Healthcare Providers’ Knowledge of Value-Based Care in Germany: An Adapted, Mixed-Methods Approach
Abstract
:1. Introduction
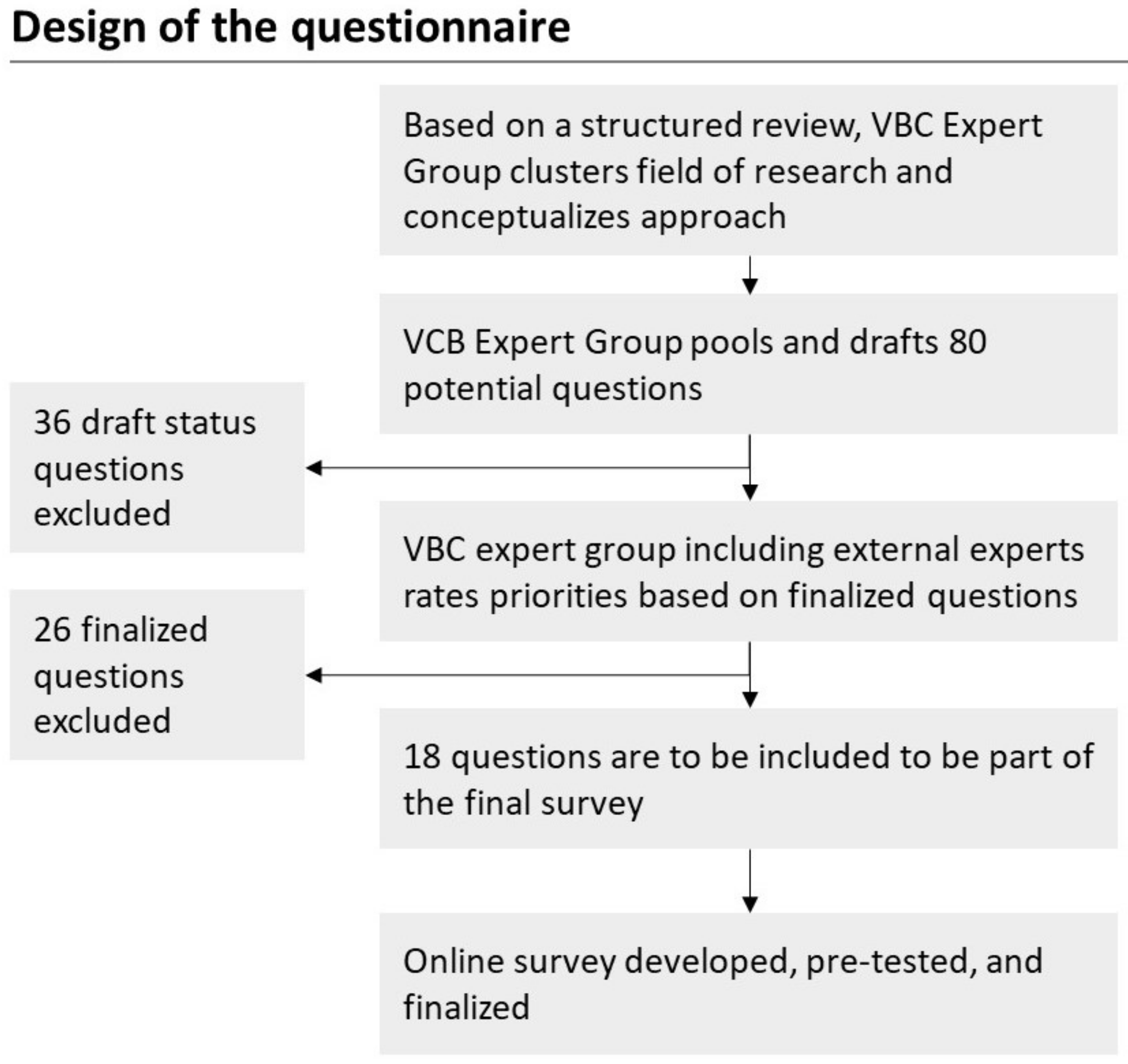
2. Materials and Methods
3. Results
3.1. Identified Published Studies for Evidence and Hypothesis Generation
3.2. Online Survey
3.3. Although Regarded as Desirable, VBC Is Not Yet Broadly Implemented in Clinical Practice
3.4. VBC Can Be Implemented across Medical Fields, but the Cycle of Care Needs to Be Well Defined
3.5. VBC Is Regarded as Carrying Significant Potential to Reduce Costs and to Increase Efficiency
3.6. Although the Implementation of VBC Is Seen as Difficult, Clear Expectations from HCPs Exist
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arce, H.E. How to face the rising costs of healthcare? Medicina 2019, 79, 529–533. [Google Scholar]
- Ray, J.C.; Kusumoto, F. The transition to value-based care. J. Interv. Card. Electrophysiol. 2016, 47, 61–68. [Google Scholar] [CrossRef]
- Jacobs, R.; Honoré, P.M.; Bagshaw, S.M.; Diltoer, M.; Spapen, H.D. Citrate Formulation Determines Filter Lifespan during Continuous Veno-Venous Hemofiltration: A Prospective Cohort Study. Blood Purif. 2015, 40, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.E. What Is Value in Health Care? N. Engl. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.E.; Guth, C. Redefining German Health Care: Moving to a Value-Based System; Springer: Berlin, Germany, 2012. [Google Scholar]
- Conrad, D.A. The Theory of Value-Based Payment Incentives and Their Application to Health Care. Health Serv. Res. 2015, 50, 2057–2089. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.M.; Brown, G.C.; Sharma, S.; Landy, J. Health care economic analyses and value-based medicine. Surv. Ophthalmol. 2003, 48, 204–223. [Google Scholar] [CrossRef]
- Techniker Krankenkasse. Modellvorhaben zur Optimierten Versorgung in der Psychiatrie. Available online: https://www.tk.de/techniker/gesundheit-und-medizin/igv-vertraege/optimierte-versorgung-in-der-psychiatrie-ovp-ruedersdorf-2015504 (accessed on 11 November 2020).
- Liberty, M. Is Germany Really Ready for PHM? 31 May 2018. Available online: https://www.signifyresearch.net/digital-health/is-germany-really-ready-for-phm/ (accessed on 11 November 2020).
