Adapting PCIT-Health for Telehealth Delivery: A Case Study
Abstract
:1. Introduction
2. Method
2.1. Case Description
2.2. Procedure
2.2.1. Eyberg Child Behavior Inventory (ECBI)
2.2.2. Psychosocial Strengths Inventory for Children and Adolescents (PSICA)
2.2.3. Emotion Regulation Checklist (ERC)
2.2.4. Sleep Questionnaire
2.2.5. Child Feeding Questionnaire (CFQ)
2.2.6. Parental Feeding Style Questionnaire (PFQ)
2.2.7. Problematic Media Use Measure-Short Form (PMUM-SF)
2.2.8. Parental Mediation Scale (PMS)
2.2.9. Parenting Stress Index-Short Form (PSI-SF)
2.2.10. Barriers to Treatment Participation Scale (BTPS)
2.2.11. Abbreviated Acceptability Rating Profile (AARP)
2.2.12. Treatment Evaluation Inventory-Short Form
2.2.13. Dyadic Parent Child Interaction System (DPICS-IV)
2.3. Treatment
PCIT-Health Telehealth Intervention
3. Results
3.1. Treatment Progress
3.2. Strengths and Challenges of Telehealth
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fryar, C.D.; Carroll, M.D.; Ogden, C.L. Prevalence of Overweight, Obesity, and Severe Obesity among Children and Adolescents Aged 2—19 Years: United States, 1963–1965 through 2015—2016; National Center for Health Statistics: Hyattsviile, MD, USA, 2018.
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity among Adults and Youth: United States, 2015—2016; CDC: Atlanta, GA, USA, 2017.
- Cote, A.T.; Harris, K.C.; Panagiotopoulos, C.; Sandor, G.G.; Devlin, A.M. Childhood obesity and cardiovascular dysfunction. J. Am. Coll. Cardiol. 2013, 62, 1309–1319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lloyd, L.; Langley-Evans, S.; McMullen, S. Childhood obesity and risk of the adult metabolic syndrome: A systematic review. Int. J. Obes. 2012, 36, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bacha, F.; Gidding, S.S. Cardiac abnormalities in youth with obesity and type 2 diabetes. Curr. Diabetes Rep. 2016, 16, 62. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, P.; The, N.S.; Adair, L.S. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obesity 2010, 18, 1801–1804. [Google Scholar] [CrossRef]
