, A.; Canonici, A.; de Conti, M.H.S.; Simeão, S.F.D.A.P. Prevalência e fatores associados à dor musculoesquelética em profissionais de atividades sedentárias. Fisioter. Em Mov. 2012, 25, 273–280. [Google Scholar] [CrossRef]
- Lipscomb, J.A.; Trinkoff, A.M.; Geiger-Brown, J.; Brady, B. Work-schedule characteristics and reported musculoskeletal disorders of registered nurses. Scand. J. Work. Environ. Health 2002, 28, 394–401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Agency for Safety & Health at Work; Kok, J.; Vroonhof, P.; Snijders, J.; Roullis, G.; Clarke, M.; Peereboom, K.; Dorst, P.; Isusi, I. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics; EU. Publications Office: Luxembourg, Luxembourg, 2020. [Google Scholar]
- Rodriguez-Nogueira, O.; Leiros-Rodriguez, R.; Benitez-Andrades, J.A.; Alvarez-Alvarez, M.J.; Marques-Sanchez, P.; Pinto-Carral, A. Musculoskeletal Pain and Teleworking in Times of the COVID-19: Analysis of the Impact on the Workers at Two Spanish Universities. Int. J. Environ. Res. Public Health 2020, 18, 31. [Google Scholar] [CrossRef] [PubMed]
- Direção-Geral da Saúde, COVID-19. 2021. Available online: https://www.sns24.gov.pt/tema/doencas-infecciosas/covid-19/#sec-0 (accessed on 9 March 2021).
- Raquel Gonçalves Caldeira Brant, L.; Helena Cardoso, M. DESAFIOS DO TELETRABALHO NA PANDEMIA COVID-19: QUANDO O HOME VIRA OFFICE. Cad. De Adm. 2020, 28, 71–75. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Lesser, I.A.; Nienhuis, C.P. The Impact of COVID-19 on Physical Activity Behavior and Well-Being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef]
- Shariat, A.; Ghannadi, S.; Anastasio, A.T.; Rostad, M.; Cleland, J.A. Novel stretching and strength-building exercise recommendations for computer-based workers during the COVID-19 quarantine. Work 2020, 66, 739–749. [Google Scholar] [CrossRef]
- Figueiredo, E.; Ribeiro, C.; Pereira, P.; Passos, C. Teletrabalho: Contributos e desafios para as organizações. Rev. Psicol. Organ. E Trab. 2021, 2, 1427–1438. [Google Scholar] [CrossRef]
- Oakman, J.; Kinsman, N.; Stuckey, R.; Graham, M.; Weale, V. A rapid review of mental and physical health effects of working at home: How do we optimise health? BMC Public Health 2020, 20, 1825. [Google Scholar] [CrossRef] [PubMed]
- Venegas Tresierra, C.E.; Leyva Pozo, A.C. La fatiga y la carga mental en los teletrabajadores: A propósito del distanciamiento social. Rev. Esp. De Salud Publica 2020, 94, 126. [Google Scholar]
- Abdin, S.; Welch, R.K.; Byron-Daniel, J.; Meyrick, J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: A systematic review. Public Health 2018, 160, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Louw, S.; Makwela, S.; Manas, L.; Meyer, L.; Terblanche, D.; Brink, Y. Effectiveness of exercise in office workers with neck pain: A systematic review and meta-analysis. S. Afr. J. Physiother. 2017, 73, 392. [Google Scholar] [CrossRef] [PubMed]
- Suni, J.H.; Rinne, M.; Tokola, K.; Mänttäri, A.; Vasankari, T. Effectiveness of a standardised exercise programme for recurrent neck and low back pain: A multicentre, randomised, two-arm, parallel group trial across 34 fitness clubs in Finland. BMJ Open Sport Exerc. Med. 2017, 3, e000233. [Google Scholar] [CrossRef] [Green Version]
