Health Economic Challenge: Geriatric Trauma—An Age-Based Observational Analysis of Treatment Costs and Reimbursement Issues
Abstract
:1. Introduction
2. Patients and Methods
2.1. Study Design
- U65 = patients aged 18–64 years with mild TBI
- G65 = geriatric patients aged ≥65 years with mild TBI
2.2. Statistical Methods
3. Results
3.1. Demographics and Clinical Data of the Patient Collective
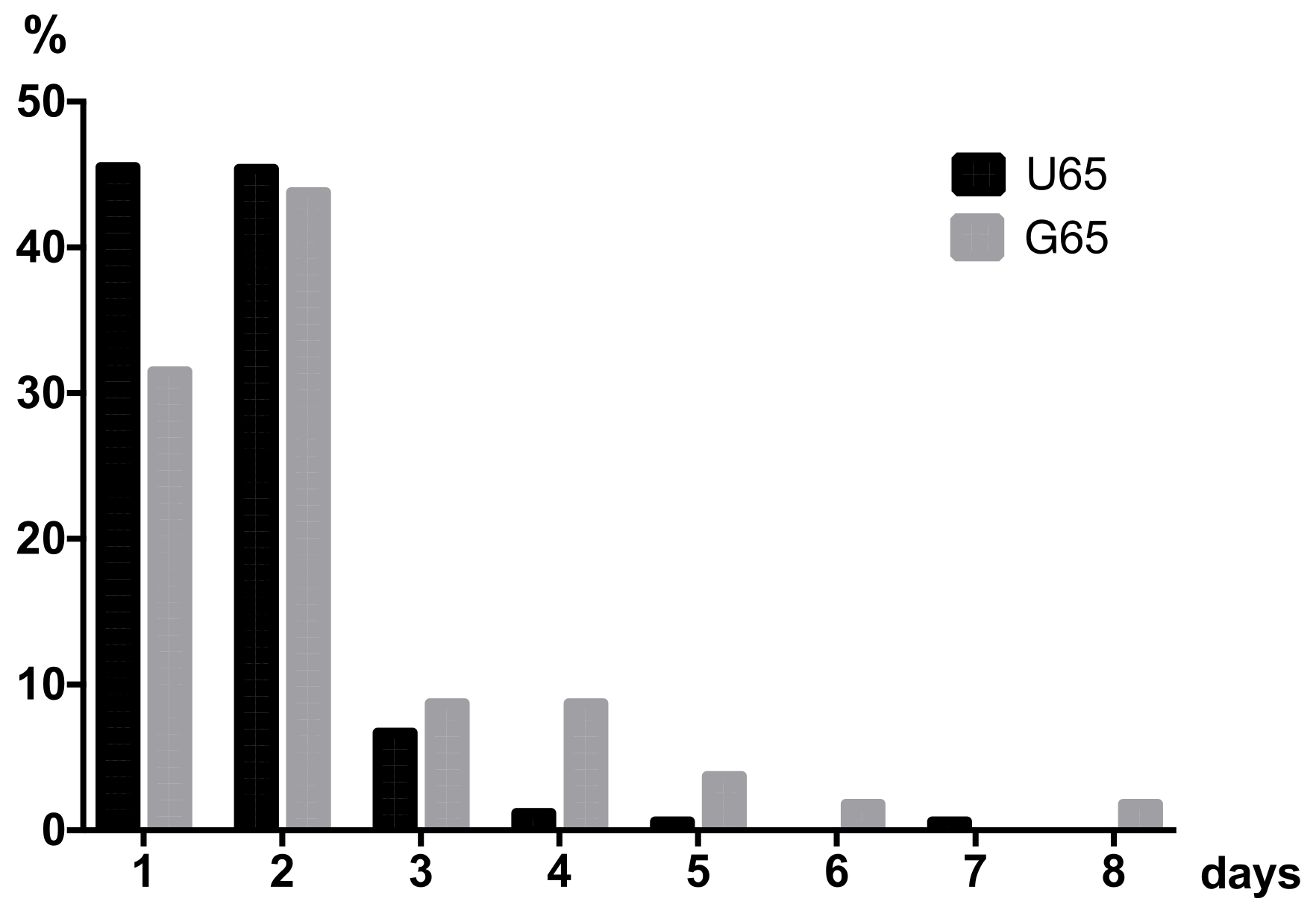
3.2. Length of Stay and Reimbursement Calculation
3.3. Cost Calculation
3.3.1. Total Costs of Admission Treatment in the ED
3.3.2. Total Costs of Inpatient Treatment
3.3.3. Comparison of the Cost-Proceeds Calculation for U65 vs. G65
4. Discussion
4.1. Risk Factors in mTBI among Geriatric Patients: Anticoagulation and Co-Morbidity
4.2. Social Care Deficit Leads to Hospitalization
4.3. G65: Higher Costs due to Longer In-Hospital Treatment
4.4. Challenge of Geriatric mTBI: Same Reimbursement but Higher Costs
4.5. Adjustment of Reimbursement to Demographic Change Required
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| U65 | G65 | |||||
|---|---|---|---|---|---|---|
| LOS (d) | EAR | B80Z (€) | n | R (€) | n | R (€) |
| 1 | 0.224 | 794.07 | 74 | 58,761.18 | 18 | 14,293.26 |
| 2 | 0.366 | 1297.46 | 74 | 96,012.04 | 25 | 32,436.50 |
| 3 | 0.366 | 1297.46 | 11 | 14,272.06 | 5 | 6487.30 |
| 4 | 0.479 | 1698.04 | 2 | 3396.08 | 3 | 5094.12 |
| 5 | 0.592 | 2098.62 | 1 | 2098.62 | 1 | 2098.62 |
| 6 | 0.705 | 2499.20 | 0 | 1 | 2499.20 | |
| 7 | 0.818 | 2899.79 | 1 | 2899.79 | 0 | |
| 8 | 0.931 | 3300.37 | 0 | 3 | 9901.11 | |
| 9 | 1.044 | 3700.95 | 0 | 1 | 3700.95 | |
| Reimbursement (total): | 163 | 174,043.69 | 57 | 76,511.06 | ||
| Average per case: | 1 | 1067.75 | 1 | 1342.30 | ||
Appendix B
Appendix B.1. Personnel Cost Calculation
| Physician | Grade (Year) | Annual Salery (€) | Incl. 19.435% (€) |
|---|---|---|---|
| 1 | 57,253.92 | 69,735.72 | |
| 4 | 67,737.12 | 81,579.72 | |
| 7 | 75,148.32 | 89,952.84 | |
| Ø Annual cost: | 80,422.76 | ||
| Annual gross hours | 365–114 days (weekends and holidays 2019) = 251 days | ||