- Tan, C.C.; Riley, H.O.; Sturza, J.; Lumeng, J.C.; Miller, A.L. Observed behavioral indicators of child satiation at mealtime: Associations with child characteristics and parent-reported child eating behaviors. Appetite 2021, 166, 105480. [Google Scholar] [CrossRef]
- Yee, A.Z.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef]
- Hearn, M.D.; Baranowski, T.; Baranowski, J.; Doyle, C.; Smith, M.; Lin, L.S.; Resnicow, K. Environmental influences on dietary behavior among children: Availability and accessibility of fruits and vegetables enable consumption. J. Health Educ. 1998, 29, 26–32. [Google Scholar] [CrossRef]
- Birch, L.L.; Fisher, J.O.; Grimm-Thomas, K.; Markey, C.N.; Sawyer, R.; Johnson, S.L. Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite 2001, 36, 201–210. [Google Scholar] [CrossRef]
- Galloway, A.T.; Fiorito, L.; Lee, Y.; Birch, L.L. Parental pressure, dietary patterns, and weight status among girls who are “picky eaters”. J. Am. Diet. Assoc. 2005, 105, 541–548. [Google Scholar] [CrossRef] [Green Version]
- Mason, T.B. Parental instrumental feeding, negative affect, and binge eating among overweight individuals. Eat. Behav. 2015, 17, 107–110. [Google Scholar] [CrossRef]
- Carlson, S.A.; Fulton, J.E.; Lee, S.M.; Foley, J.T.; Heitzler, C.; Huhman, M. Influence of limit-setting and participation in physical activity on youth screen time. Pediatrics 2010, 126, e89–e96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parkes, A.; Green, M.; Pearce, A. Do bedroom screens and the mealtime environment shape different trajectories of child overweight and obesity? Research using the Growing Up in Scotland study. Int. J. Obes. 2020, 44, 790–802. [Google Scholar]
- Buijzen, M.; Valkenburg, P.M. Parental mediation of undesired advertising effects. J. Broadcasting Electron. Media 2005, 49, 153–165. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.V.; Chuang, R.-J.; Rushing, M.; Naylor, B.; Ranjit, N.; Pomeroy, M.; Markham, C. Peer reviewed: Social determinants of health-related needs during COVID-19 among low-income households with children. Prev. Chronic Dis. 2020, 17, E119. [Google Scholar] [CrossRef]
