Abstract
Bilateral amputees are disadvantaged as they lack healthy leg support. We present the rare case of a bilateral transtibial amputee (BTA), in which we compared the first South Korean-made microprocessor-controlled prosthesis (MPA) to a conventional prosthetic ankle (CPA) with gait analysis and a patient questionnaire for long-term outcomes. A 70-year-old man presented with bilateral transtibial amputations from injury. Assessments were performed after wearing an MPA for 1 month and 1 year with three-dimensional gait analysis. Satisfaction, mobility, and pain were evaluated using the Korean version of the Prostheses Evaluation Questionnaire (K-PEQ). The spatiotemporal parameters of both sides showed increased stability from the CPA to 1 month (mMPA) and 1 year (yMPA). We observed an increased single support time, decreased step width, and almost normal stance-swing time ratio. In kinematic parameters, the ankle range of motion (ROM) was bilaterally increased at mMPA and yMPA. Unfortunately, the MPA gait showed insufficient ankle plantarflexion during the terminal stance that failed to generate push-up power. As the MPA adaptation time increased, the symmetry ratio improved to a balanced value. The questionnaire-based investigations of satisfaction, mobility, and pain revealed excellent results. The MPA proved helpful for ankle mobility in the BTA, and the questionnaire showed good satisfaction and mobility in varied terrain.
1. Introduction
Limb amputation is a major change that constrains independent living and quality of life [1,2]. Corresponding with the development of medical technology and prolonged lifespan, loss of the lower extremities from chronic diseases is gradually increasing in frequency [3,4,5,6]. Proper selection of a prosthetic limb to replace the lost extremity is important for rehabilitative gait training [7,8]. Training enables the performance of activities of daily life [9]. It is a critical process that determines the degree of functional ability.
Historically, most lower extremity amputees mainly use artificial knees and feet that passively adjust the joint angle with elastic systems such as springs, hydraulics, and air cylinders. The passive ankle prosthesis is widely used, but it has only one joint resistance, making it impossible to control and offer active feedback while responding to slippery or inclined walking terrain [10,11]. Even when attempts are made to perform appropriate gait rehabilitation, the risk of falls is very high due to the lack of ability to change walking speed, high energy consumption, and low walking stability [11,12,13,14].
To overcome this limitation, the microprocessor-controlled prosthesis (MPA) has been used increasingly since its introduction in the 1990s. The MPA responds actively to gait patterns and the surrounding terrain. Its internal microprocessors control passive characteristics and active movements at both knee and ankle joints. Use of the MPA has increased confidence and safety, reduced cognitive loading, improved energy efficiency, and increased self-selected walking speeds [15,16,17,18,19].
Previously, there have been many papers comparing the recently developed MPA with conventional prosthetic feet (CPF) to lower extremity amputation patients. However, most of the prosthetics used as CPF are not used much now [16], and most of the studies were conducted on unilateral amputees [20].
Compared to unilateral amputees, bilateral amputees are disadvantaged when it comes to ambulation and gait training. They lack the support of a healthy leg. Nevertheless, it is believed that MPAs could also improve the gait for a bilateral transtibial amputee (BTA). There were cases where MPA was applied to bilateral transfemoral amputation, not transtibial level, and the followup period was short [8,21]. The evaluation after the long-term application of MPA in varied terrain can be a strong basis for practical use, but the subjective satisfaction of patients is also very important. Few well-designed studies have been conducted on this to date, despite its importance.
Here, we present the case of a BTA, comparing the first South Korea-made MPA to a conventional prosthesis according to gait analysis and patient satisfaction. Especially with a long-term followup of one year, this will be a meaningful comparison.
2. Materials and Methods
2.1. History
The participant (male, age 70 years, 168.7 cm, 62.4 kg) had injuries to both lower extremities from a landmine explosion in the Vietnam War in 1971, for which he had undergone bilateral transtibial amputation. On presentation, the right side amputation was at 9.9 cm and the left at 7.5 cm below the tibial plateau (Figure 1a,d). Both stump surfaces were cylindrical. The soft tissue shrinkage was intact and healed (Figure 1c). The left lower extremity had a knee flexion contracture of 10° after a distal femur malunion (Figure 1b). He had a functional K-level of 3.

Figure 1.
