Care Recommendations for the Chronic Risk of COVID-19: Nursing Intervention for Behaviour Changes
Abstract
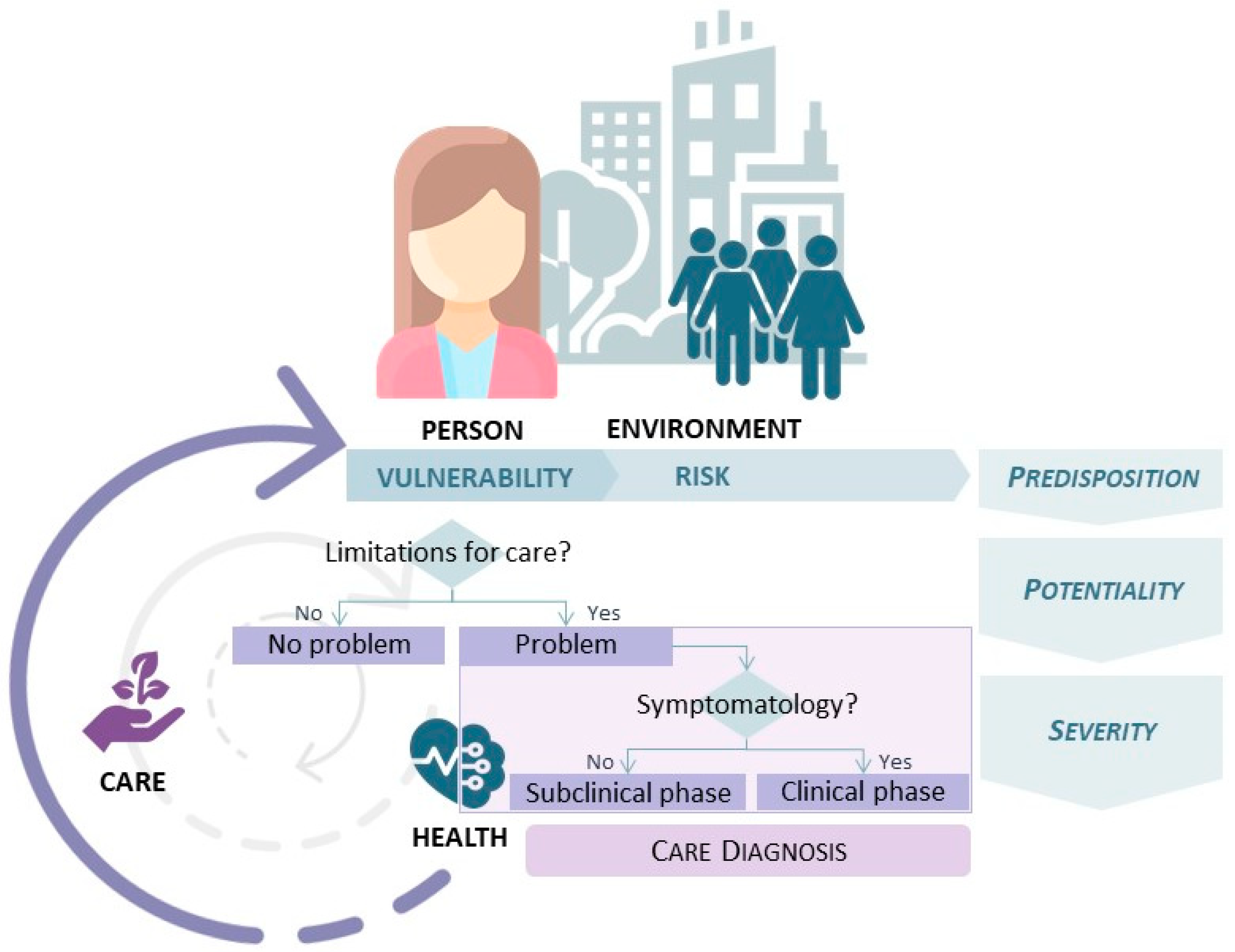
:1. Introduction
Main Aim
2. Materials and Methods
2.1. Design
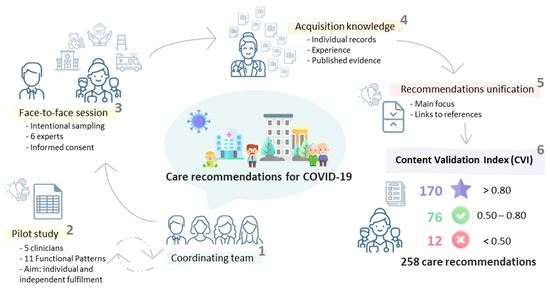
2.2. Procedure
2.2.1. Phase I—Acquisition of Expert Knowledge
2.2.2. Phase II—Validation of Recommendations
3. Results
3.1. Phase I—Acquisition of Expert Knowledge
3.2. Phase II—Validation of Recommendations
4. Discussion
4.1. Limitations and Future Lines
4.2. Relevance to Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Pneumonia of Unknown Cause—China. Available online: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkowncause-china/en/ (accessed on 1 May 2022).
