Horizontal Integration and Financing Reform of Rural Primary Care in China: A Model for Low-Resource and Remote Settings
Abstract
1. Introduction
2. Methods
2.1. Local Setting
2.2. Data Analysis
3. Results
3.1. Implementation
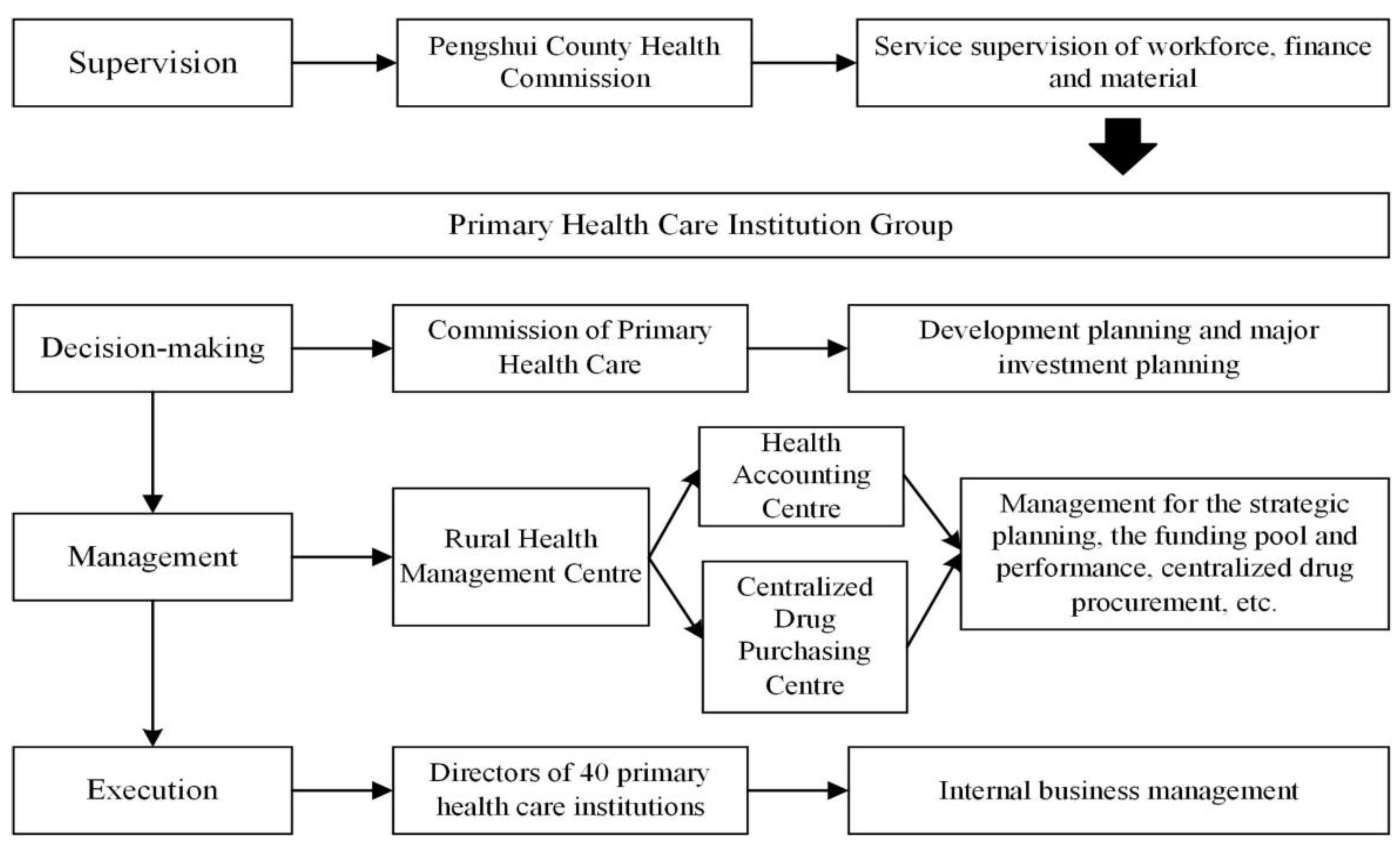
3.1.1. Governance Structure
3.1.2. Financing Mechanisms
3.1.3. Workforce Motivation
3.1.4. Service Delivery
3.2. Achievements
3.2.1. Financing
3.2.2. Equity
3.2.3. Capacity
3.2.4. Performance
4. Discussion
4.1. Lessons Learned
4.2. Future Challenges and Next Steps
4.3. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Universal Health Coverage (UHC). Available online: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc) (accessed on 3 May 2022).