- Roviello, V.; Gilhen-Baker, M.; Vicidomini, C.; Roviello, G.N. Forest-bathing and physical activity as weapons against COVID-19: A review. Environ. Chem. Lett. 2021, 20, 131–140. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Nguyen, T.M.; Nguyen, V.H.; Kim, J.H. Physical Exercise and Health-Related Quality of Life in Office Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 3791. [Google Scholar] [CrossRef]
- Debska, M.; Polechonski, J.; Mynarski, A.; Polechonski, P. Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health. Int. J. Environ. Res. Public Health 2019, 16, 3673. [Google Scholar] [CrossRef] [Green Version]
- Ryde, G.C.; Atkinson, P.; Stead, M.; Gorely, T.; Evans, J.M. Physical activity in paid work time for deskbased employees: A qualitative study of employers’ and employees’ perspectives. BMC Public Health 2020, 20, 460. [Google Scholar] [CrossRef]
- Arruda, Z.M.T.D. Atuação do Fisioterapeuta na Saúde e Qualidade de Vida de Trabalhadores Utilizadores de Terminais de Computador; Faculdade de Medicina da Universidade de Coimbra: Coimbra, Portugal, 2019. [Google Scholar]
- Mesquita, C.C.; Ribeiro, J.C.; Moreira, P. Portuguese version of the standardized Nordic musculoskeletal questionnaire: Cross cultural and reliability. J. Public Health 2010, 18, 461–466. [Google Scholar] [CrossRef]
- Mota, J.; Sardinha, L. Questionário Internacional de Actividade Física. Estudo piloto da garantia e validade numa população portuguesa. In Livro de Resumos do 8° Congresso de Educação Física e Ciências do Desporto dos Países de Língua Portuguesa. Desporto, Educação e Saúde; 8° Congresso de Educação Física e Ciências do Desporto dos Países de Língua Portuguesa; Faculdade de Motricidade Humana—Universidade Técnica de Lisboa: Lisboa, Portugal, 2000; p. 323. [Google Scholar]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sorensen, F.; Andersson, G.; Jorgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- Campaniço, H. Validade Simultânea do Questionário Internacional de Actividade. Física Através da Medição Objectiva da Actividade Física por Actigrafia ProporcionalMaster’s ThesisUniversidade de Lisboa (Portugal), ProQuest Dissertations Publishing: Lisboa, Portugal, 2016.
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- IPAQ. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire; IPAQ: Tokyo, Japan, 2005; Available online: https://sites.google.com/site/theipaq/ (accessed on 23 September 2021).
- Cheng, H. A Simple, Easy-to-Use Spreadsheet for Automatic Scoring of the Three Factor Eating Questionnaire (TFEQ)—Note to Users. 2016. Available online: https://www.researchgate.net/profile/Hoi_Lun_helen_Cheng/publication/311067926_A_simple_easy-to-use_spreadsheet_for_automatic_scoring_of_the_Three_Factor_Eating_Questionnaire_TFEQ/data/583d10e608ae1ff459833d94/TFEQ-Scoring.xlsx (accessed on 23 September 2021).
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows; Version 27.0; IBM Corp: Armonk, NY, USA, 2020; Available online: https://www.ibm.com/support/pages/how-cite-ibm-spss-statistics-or-earlier-versions-spss (accessed on 23 March 2022).
- Bu, F.; Bone, J.K.; Mitchell, J.J.; Steptoe, A.; Fancourt, D. Longitudinal changes in physical activity during and after the first national lockdown due to the COVID-19 pandemic in England. Sci. Rep. 2021, 11, 17723. [Google Scholar] [CrossRef] [PubMed]