- Jansen, E.; Thapaliya, G.; Aghababian, A.; Sadler, J.; Smith, K.; Carnell, S. Parental stress, food parenting practices and child snack intake during the COVID-19 pandemic. Appetite 2021, 161, 105119. [Google Scholar] [CrossRef]
- Dunton, G.F.; Do, B.; Wang, S.D. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health 2020, 20, 1351. [Google Scholar] [CrossRef]
- Langarizadeh, M.; Tabatabaei, M.S.; Tavakol, K.; Naghipour, M.; Rostami, A.; Moghbeli, F. Telemental health care, an effective alternative to conventional mental care: A systematic review. Acta Inform. Med. 2017, 25, 240. [Google Scholar] [CrossRef] [Green Version]
- Sampaio, M.; Navarro Haro, M.V.; De Sousa, B.; Vieira Melo, W.; Hoffman, H.G. Therapists make the switch to telepsychology to safely continue treating their patients during the COVID-19 pandemic. Virtual reality telepsychology may be next. Front. Virtual Real. 2021, 1, 576421. [Google Scholar] [CrossRef]
- Reese, R.J.; Slone, N.C.; Soares, N.; Sprang, R. Using telepsychology to provide a group parenting program: A preliminary evaluation of effectiveness. Psychol. Serv. 2015, 12, 274. [Google Scholar] [CrossRef]
- Reese, R.J.; Slone, N.C.; Soares, N.; Sprang, R. Telehealth for underserved families: An evidence-based parenting program. Psychol. Serv. 2012, 9, 320. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Dixon, J.F.; Yee, O.M.; Zhang, J.; Chen, Y.A.; DeAngelo, S.; Yellowlees, P.; Hendren, R.; Schweitzer, J.B. A study on the effectiveness of videoconferencing on teaching parent training skills to parents of children with ADHD. Telemed. e-Health 2013, 19, 192–199. [Google Scholar] [CrossRef]
- Fogler, J.M.; Normand, S.; O’Dea, N.; Mautone, J.A.; Featherston, M.; Power, T.J.; Nissley-Tsiopinis, J. Implementing group parent training in telepsychology: Lessons learned during the COVID-19 pandemic. J. Pediatric Psychol. 2020, 45, 983–989. [Google Scholar] [CrossRef] [PubMed]