| 42 h/ 5 days = 8.4 working h per day 251 days × 8.4 h = 2108.4 working h per year | |||
| Annual net hours | 2108.4 h per year–2.1% nonproductive rate = 2064.1 h = 12,3846 min | ||
| Cost per minute | €80,422.76/12,3846 min = 0.649€ per min | ||
| Nursing Staff | Grade (Year) | Annual Salery (€) | Incl. 19.435% (€) |
|---|---|---|---|
| 3 (NW) | 35,669.28 | 43,607.52 | |
| 5 (NW) | 40,408.44 | 49,401.36 | |
| 3 (NED) | 37,407.36 | 45,732.48 | |
| 5 (NED) | 41,435.40 | 50,656.80 | |
| Ø Annual cost NW | 46,504.44 | ||
| Ø Annual cost NED | 48,194.64 | ||
| Annual gross hours | 365–114 days (weekends and holidays 2019) = 251 days | ||
| 38.5 h/5 days = 7.7 working h per day 251 days × 7.7 h = 1940.4 working h per year | |||
| Annual net hours | 1940.4 h per year–6.85% nonproductive rate = 1807.5 h = 10,8450 min | ||
| Cost per minute NW | €46,504.44/108450 min = €0.429/min | ||
| Cost per minute NED | €48,194.64/108450 min = €0.444/min | ||
Appendix B.2. ED Pesonnel Cost Calculation (per Minute Costs)
Appendix B.3. Inpatient Cost Calculation
| U65 | G65 | ||||
|---|---|---|---|---|---|
| Price (€) | n | Costs (€) | n | Costs (€) | |
| Trauma ward | |||||
| Flate-rate | 300.00 | 214 | 64,200.00 | 76 | 22,800.00 |
| Routine blood tests | 22.45 | 3 | 67.35 | 13 | 291.85 |
| P | 8.44/17.52 | 214 | 1806.16 | 76 | 1331.52 |
| NW | 11.15/33.89 | 214 | 2386.10 | 76 | 2575.64 |
| Total costs | 214 | 68,459.61 | 76 | 26,999.01 | |
| Ø Costs per day | 319.90 | 355.25 | |||
| Ø Cost per patient/case (n = 127/32) | 539.05 | 843.72 | |||
| ED | |||||
| Flat-rate | 512.00 | 61 | 31,232.00 | 63 | 12,800.00 |
| Routine blood tests | 0.37 | 89 | 32.93 | 62 | 22.94 |
| P | 43.48/49.32 | 61 | 2652.28 | 63 | 3207.26 |
| Total costs | 61 | 20,026.51 | 63 | 14,052.24 | |
| Ø Costs per day | 328.30 | 223.05 | |||
| Ø Cost per patient/case (n = 36/25) | 556.29 | 562.09 | |||
References
- Saß, A.-C.; Lampert, T.; Prütz, F.; Seeling, S.; Starker, A.; Kroll, L.E.; Rommel, A.; Ryl, L.; Ziese, T. Welche Auswirkungen Hat Der Demografische Wandel Auf Gesundheit Und Gesundheitsversorgung? Gesundh. Deutschland. Gesundh. Des Bundes. Gem. Getragen Von RKI Und Destatis 2015, 9, 432–456. [Google Scholar]