- Hoffmann, W. Konzepte und Trends von “Value-Based Healthcare” in Deutschland. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwiNpd3D__zsAhVFqxoKHRQhCmcQFjADegQI-BRAC&url=https%3A%2F%2Foptimedis.de%2Ffiles%2FPetersburger_Dialog%2FHoffmann.pdf&usg=AOvVaw3jeq-4-tRi3uw-MBp5pJUX (accessed on 12 November 2020).
- Lauenroth, V.D.; Kesselheim, A.S.; Sarpatwari, A.; Stern, A.D. Lessons from the Impact of Price Regulation on the Pricing of Anticancer Drugs in Germany. Health Aff. 2020, 39, 1185–1193. [Google Scholar] [CrossRef]
- Bender, K.I.; Lutsevich, A.N. Vzaimodeistvie lekarstvennykh veshchestv s kislym alfa 1-glikoproteidom (orozomukoidom). Interaction of drugs with alpha 1-acid glycoprotein (orosomucoid). Farmakol. Toksikol. 1987, 50, 110–119. [Google Scholar]
- Thielsch, M. PsyWeb Checkliste für Online-Untersuchungen. Available online: https://psyweb.uni-muenster.de/assets/uploads/psyweb-checkliste.pdf (accessed on 7 June 2022).
- Ibrahim, A.M.; Nuliyalu, U.; Lawton, E.J.; O’Neil, S.; Dimick, J.B.; Gulseren, B.; Sinha, S.S.; Hollingsworth, J.M.; Engler, T.A.; Ryan, A.M. Evaluation of US Hospital Episode Spending for Acute Inpatient Conditions After the Patient Protection and Affordable Care Act. JAMA Netw. Open 2020, 3, e2023926. [Google Scholar] [CrossRef]
- Cerreta, F.; Ritzhaupt, A.; Metcalfe, T.; Askin, S.; Duarte, J.; Berntgen, M.; Vamvakas, S. Digital technologies for medicines: Shaping a framework for success. Nat. Rev. Drug Discov. 2020, 19, 573–574. [Google Scholar] [CrossRef]
- Viceconti, M.; Penna, S.H.; Dartee, W.; Mazzà, C.; Caulfield, B.; Becker, C.; Maetzler, W.; Garcia-Aymerich, J.; Davico, G.; Rochester, L. Toward a Regulatory Qualification of Real-World Mobility Performance Biomarkers in Parkinson’s Patients Using Digital Mobility Outcomes. Sensors 2020, 20, 5920. [Google Scholar] [CrossRef]
- Federal Ministry of Health. Driving the Digital Transformation of Germany’s Healthcare System for the Good of Patients. Available online: https://www.bundesgesundheitsministerium.de/digital-healthcare-act.html (accessed on 3 December 2020).