- Comer, J.S.; Furr, J.M.; Miguel, E.M.; Cooper-Vince, C.E.; Carpenter, A.L.; Elkins, R.M.; Kerns, C.E.; Cornacchio, D.; Chou, T.; Coxe, S. Remotely delivering real-time parent training to the home: An initial randomized trial of Internet-delivered parent–child interaction therapy (I-PCIT). J. Consult. Clin. Psychol. 2017, 85, 909. [Google Scholar] [CrossRef]
- Dodge, K.A.; Greenberg, M.T.; Malone, P.S.; Group, C.P.P.R. Testing an Idealized Dynamic Cascade Model of the Development of Serious Violence in Adolescence. Child Dev. 2008, 79, 1907–1927. [Google Scholar] [CrossRef] [Green Version]
- Fergusson, D.M.; John Horwood, L.; Ridder, E.M. Show me the child at seven: The consequences of conduct problems in childhood for psychosocial functioning in adulthood. J. Child Psychol. Psychiatry 2005, 46, 837–849. [Google Scholar] [CrossRef]
- Obradović, J.; Burt, K.B.; Masten, A.S. Testing a dual cascade model linking competence and symptoms over 20 years from childhood to adulthood. J. Clin. Child Adolesc. Psychol. 2009, 39, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Eyberg, S.; Nelson, M.; Boggs, S. Evidence-based treatments for child and adolescent disruptive behavior disorders. J. Clin. Child Adolesc. Psychol. 2008, 37, 213–235. [Google Scholar] [CrossRef] [PubMed]
- Niec, L.N. Handbook of Parent-Child Interaction Therapy: Innovations and Applications for Research and Practice; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Eyberg, S.; Funderburk, B. Parent–Child Interaction Therapy Protocol; PCIT International: Gainesville, FL, USA, 2011. [Google Scholar]
- Kaminski, J.W.; Valle, L.A.; Filene, J.H.; Boyle, C.L. A meta-analytic review of components associated with parent training program effectiveness. J. Abnorm. Child Psychol. 2008, 36, 567–589. [Google Scholar] [CrossRef] [PubMed]
- Goldfine, M.E.; Wagner, S.M.; Branstetter, S.A.; Mcneil, C.B. Parent-child interaction therapy: An examination of cost-effectiveness. J. Early Intensive Behav. Interv. 2008, 5, 119. [Google Scholar] [CrossRef] [Green Version]
- Hood, K.K.; Eyberg, S.M. Outcomes of parent-child interaction therapy: Mothers’ reports of maintenance three to six years after treatment. J. Clin. Child Adolesc. Psychol. 2003, 32, 419–429. [Google Scholar] [CrossRef]