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-openingremarks-at-the-media-briefing-on-covid-1 (accessed on 1 May 2022).
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is Suspected. Interim Guidance. 13 March 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf (accessed on 1 May 2022).
- Chaudhry, R.; Dranitsaris, G.; Mubashir, T.; Bartosko, J.; Riazi, S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. EClinicalMedicine 2020, 25, 100464. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 Vaccines. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 1 May 2022).
- Lopez Bernal, J.; Andrews, N.; Gower, C.; Robertson, C.; Stowe, J.; Tessier, E.; Simmons, R.; Cottrell, S.; Roberts, R.; O’Doherty, M.; et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on COVID-19 related symptoms, hospital admissions, and mortality in older adults in England: Test negative case-control study. BMJ 2021, 373, n1088. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Living Guidance for Clinical Management of COVID-19. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2 (accessed on 1 May 2022).
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 1 May 2022).
- World Health Organization. WHO and Partners Call for Urgent Investment in Nurses. Available online: https://www.who.int/news-room/detail/07-04-2020-who-and-partners-call-for-urgent-investment-in-nurses (accessed on 1 May 2022).
- World Health Organization; International Council of Nurses, & Nursing Now. World Health Organization. State of the World’s Nursing 2020: Investing in Education, Jobs and Leadership; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-000327-9. [Google Scholar]
- All-Party Parliamentary Group on Global Health (APPG). Triple Impact—How Developing Nursing Will Improve Health, Promote Gender Equality and Support Economic Growth; APPG: London, UK, 2016; Available online: https://globalhealth.inparliament.uk/sites/globalhealth.inparliament.uk/files/2020-12/DIGITAL%20APPG%20Triple%20Impact%20%283%29.pdf (accessed on 1 May 2022).
- Alligood, M.R. Nursing Theorists and Their Work, 9th ed.; Elsevier: St. Louis, MO, USA, 2018. [Google Scholar]
- Herdman, T.H.; Kamitsuru, S. NANDA International Nursing Diagnoses: Definitions and Classification, 2018–2020, 11th ed.; Thieme Publishers: New York, NY, USA, 2017. [Google Scholar]
- International Council of Nurses about ICNP. Available online: https://www.icn.ch/what-we-do/projects/ehealth-icnp/about-icnp (accessed on 1 May 2022).
- Martin, K.S. The Omaha System. Available online: http://omahasystemmn.org/OmahaSystemVisualization/OmahaSystem_v9.html (accessed on 1 May 2022).