- Yogi, R.R.; Sammy, I.; Paul, J.F.; Nunes, P.; Robertson, P.; Ramcharitar Maharaj, V. Falls in Older People: Comparing Older and Younger Fallers in a Developing Country. Eur. J. Trauma Emerg. Surg. 2018, 44, 567–571. [Google Scholar] [CrossRef]
- Walter, J.; Unterberg, A. Das Schädel-Hirn-Trauma Beim Älteren. Intensivmed. Up2date 2017, 13, 331–341. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk Factors for Falls among Elderly Persons Living in the Community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Schuh, V. Statistisches Jahrbuch 2019—Kapitel 4 Gesundheit. Dtsch. Med. Wochenschr. 2013, 138, 1637. [Google Scholar] [CrossRef]
- Rubenstein, L.Z. Falls in Older People: Epidemiology, Risk Factors and Strategies for Prevention. Age Ageing 2006, 35, ii37–ii41. [Google Scholar] [CrossRef] [Green Version]
- Bücking, B.; Liener, U.; Bliemel, C.; Ruchholtz, S. Unfallchirurgisch-Geriatrisches Co-Management in Der Alterstraumatologie. Orthopädie Und Unf. Up2date 2018, 13, 343–356. [Google Scholar] [CrossRef] [Green Version]
- Geissler, A.; Scheller-Kreinsen, D.; Quentin, W.; Busse, R. DRG-Systeme in Europa. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2012, 55, 633–642. [Google Scholar] [CrossRef]
- Harper, D.L. Critical Appraisal of the DRG System: Problem Areas for DRG Reimbursement in the USA. Aust. Clin. Rev. 1985, 8, 14–21. [Google Scholar]
- Verboket, R.D.; Mühlenfeld, N.; Woschek, M.; Marzi, I.; Pieper, M.; Zöllner, J.P.; Strzelczyk, A.; Willems, L.M. Inpatient Treatment Costs, Cost-Driving Factors and Potential Reimbursement Problems Due to Fall-Related Fractures in Patients with Parkinson’s Disease. Chirurg 2020, 91, 421–427. [Google Scholar] [CrossRef]
- Available online: https://www.dimdi.de/static/de/klassifikationen/icd/icd-10-gm/kode-suche/htmlgm2019/block-s00-s09.htm (accessed on 30 May 2022).
- Reimbursement.info Erstattung 2019 DRG B80Z—Andere Kopfverletzungen. Available online: https://www.aok-gesundheitspartner.de/imperia/md/gpp/bund/krankenhaus/drg_system/gdrg/kh_drg_katalog_2019.pdf (accessed on 30 May 2022).