- Schuhmann, E.M.; Foote, R.C.; Eyberg, S.M.; Boggs, S.R.; Algina, J. Efficacy of parent-child interaction therapy: Interim report of a randomized trial with short-term maintenance. J. Clin. Child Psychol. 1998, 27, 34–45. [Google Scholar] [CrossRef]
- Comer, J.S.; Furr, J.M.; Cooper-Vince, C.; Madigan, R.J.; Chow, C.; Chan, P.T.; Idrobo, F.; Chase, R.M.; McNeil, C.B.; Eyberg, S.M. Rationale and considerations for the internet-based delivery of parent–child interaction therapy. Cogn. Behav. Pract. 2015, 22, 302–316. [Google Scholar] [CrossRef] [Green Version]
- Gurwitch, R.H.; Salem, H.; Nelson, M.M.; Comer, J.S. Leveraging parent–child interaction therapy and telehealth capacities to address the unique needs of young children during the COVID-19 public health crisis. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S82. [Google Scholar] [CrossRef] [PubMed]
- Niec, L. Strengthening the Parent-Child Relationship in Therapy: Laying the Foundation for Healthy Development; American Psychological Association: Washington, DC, USA, 2022. [Google Scholar]
- Ros-DeMarize, R.; Chung, P.; Stewart, R. Pediatric behavioral telehealth in the age of COVID-19: Brief evidence review and practice considerations. Curr. Probl. Pediatric Adolesc. Health Care 2021, 51, 100949. [Google Scholar] [CrossRef]
- Breitenstein, S.M.; Gross, D.; Christophersen, R. Digital delivery methods of parenting training interventions: A systematic review. Worldviews Evid.-Based Nurs. 2014, 11, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Eyberg, S.M.; Pincus, D. ECBI & SESBI-R: Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory-Revised: Professional Manual; Psychological Assessment Resources: Lutz, FL, USA, 1999. [Google Scholar]
- Robinson, E.A.; Eyberg, S.M.; Ross, A.W. The standardization of an inventory of child conduct problem behaviors. J. Clin. Child Adolesc. Psychol. 1980, 9, 22–28. [Google Scholar] [CrossRef]
- Niec, L.; Peer, S.; Courrégé, S. Psychosocial Strengths Inventory for Children and Adolescents (PSICA): Preliminary Psychometrics and Potential Applications; Central Michigan University: Mt Pleasant, MI, USA, 2018; Unpublished manuscript. [Google Scholar]
