Information Communication Technology and Infant Mortality in Low-Income Countries: Empirical Study Using Panel Data Models
Abstract
:1. Introduction
2. The Literature on the Effects of ICT on Health Outcomes
3. Materials and Methods
3.1. Data Source, Data Processing, and Data Imputing
3.1.1. Data Source
3.1.2. Data Processing
3.1.3. Predictive Mean Matching (PMM)
3.2. Empirical Tests
3.3. Model Construction
- Ensure stationarity through the tests of 1st-generation panel unit-root;
- Test for pool-ability to utilize the POLS and, later, the PCCE;
- First step: Apply the POLS analysis and fixed effects to get their estimates results;
- Compare through F-test of individual effects to decide which estimates better depict our data and model;
- Second step: Apply random-effects analysis to obtain its estimates results;
- Compare RE with FE to decide which estimates depict better our model;
- Test for cross-sectional dependence through the results of the estimate of RE and FE;
- Apply appropriate techniques to remedy the presence of cross-sectional dependence;
- Add additional analyses to compare the final model estimates (robustness);
- To avoid redundancy and length, we only report the adequate results.
4. Results
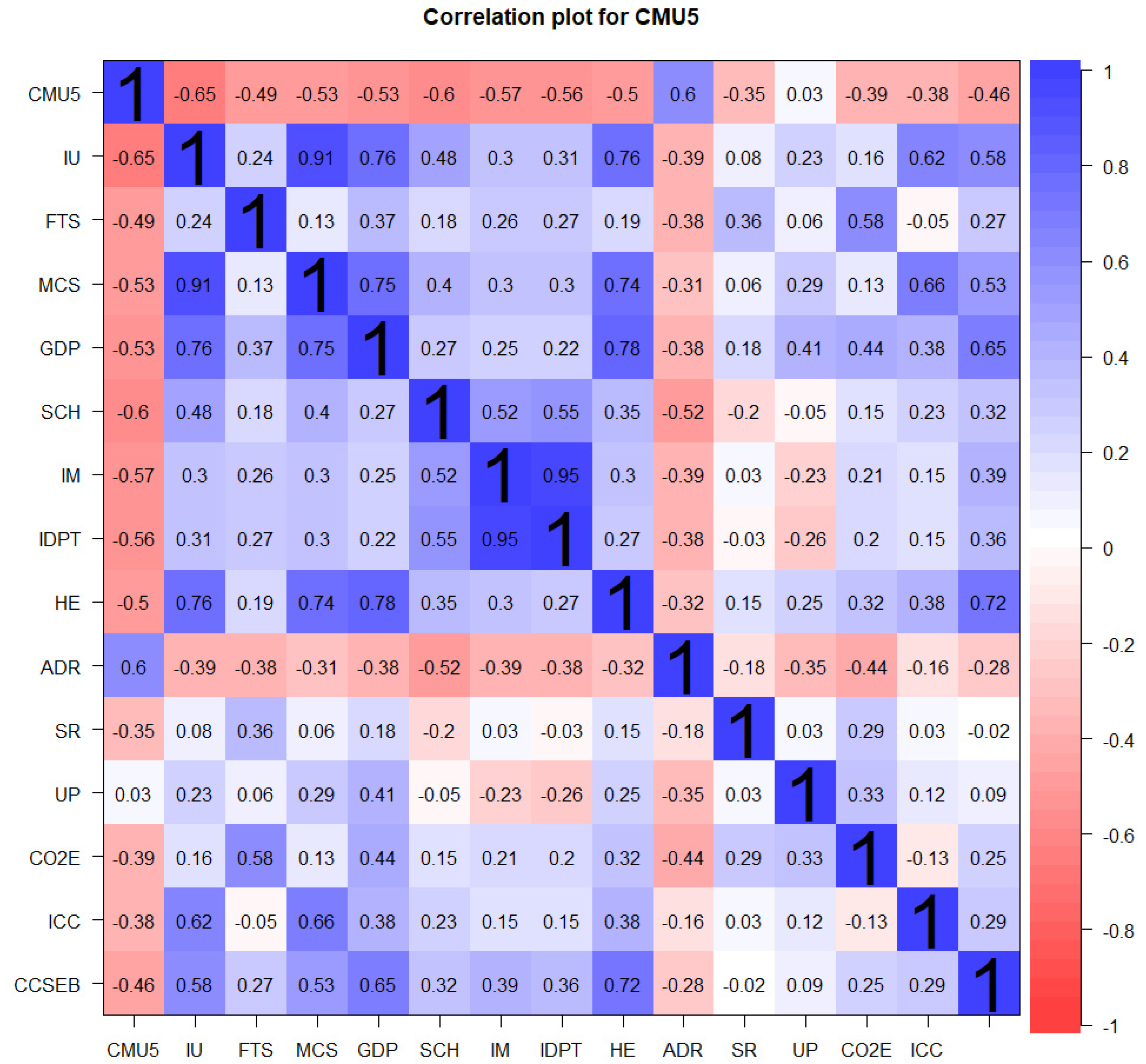
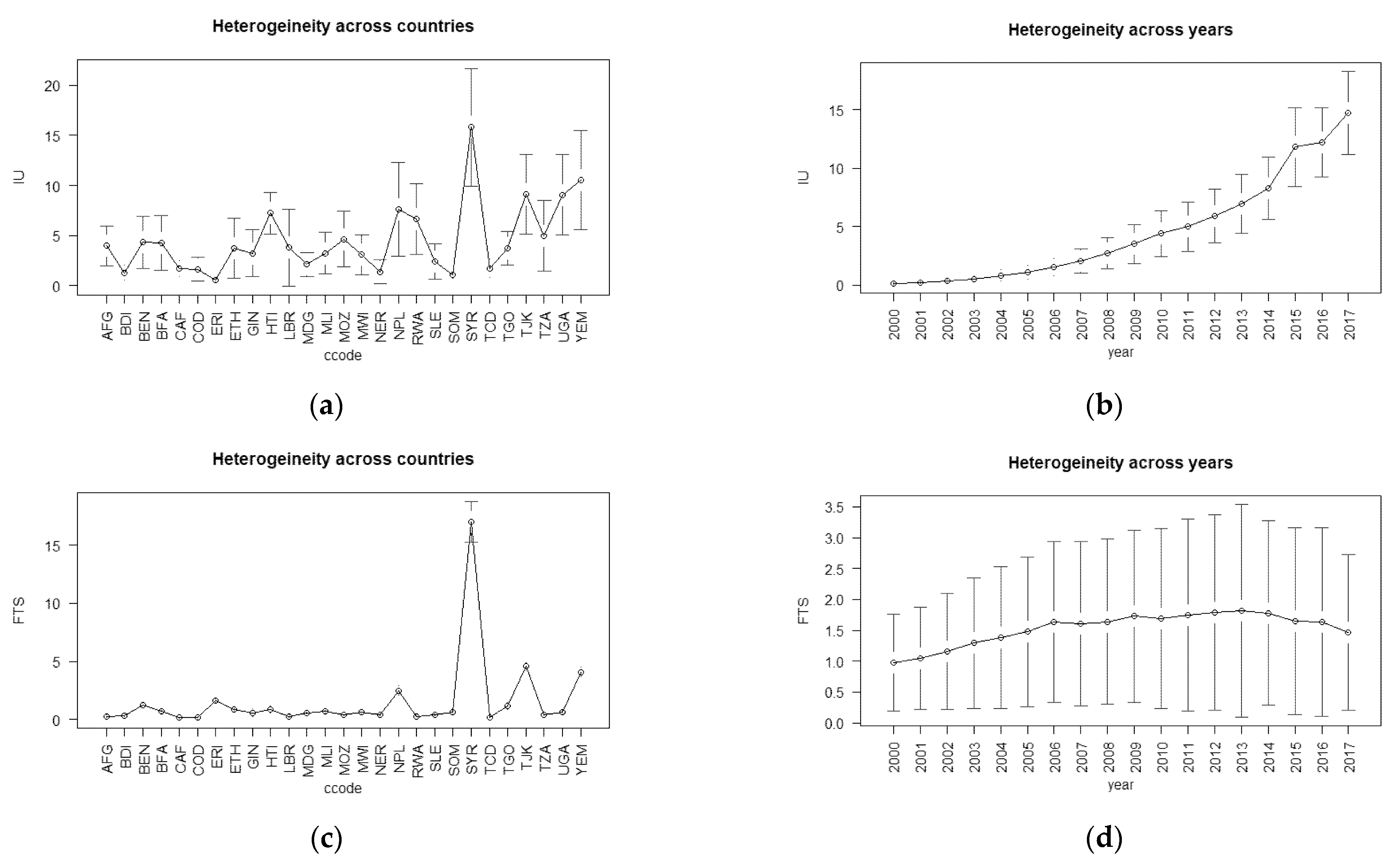
4.1. Descriptive Statistics
4.2. Fixed Effects FE Results
4.3. Two-Way FE Using Driscoll–Kraay Robust Errors with IV Estimation Results
4.4. Panel Common Correlated Effects PCCE Estimation Results
4.5. System-GMM Results
5. Discussion
5.1. INFM
5.2. CMU5
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variable | Description | Source | Related Works | Status |
|---|---|---|---|---|
| Health outcome dependent variables | ||||
| INFM | Mortality rate, infant (per 1000 live births) | World Bank Database | [2,3,52] | Included |
| CMU5 | Mortality rate, under 5 (per 1000 live births) | World Bank Database | [52] | Included |
| LEB | life expectancy at birth, total (years) | World Bank Database | [3,52] | Excluded |
| HIV | Prevalence of HIV. The percentage of people ages 15–49 who are infected with HIV | World Bank Database | [52] | Excluded |
| TBS | Incidences of tuberculosis, per 10,000 people. | World Bank Database | [52] | Excluded |
| ICT independent variables | ||||
| IU | Individuals using the Internet (% of the population) | International Telecommunications Union (ITU) | [2,3,52] | Included |
| FTS | Fixed telephone subscriptions (per 100 people) | ITU | [2,3,52] | Included |
| MCS | Mobile cellular subscriptions (per 100 people) | ITU | [2,3,52] | Included |
| FBS | fixed-broadband subscriptions per 100 inhabitants | ITU | [2] | Excluded |
| SIS | Secure servers are servers used per 1 million populations | ITU | [2] | Excluded |
| Economic Factors | ||||
| GDP | GDP per capita, PPP (constant 2017 inter ratio in USD) | World Bank Database | [3,52] | Included |
| PHY | physicians (per 1000people) | World Bank Database | [3] | Excluded |
| ADR | Age dependency ratio (% of working-age population) | World Bank Database | [52] | Excluded |
| IM | Immunization, measles (% of children ages 12–23 months) | World Bank Database | [3,52] | Included |
| IDPT | Immunization, DPT (% of children ages 12–23 months) | World Bank Database | [52] | Included |
| HE | Domestic general government health expenditure per capita, PPP (current inter ratio in USD) | World Bank Database | [2,52] | Included |
| Social Factors | ||||