- Roggio, F.; Trovato, B.; Ravalli, S.; Di Rosa, M.; Maugeri, G.; Bianco, A.; Palma, A.; Musumeci, G. One Year of COVID-19 Pandemic in Italy: Effect of Sedentary Behavior on Physical Activity Levels and Musculoskeletal Pain among University Students. Int. J. Environ. Res. Public Health 2021, 18, 8680. [Google Scholar] [CrossRef]
- Bhoyroo, R.; Chivers, P.; Millar, L.; Bulsara, C.; Piggott, B.; Lambert, M.; Codde, J. Life in a time of COVID: A mixed method study of the changes in lifestyle, mental and psychosocial health during and after lockdown in Western Australians. BMC Public Health 2021, 21, 1947. [Google Scholar] [CrossRef]
- Jain, R.; Meena, M.L.; Rana, K.B. Risk factors of musculoskeletal symptoms among mobile device users during work from home. Int. J. Occup. Saf. Ergon. 2021, 1–7. [Google Scholar] [CrossRef]
- Woo, E.H.C.; White, P.; Lai, C.W.K. Musculoskeletal impact of the use of various types of electronic devices on university students in Hong Kong: An evaluation by means of self-reported questionnaire. Man. Ther. 2016, 26, 47–53. [Google Scholar] [CrossRef]
- Intolo, P.; Shalokhon, B.; Wongwech, G.; Wisiasut, P.; Nanthavanij, S.; Baxter, D.G. Analysis of neck and shoulder postures, and muscle activities relative to perceived pain during laptop computer use at a low-height table, sofa and bed. Work 2019, 63, 361–367. [Google Scholar] [CrossRef]
- Berolo, S.; Wells, R.P.; Amick, B.C. Musculoskeletal symptoms among mobile hand-held device users and their relationship to device use: A preliminary study in a Canadian university population. Appl. Ergon. 2011, 42, 371–378. [Google Scholar] [CrossRef]
- Legan, M.; Zupan, K. Prevalence of mobile device-related musculoskeletal pain among working university students: A cross-sectional study. Int. J. Occup. Saf. Ergon. 2022, 28, 734–742. [Google Scholar] [CrossRef] [PubMed]
- Scarabottolo, C.C.; Pinto, R.Z.; Oliveira, C.B.; Zanuto, E.F.; Cardoso, J.R.; Christofaro, D.G.D. Back and neck pain prevalence and their association with physical inactivity domains in adolescents. Eur. Spine J. 2017, 26, 2274–2280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madeleine, P.; Vangsgaard, S.; Hviid Andersen, J.; Ge, H.Y.; Arendt-Nielsen, L. Computer work and self-reported variables on anthropometrics, computer usage, work ability, productivity, pain, and physical activity. BMC Musculoskelet. Disord. 2013, 14, 226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jain, R.; Verma, V.; Rana, K.B.; Meena, M.L. Effect of physical activity intervention on the musculoskeletal health of university student computer users during homestay. Int. J. Occup. Saf. Ergon. 2021, 1–6. [Google Scholar] [CrossRef]
- Argus, M.; Pääsuke, M. Effects of the COVID-19 lockdown on musculoskeletal pain, physical activity, and work environment in Estonian office workers transitioning to working from home. Work 2021, 69, 741–749. [Google Scholar] [CrossRef]
- Moreira-Silva, I.; Teixeira, P.M.; Santos, R.; Abreu, S.; Moreira, C.; Mota, J. The Effects of Workplace Physical Activity Programs on Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Workplace Health Saf. 2016, 64, 210–222. [Google Scholar] [CrossRef] [Green Version]
- Moreira, S.; Criado, M.B.; Ferreira, M.S.; Machado, J.; Gonçalves, C.; Clemente, F.M.; Mesquita, C.; Lopes, S.; Santos, P.C. Positive Effects of an Online Workplace Exercise Intervention during the COVID-19 Pandemic on Quality of Life Perception in Computer Workers: A Quasi-Experimental Study Design. Int. J. Environ. Res. Public Health 2022, 19, 3142. [Google Scholar] [CrossRef]