- Shields, A.; Cicchetti, D. Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Dev. Psychol. 1997, 33, 906. [Google Scholar] [CrossRef]
- Owens, J.A.; Spirito, A.; McGuinn, M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep 2000, 23, 1043–1052. [Google Scholar] [CrossRef] [PubMed]
- Wardle, J.; Guthrie, C.A.; Sanderson, S.; Rapoport, L. Development of the children’s eating behaviour questionnaire. J. Child Psychol. Psychiatry Allied Discip. 2001, 42, 963–970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Domoff, S.E.; Harrison, K.; Gearhardt, A.N.; Gentile, D.A.; Lumeng, J.C.; Miller, A.L. Development and validation of the Problematic Media Use Measure: A parent report measure of screen media “addiction” in children. Psychol. Pop. Media Cult. 2019, 8, 2. [Google Scholar] [CrossRef] [PubMed]
- Valkenburg, P.M.; Krcmar, M.; Peeters, A.L.; Marseille, N.M. Developing a scale to assess three styles of television mediation: “Instructive mediation,” “restrictive mediation,” and “social coviewing”. J. Broadcast. Electron. Media 1999, 43, 52–66. [Google Scholar] [CrossRef]
- Abidin, R.R. Parenting Stress Index, 4th ed.; PAR: Lutz, FL, USA, 2012. [Google Scholar]
- Kazdin, A.E.; Holland, L.; Crowley, M.; Breton, S. Barriers to Treatment Participation Scale: Evaluation and validation in the context of child outpatient treatment. J. Child Psychol. Psychiatry 1997, 38, 1051–1062. [Google Scholar] [CrossRef]
- Tarnowski, K.J.; Simonian, S.J. Assessing treatment acceptance: The Abbreviated Acceptability Rating Profile. J. Behav. Ther. Exp. Psychiatry 1992, 23, 101–106. [Google Scholar] [CrossRef]
- Witt, J.C.; Elliott, S.N. Acceptability of Classroom Intervention Strategies. In Advances in School Psychology; Kratochwill, T.R., Elliott, S.N., Gettinger, M., Eds.; Routledge: London, UK, 1985. [Google Scholar]
- Kelley, M.L.; Heffer, R.W.; Gresham, F.M.; Elliott, S.N. Development of a modified treatment evaluation inventory. J. Psychopathol. Behav. Assess. 1989, 11, 235–247. [Google Scholar] [CrossRef]
