Trends and Changes in Socio-Economic Inequality in Self-Rated Health among Migrants and Non-Migrants: Repeated Cross-Sectional Analysis of National Survey Data in Germany, 1995–2017
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Design, Sampling and Participants
2.3. Health Outcome
2.4. Socio-Economic Status
2.5. Analysis
3. Results
3.1. Descriptive Results
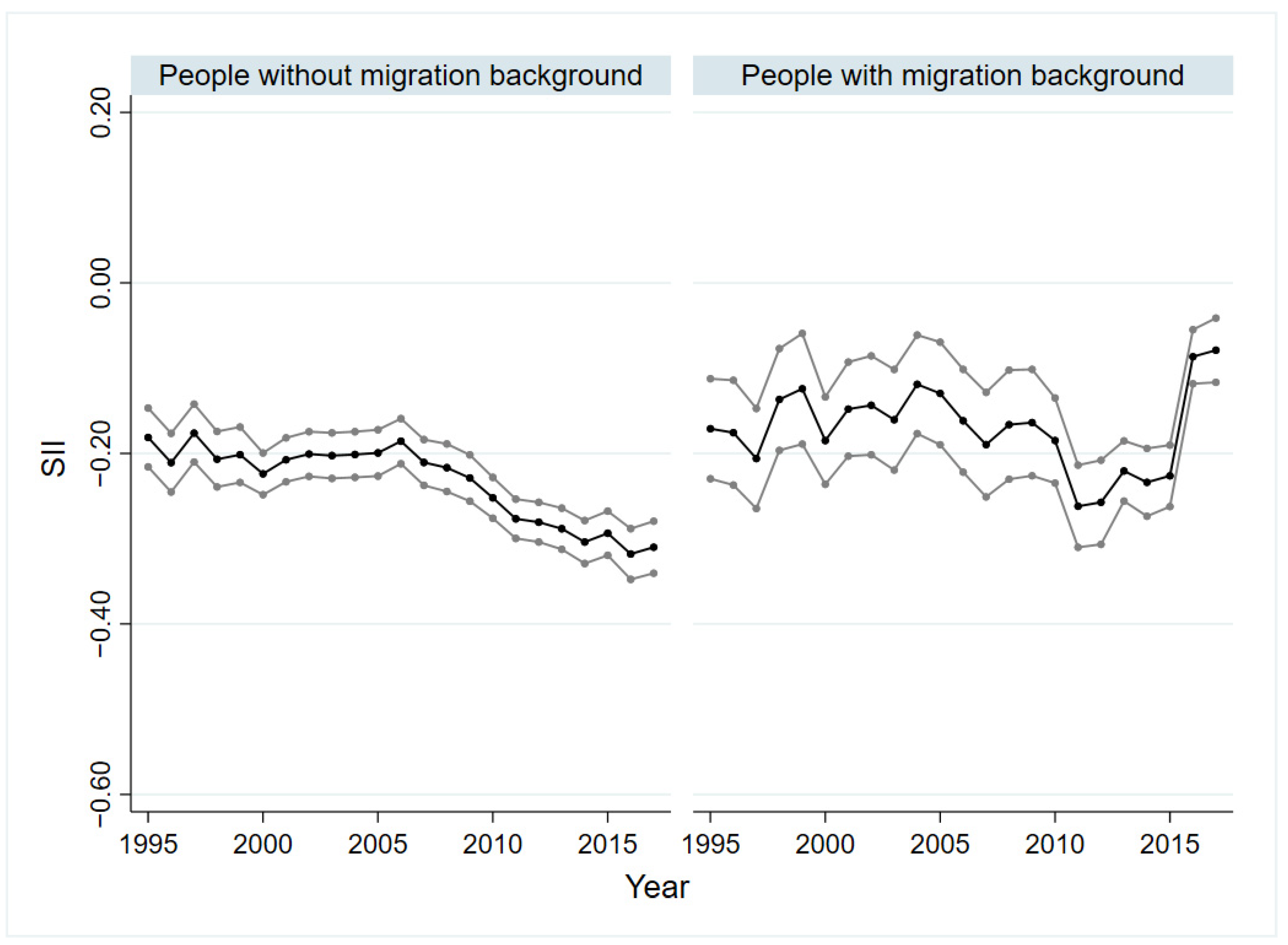
3.2. Socio-Economic Inequalities in SRH of People with and without Migration Background
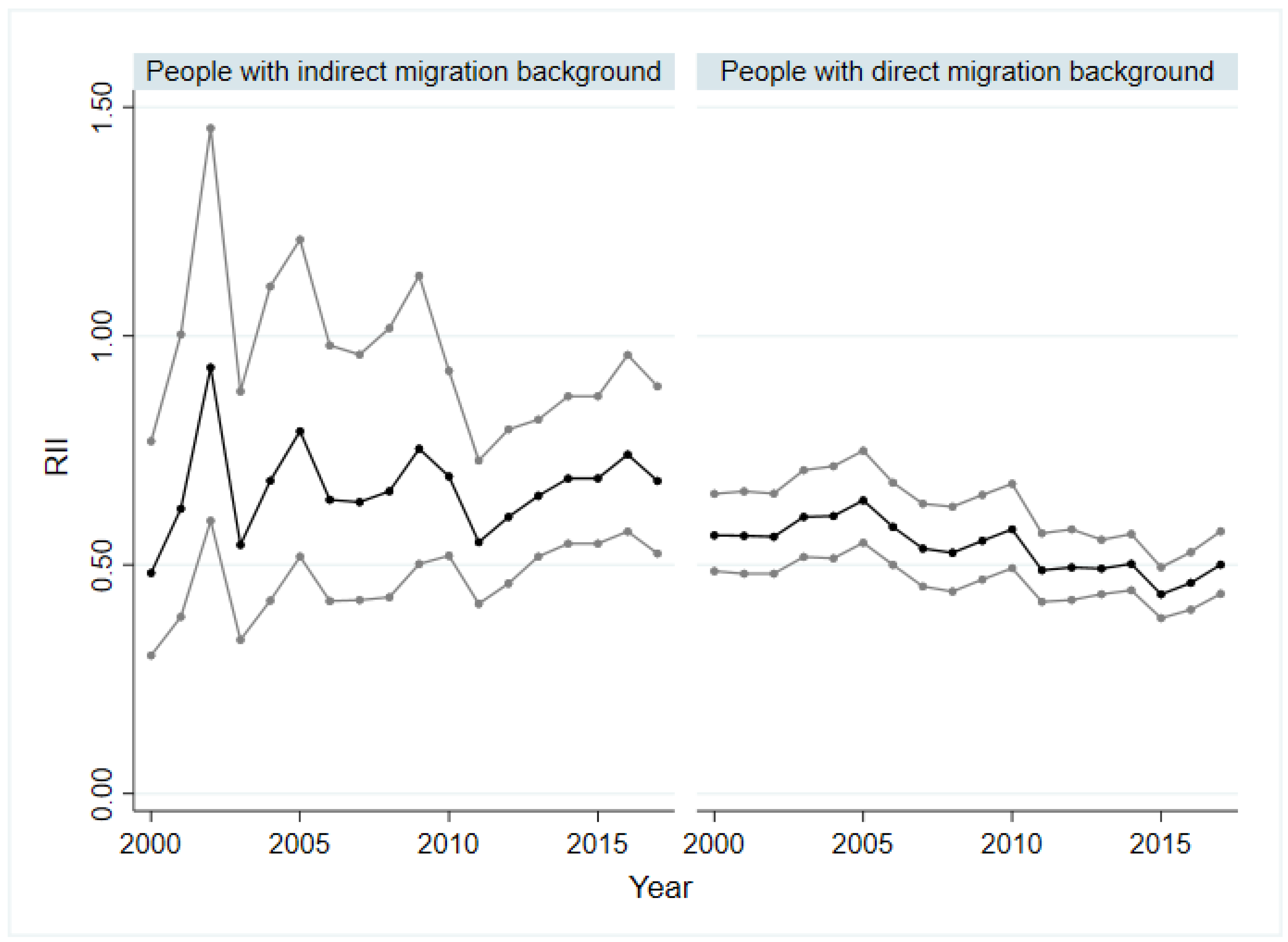
3.3. Socio-Economic Inequalities in SRH of People with Indirect and Direct Migration Background as Well as with Asylum and Refugee Background
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hosseinpoor, A.R.; Bergen, N.; Koller, T.; Prasad, A.; Schlotheuber, A.; Valentine, N.; Lynch, J.; Vega, J. Equity-Oriented Monitoring in the Context of Universal Health Coverage. PLOS Med. 2014, 11, e1001727. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpoor, A.R.; Bergen, N.; Schlotheuber, A. Promoting health equity: WHO health inequality monitoring at global and national levels. Glob. Health Action 2015, 8, 29034. [Google Scholar] [CrossRef] [PubMed]
- Health, C. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Hosseinpoor, A.R.; Bergen, N.; Schlotheuber, A.; Boerma, T. National health inequality monitoring: Current challenges and opportunities. Glob. Health Action 2018, 11, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Kunst, A.; Bos, V.; Mackenbach, J. Monitoring Socio-Economic Inequalities in Health in the European Union: Guidelines and Illustrations; Department of Public Health, Erasmus University Rotterdam: Rotterdam, The Netherlands, 2001. [Google Scholar]
- Bozorgmehr, K.; Biddle, L.; Rohleder, S.; Puthoopparambil, S.J.; Jahn, R. What Is the Evidence on Availability and Integration of Refugee and Migrant Health Data in Health Information Systems in the WHO European Region? World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Lampert, T.; Kroll, L.E.; Kuntz, B.; Hoebel, J. Health inequalities in Germany and in international comparison: Trends and developments over time. J. Health Monit. 2018, 3, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Kibele, E.U.B.; Jasilionis, D.; Shkolnikov, V.M. Widening socioeconomic differences in mortality among men aged 65 years and older in Germany. J. Epidemiol. Community Health 2013, 67, 453–457. [Google Scholar] [CrossRef] [Green Version]