- Chotchoungchatchai, S.; Marshall, A.I.; Witthayapipopsakul, W.; Panichkriangkrai, W.; Patcharanarumol, W.; Tangcharoensathien, V. Primary Health Care and Sustainable Development Goals. Bull. World Health Organ. 2020, 98, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.T.; Chang, A.Y.; Crosby, S.W.; Gloyd, S.; Harle, A.C.; Lim, S.; Lozano, R.; Micah, A.E.; Tsakalos, G.; Su, Y.; et al. Trends and Outcomes in Primary Health Care Expenditures in Low-Income and Middle-Income Countries, 2000–2017. BMJ Glob. Health 2021, 6, e005798. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, M.; Pollard, J.; Sussex, J. Vertical Integration of Primary Care Practices with Acute Hospitals in England and Wales: Why, How and so What? Findings from a Qualitative, Rapid Evaluation. BMJ Open 2022, 12, e053222. [Google Scholar] [CrossRef] [PubMed]
- Hone, T.; Macinko, J.; Millett, C. Revisiting Alma-Ata: What Is the Role of Primary Health Care in Achieving the Sustainable Development Goals? Lancet 2018, 392, 1461–1472. [Google Scholar] [CrossRef]
- Langlois, E.V.; McKenzie, A.; Schneider, H.; Mecaskey, J.W. Measures to Strengthen Primary Health-Care Systems in Low- and Middle-Income Countries. Bull. World Health Organ. 2020, 98, 781–791. [Google Scholar] [CrossRef]
- A Vision for Primary Health Care in the 21st Century: Towards Universal Health Coverage and the Sustainable Development Goals. Available online: https://apps.who.int/iris/handle/10665/328065 (accessed on 8 May 2022).
- Wenang, S.; Schaefers, J.; Afdal, A.; Gufron, A.; Geyer, S.; Dewanto, I.; Haier, J. Availability and Accessibility of Primary Care for the Remote, Rural, and Poor Population of Indonesia. Front. Public Health 2021, 9, 721886. [Google Scholar] [CrossRef]
- Garnelo, L.; Parente, R.C.P.; Puchiarelli, M.L.R.; Correia, P.C.; Torres, M.V.; Herkrath, F.J. Barriers to Access and Organization of Primary Health Care Services for Rural Riverside Populations in the Amazon. Int. J. Equity Health 2020, 19, 54. [Google Scholar] [CrossRef]
- Jin, C.; Cheng, J.; Lu, Y.; Huang, Z.; Cao, F. Spatial Inequity in Access to Healthcare Facilities at a County Level in a Developing Country: A Case Study of Deqing County, Zhejiang, China. Int. J. Equity Health 2015, 14, 67. [Google Scholar] [CrossRef]
- Zheng, L.; Zhang, L.; Chen, K.; He, Q. Unmasking Unexpected Health Care Inequalities in China Using Urban Big Data: Service-Rich and Service-Poor Communities. PLoS ONE 2022, 17, e0263577. [Google Scholar] [CrossRef]
- Walking the Talk: Reimagining Primary Health Care after COVID-19. Available online: https://openknowledge.worldbank.org/handle/10986/35842 (accessed on 15 June 2022).
- Hanson, K.; Brikci, N.; Erlangga, D.; Alebachew, A.; De Allegri, M.; Balabanova, D.; Blecher, M.; Cashin, C.; Esperato, A.; Hipgrave, D.; et al. The Lancet Global Health Commission on Financing Primary Health Care: Putting People at the Centre. Lancet Glob. Health 2022, 10, e715–e772. [Google Scholar] [CrossRef]
- Liu, X.; Wang, Z.; Zhang, H.; Meng, Q. Measuring and Evaluating Progress towards Universal Health Coverage in China. J. Glob. Health 2021, 11, 08005. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Fang, H.; Bishwajit, G.; Xiang, Y.; Fu, H.; Feng, Z. Evaluation of Rural Primary Health Care in Western China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2015, 12, 13843–13860. [Google Scholar] [CrossRef] [PubMed]
- Tao, W.; Zeng, Z.; Dang, H.; Lu, B.; Chuong, L.; Yue, D.; Wen, J.; Zhao, R.; Li, W.; Kominski, G.F. Towards Universal Health Coverage: Lessons from 10 Years of Healthcare Reform in China. BMJ Glob. Health 2020, 5, e002086. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.-M.; Yuan, Y.-X.; Lu, W.; Yang, L. Primary Health Care in China: Is China’s Health Reform Reform for the Whole Nation? Prim. Health Care Res. Dev. 2017, 18, 398–403. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yuan, S.; Fan, F.; van de Klundert, J.; van Wijngaarden, J. Primary Healthcare Professionals’ Perspective on Vertical Integration of Healthcare System in China: A Qualitative Study. BMJ Open 2022, 12, e057063. [Google Scholar] [CrossRef] [PubMed]
- Classification of Chinese Hospitals. Wikipedia. 2022. Available online: https://en.wikipedia.org/wiki/Classification_of_Chinese_hospitals (accessed on 5 May 2022).