(a) X-ray of left knee flexion contracture due to distal femur malunion. (b) Flexion contracture of 10° of the left leg. (c) Cylindrical left stump with intact soft tissue shrinkage in healing state. (d) Lower extremities X-ray view with RoFT®. (e,f) The front and side view of participant wearing RoFT®. 19 sensors attached with the Helen-Hayes method to the anterior superior iliac spines, sacrum, thighs (midpoint between the greater trochanter and the lateral femoral head), knee joint, tibial tuberosity, ankle medial and lateral malleolus, heel, and second metatarsal bone. With bilateral prostheses, it is difficult to attach sensors in the correct anatomical position.
He received initial prostheses in 1972, composed of a solid ankle cushion heel (SACH) foot and exoskeletal shank, a patellar tendon-bearing socket, and a fork-strap with a waist belt. From 1972 to 2014, the prosthesis was only used indoors and rarely when going out because of the energy expenditure and discomfort. In 2014, he began wearing the dynamic response feet, Vari-Flex® (Össur EHF, Reykjavik, Iceland). This is a conventional prosthetic ankle (CPA), with a total-surface-bearing design that uses supracondylar pin-shuttle locking suspensions on silicon liners due to the short stump length.
The first South Korean MPA, the RoFT® (Hugo dynamics, Daegu, Korea), was developed in 2017 (Figure 2). Since an MPA has sensors in the ankle joint and on the foot sole, it recognizes varied walking terrain and optimizes movement and force, increasing safety. In 2021, the patient was introduced to the MPA. Gait analysis was performed after an adaptation period of approximately one month. Followup continued for one year (Figure 3).
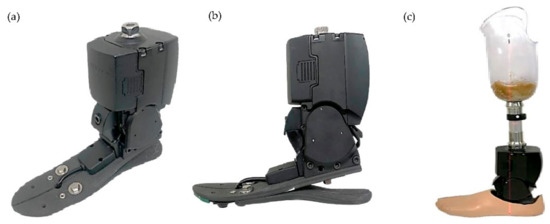
Figure 2.
(a) Oblique and (b) side view of exterior of the RoFT® (Hugo dynamics, Daegu, South Korea). (c) RoFT® with socket. The newly produced MPA in South Korea, RoFT®, works through a motor-driven method and weighs about 1750 g. It uses a battery with a usage time of 4 h after being fully charged, but it can be replaced detachably. Its maximal dorsiflexion angle is 20° and maximal plantarflexion angle is 15°.
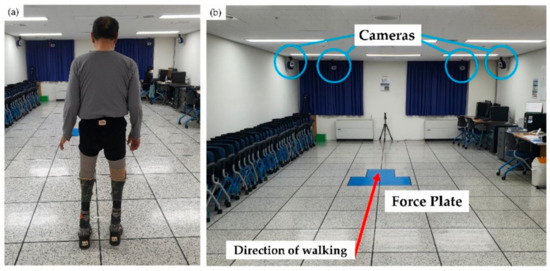
Figure 3.
Experimental setup in the laboratory. (a) The participant standing in front of the force plate with 19 markers placed at landmarks. (b) The eight infrared cameras were mounted in front and back of the walkway.
2.2. Methods
The patient’s gait was recorded with a three-dimensional motion analysis system® (Motion Analysis Corp., Santa Rosa, CA, USA). Markers were attached to anatomical landmarks, and markers for the amputation site were attached by estimating the location on the MPA (Figure 1e,f) [22]. The system tracked the attached 19 markers (Qualysis AB, Goteborg, Sweden) with diameters of 12.5 mm using eight infrared cameras (Raptor-12HS®, Motion Analysis Corp., Rohnert Park, CA, USA), positioned around the treadmill. Raptor-12HS® is considered the best of the motion capture cameras, operating up to 300 Hz at a full resolution of 12.5 Mpixel in a FOV of 64° × 50°. The marker trajectory data were recorded throughout all trials at 100 Hz and recorded in Cortex software® (Motion Analysis Corp., Santa Rosa, CA, USA).
Relative and absolute joint positions were quantified with a tracked marker and calibrated using nonlinear transformation [23]. The record of the tracked markers was analyzed with OrthoTrak® 6.4.4. (Motion Analysis Corp. Santa Rosa, CA, USA).