- Jiménez Rodríguez, M.L.; Santamaría García, J.M.; Plata Barchino, R.; Laita, L.; Laita de la Rica, L.M.; González Sotos, L.A.; Asenjo Esteve, A.L. Knowledge representation for diagnosis of care problems through an expert system: Model of the auto-care deficit situations. Expert Syst. Appl. 2008, 34, 2847–2857. [Google Scholar] [CrossRef]
- Gonzalez Aguña, A. El Lenguaje Normalizado Como Representación del Conocimiento: La Variable del Cuidado, Base Para el Desarrollo de Sistemas Basados en Conocimiento (Normalized Language as a Representation of Knowledge: Care Variable, Basis for the Development of Knowledge-Based Systems). Ph.D. Thesis, Universidad de Alcalá, Madrid, Spain, 2021. [Google Scholar]
- Jiménez Rodríguez, M.L. Sistema Basado en Conocimientos Para la Ayuda en el Diagnóstico del Cansancio del Desempeño del rol del Cuidador (Knowledge-Based System to help diagnose Caregiver Role Strains). Ph.D. Thesis, Universidad de Alcalá, Madrid, Spain, 2006. [Google Scholar]
- Santamaría García, J.M. Investigación Deductiva, Representación Lógica e Implementación Computacional Sobre las Limitaciones de Acción del Autocuidado Según el Modelo de Dorothea Orem (Deductive Research, Logical Representation and Computational Implementation on the Action Limitations of Self-Care according to Dorothea Orem’s Model). Ph.D. Thesis, Universidad de Alcalá, Madrid, Spain, 2008. [Google Scholar]
- Arribas Cachá, A.; Jiménez Rodríguez, M.L.; Santamaría García, J.M.; Sellán Soto, M.C.; Gómez González, J.L.; García Calvo, R.; Borrego de la Osa, R. Delimitación y Ponderación de las Poblaciones con Mayor Vulnerabilidad a Requerimientos de Cuidados Profesionales: Índice de Gravosidad Asistencial Basado en Factores Condicionantes Básicos, 1st ed.; FUDEN: Madrid, Spain, 2009. [Google Scholar]
- Fernández Batalla, M.; Monsalvo San Macario, E.; González Aguña, A.; Herrero Jaén, S.; Gonzalo de Diego, B.; Manrique Anaya, Y.; Jiménez Rodríguez, M.L.; Melguizo Herrera, E.; Santamaría García, J.M. Validation and reliability of the Care Vulnerability Index: A study by interrater agreement and test–retest method. Nurs. Open 2022, 9, 1766–1773. [Google Scholar] [CrossRef] [PubMed]
- González Aguña, A.; Fernández Batalla, M.; Monsalvo San Macario, E.; Sarrión Bravo, J.A.; Jiménez Rodríguez, M.L.; Santamaría García, J.M. Diagnostics of care about environment: A systematic review through nursing taxonomies. Nurs. Open 2021, 8, 2272–2283. [Google Scholar] [CrossRef] [PubMed]
- Herrero Jaén, S. Formalización del concepto de salud a través de la lógica: Impacto del lenguaje formal en las ciencias de la salud. Ene Rev. de Enfermería 2016, 10. Available online: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1988-348X2016000200006 (accessed on 26 June 2022).
- Martyushev-Poklad, A.; Yankevich, D.; Petrova, M. Improving the Effectiveness of Healthcare: Diagnosis-Centered Care Vs. Person-Centered Health Promotion, a Long Forgotten New Model. Front. Public Health 2022, 10, 819096. [Google Scholar] [CrossRef]
- Somers, M.J.; Casal, J. Patterns of coping with work-related stress: A person-centred analysis with text data. Stress Health 2021, 37, 223–231. [Google Scholar] [CrossRef]
- World Health Organization. Health System Performance Assessment: A Framework for Policy Analysis. Available online: https://www.who.int/publications/i/item/9789240042476 (accessed on 26 June 2022).
- Moorhead, S.; Macieira, T.; Lopez, K.D.; Mantovani, V.M.; Swanson, E.; Wagner, C.; Abe, N. NANDA-I, NOC, and NIC Linkages to SARSCov-2 (COVID-19): Part 1. Community Response. Int. J. Nurs. Knowl. 2021, 32, 59–67. [Google Scholar] [CrossRef]
- González Aguña, A.; Jiménez Rodríguez, M.L.; Fernández Batalla, M.; Herrero Jaén, S.; Monsalvo San Macario, E.; Real Martínez, V.; Santamaría García, J.M. Nursing Diagnoses for Coronavirus Disease, COVID-19: Identification by Taxonomic Triangulation. Int. J. Nurs. Knowl. 2021, 32, 108–116. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines. Available online: https://www.who.int/publications/who-guidelines (accessed on 1 May 2022).