- Guo, L.; Bao, Y.; Ma, J.; Li, S.; Cai, Y.; Sun, W.; Liu, Q. Quality of Community Basic Medical Service Utilization in Urban and Suburban Areas in Shanghai from 2009 to 2014. PLoS ONE 2018, 13, e0195987. [Google Scholar] [CrossRef]
- Wang, X.; Sun, X.; Birch, S.; Gong, F.; Valentijn, P.; Chen, L.; Zhang, Y.; Huang, Y.; Yang, H. People-Centred Integrated Care in Urban China. Bull. World Health Organ. 2018, 96, 843–852. [Google Scholar] [CrossRef]
- Lin, W.; Dai, T.; Zhu, X. Analysis on the Practice of Health Care Alliance Reform in Tianchang County of Anhui-Chinese Health Economics. 2017. Available online: https://en.cnki.com.cn/Article_en/CJFDTOTAL-WEIJ201704024.htm (accessed on 5 May 2022).
- Pengshui Miao and Tujia Autonomous County. Wikipedia. 2021. Available online: https://en.wikipedia.org/wiki/Pengshui_Miao_and_Tujia_Autonomous_County (accessed on 5 May 2022).
- Li, X.; Lu, J.; Hu, S.; Cheng, K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Xu, D.R.; Yip, W.; Zhang, H.; et al. The Primary Health-Care System in China. Lancet 2017, 390, 2584–2594. [Google Scholar] [CrossRef]
- Lawn, J.E.; Rohde, J.; Rifkin, S.; Were, M.; Paul, V.K.; Chopra, M. Alma-Ata 30 Years on: Revolutionary, Relevant, and Time to Revitalise. Lancet 2008, 372, 917–927. [Google Scholar] [CrossRef]
- Tao, W.; Zeng, Z.; Dang, H.; Li, P.; Chuong, L.; Yue, D.; Wen, J.; Zhao, R.; Li, W.; Kominski, G. Towards Universal Health Coverage: Achievements and Challenges of 10 Years of Healthcare Reform in China. BMJ Glob. Health 2020, 5, e002087. [Google Scholar] [CrossRef]
- Li, C.; Chen, Z.; Khan, M.M. Bypassing Primary Care Facilities: Health-Seeking Behavior of Middle Age and Older Adults in China. BMC Health Serv. Res. 2021, 21, 895. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.; Tao, W.; Liu, C.; Zhou, L.; Pan, J.; Zhang, W.; He, Y.; Zhang, W.; Zhao, R. Horizontal Integration and Financial Reform of a Primary Care Delivery System in Pengshui County, China: A Case Study. Lancet 2019, 394, S98. [Google Scholar] [CrossRef]
- Veillard, J.; Cowling, K.; Bitton, A.; Ratcliffe, H.; Kimball, M.; Barkley, S.; Mercereau, L.; Wong, E.; Taylor, C.; Hirschhorn, L.R.; et al. Better Measurement for Performance Improvement in Low- and Middle-Income Countries: The Primary Health Care Performance Initiative (PHCPI) Experience of Conceptual Framework Development and Indicator Selection: The Primary Health Care Performance Initiative. Milbank Q. 2017, 95, 836–883. [Google Scholar] [CrossRef] [PubMed]
- Vital Signs Profiles|PHCPI. Available online: https://improvingphc.org/vital-signs-profiles (accessed on 3 May 2022).
- The PHCPI Conceptual Framework. Available online: https://improvingphc.org/phcpi-conceptual-framework (accessed on 18 June 2022).