The ground reaction force (GRF) was collected and calculated through three Kistler 9260AAA® (Kistler Corp., Amherst, NY, USA) platforms. The patient walked at a self-selected speed 15 times along a 10-m walkway. Sufficient rest breaks were taken between each of the 15 “laps.” The initial assessment was completed using the CPAs and the second and third assessments using MPAs after 1 month and 1 year of wear. From the 15 analyses, we chose the most informative components of the evaluation to generate spatiotemporal, kinematic, and kinetic parameters. Symmetry ratios for step lengths and intra-cycle gait phases were calculated by dividing the value of the right foot variable by that of the left foot [24].
The survey was prepared based on the Korean version of the Prosthesis Evaluation Questionnaire (K-PEQ) for the respective compatibility of MPA and CPA [25]. From the eight K-PEQ categories, we selected the four categories of satisfaction, physical sensation, mobility, and unexpected situation occurrence. The referenced questionnaires were divided into three categories: satisfaction, physical sensation, and mobility. Each question was scored on a scale of 1 to 10 using the Likert scale. For questions 1–17 and 22–33, higher scores meant higher satisfaction; for questions 18–21, lower scores meant higher satisfaction. Moreover, the participant was asked about the pros and cons of MPA with open-ended questions.
3. Results
3.1. Spatiotemporal Parameters
At the 1-month MPA (mMPA) and 1-year MPA (yMPA) assessments, both sides showed increased single support time and decreased step width. Stance-swing time ratios were approximately 7:3 for CPA bilaterally, and gradually improved to approximately 6:4 for both mMPA and yMPA, which was close to normal. This was more pronounced on the left side (Table 1). The symmetry ratio approached more perfect balance at mMPA and yMPA than CPA, except for step length and ankle plantarflexion moment.

Table 1.
Comparison of gait analysis between CPA, 1-month MPA, and 1-year MPA.
3.2. Kinematic Parameters
The ankle plantarflexion peak angle at loading response increased for both mMPA and yMPA and was far closer to normal than with CPA (Figure 4A(c),B(c) solid arrow). The ankle dorsiflexion peak angle in the late stance increased more for yMPA than for mMPA (Figure 4A(c),B(c) white arrow). For this reason, the total ankle ROM was the largest for yMPA, followed by those for mMPA and CPA, in that order.
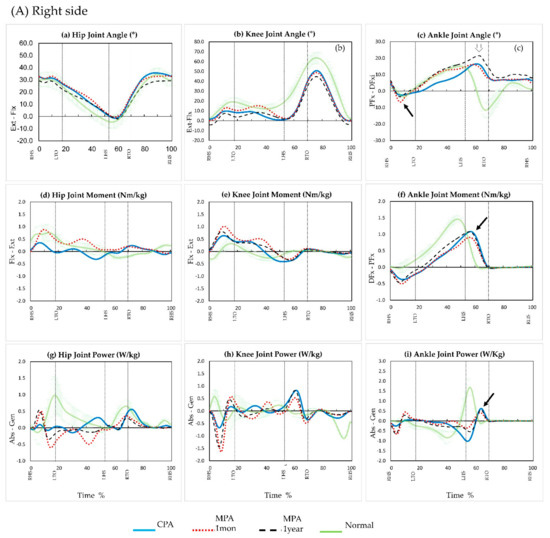
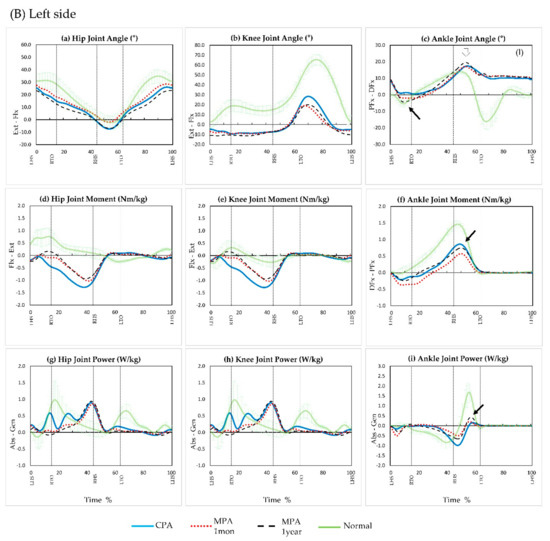
Figure 4.