- Ministerio de Sanidad, Servicio Sociales e Igualdad. Consejo Integral en Estilo de Vida en Atención Primaria, Vinculado con Recursos Comunitarios en Población Adulta Estrategia de Promoción de la Salud y Prevención en el SNS; Ministerio de Sanidad, Servicio Sociales e Igualdad: Madrid, Spain, 2019. [Google Scholar]
- O’Cathain, A.; Murphy, E.; Nicholl, J. The quality of mixed methods studies in health services research. J. Health Serv. Res. Policy. 2008, 13, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Potter, P.A.; Perry, A.G. Fundamentals of Nursing; Elsevier: St. Louis, MO, USA, 2017. [Google Scholar]
- González Aguña, A.; Fernández Batalla, M.; Díaz-Tendero Rodríguez, J.; Sarrión Bravo, J.A.; Gonzalo de Diego, B.; Santamaría García, J.M. Validation of a manual of care plans for people hospitalized with COVID-19. Nurs. Open 2021, 8, 3495–3515. [Google Scholar] [CrossRef]
- Bu, X.; Wu, Y.W. Development and psychometric evaluation of the instrument: Attitude toward patient advocacy. Res. Nurs. Health 2008, 31, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Frank-Stromborg, M.; Olsen, S. Instruments for Clinical Health-Care Research, 3rd ed.; Jones and Bartlett Publishers: London, UK, 2004. [Google Scholar]
- Polit, D.F.; Beck, C.T. Essentials of Nursing Research: Appraising Evidence for Nursing Practice, 9th ed.; Wolters Kluwer Health/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2017. [Google Scholar]
- World Health Organization. Advice for the Public: Coronavirus Disease (COVID-19). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 1 May 2022).
- Ministerio de Sanidad. Ministerio de Sanidad–Profesionales–Información Para la Ciudadanía–Coronavirus. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/ciudadania.htm (accessed on 1 May 2022).
- Tri Sakti, A.M.; Mohd Ajis, S.Z.; Azlan, A.A.; Kim, H.J.; Wong, E.; Mohamad, E. Impact of COVID-19 on School Populations and Associated Factors: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 4024. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Zhao, C. A Review of the Current Status of Clinical Management of COVID-19 in the Elderly. Med. Sci. Monit. 2021, 27, e930278. [Google Scholar] [CrossRef]
- Goveas, J.S.; Shear, M.K. Grief and the COVID-19 Pandemic in Older Adults. Am. J. Geriatr. Psychiatry 2020, 28, 1119–1125. [Google Scholar] [CrossRef]
- López, V.; Vázquez, T.; Alonso-Titos, J.; Cabello, M.; Alonso, A.; Beneyto, I.; Crespo, M.; Díaz-Corte, C.; Franco, A.; González-Roncero, F.; et al. Recommendations on management of the SARS-CoV-2 coronavirus pandemic (COVID-19) in kidney transplant patients. Nefrologia 2020, 40, 265–271. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Barrea, L.; Savastano, S.; Colao, A. Nutritional recommendations for COVID-19 quarantine. Eur. J. Clin. Nutr. 2020, 74, 850–851. [Google Scholar] [CrossRef]
- Shanthanna, H.; Strand, N.H.; Provenzano, D.A.; Lobo, C.; Eldabe, S.; Bhatia, A.; Wegener, J.; Curtis, K.; Cohen, S.; Narouze, S. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia 2020, 75, 935–944. [Google Scholar] [CrossRef] [Green Version]
- Bresadola, V.; Biddau, C.; Puggioni, A.; Tel, A.; Robiony, M.; Hodgkinson, J.; Leo, C.A. General surgery and COVID-19: Review of practical recommendations in the first pandemic phase. Surg. Today 2020, 50, 1159–1167. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. Protocols and Guidelines for the Reopening of Schools in Latin America and the Caribbean Countries. Available online: https://www.unicef.org/lac/en/protocols-and-guidelines-reopening-schools-latin-america-and-caribbean-countries (accessed on 1 May 2022).