- Assefa, Y.; Hill, P.S.; Gilks, C.F.; Admassu, M.; Tesfaye, D.; Van Damme, W. Primary Health Care Contributions to Universal Health Coverage, Ethiopia. Bull. World Health Organ. 2020, 98, 894–905A. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Fan, F.; Zhu, D. Effects of Vertical Integration Reform on Primary Healthcare Institutions in China: Evidence From a Longitudinal Study. Int. J. Health Policy Manag. 2021, 1. [Google Scholar] [CrossRef]
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 Years of Health-Care Reform in China: Progress and Gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]
- Li, X.; Krumholz, H.M.; Yip, W.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Li, C.; Lu, J.; Su, M.; et al. Quality of Primary Health Care in China: Challenges and Recommendations. Lancet 2020, 395, 1802–1812. [Google Scholar] [CrossRef]
- Angell, B.; Dodd, R.; Palagyi, A.; Gadsden, T.; Abimbola, S.; Prinja, S.; Jan, S.; Peiris, D. Primary Health Care Financing Interventions: A Systematic Review and Stakeholder-Driven Research Agenda for the Asia-Pacific Region. BMJ Glob. Health 2019, 4, e001481. [Google Scholar] [CrossRef]
- WHO/Europe|from Alma-Ata to Astana: Primary Health Care–Reflecting on the Past, Transforming for the Future. 2018. Available online: https://www.euro.who.int/en/health-topics/Health-systems/primary-health-care/publications/2018/from-alma-ata-to-astana-primary-health-care-reflecting-on-the-past,-transforming-for-the-future-2018 (accessed on 7 May 2022).
- Han, Y.; Wei, J.; Song, X.; Sarah, B.J.; Wen, C.; Zheng, X. Accessibility of Primary Health Care Workforce in Rural China. Asia Pac. J. Public Health 2012, 24, 833–847. [Google Scholar] [CrossRef]
- Zhou, S.; Xu, J.; Ma, X.; Yuan, B.; Liu, X.; Fang, H.; Meng, Q. How Can One Strengthen a Tiered Healthcare System through Health System Reform? Lessons Learnt from Beijing, China. Int. J. Environ. Res. Public Health 2020, 17, 8040. [Google Scholar] [CrossRef]
- Chan, M. Return to Alma-Ata. Lancet 2008, 372, 865–866. [Google Scholar] [CrossRef]
- Vasan, A.; Mabey, D.C.; Chaudhri, S.; Epstein, H.-A.B.; Lawn, S.D. Support and Performance Improvement for Primary Health Care Workers in Low- and Middle-Income Countries: A Scoping Review of Intervention Design and Methods. Health Policy Plan. 2017, 32, 437–452. [Google Scholar] [CrossRef]
- Gong, F.; Hu, G.; Lin, H.; Sun, X.; Wang, W. Integrated Healthcare Systems Response Strategies Based on the Luohu Model during the COVID-19 Epidemic in Shenzhen, China. Int. J. Integr. Care 2021, 21, 1. [Google Scholar] [CrossRef] [PubMed]
- Role of Primary Care in the COVID-19 Response. Available online: https://www.who.int/publications/i/item/WPR-DSE-2020-004 (accessed on 6 May 2022).
- Wan, G.; Wei, X.; Yin, H.; Qian, Z.; Wang, T.; Wang, L. The Trend in Primary Health Care Preference in China: A Cohort Study of 12,508 Residents from 2012 to 2018. BMC Health Serv. Res. 2021, 21, 768. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.; Su, M.; Si, Y.; Zhao, Y.; Zhou, Z. The Benefits of an Integrated Social Medical Insurance for Health Services Utilization in Rural China: Evidence from the China Health and Retirement Longitudinal Study. Int. J. Equity Health 2021, 20, 126. [Google Scholar] [CrossRef]
- China to Further Develop Centralized Drug Procurement. Available online: https://english.www.gov.cn/policies/latestreleases/202101/28/content_WS6012b66ac6d0f72576944b3f.html (accessed on 20 June 2022).
- Zhang, L.; Li, J.; Ma, T.; Zhang, R.; Zhang, Q. Usual Source of Care and Experiences with Primary Care among Community Health Service Centre Patients in Changchun, China: A Cross-sectional Survey. Health Soc. Care Community 2020, 28, 1979–1988. [Google Scholar] [CrossRef]
- Schwarz, D.; Duong, D.; Adam, C.; Awoonor-Williams, J.K.; Back, D.; Bang, A.; Bang, R.; Beebe, M.; Bhatt, S.; Campbell, J.; et al. Primary Care 2030: Creating an Enabling Ecosystem for Disruptive Primary Care Models to Achieve Universal Health Coverage in Low- and Middle-Income Countries. Ann. Glob. Health 2020, 86, 9. [Google Scholar] [CrossRef]
- Ilesanmi, O.; Afolabi, A. Time to Move from Vertical to Horizontal Approach in Our COVID-19 Response in Nigeria. SciMedicine J. 2020, 2, 28–29. [Google Scholar] [CrossRef]
- Continuity and Coordination of Care: A Practice Brief to Support Implementation of the WHO Framework on Integrated People-Centred Health Services. Available online: https://www.who.int/publications/i/item/9789241514033 (accessed on 6 May 2022).