| SR | Sex ratio at birth (male births per female births) | World Bank Database | [3,52] | Excluded |
| SCH | School enrollment, secondary (% gross) | World Bank Database | [3] | Included |
| SCHF | Female pupils as a percentage of total pupils at primary level includeenrollments in public and private schools | World Bank Database | [2,52] | Included |
| NETP | The net primary school enrolment rate (%). | World Bank Database | [52] | Excluded |
| Environmental Factors | ||||
| UP | Urban population (% of the total population) | World Bank Database | [2] | Included |
| SNT | People using at least basic drinking water services; taken as the percentage of total population | World Bank Database | [2,52] | Excluded |
| WATR | The percentage of the population with access to an improved water source. | World Bank Database | [52] | Excluded |
| CO2E | CO2 emissions (metric tons per capita) | World Bank Database | [3] | Included |
| Instrumental Variables | ||||
| CCSEB | Communications, computer, etc. (% of service exports, BoP) | World Bank Database | Included | |
| ICTSEBCUS | ICT service exports (BoP, current USD) | World Bank Database | Excluded | |
| ICTSESEB | ICT service exports (% of service exports, BoP) | World Bank Database | Excluded | |
| ICTGETGI | ICT goods imports (% total goods imports) | World Bank Database | Excluded | |
| ICTGETGE | ICT goods exports (% of total goods exports) | World Bank Database | Excluded | |
| CCSIB | Communications, computer, etc. (% of service imports, BoP) | World Bank Database | Excluded | |
| CCOSCSI | Computer, communications, and other services (% of commercial service imports) | World Bank Database | Excluded | |
| CCOSCSE | Computer, communications, and other services (% of commercial service exports) | World Bank Database | Excluded | |
| ICC | Dummy variable of the first year a country issued an internet country code | Author’ own calculation | Included | |
Appendix A.1. Empirical Tests
| Symbol | Second-Generation Panel Unit-Root Test | First-Generation Panel Unit-Root Test | ||||
|---|---|---|---|---|---|---|
| CIPS d | CAFD d | CIPS t | CAFD t | LLC | IPS | |
| INFM | −2.5506 * | −5.46 * | −2.159 * | −2.195 * | −27.47 * | −54.70 * |
| CMU5 | −2.55 * | −4.899 * | −2.747 * | −2.388 * | −34.31 * | −74.71 * |
| IU | −2.478 * | 0.225 | −3.475 * | −2.649 * | −6.103 * | −0.749 |
| FTS | −1.6 * | 0.48 | −1.886 * | 2.172 * | −5.01 * | −0.627 |
| MCS | −3.732 * | −8.144 * | −4.002 * | 3.614 * | −23.233 * | −17.663 * |
| GDP | −2.487 * | −1.587 * | −2.731 * | 2.29 * | −4.717 * | −1.097 |
| SCH | −2.592 * | −3.943 * | −2.744 * | −2.98 * | −6.797 * | −4.754 * |
| IM | −2.571 * | −3.902 * | −2.608 * | −1.873 * | −6.758 * | −5.357 * |
| IDPT | −2.268 * | −5.042 * | −2.702 * | −3.116 * | −13.213 * | −9.030 * |
| HE | −2.138 * | −3.262 * | −2.406 * | 2.278 * | −5.633 * | −2.265 * |
| ADR | −0.497 | 4.937 | −0.677 | 5.694 * | 3.023 | 15.379 |
| SR | −2.895 * | −8.99 * | −3.213 * | −8.27 * | −3.9749 * | −10.594 * |
| UP | −1.017 | 5.255 | −2.343 * | −1.728 * | −24.437 * | −5.148 * |
| CO2E | −1.911 * | −1.293 | −2.05 * | 1.455 | 0.777 | −1.748 * |
Appendix B
Appendix B.1. Results

| CMU5 | INFM | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| lnIU | −0.185 *** | −0.142 *** | ||||
| 0.019 | 0.015 | |||||
| lnFTS | 0.003 | 0.001 | ||||
| 0.013 | 0.010 | |||||
| lnMCS | −0.059 *** | −0.052 *** | ||||
| 0.011 | 0.009 | |||||