Graphs illustrating sagittal plane motions, moments, and power of the hip (a,d,g), knee (b,e,h), and ankle (c,f,i) across the gait cycle (0 to 100%) during walking. The green solid line represents group mean data for normal non-amputee individuals. The blue line represents the group mean data for the conventional prosthetic ankle. The red dashed line represents the group mean data for a microprocessor-controlled prosthetic knee after 1 month. The black dashed line represents the group mean data for a microprocessor-controlled prosthetic knee after 1 year. Abbreviations: Flexion (Flx), Extension (Ext), Plantarflexion (PFx), Dorsiflexion (DFx), Absorption (Abs), Generation (Gen), Right heel strike (RHS), Left heel strike (LHS), Right toe off (RTO), Left toe off (LTO), Right heel stroke (RHS), Left heel stroke (LHS).
3.3. Kinetic Parameters
At the mMPA assessment, both ankle plantarflexion peak moments in the terminal stance decreased compared to those in the CPA (Figure 4A(f),B(f) solid arrow). Thus, ankle power did not increase (Figure 4A(i),B(i) solid arrow). However, the yMPA measurements increased in moment and power compared to those at mMPA and were similar to those with the CPA (Figure 4A(i),B(i) solid arrow).
3.4. Questionnaire
The MPA was better in balance, appearance, durability, and compatibility (Figure 5 (Q6, 9, 12, 13)) from a mechanical point of view not only for skin problems (Figure 5 (Q14–17)) but also for related pain and was rated better than the CPA, where pain was felt at the stump site and lower back (Figure 5 (Q18–21)). In addition, the gait with the MPA scored high in various walking environments (Figure 5 (Q22–33)). No difference was noted on the stairs or downhill in mMPA, but the yMPA showed high improvement.
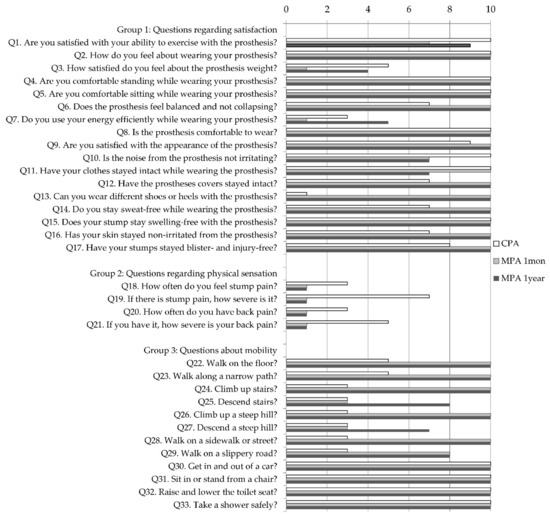
Figure 5.
Questionnaire regarding satisfaction and mobility after using CPA and MPA for 1 month and 1 year. It is referenced from the Korean version of the Prosthesis Evaluation Questionnaire (K-PEQ) and divided into three categories: satisfaction, physical sensation, and mobility. Each is scored 1–10 points; for Q1–17 and Q22–33 higher scores indicate higher satisfaction, and for Q18–21, lower scores indicate higher satisfaction.
For the open-ended questions, the participant wanted the battery to last longer and felt uncomfortable with some noise. However, the weight which we were concerned with did not matter much. Rather, he was satisfied that daily life had become much better than before and waswilling to continue wearing the MPA.
4. Discussion
The BTA usually encounters more disadvantages than unilateral amputees. According to Su PF et al. [26], compared to unilateral amputees, patients with BTA walk at slower speeds and lower cadences. They have reduced ankle dorsiflexion and knee flexion angle in peak-to-peak stance phase (loading response), reduced ankle plantar flexor peak moment, and reduced ankle power in late stance. Various prosthetic technologies have been introduced to support the absence of the ankle plantar flexor muscles and moment in particular. The newly-produced RoFT® MPA from South Korea is one of these.
As in the BTA patient described above, walking velocity and cadence were decreased for mMPA and yMPA when compared to a normal gait. The step length also decreased for mMPA, but increased somewhat on the right for yMPA. This is expected because of the weight. The MPA weighed 1750 g, which is more than 10 times heavier than the CPA (130 g). Thus the stress on the socket-residual limb interface increased. Gitter et al. assessed the addition of 1.34 kg of mass [27]. In that case, an increase of 5.4 J was required to accelerate the heavier prosthetic limb into the swing phase. The weight of the prosthetic leg is also important in terms of patient preference and gait efficiency [24]. In our yMPA assessment, there was an increase in step length. This seems to have improved with MPA adaptation. The increasing subjective satisfaction rating about weight also confirmed patient adaptation. Nevertheless, the weight disadvantage should be addressed in the future. This could improve the yield for various parameters.