- Eyberg, S.; Nelson, M.; Ginn, N.; Bhuiyan, N.; Boggs, S. Dyadic Parent–Child Interaction Coding System (DPICS) Comprehensive Manual for Research and Training, 4th ed.; PCIT International: Gainesville, FL, USA, 2013. [Google Scholar]
- Domoff, S.E.; Niec, L.N. Parent-child interaction therapy as a prevention model for childhood obesity: A novel application for high-risk families. Child. Youth Serv. Rev. 2018, 91, 77–84. [Google Scholar] [CrossRef]
- Niec, L.N.; Barnett, M.L.; Prewett, M.S.; Shanley Chatham, J.R. Group parent-child interaction therapy: A randomized control trial for the treatment of conduct problems in young children. J. Consult. Clin. Psychol. 2016, 84, 682–698. [Google Scholar] [CrossRef]
- Nixon, R.D.; Sweeney, L.; Erickson, D.B.; Touyz, S.W. Parent–child interaction therapy: One-and two-year follow-up of standard and abbreviated treatments for oppositional preschoolers. J. Abnorm. Child Psychol. 2004, 32, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Niec, L.N.; Todd, M.; Brodd, I.; Domoff, S.E. PCIT-Health: Preventing Childhood Obesity by Strengthening the Parent–Child Relationship. Cogn. Behav. Pract. 2020, 29, 335–347. [Google Scholar] [CrossRef]
- Peskin, A.; Sherman, J.; Schmidt, E.; Parlade, M.; Jent, J.; Rothenberg, W.A. Internet Based-PCIT (IPCIT): Recommendations for Service Delivery Prepared in Response to COVID-19 Version 2; PCIT International: High Springs, FL, USA, 2016. [Google Scholar]
- Barnett, M.L.; Sigal, M.; Rosas, Y.G.; Corcoran, F.; Rastogi, M.; Jent, J.F. Therapist experiences and attitudes about implementing Internet-delivered Parent-Child Interaction Therapy during COVID-19. Cogn. Behav. Pract. 2021, 28, 630–641. [Google Scholar] [CrossRef]
- Shinn, M.M.; Timmer, S.G.; Sandoz, T.K. Coaching to improve mealtime parenting in treating pediatric obesity. Clin. Pract. Pediatric Psychol. 2017, 5, 232. [Google Scholar] [CrossRef]
| Survey-Scale | Father | Mother | ||
|---|---|---|---|---|
| Pre-Treatment | Post-Treatment | Pre-Treatment | Post-Treatment | |
| Parenting Practices | ||||
| CFQ—Pressuring to Eat | 3.00 | 1.75 | 3.75 | 1.50 |
| CFQ—Food Restriction | 2.63 | 1.88 | 2.63 | 1.25 |