| lnGDP | 0.064 ** | −0.286 *** | −0.124 *** | 0.042 ** | −0.226 *** | −0.084 *** |
| 0.029 | 0.059 | 0.036 | 0.020 | 0.050 | 0.031 | |
| lnSCH | 0.005 | −0.139 ** | −0.069 | 0.040 | −0.071 ** | −0.008 |
| 0.081 | 0.065 | 0.070 | 0.047 | 0.031 | 0.037 | |
| lnIM | 0.051 | 0.197 *** | 0.191 *** | 0.044 | 0.157 *** | 0.151 *** |
| 0.092 | 0.041 | 0.040 | 0.081 | 0.031 | 0.028 | |
| lnIDPT | −0.053 | −0.237 *** | −0.197 *** | −0.039 | −0.180 *** | −0.144 *** |
| 0.062 | 0.064 | 0.058 | 0.050 | 0.047 | 0.039 | |
| lnHE | 0.031 | −0.142 *** | −0.089 ** | −0.005 | −0.138 *** | −0.091 ** |
| 0.064 | 0.044 | 0.044 | 0.050 | 0.036 | 0.037 | |
| lnADR | −0.330 | 0.075 | 0.034 | −0.076 | 0.235 * | 0.198 * |
| 0.111 | 0.154 | 0.139 | 0.087 | 0.125 | 0.111 | |
| lnSR | −19.152 *** | −25.727 *** | −26.321 *** | −15.777 *** | −20.850 *** | −21.333 *** |
| 4.916 | 6.082 | 5.044 | 3.742 | 4.589 | 3.659 | |
| lnUP | 0.034 | −0.148 ** | −0.100 ** | 0.040 | −0.100 * | −0.057 |
| 0.065 | 0.068 | 0.050 | 0.047 | 0.058 | 0.040 | |
| lnCO2E | −0.003 | 0.064 *** | 0.050 *** | −0.004 | 0.048 *** | 0.035 *** |
| 0.027 | 0.010 | 0.013 | 0.020 | 0.007 | 0.009 | |
| Total Sum of Squares: | 30.251 | 30.251 | 30.251 | 20.507 | 20.507 | 20.507 |
| Residual Sum of Squares: | 8.796 | 6.619 | 5.526 | 4.905 | 4.008 | 3.154 |
| R-Squared: | 0.741 | 0.781 | 0.817 | 0.782 | 0.804 | 0.846 |
| Adj. R-Squared: | 0.720 | 0.763 | 0.802 | 0.765 | 0.788 | 0.833 |
| Chi-Squared on 10 DF: | 1277.240 | 1602.840 | 2008.710 | 1585.210 | 1847.810 | 2469.560 |
| CMU5 | INFM | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| lnIU | −0.019 ** | −0.016 *** | ||||
| 0.008 | 0.005 | |||||
| lnFTS | −0.007 | −0.006 | ||||
| 0.010 | 0.007 | |||||
| lnMCS | −0.028 *** | −0.023 *** | ||||
| 0.006 | 0.006 | |||||
| lnGDP | −0.107 *** | −0.115 ** | −0.092 ** | −0.071 ** | −0.078 * | −0.058 * |
| 0.032 | 0.046 | 0.040 | 0.029 | 0.040 | 0.034 | |
| lnSCH | −0.047 | −0.050 | −0.037 | 0.009 | 0.006 | 0.017 |
| 0.071 | 0.071 | 0.071 | 0.038 | 0.037 | 0.037 | |
| lnIM | 0.196 *** | 0.221 *** | 0.193 *** | 0.165 *** | 0.185 *** | 0.162 *** |
| 0.045 | 0.039 | 0.029 | 0.045 | 0.040 | 0.031 | |
| lnIDPT | −0.216 *** | −0.234 *** | −0.213 *** | −0.165 *** | −0.180 *** | −0.162 *** |
| 0.042 | 0.044 | 0.042 | 0.027 | 0.026 | 0.024 | |
| lnHE | −0.073 | −0.083 | −0.075 | −0.078 * | −0.087 ** | −0.08 ** |
| 0.052 | 0.051 | 0.049 | 0.041 | 0.041 | 0.039 | |
| lnADR | −0.040 | −0.009 | −0.013 | 0.141 | 0.166 | 0.163 |
| 0.127 | 0.128 | 0.135 | 0.098 | 0.101 | 0.107 | |
| lnSR | −19.205 *** | −19.364 *** | −20.299 *** | −15.534 *** | −15.671 *** | −16.456 *** |
| 5.023 | 4.864 | 4.570 | 3.776 | 3.683 | 3.462 | |
| lnUP | −0.023 | −0.027 | −0.034 | 0.008 | 0.005 | −0.001 |
| 0.030 | 0.034 | 0.030 | 0.023 | 0.027 | 0.023 | |
| lnCO2E | −0.002 | −0.003 | −0.004 | −0.004 | −0.005 | −0.005 |
| 0.009 | 0.008 | 0.006 | 0.007 | 0.005 | 0.004 | |
| Total Sum of Squares: | 5.733 | 5.733 | 5.733 | 3.438 | 3.438 | 3.438 |
| Residual Sum of Squares: | 4.100 | 4.148 | 4.065 | 2.316 | 2.349 | 2.290 |
| R-Squared: | 0.284 | 0.276 | 0.290 | 0.326 | 0.316 | 0.333 |
| Adj. R-Squared: | 0.197 | 0.187 | 0.203 | 0.243 | 0.232 | 0.252 |
| F-statistic on 10 and 432 DF: | 17.209 | 16.499 | 17.723 | 20.913 | 20.029 | 21.654 |
References
- Global Health-Newsroom-Global Health Security. 25 October 2019. Available online: https://www.cdc.gov/globalhealth/newsroom/topics/ghs/index.html (accessed on 22 March 2022).