For patients with BTA, an increase in step width usually occurs due to poor walking stability [26,28]. In this case, however, the step width measured for mMPA and yMPA decreased significantly, which meant increasing stability. Further, the answers on the mobility questions about stability on various terrain support this result.
When a prosthetic foot is worn, heel contact time is delayed, and an early heel rise occurs. This shortens the ground contact period, which in turn delays the toe-off of the opposite. Accordingly, the loading response phase (LRP) occupies close to 20% of the gait cycle with the CPA and 12% in normal patients without a prosthesis [29]. In contrast, the LRP for the mMPA and yMPA were close to normal. This is because the heel-only period was shortened. Ankle movement occurred before the shank moved forward due to increased plantarflexion within the initial stage of LRP on both sides. This made the time of the foot-to-ground contact shorter than with the CPA.
Under normal conditions, a plantarflexion moment would be generated, which corresponds to the dorsiflexion [29]. However, the right ankle plantarflexion moment during LRP was not sufficient with the CPA or MPA, although it stored energy during dorsiflexion. Neither the CPA nor the MPA generated as much plantarflexion power. Additionally, in unilateral amputation, the unaffected side provides sufficient stability, and there is sufficient time for toe-off to occur sequentially after heel rise. However, in BTA, the ankle moment and power are reduced as described above, because the time when MPA provides power for plantarflexion is shortened. Therefore, the shank movement is reduced, and the swing phase knee flexion angle is decreased, so that dorsiflexion is slightly extended. According to the results of the yMPA, which were higher than that of the mMPA, it seems encouraging to expect that more stable support time can secured in the future.
Compared to a normal gait, vertical movement is usually decreased in BTA [29]. Our patient also did not have much up and down movement in the center of mass. However, as the MPA adaptation time increased, the symmetry ratio improved to a balanced value (Table 1). In particular, the ankle plantarflexion power symmetry ratio showed significant improvement. The questionnaire answers regarding balance also yielded high marks for MPA, supporting this idea (Figure 5 (Q6)).
Today, various lower extremity prosthetic devices exist. Each device has a different design and function [30]. One of the relatively new and emerging types of prosthetics is one controlled by a microprocessor. The RoFT® MPA is one such prosthesis, with the ability to attain input information for the various environmental factors and make a strategic output of the device. Although RoFT® has the advantages described above as an MPA, it also needs to be compared with other MPAs. There are MPAs that have tried to reduce the weight, and there are MPAs with different designs, so comparison with other MPAs is important [31,32]. This study was meaningful in that MPA was applied to a BTA and followed for a long time; however, the study only followed on person. In a further study, it would be good to evaluate more patients and performance on a sloped terrain.
5. Conclusions
The new RoFT® MPA enabled our patient to walk in a more physiologic manner due to the increased single support time, symmetry ratio, and improvements in ankle kinematics. However, the decreased plantarflexion power produced less physiologic kinematics and kinetics, which was negative. The prosthetic weight and operating noise can be improved. Nevertheless, after 1 year of followup, significant increases in moment, power, and balance were observed. Because outdoor terrain is more diverse than indoors, gait training and living with various conditions are important. Our patient reported improved satisfaction when walking in varied terrain with more efficiency. This is encouraging for the MPA. These analyses and positive feedback should be helpful in continued MPA development and safe gait training in varied terrain for patients with BTA.
Author Contributions
Conceptualization, H.S.Y.; data curation, J.H.J. and P.-h.C.; formal analysis, J.H.J., H.S.Y., P.-h.C. and E.J.A.; investigation, E.J.A., W.S.S., D.Y.A. and J.Y.K.; resources, W.S.S., D.Y.A., J.Y.K., S.B.N.L., M.J. and M.H.C.; writing—original draft preparation, J.H.J.; writing—review and editing, H.S.Y. and P.-h.C.; visualization, P.-h.C.; supervision, H.S.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (Project Number: 1711135029, KMDF_PR_20200901_0158). The cost of the prostheses was carried by the patient and, thus, did not affect our results.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the Veterans Health Service Medical Center (2020-11-016-005).