- Papanicolas, I.; Woskie, L.; Jha, A.K. Health Care Spending in the United States and Other High-Income Countries. JAMA 2018, 319, 1024–1039. [Google Scholar] [CrossRef] [PubMed]
- Kraus, J.M.; Lausser, L.; Kuhn, P.; Jobst, F.; Bock, M.; Halanke, C.; Hummel, M.; Heuschmann, P.; Kestler, H.A. Big data and precision medicine: Challenges and strategies with healthcare data. Int. J. Data Sci. Anal. 2018, 6, 241–249. [Google Scholar] [CrossRef]
- Gostin, L.O.; Halabi, S.F.; Wilson, K. Health Data and Privacy in the Digital Era. JAMA 2018, 320, 233. [Google Scholar] [CrossRef] [PubMed]
- Perry, L.L.; Williams, I.R. Regulation of transplantation immunity in vivo by monoclonal antibodies recognizing host class II restriction elements. I. Genetics and specificity of anti-Ia immunotherapy in murine skin allograft recipients. J. Immunol. 1985, 134, 2935–2941. [Google Scholar]
- Gusmano, M.K.; Laugesen, M.; Rodwin, V.G.; Brown, L.D. Getting the Price Right: How Some Countries Control Spending in a Fee-For-Service System. Health Aff. 2020, 39, 1867–1874. [Google Scholar] [CrossRef]
- Gaßner, H.; Sanders, P.; Dietrich, A.; Marxreiter, F.; Eskofier, B.M.; Winkler, J.; Klucken, J. Clinical Relevance of Standardized Mobile Gait Tests. Reliability Analysis between Gait Recordings at Hospital and Home in Parkinson’s Disease: A Pilot Study. J. Park. Dis. 2020, 10, 1763–1773. [Google Scholar] [CrossRef]
- Polhemus, A.M.; Bergquist, R.; de Basea, M.B.; Brittain, G.; Buttery, S.C.; Chynkiamis, N.; Costa, G.D.; Ortiz, L.D.; Demeyer, H.; Emmert, K.; et al. Walking-related digital mobility outcomes as clinical trial endpoint measures: Protocol for a scoping review. BMJ Open 2020, 10, e038704. [Google Scholar] [CrossRef]
- DiGioia, A.M.; Greenhouse, P.K.; Giarrusso, M.L.; Kress, J.M. Determining the True Cost to Deliver Total Hip and Knee Arthroplasty Over the Full Cycle of Care: Preparing for Bundling and Reference-Based Pricing. J. Arthroplast. 2016, 31, 1–6. [Google Scholar] [CrossRef]
- Blaschke, B.L.; Parikh, H.R.; Vang, S.X.; Cunningham, B.P. Time-Driven Activity-Based Costing: A Better Way to Understand the Cost of Caring for Hip Fractures. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320958202. [Google Scholar] [CrossRef]
- Papanicolas, I.; Mossialos, E.; Gundersen, A.; Woskie, L.; Jha, A.K. Performance of UK National Health Service compared with other high income countries: Observational study. BMJ 2019, 367, l6326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gottlieb, N.; Schülle, M. An overview of health policies for asylum-seekers in Germany. Health Policy 2020, 125, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Die Gesetzlichen Krankenkassen. GKV Spitzenverband. 1 January 2020. Available online: https://www.gkv-spitzenverband.de/krankenversicherung/kv_grundprinzipien/alle_gesetzlichen_krankenkassen/alle_gesetzlichen_krankenkassen.jsp#:~:text=Heute%20gibt%20es%20nur%20noch%20105%20Kassen%20(Stand%3A%2001 (accessed on 3 December 2020).