- Dutta, U.P.; Gupta, H.; Sengupta, P.P. ICT and health outcome nexus in 30 selected Asian countries: Fresh evidence from panel data analysis. Technol. Soc. 2019, 59, 101184. [Google Scholar] [CrossRef]
- Majeed, M.T.; Khan, F.N. Do information and communication technologies (ICTs) contribute to health outcomes? An empirical analysis. Qual. Quant. 2018, 53, 183–206. [Google Scholar] [CrossRef]
- Cutler, D.; Miller, G. The role of public health improvements in health advances: The twentieth-century United States. Demography 2005, 42, 1–22. [Google Scholar] [CrossRef] [PubMed]
- World Bank. Engendering Development: Through Gender Equality in Rights, Resources, and Voice; World Bank: Washington, DC, USA; New York, NY, USA; Oxford University Press: Oxford, UK, 2001. [Google Scholar]
- Baltagi, B.H.; Feng, Q.; Kao, C. A Lagrange Multiplier test for cross-sectional dependence in a fixed effects panel data model. J. Econ. 2012, 170, 164–177. [Google Scholar] [CrossRef] [Green Version]
- Choudhury, M.A.; Zaman, S.I.; Harahap, S.S. An Evolutionary Topological Theory of Participatory Socioeconomic Development. World Future 2007, 63, 584–598. [Google Scholar] [CrossRef]
- García-Muñiz, A.S.; Vicente, M.R. ICT technologies in Europe: A study of technological diffusion and economic growth under network theory. Telecommun. Policy 2014, 38, 360–370. [Google Scholar] [CrossRef]
- Lee, J.W.; Brahmasrene, T. ICT, CO2 Emissions and Economic Growth: Evidence from a Panel of ASEAN. Glob. Econ. Rev. 2014, 43, 93–109. [Google Scholar] [CrossRef]
- Pradhan, R.P.; Arvin, M.B.; Norman, N.R.; Bele, S.K. Economic growth and the development of telecommunications infrastructure in the G-20 countries: A panel-VAR approach. Telecommun. Policy 2014, 38, 634–649. [Google Scholar] [CrossRef]
- McConnell, R.R.; Shields, T.; Drury, P.; Kumekawa, J.; Louw, J.; Fereday, G.; Nyamai-Kisia, C. Improving health, connecting people: The role of ICTs in the health sector of developing countries A framework paper. 2006. Available online: https://asksource.info/pdf/framework2.pdf (accessed on 22 March 2022).
- Kaplan, W.A. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Glob. Health 2006, 2, 9. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.H.; Levendis, J.; Gutierrez, L. Telecommunications and economic growth: An empirical analysis of sub-Saharan Africa. Appl. Econ. 2012, 44, 461–469. [Google Scholar] [CrossRef] [Green Version]
- Cutler, D.; Deaton, A.; Lleras-Muney, A. The Determinants of Mortality. J. Econ. Perspect. 2006, 20, 97–120. [Google Scholar] [CrossRef] [Green Version]
- Ball, M.J.; Lillis, J. E-health: Transforming the physician/patient relationship. Int. J. Med. Inform. 2001, 61, 1–10. [Google Scholar] [CrossRef]
- Broom, A. Virtually He@lthy: The Impact of Internet Use on Disease Experience and the Doctor-Patient Relationship. Qual. Health Res. 2005, 15, 325–345. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, T. Online patient-helpers and physicians working together: A new partnership for high quality health care. BMJ 2000, 321, 1129–1132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerber, B.S.; Eiser, A.R. The Patient-Physician Relationship in the Internet Age: Future Prospects and the Research Agenda. J. Med. Internet Res. 2001, 3, e15. [Google Scholar] [CrossRef]
- Haddon, L. Information and Communication Technologies in Everyday Life; Berg Publishers: Oxford, UK, 2004. [Google Scholar]
- Wilson, E.V. Modeling Patients’ Acceptance of Provider-delivered E-health. J. Am. Med. Inform. Assoc. 2004, 11, 241–248. [Google Scholar] [CrossRef] [Green Version]
- The Mobile Connection: The Cell Phone’s Impact on Society-Rich Ling-Google Books. Available online: https://books.google.dz/books?hl=en&lr=&id=oSwCQ6y6wq8C&oi=fnd&pg=PP1&dq=42.%09Ling,+R.,+2004.+The+mobile+connection:+The+cell+phone%E2%80%99s+impact+on+society.+Elsevier.&ots=6N2A3qiEdU&sig=l0mULTKMLD4DMG5WHRo7MCfsFEA&redir_esc=y#v=onepage&q=42.%09Ling%2C%20R.%2C%202004.%20The%20mobile%20connection%3A%20The%20cell%20phone%E2%80%99s%20impact%20on%20society.%20Elsevier.&f=false (accessed on 22 March 2022).