- Hoebel, J.; Kuntz, B.; Kroll, L.E.; Schienkiewitz, A.; Finger, J.D.; Lange, C.; Lampert, T. Socioeconomic Inequalities in the Rise of Adult Obesity: A Time-Trend Analysis of National Examination Data from Germany, 1990–2011. Obes. Facts 2019, 12, 344–356. [Google Scholar] [CrossRef]
- Hoebel, J.; Kuntz, B.; Kroll, L.E.; Finger, J.D.; Zeiher, J.; Lange, C.; Lampert, T. Trends in Absolute and Relative Educational Inequalities in Adult Smoking Since the Early 2000s: The Case of Germany. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob. 2018, 20, 295–302. [Google Scholar] [CrossRef]
- Wachtler, B.; Hoebel, J.; Lampert, T. Trends in socioeconomic inequalities in self-rated health in Germany: A time-trend analysis of repeated cross-sectional health surveys between 2003 and 2012. BMJ Open 2019, 9, e030216. [Google Scholar] [CrossRef] [Green Version]
- Siegel, M.; Vogt, V.; Sundmacher, L. From a conservative to a liberal welfare state: Decomposing changes in income-related health inequalities in Germany, 1994–2011. Soc. Sci. Med. 2014, 108, 10–19. [Google Scholar] [CrossRef]
- Moor, I.; Günther, S.; Knöchelmann, A.; Hoebel, J.; Pförtner, T.-K.; Lampert, T.; Richter, M. Educational inequalities in subjective health in Germany from 1994 to 2014: A trend analysis using the German Socio-Economic Panel study (GSOEP). BMJ Open 2018, 8, e019755. [Google Scholar] [CrossRef]
- Schupp, J. Das Sozio-oekonomische Panel (SOEP). Bundesgesundheitsbl. Gesundh. Gesundh. 2012, 55, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Brücker, H.; Kroh, M.; Bartsch, S.; Goebel, J.; Kühne, S.; Liebau, E.; Trübswetter, P.; Tucci, I.; Schupp, J. The New IAB-SOEP Migration Sample: An Introduction into the Methodology and the Contents; Deutsches Institut für Wirtschaftsforschung (DIW): Berlin, Germany, 2014. [Google Scholar]
- Brücker, H.; Rother, N.; Schupp, J. IAB-BAMF-SOEP-Befragung von Geflüchteten 2016: Studiendesign, Feldergebnisse sowie Analysen zu Schulischer wie Beruflicher Qualifikation, Sprachkenntnissen sowie Kognitiven Potenzialen. Forschungsbericht 30; Bundesamt für Migration und Flüchtlinge: Nürnberg, Germany, 2017. [Google Scholar]
- Destatis, S.B. Bevölkerung und Erwerbstätigkeit. Bevölkerung mit Migrationshintergrund Ergebnisse des Mikrozensus 2018; Statistisches Bundesamt: Wiesbaden, Germany, 2019. [Google Scholar]
- Moor, I.; Spallek, J.; Richter, M. Explaining socioeconomic inequalities in self-rated health: A systematic review of the relative contribution of material, psychosocial and behavioural factors. J. Epidemiol. Community Health 2017, 71, 565–575. [Google Scholar] [CrossRef] [PubMed]