- Phipps-Taylor, M.; Shortell, S.M. More than Money: Motivating Physician Behavior Change in Accountable Care Organizations. Milbank Q. 2016, 94, 832–861. [Google Scholar] [CrossRef] [Green Version]
- Carignani, V. Management of change in health care organisations and human resource role. Eur. J. Radiol. 2000, 33, 8–13. [Google Scholar] [CrossRef]
- Vennemann, M.; Ruland, V.; Kruse, J.-P.; Harloff, C.; Trübel, H.; Gielen-Haertwig, H. Future unmet medical need as a guiding principle for pharmaceutical R&D. Drug Discov. Today 2019, 24, 1924–1929. [Google Scholar] [CrossRef] [PubMed]
- Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. Aufgaben und Ziele des IQWiG. Available online: https://www.iqwig.de/de/ueber-uns/aufgaben-und-ziele.2946.html (accessed on 3 December 2020).
- Hansen, A.; Herrmann, M.; Ehlers, J.P.; Mondritzki, T.; Hensel, K.O.; Truebel, H.; Boehme, P. Perception of the Progressing Digitization and Transformation of the German Health Care System Among Experts and the Public: Mixed Methods Study. JMIR Public Health Surveill. 2019, 5, e14689. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Demographics | Options | N | Percentage |
|---|---|---|---|
| Gender | Male | 353 | 51.4 |
| Female | 319 | 46.4 | |
| Divers | 1 | 0.1 | |
| N/A | 14 | 2.1 | |
| Age | 16–20 | 12 | 1.7 |
| 21–30 | 211 | 30.7 | |
| 31–40 | 215 | 31.3 | |
| 41–50 | 110 | 16 | |
| 51–60 | 110 | 16 | |
| 61–70 | 25 | 3.6 | |
| N/A | 4 | 0.6 | |
| Profession | Physician | 438 | 63.8 |
| Nurse | 65 | 9.5 | |
| Medical student | 126 | 18.3 | |
| Miscellaneous | 58 | 8.4 | |
| Professional experience (years) | N/A & Med-students | 134 | 19.5 |
| 1–5 | 156 | 22.7 | |
| 6–10 | 120 | 17.5 | |
| 11–20 | 124 | 18.1 | |
| 21–30 | 106 | 15.4 | |
| >30 | 47 | 6.8 | |
| Leading position | Yes | 252 | 36.7 |
| No | 333 | 48.5 | |
| N/MA | 93 | 13.5 | |
| N/A | 9 | 1.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuck, A.; Kinscher, K.; Fehring, L.; Hildebrandt, H.; Doerner, J.; Lange, J.; Truebel, H.; Boehme, P.; Bade, C.; Mondritzki, T. Healthcare Providers’ Knowledge of Value-Based Care in Germany: An Adapted, Mixed-Methods Approach. Int. J. Environ. Res. Public Health 2022, 19, 8466. https://doi.org/10.3390/ijerph19148466
Kuck A, Kinscher K, Fehring L, Hildebrandt H, Doerner J, Lange J, Truebel H, Boehme P, Bade C, Mondritzki T. Healthcare Providers’ Knowledge of Value-Based Care in Germany: An Adapted, Mixed-Methods Approach. International Journal of Environmental Research and Public Health. 2022; 19(14):8466. https://doi.org/10.3390/ijerph19148466
Chicago/Turabian StyleKuck, Axel, Kristian Kinscher, Leonard Fehring, Helmut Hildebrandt, Johannes Doerner, Jonas Lange, Hubert Truebel, Philip Boehme, Celina Bade, and Thomas Mondritzki. 2022. "Healthcare Providers’ Knowledge of Value-Based Care in Germany: An Adapted, Mixed-Methods Approach" International Journal of Environmental Research and Public Health 19, no. 14: 8466. https://doi.org/10.3390/ijerph19148466
APA StyleKuck, A., Kinscher, K., Fehring, L., Hildebrandt, H., Doerner, J., Lange, J., Truebel, H., Boehme, P., Bade, C., & Mondritzki, T. (2022). Healthcare Providers’ Knowledge of Value-Based Care in Germany: An Adapted, Mixed-Methods Approach. International Journal of Environmental Research and Public Health, 19(14), 8466. https://doi.org/10.3390/ijerph19148466