- Mechael, P.N. Exploring Health-related Uses of Mobile Phones: An Egyptian Case Study. Doctoral Dissertation, University of London, London, UK, 2007; p. 264. [Google Scholar]
- Lacal, J.C. Proceedings. 5th International Workshop on Enterprise Networking and Computing in Healthcare Industry (IEEE Cat. No.03EX717). In Proceedings of the 18th IEEE International Symposium on Defect and Fault Tolerance in VLSI Systems, Santa Monica, CA, USA, 7 June 2003; p. 1218710. [Google Scholar] [CrossRef]
- Bukachi, F.; Pakenham-Walsh, N. Information Technology for Health in Developing Countries. Chest 2007, 132, 1624–1630. [Google Scholar] [CrossRef] [Green Version]
- Wald, H.S.; Dube, C.E.; Anthony, D.C. Untangling the Web—The impact of Internet use on health care and the physician–patient relationship. Patient Educ. Couns. 2007, 68, 218–224. [Google Scholar] [CrossRef]
- Bankole, F.O.; Osei-Bryson, K.-M.; Brown, I. The Impact of ICT Investments on Human Development: A Regression Splines Analysis. J. Glob. Inf. Technol. Manag. 2013, 16, 59–85. [Google Scholar] [CrossRef] [Green Version]
- Lucas, H. Information and communications technology for future health systems in developing countries. Soc. Sci. Med. 2008, 66, 2122–2132. [Google Scholar] [CrossRef]
- Blaya, J.A.; Fraser, H.S.F.; Holt, B. E-Health Technologies Show Promise In Developing Countries. Health Aff. 2010, 29, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Cole-Lewis, H.; Kershaw, T. Text Messaging as a Tool for Behavior Change in Disease Prevention and Management. Epidemiol. Rev. 2010, 32, 56–69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibbons, M.C.; Fleisher, L.; Slamon, R.E.; Bass, S.; Kandadai, V.; Beck, J.R. Exploring the Potential of Web 2.0 to Address Health Disparities. J. Health Commun. 2011, 16, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Déglise, C.; Suggs, L.S.; Odermatt, P. SMS for disease control in developing countries: A systematic review of mobile health applications. J. Telemed. Telecare 2012, 18, 273–281. [Google Scholar] [CrossRef]
- Nilseng, J.; Gustafsson, L.L.; Nungu, A.; Bastholm-Rahmner, P.; Mazali, D.; Pehrson, B.; Eriksen, J. A cross-sectional pilot study assessing needs and attitudes to implementation of Information and Communication Technology for rational use of medicines among healthcare staff in rural Tanzania. BMC Med. Inform. Decis. Mak. 2014, 14, 78. [Google Scholar] [CrossRef] [Green Version]
- Fedha, T. Impact of Mobile Telephone on Maternal Health Service Care: A Case of Njoro Division. Open J. Prev. Med. 2014, 4, 365–376. [Google Scholar] [CrossRef] [Green Version]
- Nasir, S.; Kalirajan, K. Information and Communication Technology-Enabled Modern Services Export Performances of Asian Economies. Asian Dev. Rev. 2016, 33, 1–27. [Google Scholar] [CrossRef]
- Cole, J.; Watkins, C.; Kleine, D. Health Advice from Internet Discussion Forums: How Bad Is Dangerous? J. Med. Internet Res. 2016, 18, e4. [Google Scholar] [CrossRef] [Green Version]
- Tsai, Y.-Y.; Chao, C.-M.; Lin, H.-M.; Cheng, B.-W. Nursing staff intentions to continuously use a blended e-learning system from an integrative perspective. Qual. Quant. 2017, 52, 2495–2513. [Google Scholar] [CrossRef]
- Kiley, R. Does the internet harm health? BMJ 2002, 324, 238–239. [Google Scholar] [CrossRef]
- Murray, E.; Lo, B.; Pollack, L.; Donelan, K.; Catania, J.; White, M.; Zapert, K.; Turner, R. The Impact of Health Information on the Internet on the Physician-Patient Relationship: Patient Perceptions. Arch. Intern. Med. 2003, 163, 1727–1734. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morawczynski, O.; Ngwenyama, O. Unraveling the Impact of Investments in ICT, Education and Health on Development: An Analysis of Archival Data of Five West African Countries Using Regression Splines. Electron. J. Inf. Syst. Dev. Ctries. 2007, 29, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Ngwenyama, O.; Andoh-Baidoo, F.K.; Bollou, F.; Morawczynski, O. Is There A Relationship Between ICT, Health, Education And Development? An Empirical Analysis of five West African Countries from 1997-2003. Electron. J. Inf. Syst. Dev. Ctries. 2006, 23, 1–11. [Google Scholar] [CrossRef]
- Bend, J. Public Value and Ehealth. Institute for Public Policy Research. 2004. Available online: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.515.8120&rep=rep1&type=pdf (accessed on 22 March 2022).
- Tanis, M.; Hartmann, T.; Poel, F.T. Online health anxiety and consultation satisfaction: A quantitative exploratory study on their relations. Patient Educ. Couns. 2016, 99, 1227–1232. [Google Scholar] [CrossRef]
- Kleinke, K. Multiple Imputation Under Violated Distributional Assumptions: A Systematic Evaluation of the Assumed Robustness of Predictive Mean Matching. J. Educ. Behav. Stat. 2017, 42, 371–404. [Google Scholar] [CrossRef]
- van Buuren, S.; Brand, J.P.L.; Groothuis-Oudshoorn, C.G.M.; Rubin, D.B. Fully conditional specification in multivariate imputation. J. Stat. Comput. Simul. 2006, 76, 1049–1064. [Google Scholar] [CrossRef]