- Ministerio de Educación y Formación Profesional. Plan de Contingencia. Incorporación a las Aulas en Septiembre Curso 2020–21. Available online: https://www.educacionyfp.gob.es/dam/jcr:3bf07ead-5a95-4240-97dc-b5c84fc35f83/plan-contingencia-covid2021.pdf (accessed on 1 May 2022).
- Koleva, G.; Rico, M.; García López, F.J.; Figuera, D.; Padilla, J.; García, M. The impact of COVID-19 in nursing homes in Madrid, Spain: A need for assessment. Lancet Reg. Health Eur. 2021, 11, 100261. [Google Scholar] [CrossRef] [PubMed]
- Escribano, P.; Pérez Granda, M.J.; Alonso, R.; Catalán, P.; Alcalá, L.; Serra-Rexarch, J.A.; Osuna, L.; Fernández, A.; Conti, A.; Castellanos, A.; et al. High incidence of COVID-19 at nursing homes in Madrid, Spain, despite preventive measures. Rev. Esp. Quimioter. 2022, 35, 288–292. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine. The Future of Nursing 2020–2030: Charting a Path to Achieve Health Equity; The National Academies Press: Washington, DC, USA, 2021. [Google Scholar]
- World Health Organization. Global Strategic Directions for Nursing and Midwifery 2021–2025; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
| Data | Meaning |
|---|---|
| Recommendation element | Subunit that guides the global assessment of the different aspects that constitute each pattern |
| Recommendation regarding | Cell for recording the contributions of each participant that will be converted into a recommendation |
| Bibliographicl source | Cell for recording the bibliographic sources that support the contribution made. |
| Functional Pattern | Records Provided (n) | Recommendations n (%) |
|---|---|---|
| 1. Health Perception–Health Management | 73 | 30 (11.63) |
| 2. Nutrition–Metabolism | 84 | 27 (10.47) |
| 3. Elimination | 26 | 12 (4.65) |
| 4. Activity–Exercise | 74 | 30 (11.63) |
| 5. Sleep–Rest | 33 | 14 (5.43) |
| 6. Cognition–Perception | 58 | 31 (12.02) |
| 7. Self-Perception–Self-Concept | 48 | 18 (6.98) |
| 8. Roles–Relationships | 71 | 31 (12.02) |
| 9. Sexuality–Reproduction | 53 | 21 (8.14) |
| 10. Coping–Stress Tolerance | 53 | 20 (7.75) |
| 11. Values–Belief | 51 | 24 (9.30) |
| Functional Pattern | Mean CVI | Max. CVI | Min. CVI | Recommendations High Validation n (%) | Recommendations Not Approved n (%) | No Answer n (%) |
|---|---|---|---|---|---|---|
| 1. Health Perception–Health Management | 0.83 | 1.00 | 0.20 | 20 (66.67) | 2 (6.67) | 6 (3.33) |
| 2. Nutrition–Metabolism | 0.87 | 1.00 | 0.40 | 19 (70.37) | 1 (3.70) | 5 (3.09) |
| 3. Elimination | 0.87 | 1.00 | 0.40 | 9 (75.00) | 1 (8.33) | 4 (5.56) |
| 4. Activity–Exercise | 0.82 | 1.00 | 0.33 | 18 (60.00) | 1 (3.33) | 2 (1.11) |
| 5. Sleep–Rest | 0.83 | 1.00 | 0.50 | 9 (64.29) | 0 (0.00) | 2 (2.38) |
| 6. Cognition–Perception | 0.81 | 1.00 | 0.50 | 20 (64.52) | 0 (0.00) | 5 (2.69) |
