Effects of a Two-Step Cognitive and Relaxation Training Program in Care Home Residents with Mild Cognitive Impairment
Abstract
1. Introduction
2. Materials and Methods
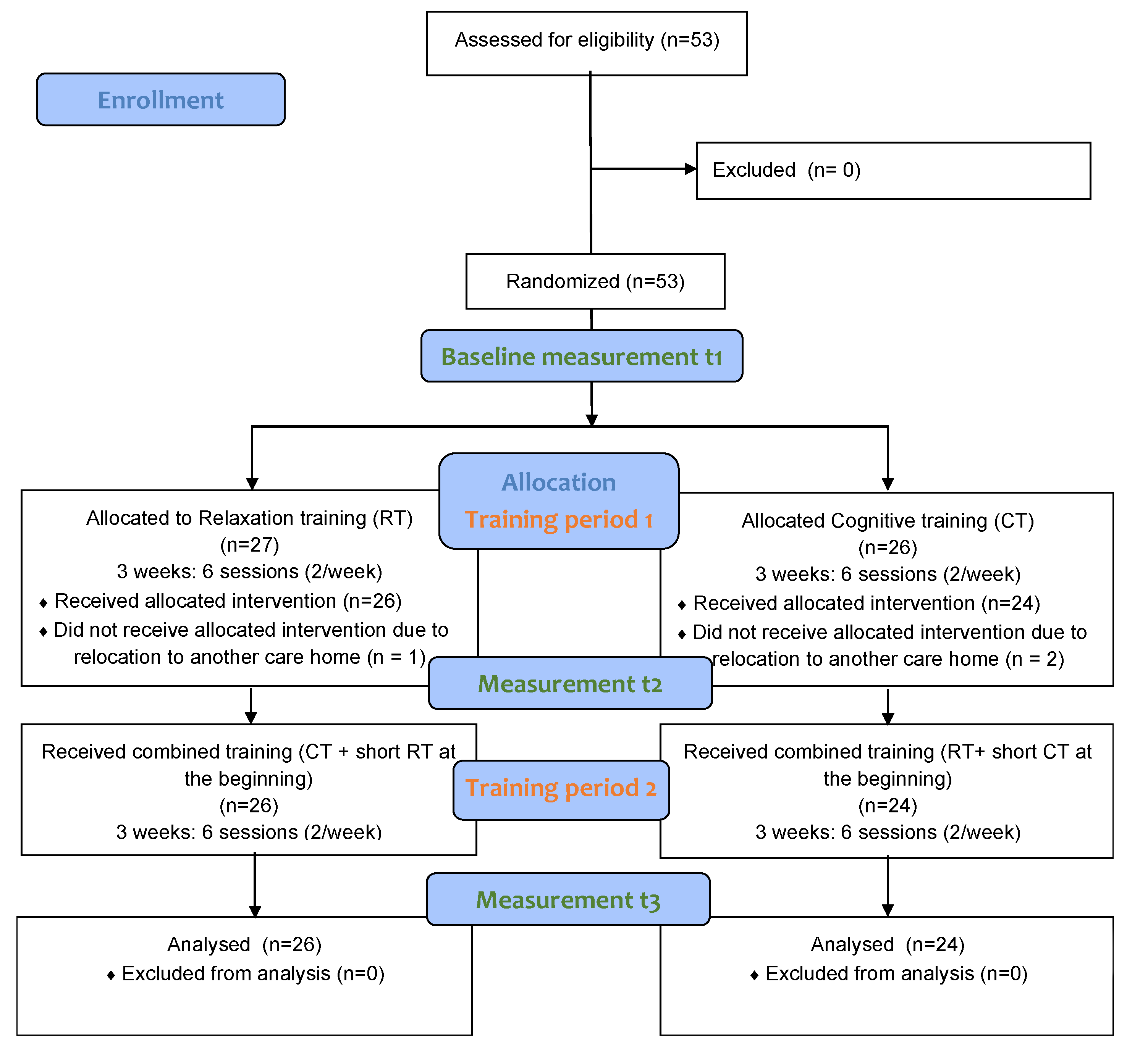
2.1. Design and Procedure
2.2. Participants
2.3. Intervention
2.3.1. Relaxation Training (RT)
2.3.2. Cognitive Training (CT)
2.3.3. Combined Training
2.4. Measurements
2.4.1. Sociodemographic Data
2.4.2. Assessment of Effectiveness on Cognitive and Emotional Status
- (a)
- Mini-Mental State Examination (MMSE)
- (b)
- Age-Concentration-Test (ACT)
- (c)
- Clinical Self-Rating Scale (CSRS-AMS)
- (d)
- Geriatric Depression Scale-Short Form (GDS-SF)
- (e)
- Visual Analog Scale (VAS) for the Measurement of Experience of Pain
2.4.3. Assessment of Acceptability
2.5. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Data
3.2. Efficacy of Training Programs
3.2.1. Cognitive Status
3.2.2. Emotional Status
3.2.3. Experience of Pain
3.3. Acceptability
4. Discussion
4.1. Cognitive Status
4.2. Emotional Status
4.3. Experience of Pain
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Petersen, R.C.; Roberts, R.O.; Knopman, D.S.; Boeve, B.F.; Geda, Y.E.; Ivnik, R.J.; Smith, G.E.; Jack, C.R. Mild cognitive impairment: Ten years later. Arch. Neurol. 2009, 66, 1447–1455. [Google Scholar] [CrossRef] [PubMed]
- Ganguli, M.; Chang, C.-C.H.; Snitz, B.E.; Saxton, J.A.; Vanderbilt, J.; Lee, C.-W. Prevalence of mild cognitive impairment by multiple classifications: The Monongahela-Youghiogheny Healthy Aging Team (MYHAT) project. Am. J. Geriatr. Psychiatry 2010, 18, 674–683. [Google Scholar] [CrossRef]
- Petersen, R.C.; Doody, R.; Kurz, A.; Mohs, R.C.; Morris, J.C.; Rabins, P.V.; Ritchie, K.; Rossor, M.; Thal, L.; Winblad, B. Current concepts in mild cognitive impairment. Arch. Neurol. 2001, 58, 1985–1992. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.A.; Hall, J.R.; O’Bryant, S.E. A depressive endophenotype of mild cognitive impairment and Alzheimer’s disease. PLoS ONE 2013, 8, e68848. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, R.; Liberman, D.; Rosenberg, J.; Alston, J.; Straus, S. Preventing cognitive decline in healthy older adults. CMAJ 2013, 185, 881–885. [Google Scholar] [CrossRef]
- Sanford, A.M. Mild Cognitive Impairment. Clin. Geriatr Med. 2017, 33, 325–337. [Google Scholar] [CrossRef]
- Li, H.; Li, J.; Li, N.; Li, B.; Wang, P.; Zhou, T. Cognitive intervention for persons with mild cognitive impairment: A meta-analysis. Ageing Res. Rev. 2011, 10, 285–296. [Google Scholar] [CrossRef]
- Hall, C.B.; Lipton, R.B.; Sliwinski, M.; Katz, M.J.; Derby, C.A.; Verghese, J. Cognitive activities delay onset of memory decline in persons who develop dementia. Neurology 2009, 73, 356–361. [Google Scholar] [CrossRef]
- Grawe, K.; Donati, R.; Bernauer, F. Psychotherapie im Wandel: Von der Konfession zur Profession, 5th ed.; Hogrefe: Göttingen, Germany, 2001. [Google Scholar]