- McCusker, J.; Bellavance, F.; Cardin, S.; Trépanier, S.; Verdon, J.; Ardman, O. Detection of Older People at Increased Risk of Adverse Health Outcomes after an Emergency Visit: The ISAR Screening Tool. J. Am. Geriatr. Soc. 1999, 47, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Woschek, M.; Schindler, C.R.; Sterz, J.; Störmann, P.; Willems, L.; Marzi, I.; Verboket, R.D. Aufnahmediagnose Prellung: Ätiologie, Epidemiologie Und Kostenfaktoren. Z. Für Gerontol. Und Geriatr. 2020, 54, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Verboket, R.; Verboket, C.; Schöffski, O.; Tlatlik, J.; Marzi, I.; Nau, C. Kosten Und Erlöse von Über Den Schockraum Eingelieferten Patienten Mit Leichtem Schädel-Hirn-Trauma. Unfallchirurg 2019, 122, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Thiem, U.; Greuel, H.W.; Reingräber, A.; Koch-Gwinner, P.; Püllen, R.; Heppner, H.J.; Pfisterer, M. Positionspapier Zur Identifizierung Geriatrischer Patienten in Notaufnahmen in Deutschland. Z. Fur Gerontol. Und Geriatr. 2012, 45, 310–314. [Google Scholar] [CrossRef]
- Maegele, M.; Lefering, R.; Sakowitz, O.; Kopp, M.A.; Schwab, J.M.; Steudel, W.-I.; Unterberg, A.; Hoffmann, R.; Uhl, E.; Marzi, I. The Incidence and Management of Moderate to Severe Head Injury. Dtsch. Aerzteblatt Online 2019, 116, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Leidel, B.A.; Lindner, T.; Wolf, S.; Bogner, V.; Steinbeck, A.; Börner, N.; Peiser, C.; Audebert, H.J.; Biberthaler, P.; Kanz, K.-G. Leichtes Schädel-Hirn-Trauma Bei Kindern Und Erwachsenen. Med. Klin.-Intensivmed. Und Notf. 2015, 110, 379–396. [Google Scholar] [CrossRef] [PubMed]
- Stuke, L.; Diaz-Arrastia, R.; Gentilello, L.M.; Shafi, S. Effect of Alcohol on Glasgow Coma Scale in Head-Injured Patients. Ann. Surg. 2007, 245, 651–655. [Google Scholar] [CrossRef]
- Opreanu, R.; Kuhn, D.; Basson, M. NIH Public Access The Influence of Alcohol on Mortality in Traumatic Brain Injury. J. Am. Coll. Surg. 2012, 29, 997–1003. [Google Scholar] [CrossRef]
- Available online: https://www.uptodate.com/contents/traumatic-brain-injury-epidemiology-classification-and-pathophysiology (accessed on 30 May 2022).
- Cohen, D.B.; Rinker, C.; Wilberger, J.E. Traumatic Brain Injury in Anticoagulated Patients. J. Trauma-Inj. Infect. Crit. Care 2006, 60, 553–557. [Google Scholar] [CrossRef]
- Sartin, R.; Kim, C.; Dissanaike, S. Discussion of: “Is Routine Head CT Indicated in Awake Stable Older Patients after a Ground Level Fall?”. Am. J. Surg. 2017, 214, 1055–1058. [Google Scholar] [CrossRef]
- Lohmann, R.; Haid, K.; Stöckle, U.; Raschke, M. Epidemiologie Und Perspektiven Der Alterstraumatologie. Unfallchirurg 2007, 110, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Schindler, C.R.; Lustenberger, T.; Woschek, M.; Störmann, P.; Henrich, D.; Radermacher, P.; Marzi, I. Severe Traumatic Brain Injury (TBI) Modulates the Kinetic Profile of the Inflammatory Response of Markers for Neuronal Damage. J. Clin. Med. 2020, 9, 1667. [Google Scholar] [CrossRef] [PubMed]
- Vedin, T.; Svensson, S.; Edelhamre, M.; Karlsson, M.; Bergenheim, M.; Larsson, P.-A. Management of Mild Traumatic Brain Injury–Trauma Energy Level and Medical History as Possible Predictors for Intracranial Hemorrhage. Eur. J. Trauma Emerg. Surg. 2019, 45, 901–907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Firsching, A.R.; Rickels, E.; Mauer, U.M.; Sakowitz, O.W.; Dgai, K.E.; Dgn, P.S.; Linn, J.; Vertreter, K.S. S1-Leitlinie SHT. 2015. 109. Available online: https://www.awmf.org/uploads/tx_szleitlinien/008-001m_S2e_Schaedelhirntrauma_SHT_Erwachsene_2015-12-abgelaufen.pdf (accessed on 30 May 2022).