| 7. Self-Perception–Self-Concept | 0.87 | 1.00 | 0.33 | 15 (83.33) | 1 (5.56) | 0 (0.00) |
| 8. Roles–Relationships | 0.83 | 1.00 | 0.33 | 22 (70.97) | 1 (3.23) | 2 (1.08) |
| 9. Sexuality–Reproduction | 0.70 | 1.00 | 0.17 | 6 (28.57) | 4 (19.05) | 4 (3.17) |
| 10. Coping–Stress Tolerance | 0.93 | 1.00 | 0.67 | 16 (80.00) | 0 (0.00) | 0 (0.00) |
| 11. Values–Belief | 0.87 | 1.00 | 0.17 | 16 (66.67) | 1 (4.17) | 0 (0.00) |
| Functional Pattern | Recommendation | Contributing Participants % | CVI |
|---|---|---|---|
| 1 |
| 17% | 1.00 |
| 17% | 1.00 | |
| 2 |
| 83% | 1.00 |
| 3 |
| 67% | 1.00 |
| 67% | 1.00 | |
| 4 |
| 83% | 1.00 |
| 50% | 1.00 | |
| 50% | 1.00 | |
| 5 |
| 33% | 1.00 |
| 6 |
| 33% | 1.00 |
| 7 |
| 83% | 1.00 |
| 17% | 1.00 | |
| 83% | 1.00 | |
| 8 |
| 67% | 1.00 |
| 50% | 1.00 | |
| 33% | 1.00 | |
| 67% | 1.00 | |
| 50% | 1.00 | |
| 9 |
| 67% | 1.00 |
| 10 |
| 17% | 1.00 |
| 67% | 1.00 | |
| 11 |
| 50% | 1.00 |
| Functional Pattern | Recommendation | Contributing Participants % | CVI |
|---|---|---|---|
| 1 |
| 17% | 0.40 |
| 17% | 0.20 | |
| 2 |
| 17% | 0.40 |
| 3 |
| 17% | 0.40 |
| 4 |
| 17% | 0.33 |
| 7 |
| 17% | 0.33 |
| 8 |
| 17% | 0.33 |
| 9 |
| 17% | 0.17 |
| 17% | 0.33 | |
| 17% | 0.33 | |
| 17% | 0.33 | |
| 11 |
| 17% | 0.17 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González Aguña, A.; Fernández Batalla, M.; Gonzalo de Diego, B.; Jiménez Rodríguez, M.L.; Martínez Muñoz, M.L.; Santamaría García, J.M. Care Recommendations for the Chronic Risk of COVID-19: Nursing Intervention for Behaviour Changes. Int. J. Environ. Res. Public Health 2022, 19, 8532. https://doi.org/10.3390/ijerph19148532
González Aguña A, Fernández Batalla M, Gonzalo de Diego B, Jiménez Rodríguez ML, Martínez Muñoz ML, Santamaría García JM. Care Recommendations for the Chronic Risk of COVID-19: Nursing Intervention for Behaviour Changes. International Journal of Environmental Research and Public Health. 2022; 19(14):8532. https://doi.org/10.3390/ijerph19148532
Chicago/Turabian StyleGonzález Aguña, Alexandra, Marta Fernández Batalla, Blanca Gonzalo de Diego, María Lourdes Jiménez Rodríguez, María Lourdes Martínez Muñoz, and José María Santamaría García. 2022. "Care Recommendations for the Chronic Risk of COVID-19: Nursing Intervention for Behaviour Changes" International Journal of Environmental Research and Public Health 19, no. 14: 8532. https://doi.org/10.3390/ijerph19148532
APA StyleGonzález Aguña, A., Fernández Batalla, M., Gonzalo de Diego, B., Jiménez Rodríguez, M. L., Martínez Muñoz, M. L., & Santamaría García, J. M. (2022). Care Recommendations for the Chronic Risk of COVID-19: Nursing Intervention for Behaviour Changes. International Journal of Environmental Research and Public Health, 19(14), 8532. https://doi.org/10.3390/ijerph19148532