- Miething, A. A matter of perception: Exploring the role of income satisfaction in the income-mortality relationship in German survey data 1995–2010. Soc. Sci. Med. 2013, 99, 72–79. [Google Scholar] [CrossRef]
- Lampert, T.; Kroll, L.; Müters, S.; Stolzenberg, H. Messung des sozioökonomischen Status in der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsbl. Gesundh. Gesundh. 2013, 56, 631–636. [Google Scholar] [CrossRef] [Green Version]
- Group, S. SOEP-Core v34. PGEN: Person-Related Status and Generated Variables; DIW Berlin/SOEP: Berlin, Germany, 2019. [Google Scholar]
- Ganzeboom, H.B.G.; De Graaf, P.M.; Treiman, D.J. A standard international socio-economic index of occupational status. Soc. Sci. Res. 1992, 21, 1–56. [Google Scholar] [CrossRef] [Green Version]
- OECD. OECD Framework for Statistics on the Distribution of Household Income, Consumption and Wealth; OECD: Paris, French, 2013. [Google Scholar]
- Regidor, E. Measures of health inequalities: Part 2. J. Epidemiol. Community Health 2004, 58, 900–903. [Google Scholar] [CrossRef] [PubMed]
- Barros, A.J.D.; Hirakata, V.N. Alternatives for logistic regression in cross-sectional studies: An empirical comparison of models that directly estimate the prevalence ratio. BMC Med. Res. Methodol. 2003, 3, 21. [Google Scholar] [CrossRef] [Green Version]
- Khang, Y.-H.; Yun, S.-C.; Lynch, J.W. Monitoring trends in socioeconomic health inequalities: It matters how you measure. BMC Public Health 2008, 8, 66. [Google Scholar] [CrossRef] [Green Version]
- Ernstsen, L.; Strand, B.H.; Nilsen, S.M.; Espnes, G.A.; Krokstad, S. Trends in absolute and relative educational inequalities in four modifiable ischaemic heart disease risk factors: Repeated cross-sectional surveys from the Nord-Trøndelag Health Study (HUNT) 1984–2008. BMC Public Health 2012, 12, 266. [Google Scholar] [CrossRef] [Green Version]
- Kroll, L.E.; Lampert, T. Changing health inequalities in Germany from 1994 to 2008 between employed and unemployed adults. Int. J. Public Health 2011, 56, 329–339. [Google Scholar] [CrossRef] [Green Version]