- Moreira, S.; Ferreira, M.S.; Criado, M.B.; Machado, J.; Mesquita, C.; Lopes, S.; Santos, P.C. Occupational Health: Does Compliance with Physical Activity Recommendations Have a Preventive Effect on Musculoskeletal Symptoms in Computer Workers? A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 7604. [Google Scholar] [CrossRef]
- Serra, M.; Camargo, P.R.; Zaia, J.E.; Tonello, M.G.M.; Quemelo, P.R.V. Effects of physical exercise on musculoskeletal disorders, stress and quality of life in workers. Int. J. Occup. Saf. Ergon. 2018, 24, 62–67. [Google Scholar] [CrossRef]
- Seghetto, A.; Piccoli, J.C.J. Nível de atividade física, prevalência de desconforto e dor muscular e capacidade de trabalho: Uma avaliação no setor de call center de um banco do Rio Grande do Sul, Brasil. Rev. Bras. De Ciência E Mov. 2012, 20, 105–117. [Google Scholar]
- Stamatakis, E.; Gale, J.; Bauman, A.; Ekelund, U.; Hamer, M.; Ding, D. Sitting Time, Physical Activity, and Risk of Mortality in Adults. J. Am. Coll. Cardiol. 2019, 73, 2062–2072. [Google Scholar] [CrossRef] [PubMed]
- McDowell, C.P.; Herring, M.P.; Lansing, J.; Brower, C.; Meyer, J.D. Working From Home and Job Loss Due to the COVID-19 Pandemic Are Associated With Greater Time in Sedentary Behaviors. Frontiers in Public Health 2020, 8, 750. [Google Scholar] [CrossRef] [PubMed]
- Braccialli, L.M.P.; Vilarta, R. Aspectos a serem considerados na elaboração de programas de prevenção e orientação de problemas posturais. Rev. Paul. Educ. Fís. 2000, 14, 159–171. [Google Scholar]
- Buckle, P.W.; Jason Devereux, J. The nature of work-related neck and upper limb musculoskeletal disorders. Appl. Ergon. 2002, 33, 207–217. [Google Scholar] [CrossRef]
- Augusto, V.G.; Sampaio, R.F.; Tirado, M.G.A.; Mancini, M.C.; Parreira, V.F. A look into Repetitive Strain Injury/Work-Related Musculoskeletal Disorders within physical therapists’ clinical context. Braz. J. Phys. Ther. 2008, 12, 49–56. [Google Scholar]
- Callaghan, P. Exercise: A neglected intervention in mental health care? J. Psychiatr. Ment. Health Nurs. 2004, 11, 476–483. [Google Scholar] [CrossRef] [PubMed]
| n | % | |
|---|---|---|
| Gender | ||
| Female | 14 | 35.0 |
| Male | 26 | 65.0 |
| Marital Status | ||
| Single | 15 | 37.5 |
| Married/Cohabitation | 22 | 55.0 |
| Separated/Divorced | 3 | 7.5 |
| Educational Attainment | ||
| Middle school | 1 | 2.5 |
| Secondary school | 14 | 35.0 |
| Bachelor’s degree | 18 | 45.0 |
| Master’s degree | 7 | 17.5 |
| BMI Category | ||
| Low weight | 1 | 2.5 |
| Normal weight | 19 | 47.5 |
| Pre-obesity | 12 | 30.0 |
| Obesity | 8 | 20.0 |
| Mean | Standard Deviation | |
| Age (years) | 35.75 | 7.32 |
| Height (m) | 1.72 | 0.10 |
| Body mass (kg) | 76.58 | 16.86 |
| BMI (kg/m2) | 25.72 | 4.97 |
| Musculoskeletal Symptoms | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anatomical Regions | Symptomatology Last 12 Months | ADL Limitation Last 12 Months | Symptomatology Last 7 Days | Pain Intensity | |||||||||
| M1 | M2 | M1 | M2 | M1 | M2 | M1 | M2 | ||||||
| n (%) | n (%) | p(1) | n (%) | n (%) | p(1) | n (%) | n (%) | p(1) | M(SD) | M(SD) | p(2) | d | |
| Neck | 18 (45.0) | 25 (62.5) | 0.046 | 7 (17.5) | 6 (15.0) | 0.500 | 9 (22.5) | 15 (37.5) | 0.073 | 1.83 (2.26) | 2.23 (2.42) | 0.156 | 0.17 |