- Taheri, P.A.; Butz, D.A.; Lottenberg, L.; Clawson, A.F.L. The Costs of Trauma Center Readiness. Am. J. Surg. 2002, 187, 7–13. [Google Scholar] [CrossRef] [PubMed]

| DRG B80Z (n = 220) | U65 (n = 163) | G65 (n = 57) | p-Value | |
|---|---|---|---|---|
| Sex (male; %) | 57.3 | 60.1 | 49.1 | 0.157 |
| Age (y; median (IQR)) | 49 (32–66) | 40 (29–51) | 79 (74–86) | |
| ISAR (pts., median (IQR)) | 4 (4–5) | |||
| GCS (pts., median (IQR)) | 15 (14–15) | 15 (14–15) | 15 (15–15) | 0.218 |
| Neurological Symptoms (n, %) | 138 (62.7) | 125 (76.7) | 13 (22.8) | <0.001 |
| Blood alcohol ≥ 0.3‰ (n, %) | 41 (18.6%) | 34 (20.9%) | 7 (12.3%) | <0.001 |
| Oral Anticoagulation (n, %) | 62 (28.2) | 28 (17.2) | 39 (68.4) | <0.001 |
| Relevant disorder (n, %) | 31 (14.1) | 7 (4.3) | 24 (42.1) | 0.002 |
| Social care deficit (n, %) | 42 (19.1) | 23 (14.11) | 19 (33.3) | 0.19 |
| Inpatient days (total; d) | 414 | 275 | 139 | 0.007 |
| Length of stay (d, mean ± SD) | 1.9 ± 1.4 | 1.7 ± 0.8 | 2.4 ± 1.9 | 0.007 |
| U65 (n = 163) | G65 (n = 57) | ||||
|---|---|---|---|---|---|
| Medical Service | Price (€) | n | Costs (€) | n | Costs (€) |
| cCT | 123.44 | 38 | 4690.72 | 54 | 6665.76 |
| X-ray extremities | 29.63 | 27 | 800.01 | 13 | 385.19 |
| X-ray spine | 12.34 | 47 | 579.98 | 43 | 530.62 |
| X-ray pelvis | 12.34 | 9 | 111.06 | 33 | 407.22 |
| X-ray thorax | 11.52 | 32 | 368.64 | 23 | 264.96 |
| Routine blood test | 22.45 | 168 | 3771.60 | 67 | 1504.15 |
| BGA | 0.37 | 173 | 64.01 | 89 | 32.93 |
| Physician (Appendix B) | 15.38/22.65 | 163 | 2506.94 | 57 | 1291.05 |
| Nurse (Appendix B) | 15.50/20.82 | 163 | 2526.50 | 57 | 1186.74 |
| Total costs | 15,419.46 | 12,268.62 | |||
| Ø cost per case | 94.60 | 215.24 | |||
| U65 (n = 163) | G65 (n = 57) | |||
|---|---|---|---|---|
| Costs and Proceeds | n/d | € | d | € |
| ED (n) | 163 | 15,419.46 | 57 | 12,268.62 |
| Trauma ward (d) | 214 | 68,459.61 | 76 | 26,999.01 |
| Monitor bed (d) | 61 | 20,026.51 | 63 | 14,052.24 |
| Total costs | 163 | 103,905.58 | 57 | 53,319.87 |
| Ø Costs per patient/case | 637.46 | 935.44 | ||
| Refund DRG B80Z | 163 | 174,043.69 | 57 | 71,704.07 |
| Ø Refund per patient/case | 1067.75 | 1257.97 | ||
| Cost-proceed difference | 70,138.11 | 18,384.20 | ||
| Ø Difference per patient/case | 430.30 | 322.53 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schindler, C.R.; Woschek, M.; Mühlenfeld, N.; Seifert, L.; Marzi, I.; Störmann, P.; Verboket, R.D. Health Economic Challenge: Geriatric Trauma—An Age-Based Observational Analysis of Treatment Costs and Reimbursement Issues. Int. J. Environ. Res. Public Health 2022, 19, 8270. https://doi.org/10.3390/ijerph19148270
Schindler CR, Woschek M, Mühlenfeld N, Seifert L, Marzi I, Störmann P, Verboket RD. Health Economic Challenge: Geriatric Trauma—An Age-Based Observational Analysis of Treatment Costs and Reimbursement Issues. International Journal of Environmental Research and Public Health. 2022; 19(14):8270. https://doi.org/10.3390/ijerph19148270
Chicago/Turabian StyleSchindler, Cora Rebecca, Mathias Woschek, Nils Mühlenfeld, Lukas Seifert, Ingo Marzi, Philipp Störmann, and René Danilo Verboket. 2022. "Health Economic Challenge: Geriatric Trauma—An Age-Based Observational Analysis of Treatment Costs and Reimbursement Issues" International Journal of Environmental Research and Public Health 19, no. 14: 8270. https://doi.org/10.3390/ijerph19148270
APA StyleSchindler, C. R., Woschek, M., Mühlenfeld, N., Seifert, L., Marzi, I., Störmann, P., & Verboket, R. D. (2022). Health Economic Challenge: Geriatric Trauma—An Age-Based Observational Analysis of Treatment Costs and Reimbursement Issues. International Journal of Environmental Research and Public Health, 19(14), 8270. https://doi.org/10.3390/ijerph19148270