- Grossman, M. On the Concept of Health Capital and the Demand for Health. J. Politi-Econ. 1972, 80, 223–255. [Google Scholar] [CrossRef] [Green Version]
- Fayissa, B.; Gutema, P. The Determinants of Health Status in Sub-Saharan Africa (Ssa). Am. Econ. 2005, 49, 60–66. [Google Scholar] [CrossRef]
- Hoechle, D. Robust Standard Errors for Panel Regressions with Cross-Sectional Dependence. Stata J. Promot. Commun. Stat. Stata 2007, 7, 281–312. [Google Scholar] [CrossRef] [Green Version]
- Driscoll, J.C.; Kraay, A.C. Consistent Covariance Matrix Estimation with Spatially Dependent Panel Data. Rev. Econ. Stat. 1998, 80, 549–560. [Google Scholar] [CrossRef]
- Pesaran, M.H. Estimation and Inference in Large Heterogeneous Panels with a Multifactor Error Structure. Econometrica 2006, 74, 967–1012. [Google Scholar] [CrossRef] [Green Version]
- Bai, J. “Panel Data Models With Interactive Fixed Effects. Econometrica 2009, 77, 1229–1279. [Google Scholar] [CrossRef] [Green Version]
- Juodis, A.; Karabiyik, H.; Westerlund, J. On the robustness of the pooled CCE estimator. J. Econ. 2020, 220, 325–348. [Google Scholar] [CrossRef]
- Lee, M.-H.; Liu, P.-Y.; Lio, M.-C. The Impact of the Diffusion of Information and Communication Technology on Health: A Cross-Country Study. Appl. Res. Qual. Life 2014, 11, 471–491. [Google Scholar] [CrossRef]
- Shi, W.; Lee, L. Spatial dynamic panel data models with interactive fixed effects. J. Econ. 2017, 197, 323–347. [Google Scholar] [CrossRef]
- Im, K.S.; Pesaran, M.H.; Shin, Y. Testing for unit roots in heterogeneous panels. J. Econ. 2003, 115, 53–74. [Google Scholar] [CrossRef]
- Levin, A.; Lin, C.-F.; Chu, C.-S.J. Unit root tests in panel data: Asymptotic and finite-sample properties. J. Econ. 2002, 108, 1–24. [Google Scholar] [CrossRef]
- Pesaran, M.H. A simple panel unit root test in the presence of cross-section dependence. J. Appl. Econ. 2007, 22, 265–312. [Google Scholar] [CrossRef] [Green Version]
- Granger, C.W.J. Investigating Causal Relations by Econometric Models and Cross-spectral Methods. Econometrica 1969, 37, 424–438. [Google Scholar] [CrossRef]
- Dumitrescu, E.-I.; Hurlin, C. Testing for Granger non-causality in heterogeneous panels. Econ. Model. 2012, 29, 1450–1460. [Google Scholar] [CrossRef] [Green Version]
- Lopez, L.; Weber, S. Testing for Granger Causality in Panel Data. Stata J. Promot. Commun. Stat. Stata 2017, 17, 972–984. [Google Scholar] [CrossRef] [Green Version]
- Lu, X.; Su, L.; White, H. Granger Causality and Structural Causality in Cross-Section and Panel Data. Econ. Theory 2016, 33, 263–291. [Google Scholar] [CrossRef] [Green Version]
- Breusch, T.S.; Pagan, A.R. The Lagrange Multiplier Test and its Applications to Model Specification in Econometrics. Rev. Econ. Stud. 1980, 47, 239–253. [Google Scholar] [CrossRef]
- Pesaran, M.H. General diagnostic tests for cross-sectional dependence in panels. Empir. Econ. 2021, 60, 13–50. [Google Scholar] [CrossRef]
- Hausman, J.A. Specification Tests in Econometrics. Econometrica 1978, 46, 1251–1271. [Google Scholar] [CrossRef] [Green Version]



| Symbol | Descriptive Statistic | ||||
|---|---|---|---|---|---|
| mean | SD | min | max | Median | |
| Dependent Variables | |||||
| INFM | 67.14 | 24.502 | 13.80 | 142.40 | 66.25 |
| CMU5 | 104.12 | 44.740 | 16.10 | 234.00 | 101.05 |
| Independent Variables | |||||
| IU | 4.561 | 6.519 | 0.004 | 34.253 | 1.549 |
| FTS | 1.528 | 3.307 | 0.005 | 22.620 | 0.504 |
| MCS | 28.685 | 29.752 | 0.018 | 138.80 | 20.008 |
| Control Variables | |||||
| GDP | 546.1 | 330.13 | 111.9 | 2032.6 | 467.7 |
| SCH | 93.17 | 29.436 | 16.63 | 156.03 | 92.38 |
| IM | 69.38 | 18.056 | 16.00 | 99.00 | 70.00 |
| IDPT | 70.31 | 19.570 | 19.00 | 99.00 | 74.00 |
| HE | 30.242 | 19.067 | 4.691 | 139.75 | 24.814 |
| ADR | 90.09 | 11.710 | 56.61 | 111.94 | 91.06 |
| SR | 1.038 | 0.014 | 1.010 | 1.071 | 1.030 |
| UP | 29.744 | 11.374 | 8.246 | 55.60 | 29.909 |
| CO2E | 0.246 | 0.497 | 0.017 | 3.343 | 0.0947 |
| Instrumental Variables | |||||
| ICC | 0.277 | 0.448 | 0.000 | 1.000 | 0.000 |
| CCSEB | 6.988 | 6.408 | 0.144 | 42.219 | 5.631 |
| lnCMU5 | lnINFM | |||||
|---|---|---|---|---|---|---|
| Ztilde | Zbar | Wbar | Ztilde | Zbar | Wbar | |
| lnIU | 8.703 *** | 12.19 *** | 4.317 *** | 8.273 *** | 11.618 *** | 4.162 *** |
| lnFTS | 12.489 *** | 17.225 *** | 5.688 *** | 13.606 *** | 18.711 *** | 6.092 *** |
| lnMCS | 39.138 *** | 52.674 *** | 15.336 *** | 35.051 *** | 47.237 *** | 13.856 *** |
| INFM | CMU5 | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| lnIU | −0.070 *** | −0.040 *** | −0.059 *** | −0.051 *** | ||||
| 0.016 | (0.012) | 0.011 | (0.018) | |||||
| lnFTS | 0.003 | 0.006 | 0.001 | 0.008 | ||||
| 0.013 | (0.009) | 0.010 | (0.013) | |||||
| lnMCS | −0.059 *** | −0.030 *** | −0.052 *** | −0.031 *** | ||||
| 0.011 | (0.005) | 0.009 | (0.007) | |||||
| lnGDP | −0.152 *** | −0.286 *** | −0.124 *** | −0.073 *** | −0.114 *** | −0.226 *** | −0.084 *** | −0.110 *** |