| Shoulders | 15 (37.5) | 22 (55.0) | 0.033 | 2 (5.0) | 6 (15.0) | 0.109 | 4 (10.0) | 10 (25.0) | 0.055 | 1.43 (2.24) | 2.35 (2.55) | 0.003 | 0.38 |
| Elbows | 3 (7.5) | 8 (20.0) | 0.063 | 0 (0.0) | 1 (2.5) | 0.500 | 0 (0.0) | 3 (7.5) | 0.125 | 0.18 (0.59) | 0.60 (1.34) | 0.015 | 0.41 |
| Wrists and hands | 10 (25.0) | 18 (45.0) | 0.019 | 1 (2.5) | 5 (12.5) | 0.063 | 2 (5.0) | 2 (5.0) | 0.750 | 0.65 (1.19) | 0.93 (1.56) | 0.183 | 0.20 |
| Thoracic | 5 (12.5) | 4 (10.0) | 0.500 | 1 (2.5) | 3 (7.5) | 0.250 | 1 (2.5) | 0 (0.0) | 0.500 | 0.38 (1.21) | 0.20 (0.56) | 0.273 | 0.19 |
| Low back | 22 (55.0) | 24 (60.0) | 0.395 | 6 (15.0) | 7 (17.5) | 0.500 | 10 (25.0) | 13 (32.5) | 0.291 | 2.10 (2.72) | 2.38 (2.48) | 0.330 | 0.11 |
| Hips and thighs | 11 (27.5) | 8 (20.0) | 0.291 | 1 (2.5) | 1 (2.5) | 0.750 | 2 (5.0) | 2 (5.0) | 0.750 | 0.68 (1.49) | 0.48 (1.04) | 0.363 | 0.16 |
| Knees | 14 (35.0) | 16 (40.0) | 0.387 | 3 (7.5) | 2 (5.0) | 0.500 | 5 (12.5) | 5 (12.5) | 0.656 | 1.13 (2.03) | 1.00 (1.52) | 0.367 | 0.07 |
| Ankles and feet | 12 (30.0) | 9 (22.5) | 0.304 | 1 (2.5) | 2 (5.0) | 0.500 | 2 (5.0) | 4 (10.0) | 0.313 | 0.70 (1.56) | 0.50 (1.40) | 0.280 | 0.13 |
| M1 | M2 | p | d | |
|---|---|---|---|---|
| Physical Activity (METs) | M (SD) | M (SD) | ||
| Vigorous (minutes/week) | 791.00 (1252.18) | 1044.00 (1739.67) | 0.291 (1) | 0.17 |
| Moderate (minutes/week) | 340.00 (576.30) | 279.50 (519.69) | 0.241 (1) | 0.11 |
| Walking (minutes/week) | 526.76 (594.86) | 727.24 (925.81) | 0.281 (1) | 0.26 |
| Total (minutes/week) | 1657.80 (1825.07) | 2050.78 (2675.69) | 0.475 (1) | 0.17 |
| Physical Activity Level | n (%) | n (%) | ||
| Low | 16 (40.0%) | 16 (40.0%) | 0.372 (1) | |
| Medium | 15 (37.5%) | 13 (32.5%) | ||
| High | 9 (22.5%) | 11 (27.5%) | ||
| Meets WHO recommendations | n (%) | n (%) | ||
| No | 21 (52.5%) | 22 (55.0%) | 0.500 (2) | |
| Yes | 19 (47.5%) | 18 (45.0%) | ||
| Sitting time | M (SD) | M (SD) | ||
| Weekday (hours/day) | 4.85 (3.05) | 6.75 (3.41) | < 0.001 (1) | 0.59 |
| Weekend day (hours/day) | 4.48 (2.59) | 5.03 (2.61) | 0.064 (1) | 0.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreira, S.; Criado, M.B.; Ferreira, M.S.; Machado, J.; Gonçalves, C.; Mesquita, C.; Lopes, S.; Santos, P.C. The Effects of COVID-19 Lockdown on the Perception of Physical Activity and on the Perception of Musculoskeletal Symptoms in Computer Workers: Comparative Longitudinal Study Design. Int. J. Environ. Res. Public Health 2022, 19, 7311. https://doi.org/10.3390/ijerph19127311
Moreira S, Criado MB, Ferreira MS, Machado J, Gonçalves C, Mesquita C, Lopes S, Santos PC. The Effects of COVID-19 Lockdown on the Perception of Physical Activity and on the Perception of Musculoskeletal Symptoms in Computer Workers: Comparative Longitudinal Study Design. International Journal of Environmental Research and Public Health. 2022; 19(12):7311. https://doi.org/10.3390/ijerph19127311
Chicago/Turabian StyleMoreira, Sara, Maria Begoña Criado, Maria Salomé Ferreira, Jorge Machado, Carla Gonçalves, Cristina Mesquita, Sofia Lopes, and Paula Clara Santos. 2022. "The Effects of COVID-19 Lockdown on the Perception of Physical Activity and on the Perception of Musculoskeletal Symptoms in Computer Workers: Comparative Longitudinal Study Design" International Journal of Environmental Research and Public Health 19, no. 12: 7311. https://doi.org/10.3390/ijerph19127311