Informed Consent Statement
Informed consent was obtained from the subject involved in the study. Written informed consent was obtained from the patient to publish this paper.
Data Availability Statement
Data will be made available on reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Braddom, R.L. Physical Medicine and Rehabilitation, 4th ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2010. [Google Scholar]
- Shinha, R.; Van Den Heuvel, W.J.A. A systematic literature review of quality of life in lower limb amputees. Disabil. Rehabil. 2011, 33, 883–899. [Google Scholar] [CrossRef] [PubMed]
- Dillingham, T.R.; Pezzin, L.E.; MacKenzie, E.J. Limb amputation and limb deficiency: Epidemiology and recent trends in the United States. South Med. J. 2002, 95, 875–884. [Google Scholar] [CrossRef] [PubMed]
- Varma, P.; Stineman, M.G.; Dilingham, T.R. Epidemiology of limb loss. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429. [Google Scholar] [CrossRef]
- Hughes, W.; Goodall, R.; Salciccioli, J.D.; Marshall, D.C.; Davies, A.H.; Shalhoub, J. Editor’s Choice—Trends in Lower Extremity Amputation Incidence in European Union 15+ Countries 1990-2017. Eur. J. Vasc. Endovasc. Surg. 2020, 60, 602–612. [Google Scholar] [CrossRef] [PubMed]
- Esquenazi, A.; DiGiacomo, R. Rehabiliattion after amputation. J. Am. Podiatr. Med. Assoc. 2001, 91, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Kanata, Y.; Ito, T.; Yoshida, T.; Koyama, T.; Mikami, Y.; Domen, K. Prosthetic walking after bilateral transfemoral amputation in a patient with dilated cardiomyopathy: A case report. Prosthet. Orthot. Int. 2022, 46, 195–198. [Google Scholar] [CrossRef]
- Mohanty, R.K.; Kumar, J.P.; Rout, S.; Das, S.P. Successful prosthetic rehabilitation and gait analysis of individual with bilateral transtibial amputation: A case study with comparison to able-bodied gait. J. Orthop. Trauma Rehabil. 2020, 27, 93–100. [Google Scholar] [CrossRef]
- Agrawal, V.; Gailey, R.S.; Gaunaurd, I.A.; O’Toole, C.; Finnieston, A.; Tolchin, R. Comparison of four different categories of prosthetic feet during ramp ambulation in unilateral transtibial amputees. Prosthet. Orthot. Int. 2015, 39, 380–390. [Google Scholar] [CrossRef]
- Vickers, D.R.; Palk, C.; McIntosh, A.S.; Beatty, K.T. Elderly unilateral transtibial amputee gait on an inclined walkway: A biomechanical analysis. Gait Posture 2008, 27, 518–529. [Google Scholar] [CrossRef]
- Ko, C.Y.; Shin, H.J.; Ryu, J.C.; Kim, K.S. State-of-the-art in microprocessor controlled prostheses for the lower limb amputees. J. Korean Soc. Prosthet. Orthot. 2016, 10, 1–8. [Google Scholar]
- Versluys, R.; Beyl, P.; Van Damme, M.; Desomer, A.; Van Ham, R.; Lefeber, D. Prosthetic feet: State-of-the-art review and the importance of mimicking human ankle–foot biomechanics. Disabil. Rehabil. Assist. Technol. 2009, 4, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Sagawa, Y., Jr.; Turcot, K.; Armand, S.; Thevenon, A.; Vuillerme, N.; Watelain, E. Biomechanics and physiological parame-ters during gait in lower-limb amputees: A systematic review. Gait Posture 2011, 33, 511–526. [Google Scholar] [CrossRef] [PubMed]
- Webster, J.B.; Murphy, D.P. Atlas of Orthoses and Assistive Devices, 5th ed.; Elsevier: Philadelphia, PA, USA, 2019; pp. 69–95. [Google Scholar]
- Agrawal, V.; Gailey, R.S.; Gaunaurd, I.A.; O’Toole, C.; Finnieston, A.A. Comparison between microprocessor-controlled ankle/foot and conventional prosthetic feet during stair negotiation in people with unilateral transtibial amputation. J. Rehabil. Res. Dev. 2013, 50, 941–950. [Google Scholar] [CrossRef]