| 0.027 | 0.059 | 0.036 | (0.024) | 0.024 | 0.050 | 0.031 | (0.026) | |
| lnSCH | −0.084 | −0.139 | −0.069 | −0.003 | −0.025 | −0.071** | −0.008 | −0.062 |
| 0.071 | 0.065 | 0.070 | (0.038) | 0.038 | 0.031 | 0.037 | (0.073) | |
| lnIM | 0.142 *** | 0.197 *** | 0.191 *** | 0.120 *** | 0.110 ** | 0.157 *** | 0.151 *** | 0.151 *** |
| 0.047 | 0.041 | 0.040 | (0.036) | 0.046 | 0.031 | 0.028 | (0.037) | |
| lnIDPT | −0.167 *** | −0.237 *** | −0.197 *** | −0.120 *** | −0.121 *** | −0.180 *** | −0.144 *** | −0.165 *** |
| 0.047 | 0.064 | 0.058 | (0.027) | 0.037 | 0.047 | 0.039 | (0.040) | |
| lnHE | −0.076 | −0.142 *** | −0.089 ** | −0.071 | −0.083 ** | −0.138 *** | −0.091 ** | −0.064 |
| 0.052 | 0.044 | 0.044 | (0.044) | 0.041 | 0.036 | 0.037 | (0.055) | |
| lnADR | −0.080 | 0.075 | 0.034 | 0.127 | 0.105 | 0.235 * | 0.198 * | −0.057 |
| 0.125 | 0.154 | 0.139 | (0.106) | 0.096 | 0.125 | 0.111 | (0.136) | |
| lnSR | −23.289 *** | −25.727 *** | −26.321 *** | −19.500 *** | −18.768 *** | −20.850 *** | −21.333 *** | −23.955 *** |
| 5.412 | 6.082 | 5.044 | (3.190) | 4.057 | 4.589 | 3.659 | (4.291) | |
| lnUP | −0.079 * | −0.148 ** | −0.100 ** | −0.033 | −0.042 | −0.100 * | −0.057 | −0.069 |
| 0.048 | 0.068 | 0.050 | (0.038) | 0.040 | 0.058 | 0.040 | (0.045) | |
| lnCO2E | 0.039 ** | 0.064 *** | 0.050 *** | 0.025** | 0.026** | 0.048 *** | 0.035 *** | 0.037 ** |
| 0.015 | 0.010 | 0.013 | (0.010) | 0.011 | 0.007 | 0.009 | (0.015) | |
| R2 | 0.850 | 0.805 | 0.846 | 0.859 | 0.825 | 0.781 | 0.817 | 0.832 |
| Adj. R2 | 0.838 | 0.789 | 0.834 | 0.847 | 0.811 | 0.764 | 0.803 | 0.818 |
| F-Stat | 254.624 *** | 184.781 *** | 246.956 *** | 227.488 *** | 211.733 *** | 211.733 *** | 211.733 *** | 184.226 *** |
| Lagrange Multiplier Test (Breusch–Pagan) for balanced panels, X2 | ||||||||
| 1984.1 *** | 1846.2 *** | 1984.1 *** | 1930.7 *** | 1670.5 *** | 1603.2 *** | 1670.5 *** | 1665.3 *** | |
| F test for individual effects | ||||||||
| 124.83 *** | 95.708 *** | 131.94 *** | 126.42 *** | 88.073 *** | 71.707 *** | 91.224 *** | 88.682 *** | |
| Breusch–Pagan LM test for cross-sectional dependence in panels | ||||||||
| 1485.8 *** | 1333.9 *** | 1595.3 *** | 1609 *** | 1381.9 *** | 1287.7 *** | 1549.1 *** | 1565 *** | |
| Pesaran CD test for cross-sectional dependence in panels | ||||||||
| 1572.8 *** | 1380.5 *** | 1661.4 *** | 7.690 *** | 1573.6 *** | 1363.9 *** | 1646.9 *** | 9.518 *** | |
| Hausman Test | ||||||||
| 111.79 *** | 69.428 *** | 553.31 *** | 242.09 *** | 117.69 *** | 80.781 *** | 222.17 *** | 145 *** | |
| CMU5 | INFM | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| lnIU | −0.053 | −0.012 | −0.049 | −0.010 | ||||
| 0.047 | (0.010) | 0.042 | (0.006) | |||||
| lnFTS | −0.007 | −0.005 | −0.006 | −0.004 | ||||
| 0.010 | (0.011) | 0.007 | (0.008) | |||||
| lnMCS | −0.028 *** | −0.023 *** | −0.023 *** | −0.020 *** | ||||
| 0.006 | (0.007) | 0.006 | (0.006) | |||||
| lnGDP | −0.083 * | −0.115 ** | −0.092 ** | −0.083 ** | −0.048 | −0.078 * | −0.058 * | −0.051 |
| 0.045 | 0.046 | 0.040 | (0.039) | 0.036 | 0.040 | 0.034 | (0.034) | |
| lnSCH | −0.042 | −0.050 | −0.037 | −0.038 | 0.013 | 0.006 | 0.017 | 0.016 |
| 0.075 | 0.071 | 0.071 | (0.072) | 0.041 | 0.037 | 0.037 | (0.037) | |
| lnIM | 0.157 *** | 0.221 *** | 0.193 *** | 0.185 *** | 0.126 *** | 0.185 *** | 0.162 *** | 0.155 *** |
| 0.056 | 0.039 | 0.029 | (0.035) | 0.062 | 0.040 | 0.031 | (0.038) | |
| lnIDPT | −0.185 *** | −0.234 *** | −0.213 *** | −0.205 *** | −0.135 *** | −0.180 *** | −0.162 *** | −0.156 *** |
| 0.034 | 0.044 | 0.042 | (0.038) | 0.028 | 0.026 | 0.024 | (0.023) | |
| lnHE | −0.059 | −0.083 | −0.075 | −0.073 | −0.065 | −0.087 ** | −0.080 ** | −0.079 * |
| 0.051 | 0.051 | 0.049 | (0.055) | 0.044 | 0.041 | 0.039 | (0.044) | |
| lnADR | −0.091 | −0.009 | −0.013 | −0.031 | 0.090 | 0.166 | 0.163 | 0.148 |
| 0.108 | 0.128 | 0.135 | (0.138) | 0.091 | 0.101 | 0.107 | (0.107) | |
| lnSR | −19.318 *** | −19.364 *** | −20.299 *** | −20.315 *** | −15.645 *** | −15.671 *** | −16.456 *** | −16.478 *** |
| 4.973 | 4.864 | 4.570 | (4.343) | 3.768 | 3.683 | 3.462 | (3.341) | |
| lnUP | −0.022 | −0.027 | −0.034 | −0.035 | 0.009 | 0.005 | −0.001 | −0.001 |
| 0.024 | 0.034 | 0.030 | (0.024) | 0.017 | 0.027 | 0.023 | (0.019) | |
| lnCO2E | 0.000 | −0.003 | −0.004 | −0.002 | −0.002 | −0.005 | −0.005 | −0.004 |
| 0.015 | 0.008 | 0.006 | (0.008) | 0.012 | 0.005 | 0.004 | (0.006) | |
| R-Squared: | 0.261 | 0.276 | 0.290 | 0.296 | 0.290 | 0.316 | 0.333 | 0.339 |
| Adj. R-Squared: | 0.170 | 0.187 | 0.203 | 0.206 | 0.203 | 0.232 | 0.252 | 0.255 |
| F-statistic on 10 and 432 DF | 160.452 | 164.994 | 177.230 | 15.039 | 190.025 | 200.290 | 216.549 | 18.387 |
| CMU5 | INFM | |||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| lnIU | −0.003 *** | −0.001 | −0.002 *** | −0.001 | ||||
| (0.001) | (0.001) | (0.001) | (0.001) | |||||
| lnFTS | 0.000 | −0.011 ** | −0.002 | −0.006 ** | ||||
| (0.002) | (0.004) | (0.003) | (0.002) | |||||