- Bozorgmehr, K.; Schneider, C.; Joos, S. Equity in access to health care among asylum seekers in Germany: Evidence from an exploratory population-based cross-sectional study. BMC Health Serv. Res. 2015, 15, 502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, D.; Biddle, L.; Mühling, C.; Bozorgmehr, K. Subjective social status mobility and mental health of asylum seekers and refugees: Population-based, cross-sectional study in a German federal state. J. Migr. Health 2020, 1–2, 100020. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.S.; Hempler, N.F.; Krasnik, A. Issues to consider when measuring and applying socioeconomic position quantitatively in immigrant health research. Int. J. Environ. Res. Public Health 2013, 10, 6354–6365. [Google Scholar] [CrossRef] [PubMed]
- Regidor, E. Measures of health inequalities: Part 1. J. Epidemiol. Community Health 2004, 58, 858–861. [Google Scholar] [CrossRef] [PubMed]


| Year | 1995 | 2000 | 2005 | 2010 | 2015 | Total, 1995–2017 |
|---|---|---|---|---|---|---|
| Sex,n(%) | ||||||
| Male | 6527 (48.2) | 11,608 (48) | 8980 (47.51) | 11,512 (45.54) | 11,936 (45.85) | 231,857 (46.85) |
| Female | 7015 (51.8) | 12,574 (52) | 9923 (52.49) | 13,765 (54.46) | 14,096 (54.15) | 259,997 (53.15) |
| Age,n(%) | ||||||
| 18–39 years | 6396 (47.23) | 9604 (39.72) | 6685 (35.36) | 9874 (39.06) | 9184 (35.28) | 183,905 (38.68) |
| 40–65 years | 5581 (41.21) | 10,919 (45.16) | 8579 (45.38) | 11,152 (44.12) | 12,203 (46.88) | 223,314 (44.87) |
| >65 years | 1565 (11.56) | 3657 (15.12) | 3639 (19.25) | 4251 (16.82) | 4642 (17.83) | 84,616 (16.45) |
| Migration background,n(%) | ||||||
| Individuals without migration background | 10,147 (74.93) | 19,985 (82.64) | 15,784 (83.50) | 20,855 (82.51) | 18,226 (70.01) | 383,017 (78.75) |
| Individuals with migration background | 3395 (25.07) | 4197 (17.36) | 3119 (16.50) | 4422 (17.49) | 7807 (29.99) | 108,842 (21.25) |
| Migrant status,n(%) | ||||||
| Indirect migration background | 459 (13.99) | 778 (19.41) | 739 (24.26) | 1244 (28.41) | 1835 (23.68) | 23,635 (22.51) |
| Direct migration background | 2744 (83.66) | 3099 (77.32) | 2180 (71.57) | 2792 (63.77) | 5251 (67.77) | 67,711 (71.53) |
| Asylum seeker and refugee | 77 (2.35) | 131 (3.27) | 127 (4.17) | 342 (7.81) | 662 (8.54) | 15,587 (5.96) |
| SES,n(%) | ||||||
| Low | 4059 (30.52) | 6275 (26.52) | 3585 (19.89) | 4940 (20.45) | 4011 (16.18) | 100,418 (22.00) |
| Moderate | 7960 (59.85) | 14,435 (61.00) | 11,455 (63.54) | 14,623 (60.52) | 15,025 (60.63) | 286,499 (61.09) |
| High | 1281 (9.63) | 2953 (12.48) | 2987 (16.57) | 4598 (19.03) | 5747 (23.19) | 82,434 (16.90) |
| Educational level, n (%) | ||||||
| Low | 3117 (23.39) | 4320 (18.18) | 2844 (15.63) | 3287 (13.46) | 3696 (14.85) | 80,405 (16.50) |