- Hirsch, R.D.; Hespos, M.A. Autogenes Training bis ins hohe Alter: Basistherapeutikum und Gesundheitsförderung; mit 9 Tabellen; Reinhardts Gerontologische Reihe, Reinhardt: Munich, Germany, 2000. [Google Scholar]
- Kircher, T.; Stetter, F.; Wormstall, H. Der Einsatz von supportivem autogenem Training bei multimorbiden, gerontopsychiatrischen Patienten. Z. Gerontol. Geriatr. 1997, 30, 348–353. [Google Scholar]
- Gatterer, G. Effizienz spezifischer neuropsychologischer und klinisch-psychologischer Interventionen im Alter. Z. Gerontol. Geriatr. 2007, 40, 88–95. [Google Scholar] [CrossRef]
- Lupien, S.J.; McEwen, B.S.; Gunnar, M.R.; Heim, C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat. Rev. Neurosci. 2009, 10, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Brosschot, J.F.; Gerin, W.; Thayer, J.F. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. J. Psychosom. Res. 2006, 60, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Korten, N.C.M.; Comijs, H.C.; Penninx, B.W.J.H.; Deeg, D.J.H. Perceived stress and cognitive function in older adults: Which aspect of perceived stress is important? Int. J. Geriatr. Psychiatry 2017, 32, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Ihle, A.; Oris, M.; Sauter, J.; Rimmele, U.; Kliegel, M. Cognitive Reserve and Social Capital Accrued in Early and Midlife Moderate the Relation of Psychological Stress to Cognitive Performance in Old Age. Dement. Geriatr. Cogn. Disord. 2018, 45, 190–197. [Google Scholar] [CrossRef] [PubMed]
- McHugh Power, J.; Tang, J.; Lawlor, B.; Kenny, R.A.; Kee, F. Mediators of the relationship between social activities and cognitive function among older Irish adults: Results from the Irish longitudinal study on ageing. Aging Ment. Health 2018, 22, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Sandi, C. Stress and cognition. Wiley Interdiscip. Rev. Cogn. Sci. 2013, 4, 245–261. [Google Scholar] [CrossRef]
- Huntley, J.D.; Gould, R.L.; Liu, K.; Smith, M.; Howard, R.J. Do cognitive interventions improve general cognition in dementia? A meta-analysis and meta-regression. BMJ Open 2015, 5, e005247. [Google Scholar] [CrossRef]
- Jacobson, E. Progressive Relaxation. Am. J. Psychol. 1987, 100, 522. [Google Scholar] [CrossRef]
- Petermann, U.; Pätel, J. Entspannungsverfahren. In Lehrbuch der Verhaltenstherapie; Schneider, S., Margraf, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 243–254. [Google Scholar]
- Suhr, J. Progressive Muscle Relaxation in the Management of Behavioural Disturbance in Alzheimer’s Disease. Neuropsychol. Rehabil. 1999, 9, 31–44. [Google Scholar] [CrossRef]
- Ikemata, S.; Momose, Y. Effects of a progressive muscle relaxation intervention on dementia symptoms, activities of daily living, and immune function in group home residents with dementia in Japan. Jpn. J. Nurs. Sci. 2017, 14, 135–145. [Google Scholar] [CrossRef]