| lnMCS | 0.000 | 0.002 *** | −0.001 | 0.000 | ||||
| (0.001) | (0.001) | (0.001) | (0.001) | |||||
| lnGDP | −0.001 | −0.009 | −0.004 | 0.005 | −0.006 ** | −0.012 * | −0.005 * | −0.005 |
| (0.005) | (0.007) | (0.003) | (0.007) | (0.003) | (0.007) | (0.003) | (0.003) | |
| lnSCH | 0.002 | −0.009 | −0.005 | −0.023 ** | −0.006 * | −0.031 ** | −0.009 ** | −0.012 * |
| (0.004) | (0.006) | (0.004) | (0.009) | (0.003) | (0.012) | (0.004) | (0.006) | |
| lnIM | 0.012 *** | 0.029 *** | −0.004 | −0.026 ** | 0.005 | 0.014 ** | −0.01 ** | −0.016 ** |
| (0.004) | (0.01) | (0.008) | (0.013) | (0.003) | −0.006 | (0.004) | (0.008) | |
| lnIDPT | −0.021 *** | −0.017 ** | 0.000 | 0.016 * | −0.013 *** | −0.010 | 0.006 * | 0.013 ** |
| (0.005) | (0.009) | (0.007) | (0.01) | (0.003) | (0.009) | (0.003) | (0.006) | |
| lnHE | −0.001 | −0.015 *** | 0.008 *** | 0.015 ** | 0.001 | −0.006 ** | 0.009 *** | 0.012 *** |
| (0.004) | (0.004) | (0.003) | (0.006) | (0.002) | (0.003) | (0.001) | (0.004) | |
| lnADR | 0.115 *** | 0.129 *** | −0.105 | −0.159 * | 0.033 | 0.071 ** | −0.159 *** | −0.169 *** |
| (0.026) | (0.025) | (0.074) | (0.087) | (0.023) | (0.03) | (0.04) | (0.04) | |
| lnSR | −0.141 | −0.120 | −0.007 | −2.665 ** | 0.051 | 0.068 | 0.227 | −0.888 |
| (0.794) | (0.933) | (0.736) | (1.076) | (0.618) | (1.154) | (0.58) | (0.928) | |
| lnUP | −0.069 | 0.125 | 0.075 ** | 0.118 ** | 0.025 | 0.203 *** | 0.136 *** | 0.185 *** |
| (0.051) | (0.079) | (0.037) | (0.046) | (0.055) | (0.059) | (0.02) | (0.036) | |
| lnCO2E | −0.009 *** | −0.007 *** | −0.009 *** | −0.009 *** | −0.004 *** | −0.006 *** | −0.005 *** | −0.005 *** |
| (0.002) | (0.001) | (0.002) | (0.002) | (0.001) | (0.002) | (0.001) | (0.001) | |
| Total Sum of Squares: | 131,245 | 131,245 | 131,245 | 131,245 | 90,734 | 90,734 | 90,734 | 90,734 |
| Residual Sum of Squares: | 0.017 | 0.038 | 0.013 | 0.008 | 0.009 | 0.023 | 0.006 | 0.003 |
| HPY R2: | 0.998 | 0.996 | 0.999 | 0.999 | 0.999 | 0.997 | 0.999 | 0.999 |
| INFM | CMU5 | |||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| IU | −0.093 *** | −0.105 *** | ||||
| (0.026) | (0.030) | |||||
| FTS | −0.051 | −0.046 | ||||
| (0.033) | (0.037) | |||||
| MCS | −0.036 | −0.040 | ||||
| (0.024) | (0.027) | |||||
| GDP | −0.170 * | −0.281 ** | −0.270 ** | −0.136 | −0.271 ** | −0.249 ** |
| (0.091) | (0.124) | (0.109) | (0.102) | (0.134) | (0.117) | |
| SCH | −0.132 | −0.167 | −0.181 * | −0.276 *** | −0.317 *** | −0.331 *** |
| (0.097) | (0.102) | (0.095) | (0.102) | (0.104) | (0.100) | |
| IM | −0.292 | −0.122 | −0.176 | −0.370 | −0.181 | −0.238 |
| (0.319) | (0.314) | (0.321) | (0.342) | (0.342) | (0.347) | |
| IDPT | 0.252 | 0.118 | 0.165 | 0.313 | 0.159 | 0.213 |
| (0.316) | (0.327) | (0.330) | (0.332) | (0.352) | (0.349) | |
| HE | 0.115 | −0.001 | 0.070 | 0.127 | 0.003 | 0.076 |
| (0.084) | (0.105) | (0.101) | (0.091) | (0.112) | (0.111) | |
| ADR | 1.176 *** | 1.104 *** | 1.176 *** | 1.172 *** | 1.468 *** | 1.382 *** |
| (0.096) | (0.110) | (0.096) | (0.102) | (0.106) | (0.108) | |
| SR | −2.547 | −3.824 * | −2.547 | −6.324 *** | −5.040 * | −6.285 *** |
| (2.576) | (2.221) | (2.576) | (2.030) | (2.718) | (2.214) | |
| UP | 0.395 *** | 0.388 *** | 0.431 *** | 0.333 *** | 0.334 *** | 0.374 *** |
| (0.075) | (0.101) | (0.088) | (0.088) | (0.110) | (0.098) | |
| CO2E | −0.136 ** | −0.054 | −0.114 ** | −0.155 ** | −0.070 | −0.130 ** |
| (0.064) | (0.044) | (0.056) | (0.068) | (0.049) | (0.060) | |
| Sargan test: chisq (162) = | 27 | 27 | 27 | 27 | 27 | 27 |
| p-value = | 1 | 1 | 1 | 1 | 1 | 1 |
| Autocorrelation test (1): normal = | −1.230 | −0.615 | −0.957 | −1.595 | −1.168 | −1.405 |
| p-value = | 0.219 | 0.538 | 0.338 | 0.111 | 0.243 | 0.160 |
| Autocorrelation test (2): normal = | −0.432 | −0.187 | −0.410 | −0.693 | −0.361 | −0.529 |
| p-value = | 0.665 | 0.852 | 0.682 | 0.489 | 0.718 | 0.597 |
| Wald test for coefficients: chisq (10) = | 37,675.47 | 25,405.61 | 27,954.66 | 63,688.66 | 27,759.88 | 32,799.97 |
| p-value = | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khelfaoui, I.; Xie, Y.; Hafeez, M.; Ahmed, D.; Degha, H.E.; Meskher, H. Information Communication Technology and Infant Mortality in Low-Income Countries: Empirical Study Using Panel Data Models. Int. J. Environ. Res. Public Health 2022, 19, 7338. https://doi.org/10.3390/ijerph19127338
Khelfaoui I, Xie Y, Hafeez M, Ahmed D, Degha HE, Meskher H. Information Communication Technology and Infant Mortality in Low-Income Countries: Empirical Study Using Panel Data Models. International Journal of Environmental Research and Public Health. 2022; 19(12):7338. https://doi.org/10.3390/ijerph19127338
Chicago/Turabian StyleKhelfaoui, Issam, Yuantao Xie, Muhammad Hafeez, Danish Ahmed, Houssem Eddine Degha, and Hicham Meskher. 2022. "Information Communication Technology and Infant Mortality in Low-Income Countries: Empirical Study Using Panel Data Models" International Journal of Environmental Research and Public Health 19, no. 12: 7338. https://doi.org/10.3390/ijerph19127338