| Index | Domains | Indicator | Definition | Year | % Change (2009–2018) | |
|---|---|---|---|---|---|---|
| 2009 | 2018 | |||||
| Affordability | Financing | Government spending on PHC as % of government health spending (%) | Share of general domestic government health expenditure allocated to PHC | 14.35 | 53.15 | +270.38 |
| Total PHC spending per capita per year (¥) | The absolute amount of spending on PHC per person per year | 86.41 | 429.44 | +396.98 | ||
| Equity | Average cost per outpatient in PHC (¥) | Patients’ average financial burden | 38 | 69 | +81.58 | |
| Average cost per inpatient in PHC (¥) | Patients’ average financial burden | 819 | 1615 | +97.19 | ||
| Accessibility | Capacity | Number of medical beds in PHC | Availability of health facility | 410 | 1242 | +202.93 |
| Number of physicians in PHC | Availability of health workforce | 363 | 857 | +136.09 | ||
| Number of nurses in PHC | Availability of health workforce | 66 | 209 | +216.67 | ||
| Number of health technicians per 1000 population | Availability of health workforce | 1.61 | 5.14 | +219.25 | ||
| Number of physicians per 1000 population | Availability of health workforce | 0.73 | 3.12 | +327.40 | ||
| Number of nurses per 1000 population | Availability of health workforce | 0.43 | 2.12 | +393.02 | ||
| Performance | Number of outpatient visits to PHC (10,000) | Utilization of outpatient services | 52.27 | 84.99 | +62.60 | |
| Number of inpatients in PHC (10,000) | Utilization of inpatient services | 3.05 | 9.32 | +205.57 | ||
| % of outpatient service utilization at PHC level (%) | The attractiveness to patients to use PHC services | 29 | 40 | +37.93 | ||
| % of inpatient service utilization at PHC level (%) | The attractiveness to patients to use PHC services | 67 | 60 | −10.45 | ||
| Typical Model | Context (2020) | Type of Integration | Involved Providers | Funding and Incentives Mechanism | Governance Structure |
|---|---|---|---|---|---|
| Pengshui | Location: county, in a rural area Population: 530,599 GDP: 24.51 billion Area: 3903 km2 | Horizontal integration | Township health centers and community health centers | The policy of fundraising and mutual aid-sharing of compulsory payment improved the compensation mechanism | A clear division of responsibilities and governance structure was developed by establishing a primary health care institution group |
| Luohu | Location: district, in an urban area Population: 1,143,800 GDP: 237.53 billion Area: 78.75 km2 | Vertical integration | Community health centers and local hospitals | A needs-based capitation approach in social health insurance reimbursement, accompanied by differentiated pricing policies, to incentivise primary care groups to save costs | A primary care group was established, which is a network of integrated management, shared responsibilities, and common interests |
| Tianchang | Location: county, close to urban area Population: 603,780 GDP: 54.93 billion Area: 1770 km2 | Vertical integration | Township health centers, community health centers, and local hospitals | An incentive distribution mechanism was designed to contain costs by providing more preventive care to residents | Three primary care groups were established, two of them were led by local public hospitals, and the other group’s leading hospital was a non-profit private hospital |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeng, Z.; Tao, W.; Ding, S.; Fang, J.; Wen, J.; Yao, J.; Zhang, W. Horizontal Integration and Financing Reform of Rural Primary Care in China: A Model for Low-Resource and Remote Settings. Int. J. Environ. Res. Public Health 2022, 19, 8356. https://doi.org/10.3390/ijerph19148356
Zeng Z, Tao W, Ding S, Fang J, Wen J, Yao J, Zhang W. Horizontal Integration and Financing Reform of Rural Primary Care in China: A Model for Low-Resource and Remote Settings. International Journal of Environmental Research and Public Health. 2022; 19(14):8356. https://doi.org/10.3390/ijerph19148356
Chicago/Turabian StyleZeng, Zhi, Wenjuan Tao, Shanlong Ding, Jianlong Fang, Jin Wen, Jianhong Yao, and Wei Zhang. 2022. "Horizontal Integration and Financing Reform of Rural Primary Care in China: A Model for Low-Resource and Remote Settings" International Journal of Environmental Research and Public Health 19, no. 14: 8356. https://doi.org/10.3390/ijerph19148356
APA StyleZeng, Z., Tao, W., Ding, S., Fang, J., Wen, J., Yao, J., & Zhang, W. (2022). Horizontal Integration and Financing Reform of Rural Primary Care in China: A Model for Low-Resource and Remote Settings. International Journal of Environmental Research and Public Health, 19(14), 8356. https://doi.org/10.3390/ijerph19148356