- Mammarella, N.; Fairfield, B.; Cornoldi, C. Does music enhance cognitive performance in healthy older adults? The Vivaldi effect. Aging Clin. Exp. Res. 2007, 19, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Särkämö, T.; Tervaniemi, M.; Laitinen, S.; Forsblom, A.; Soinila, S.; Mikkonen, M.; Autti, T.; Silvennoinen, H.M.; Erkkilä, J.; Laine, M.; et al. Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain 2008, 131, 866–876. [Google Scholar] [CrossRef] [PubMed]
- Ziv, N.; Rotem, T.; Arnon, Z.; Haimov, I. The effect of music relaxation versus progressive muscular relaxation on insomnia in older people and their relationship to personality traits. J. Music 2008, 45, 360–380. [Google Scholar] [CrossRef]
- Bernstein, D.A.; Borkovec, T.D.; Ullmann, L.P.; Höfler, R.; Kattenbeck, M.; Oeke, M.; Heyse, H. Entspannungstraining: Handbuch der Progressiven Muskelentspannung nach Jacobson, 14th ed.; Klett-Cotta: Stuttgart, Germany, 2013; Volume 16, 199p, ISBN 9783608892505. [Google Scholar]
- Lehner, B.; Eich, F.X. Neuropsychologisches Funktionstrainung Für Hirnverletzte Patienten (NFT): Therapiemanual zur Förderung Kognitiver Funktionen. Materialien Für die Psychosoziale Praxis; Psychologie-Verl.-Union: Munich, Germany, 1990. [Google Scholar]
- Oppolzer, U. Hirntraining mit ganzheitlichem Ansatz: Grundlagen, Anregungen und Trainingsmaterial für Gruppenleiter und Dozenten; Borgmann: Dortmund, Germany, 1998. [Google Scholar]
- Rigling, P. Hirnleistungstraining: Übungen zur Verbesserung der Konzentrationsfähigkeit, 7th ed.; Verl. Modernes Lernen: Dortmund, Germany, 2002. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Gatterer, G.; Fischer, P.; Simanyi, M.; Danielczyk, W. The A-K-T (“Alters-Konzentrations-Test”) a new psychometric test for geriatric patients. Funct. Neurol. 1989, 4, 273–276. [Google Scholar]
- Von Zerssen, D. Clinical Self-Rating Scales (CSRS) of the Munich Psychiatric Information System (PSYCHIS München). In Assessment of Depression; Sartorius, N., Ban, T.A., Eds.; Springer: Berlin/Heidelberg, Germany, 1986; pp. 270–303. [Google Scholar]
- Von Zerssen, D.; Petermann, F. Bf-SR: Die Befindlichkeits-Skala; Manual; Hogrefe: Göttingen, Germany, 2011. [Google Scholar]
- Yesavage, J.A.; Sheikh, J.I. 9/Geriatric Depression Scale (GDS). Clin. Gerontol. 1986, 5, 165–173. [Google Scholar] [CrossRef]
- Schomacher, J. Gütekriterien der visuellen Analogskala zur Schmerzbewertung. Physioscience 2008, 4, 125–133. [Google Scholar] [CrossRef]
- Schloffer, H.; Prang, E.; Frick-Salzmann, A. Gedächtnistraining; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Gatz, M. Educating the brain to avoid dementia: Can mental exercise prevent Alzheimer disease? PLoS Med. 2005, 2, e7. [Google Scholar] [CrossRef]
- Golombek, U. Progressive Muskelentspannung nach Jacobson in einer psychiatrisch-psychotherapeutischen Abteilung—empirische Ergebnisse. Psychiatr Prax. 2001, 28, 402–404. [Google Scholar] [CrossRef]