- Sinitski, E.H.; Hansen, A.H.; Wilken, J.M. Biomechanics of the ankle–foot system during stair ambulation: Implications for design of advanced ankle–foot prostheses. J. Biomech. 2012, 45, 588–594. [Google Scholar] [CrossRef]
- Au, S.K.; Herr, H.; Weber, J.; Martinez-Villalpando, E.C. Powered ankle-foot prosthesis for the improvement of amputee ambulation. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 3020–3026. [Google Scholar]
- Ferris, A.E.; Aldridge, J.M.; Rábago, C.A.; Wilken, J.M. Evaluation of a powered ankle-foot prosthetic system during walking. Arch. Phys. Med. Rehabil. 2012, 93, 1911–1918. [Google Scholar] [CrossRef]
- Thomas-Pohl, M.; Villa, C.; Davot, J.; Bonnet, X.; Facione, J.; Lapeyre, E.; Bascou, J.; Pillet, H. Microprocessor prosthetic ankles: Comparative biomechanical evaluation of people with transtibial traumatic amputation during standing on level ground and slope. Disabil. Rehabil. Assist. Technol. 2021, 16, 17–26. [Google Scholar] [CrossRef]
- Hafner, B.J.; Willingham, L.L.; Buell, N.C.; Allyn, K.J.; Smith, D.G. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch. Phys. Med. Rehabil. 2007, 88, 207–217. [Google Scholar] [CrossRef]
- Collins, T.D.; Ghoussayni, S.N.; Ewins, D.J.; Kent, J.A. A six degrees-of-freedom marker set for gait analysis: Repeatability and comparison with a modified Helen Hayes set. Gait Posture 2009, 30, 173–180. [Google Scholar] [CrossRef]
- Park, S.H.; Yoon, S.H. Validity Evaluation of an Inertial Measurement Unit (IMU) in Gait Analysis Using Statistical Parametric Mapping (SPM). Sensors 2021, 21, 3667. [Google Scholar] [CrossRef]
- Lenzi, T.; Cempini, M.; Newkirk, J.; Hargrove, L.J.; Kuiken, T.A. A lightweight robotic ankle prosthesis with non-backdrivable cam-based transmission. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 1142–1147. [Google Scholar]
- Seong, W.S.; Kim, J.H.; Jung, D.H. Development and validity verification of Korean-Prosthesis Evaluation Questionnaire (KPEQ) for amputee’s use of prosthesis. J. Spec. Educ. Rehabil. Sci. 2017, 56, 293–330. [Google Scholar] [CrossRef]
- Su, P.; Gard, S.A.; Lipschutz, R.D.; Kuiken, T.A. Gait characteristics of persons with bilateral transtibial amputations. J. Rehabil. Res. Dev. 2007, 44, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Gitter, A.; Czerniecki, J.; Meinders, M. Effect of prosthetic mass on swing phase work during above knee amputee ambulation. Am. J. Phys. Med. Rehabil. 1997, 76, 114–121. [Google Scholar] [CrossRef]
- Sadeghi, H.; Allard, P.; Duhaime, P. Muscle power compensatory mechanisms in below-knee amputee gait. Am. J. Phys. Med. Rehabil. 2001, 80, 25–32. [Google Scholar] [CrossRef]
- Perry, J.; Burnfield, J.M. Gait Analysis: Normal and Pathological Function, 2nd ed.; Slack Incorporated: Pomona, CA, USA, 2010. [Google Scholar]
- Martin, J.; Pollock, A.; Hettinger, J. Microprocessor Lower Limb Prosthetics: Review of Current State of the Art. J. Prosthet. Orthot. 2010, 22, 183–193. [Google Scholar] [CrossRef]
- Xiu, H.; Han, Y.; Wang, X.; Zhang, Y.; Liang, W.; Wei, G.; Ren, L.; Ren, L. Design, development, and clinical validation of a two degrees of freedom compliant ankle-foot prosthesis based on a 4-4r parallel mechanism. Mech. Mach. Theory. 2022, 172, 104818. [Google Scholar] [CrossRef]
- Au, S.K.; Weber, J.; Herr, H. Biomechanical Design of a Powered Ankle-Foot Prosthesis. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 298–303. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).