| Moderate | 7452 (55.92) | 13,758 (57.91) | 10,571 (58.09) | 13,545 (55.45) | 12,730 (51.13) | 259,371 (55.50) |
| High | 2757 (20.69) | 5679 (23.90) | 4784 (26.29) | 7597 (31.10) | 8469 (34.02) | 133,688 (28.00) |
| Income | ||||||
| Mean | 1122.07 | 1283.20 | 1429.05 | 1487.13 | 1668.97 | 1455.00 |
| Standard deviation | 606.92 | 647.52 | 780.73 | 860.25 | 938.27 | 858.00 |
| Occupational level, n (%) | ||||||
| No occupation | 2529 (18.71) | 6871 (28.52) | 3755 (20.06) | 6377 (25.52) | 5455 (21.06) | 114,520 (23.31) |
| Low | 6225 (46.06) | 8831 (36.66) | 7399 (39.54) | 8825 (35.32) | 9954 (38.43) | 184,796 (38.46) |
| Moderate | 3558 (26.32) | 5962 (24.75) | 5342 (28.54) | 6607 (26.44) | 7006 (27.05) | 130,198 (26.56) |
| High | 1204 (8.91) | 2424 (10.06) | 2219 (11.86) | 3178 (12.72) | 3488 (13.47) | 57,956 (11.67) |
| SRH, n (%) | ||||||
| Poor | 6862 (50.83) | 12,312 (51.00) | 9037 (47.98) | 13,165 (52.13) | 13,315 (51.22) | 244,509 (50.77) |
| Good | 6638 (49.17) | 11,829 (49.00) | 9799 (52.02) | 12,088 (47.87) | 12,679 (48.78) | 239,975 (49.23) |
| Total n | 19,947 | 34,302 | 30,339 | 45,977 | 26,108 | 849,190 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wulkotte, E.; Bozorgmehr, K. Trends and Changes in Socio-Economic Inequality in Self-Rated Health among Migrants and Non-Migrants: Repeated Cross-Sectional Analysis of National Survey Data in Germany, 1995–2017. Int. J. Environ. Res. Public Health 2022, 19, 8304. https://doi.org/10.3390/ijerph19148304
Wulkotte E, Bozorgmehr K. Trends and Changes in Socio-Economic Inequality in Self-Rated Health among Migrants and Non-Migrants: Repeated Cross-Sectional Analysis of National Survey Data in Germany, 1995–2017. International Journal of Environmental Research and Public Health. 2022; 19(14):8304. https://doi.org/10.3390/ijerph19148304
Chicago/Turabian StyleWulkotte, Elisa, and Kayvan Bozorgmehr. 2022. "Trends and Changes in Socio-Economic Inequality in Self-Rated Health among Migrants and Non-Migrants: Repeated Cross-Sectional Analysis of National Survey Data in Germany, 1995–2017" International Journal of Environmental Research and Public Health 19, no. 14: 8304. https://doi.org/10.3390/ijerph19148304
APA StyleWulkotte, E., & Bozorgmehr, K. (2022). Trends and Changes in Socio-Economic Inequality in Self-Rated Health among Migrants and Non-Migrants: Repeated Cross-Sectional Analysis of National Survey Data in Germany, 1995–2017. International Journal of Environmental Research and Public Health, 19(14), 8304. https://doi.org/10.3390/ijerph19148304