- Ruthirakuhan, M.; Luedke, A.C.; Tam, A.; Goel, A.; Kurji, A.; Garcia, A. Use of physical and intellectual activities and socialization in the management of cognitive decline of aging and in dementia: A review. J. Aging Res. 2012, 2012, 384875. [Google Scholar] [CrossRef]
- Singh, V.P.; Rao, V.; Prem, V.; Sahoo, R.C.; Keshav Pai, K. Comparison of the effectiveness of music and progressive muscle relaxation for anxiety in COPD—A randomized controlled pilot study. Chron. Respir. Dis. 2009, 6, 209–216. [Google Scholar] [CrossRef] [PubMed]
| Variable | RT | CT |
|---|---|---|
| Participants (%) | 26 (52%) | 24 (48%) |
| Age: M ± SD | 87 ± 7 | 87 ± 5 |
| Number of female/male | 25/1 | 24/0 |
| Education level | % | % |
| Primary school | 38 | 25 |
| Apprenticeship | 35 | 17 |
| University-entry diploma | 19 | 41 |
| University degree | 8 | 17 |
| Family Status | % | % |
| Single | 31 | 21 |
| Married or in a Partnership | 8 | 17 |
| Widowed | 61 | 62 |
| Level of care | % | % |
| Level 1–4 (no permanent care needed) | 65 | 75 |
| Level 5–7 (increased & permanent care needed) | 35 | 25 |
| Medication Status | % | % |
| psychotropic medication | 11 | 8 |
| medication for physical illness | 58 | 67 |
| combined psychotropic- & medication for physical illness | 23 | 17 |
| no medication | 8 | 8 |
| Descriptives M (SD) | Inferential | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| t1 | t2 | t3 | p-Value | Partial η2 | ||||||||
| Variables | M | SD | M | SD | M | SD | Group | Time | Inter-Action | Group | Time | Inter-Action |
| Cognitive Status | ||||||||||||
| Mini-Mental State Examination (MMSE) | ||||||||||||
| MMSE total score | 0.261 | <0.001 | 0.099 | 0.03 | 0.28 | 0.05 | ||||||
| RT | 24.8 | (3.5) | 26.4 | (3.0) | 26.8 | (2.2) | ||||||
| CT | 26.3 | (2.7) | 26.9 | (2.8) | 27.4 | (2.3) | ||||||
| MMSE orientation | 0.252 | 0.008 | 0.786 | 0.03 | 0.10 | 0.01 | ||||||
| RT | 9.1 | (1.2) | 9.4 | (0.8) | 9.7 | (0.6) | ||||||
| CT | 8.9 | (1.0) | 9.3 | (1.1) | 9.3 | (0.8) | ||||||
| MMSE registration | 0.701 | 0.781 | 0.349 | <0.01 | <0.01 | 0.02 | ||||||
| RT | 3.0 | (0.5) | 3.0 | (0.2) | 3.0 | (0.0) | ||||||
| CT | 3.0 | (0.2) | 3.0 | (0.0) | 3.0 | (0.0) | ||||||
| MMSE attention and calculation | 0.045 | 0.006 | 0.038 | 0.08 | 0.10 | 0.07 | ||||||
| RT | 3.6 | (1.6) | 4.1 | (1.0) | 4.4 | (0.8) | ||||||
| CT | 4.5 | (0.8) | 4.5 | (1.1) | 4.7 | (0.7) | ||||||
| MMSE recall | 0.359 | 0.002 | 0.238 | 0.02 | 0.12 | 0.03 | ||||||
| RT | 1.5 | (1.2) | 2.1 | (1.7) | 2.0 | (0.9) | ||||||
| CT | 1.8 | (1.0) | 2.0 | (0.9) | 2.4 | (0.7) | ||||||
| MMSE language | 0.262 | 0.345 | 0.695 | 0.03 | 0.02 | 0.01 | ||||||
| RT | 7.5 | (1.0) | 7.8 | (1.3) | 7.9 | (0.8) | ||||||
| CT | 7.9 | (1.1) | 7.9 | (1.0) | 8.0 | (1.0) | ||||||
| Age-Concentration-Test (ACT) | ||||||||||||