| PFQ—Emotional Feeding | 2.00 | 1.20 | 1.40 | 1.00 |
| PFQ—Instrumental Feeding | 2.50 | 1.50 | 1.50 | 1.25 |
| PMS—Active Mediation | 10.00 | 15.00 | 11.00 | 20.00 |
| PMS—Restrictive Mediation | 17.00 | 16.00 | 20.00 | 20.00 |
| PMS—Social Co-Viewing | 13.00 | 14.00 | 15.00 | 20.00 |
| PSI—Total Stress | 81.00 | 57.00 | 81.00 | 63.00 |
| Child Functioning | ||||
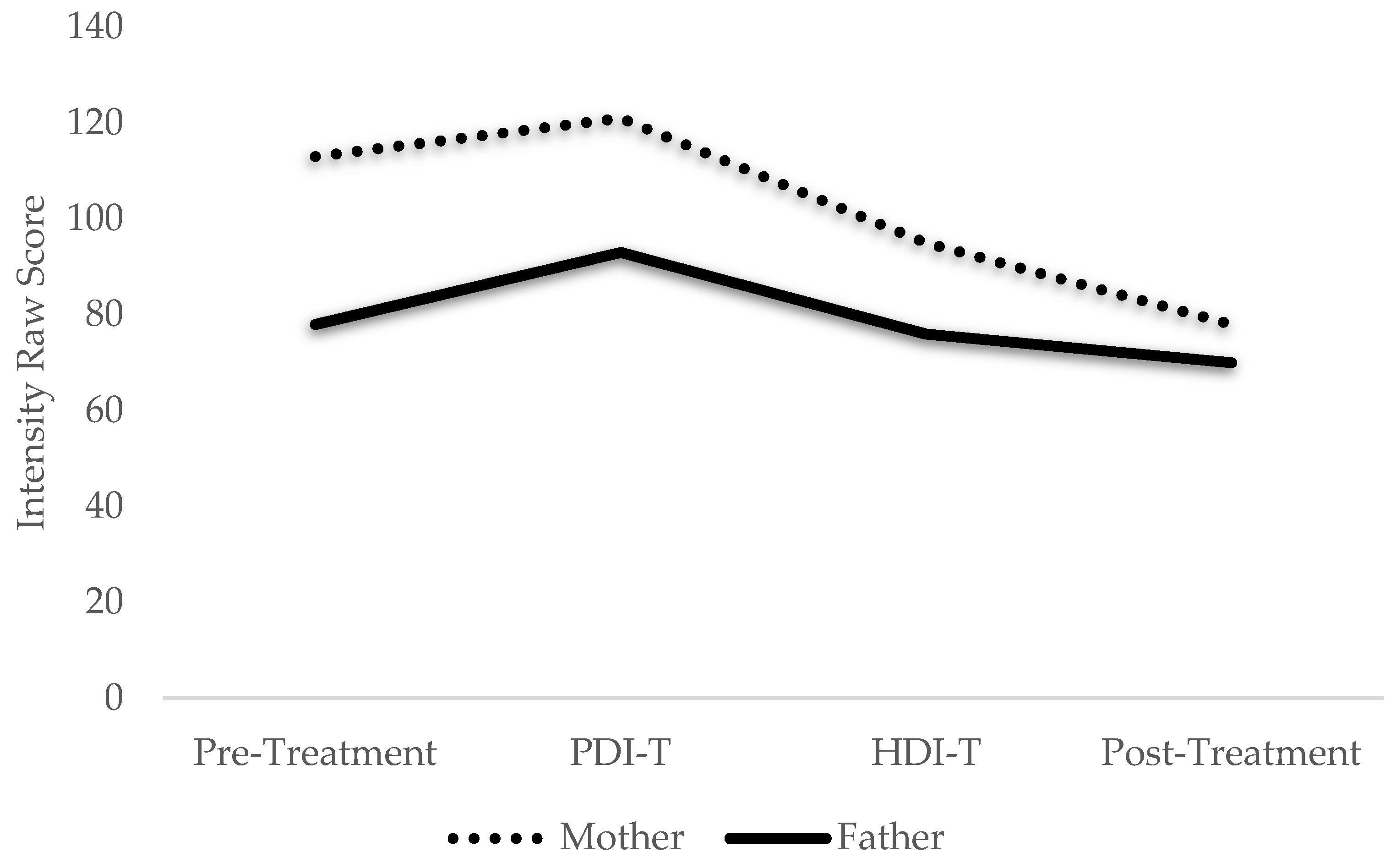
| ECBI—Intensity | 78.00 | 70.00 | 113.00 | 78.00 |
| ERC—Negative Lability | 31.00 | 24.00 | 31.00 | 27.00 |
| ERC—Emotion Regulation | 27.00 | 29.00 | 30.00 | 32.00 |
| PMUM | 2.00 | 1.22 | 1.67 | 1.11 |
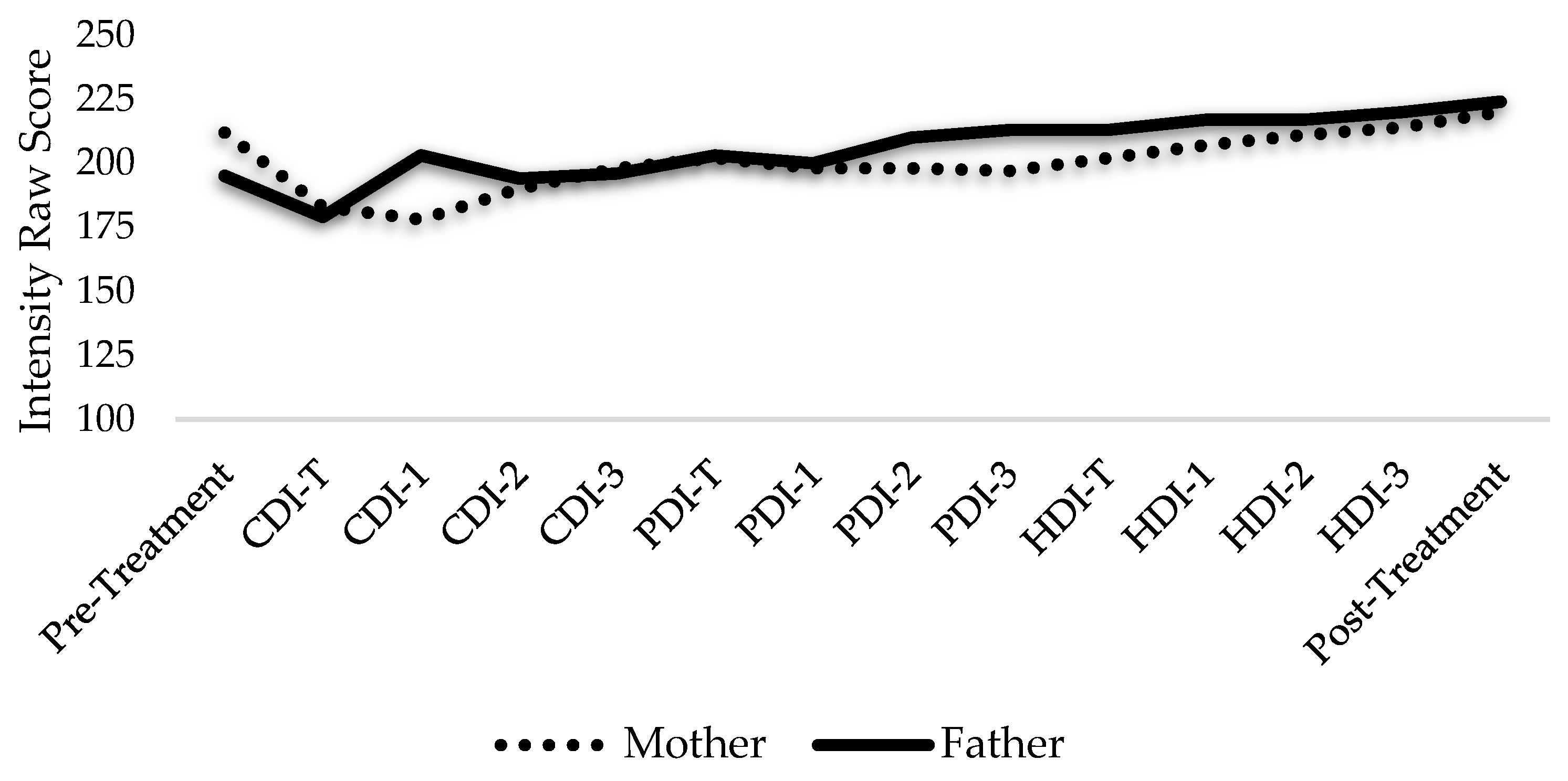
| PSICA—Intensity | 195.00 | 224.00 | 212.00 | 220.00 |
| Screen Time (hours/week) | 18.00 | 10.00 | 9.00 | 2:00 |
| Sleep (hours/night) | 10.00 | 10.00 | 9.00 | 9:00 |
| DPICS-IV Category | Father | Mother | ||
|---|---|---|---|---|
| Pre-Treatment | Post-Treatment | Pre-Treatment | Post-Treatment | |
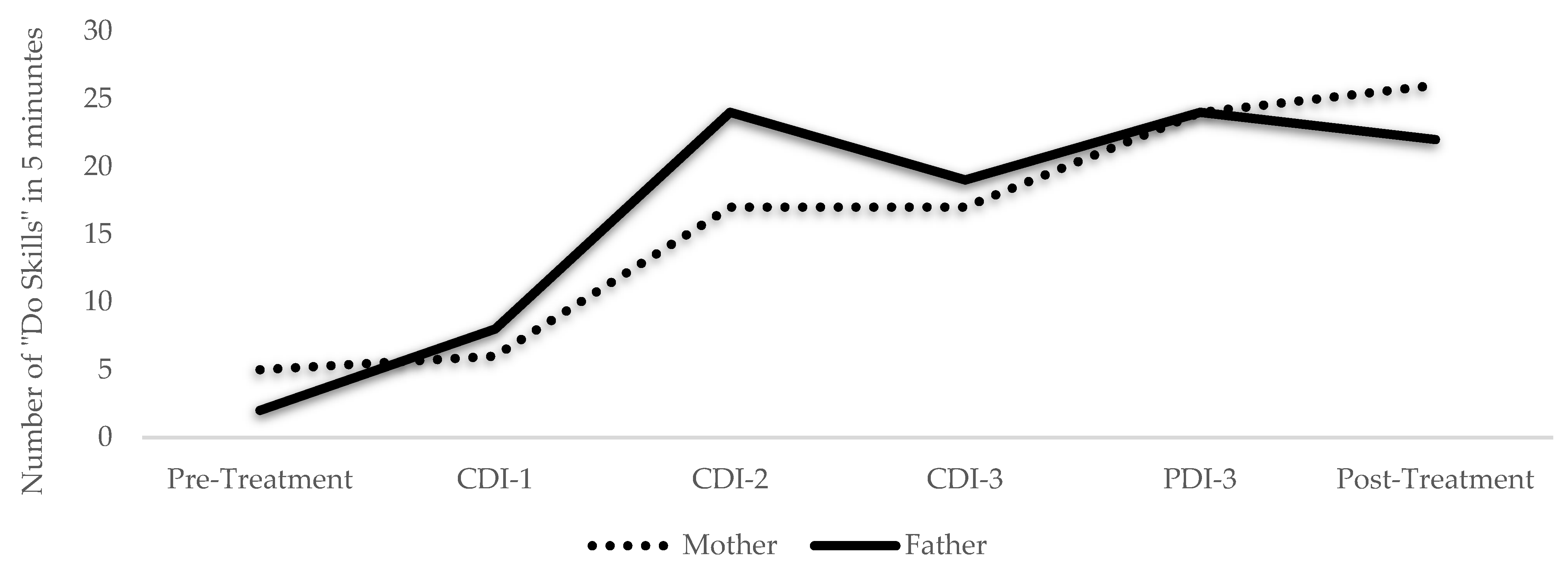
| Do Skills | ||||
| Behavior Descriptions | 0 | 8 | 0 | 5 |
| Reflections | 2 | 4 | 5 | 8 |
| Labeled Praises | 0 | 10 | 0 | 13 |
| Unlabeled Praises | 2 | 0 | 6 | 5 |
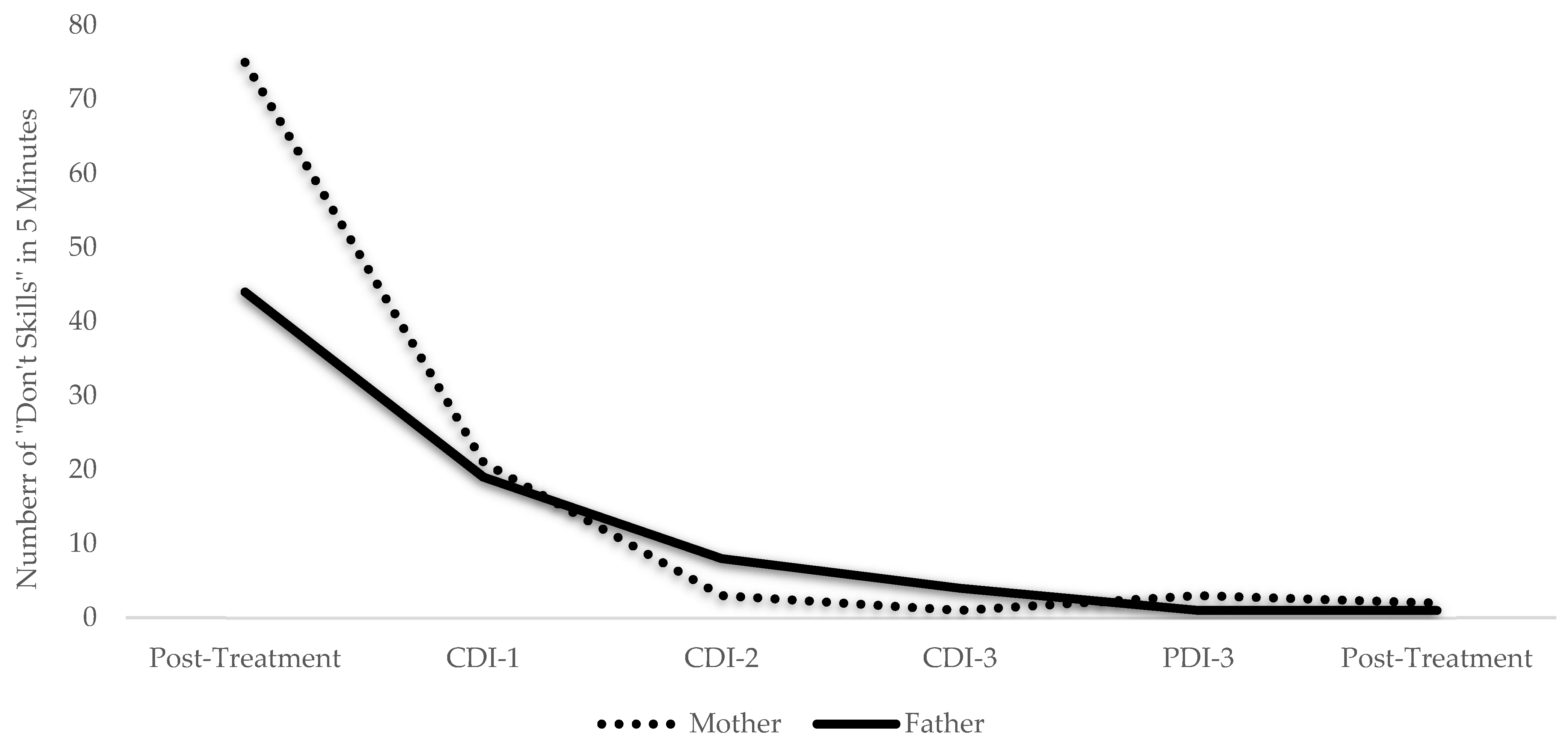
| Don’t Skills | ||||
| Questions | 40 | 0 | 73 | 0 |
| Commands | 4 | 1 | 2 | 2 |
| Criticisms | 0 | 0 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domoff, S.E.; Overton, M.M.; Borgen, A.L.; Niec, L.N. Adapting PCIT-Health for Telehealth Delivery: A Case Study. Int. J. Environ. Res. Public Health 2022, 19, 8352. https://doi.org/10.3390/ijerph19148352
Domoff SE, Overton MM, Borgen AL, Niec LN. Adapting PCIT-Health for Telehealth Delivery: A Case Study. International Journal of Environmental Research and Public Health. 2022; 19(14):8352. https://doi.org/10.3390/ijerph19148352
Chicago/Turabian StyleDomoff, Sarah E., Mikaela M. Overton, Aubrey L. Borgen, and Larissa N. Niec. 2022. "Adapting PCIT-Health for Telehealth Delivery: A Case Study" International Journal of Environmental Research and Public Health 19, no. 14: 8352. https://doi.org/10.3390/ijerph19148352