| ACT overall score | 0.143 | 0.108 | 0.717 | 0.04 | 0.05 | <0.01 | ||||||
| RT | 3.8 | (0.4) | 3.9 | (0.1) | 3.9 | (0.1) | ||||||
| CT | 3.9 | (0.2) | 4.0 | (0.1) | 4.0 | (0.9) | ||||||
| ACT work pace | 0.370 | <0.001 | 0.026 | 0.02 | 0.19 | 0.08 | ||||||
| RT | 4.6 | (0.8) | 4.5 | (0.7) | 4.4 | (0.7) | ||||||
| CT | 4.5 | (0.6) | 4.5 | (0.6) | 4.2 | (0.6) | ||||||
| ACT correct answer | 0.662 | 0.153 | 0.211 | <0.01 | 0.04 | 0.03 | ||||||
| RT | 2.8 | (0.2) | 2.9 | (0.1) | 2.9 | (0.2) | ||||||
| CT | 2.8 | (0.3) | 2.9 | (0.2) | 2.9 | (0.2) | ||||||
| ACT percentage of mistakes | 0.155 | 0.024 | 0.765 | 0.04 | 0.08 | 0.01 | ||||||
| RT | 2.6 | (1.0) | 2.8 | (0.7) | 2.8 | (0.6) | ||||||
| CT | 2.6 | (0.8) | 2.1 | (0.5) | 2.3 | (0.9) | ||||||
| Emotional Status | ||||||||||||
| Clinical Self-Rating Scale (CSRS-AMS) | 0.613 | <0.001 | 0.376 | 0.01 | 0.30 | 0.02 | ||||||
| RT | 14.7 | (9.7) | 11.0 | (7.8) | 8.7 | (6.9) | ||||||
| CT | 12.5 | (7.6) | 10.9 | (5.5) | 8.2 | (5.4) | ||||||
| Geriatric Depression Scale—Short Form (GDS-SF) | 0.801 | <0.001 | 0.325 | <0.01 | 0.28 | 0.02 | ||||||
| RT | 3.1 | (3.0) | 1.9 | (2.4) | 1.4 | (1.5) | ||||||
| CT | 2.8 | (2.1) | 2.3 | (1.6) | 1.6 | (1.6) | ||||||
| Experience of Pain | ||||||||||||
| Visual Analog Scale (VAS) Measurement of Pain | 0.542 | 0.019 | 0.681 | 0.01 | 0.08 | 0.01 | ||||||
| RT | 2.8 | (3.1) | 2.9 | (3.2) | 2.2 | (2.6) | ||||||
| CT | 3.6 | (3.0) | 3.2 | (2.6) | 2.3 | (2.2) | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stuerz, K.; Hartmann, S.; Holzner, B.; Bichler, C.S.; Niedermeier, M.; Kopp, M.; Guenther, V. Effects of a Two-Step Cognitive and Relaxation Training Program in Care Home Residents with Mild Cognitive Impairment. Int. J. Environ. Res. Public Health 2022, 19, 8316. https://doi.org/10.3390/ijerph19148316
Stuerz K, Hartmann S, Holzner B, Bichler CS, Niedermeier M, Kopp M, Guenther V. Effects of a Two-Step Cognitive and Relaxation Training Program in Care Home Residents with Mild Cognitive Impairment. International Journal of Environmental Research and Public Health. 2022; 19(14):8316. https://doi.org/10.3390/ijerph19148316
Chicago/Turabian StyleStuerz, Kristina, Sabine Hartmann, Bernhard Holzner, Carina S. Bichler, Martin Niedermeier, Martin Kopp, and Verena Guenther. 2022. "Effects of a Two-Step Cognitive and Relaxation Training Program in Care Home Residents with Mild Cognitive Impairment" International Journal of Environmental Research and Public Health 19, no. 14: 8316. https://doi.org/10.3390/ijerph19148316
APA StyleStuerz, K., Hartmann, S., Holzner, B., Bichler, C. S., Niedermeier, M., Kopp, M., & Guenther, V. (2022). Effects of a Two-Step Cognitive and Relaxation Training Program in Care Home Residents with Mild Cognitive Impairment. International Journal of Environmental Research and Public Health, 19(14), 8316. https://doi.org/10.3390/ijerph19148316






