Spatial Variations and Determinants of Anemia among Under-five Children in Nepal, DHS (2006–2016)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Data Source
2.3. Sampling Method and Sample Size
2.4. Outcome Variable
2.5. Explanatory Variables
2.6. Data Analysis
3. Results
3.1. Sociodemographics Chacterictics
3.2. Under-Five Children Charcteristics
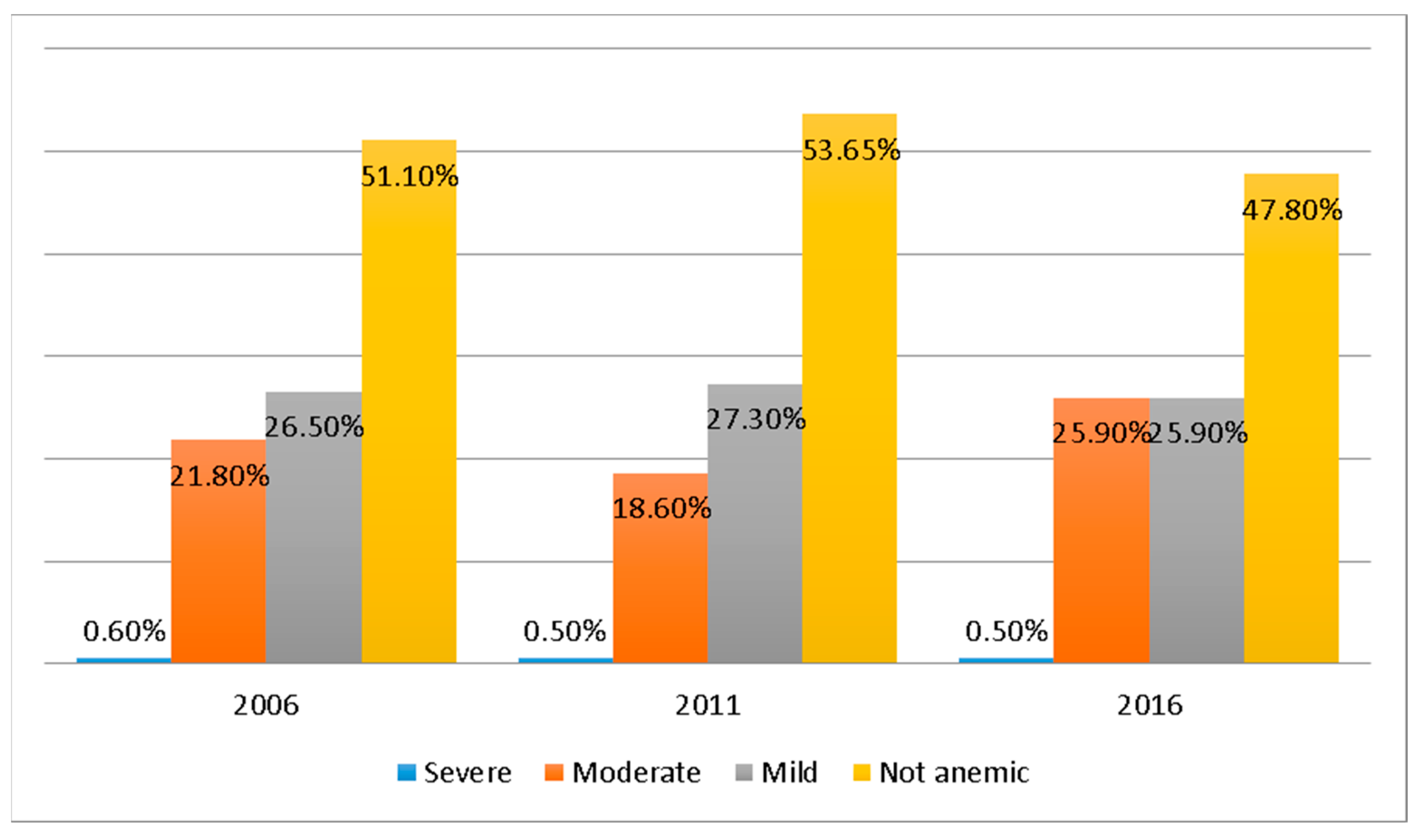
3.3. Prevalence of Anemia among Under-5 Children in Nepal
3.4. Spatial Variation of Anemia among Under-5 Children in Nepal
3.5. Determinants of Anemia among Under-5 Children
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vieth, J.T.; Lane, D.R. Anemia. Emerg. Med. Clin. N. Am. 2014, 32, 613–628. [Google Scholar] [CrossRef]
- Dangour, A.D.; Mace, G.; Shankar, B. Food Systems, Nutrition, Health and the Environment. Lancet Planet. Health 2017, 1, e8–e9. [Google Scholar] [CrossRef]
- Hay, S.I.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; et al. Global, Regional, and National Disability-Adjusted Life-Years (DALYs) for 333 Diseases and Injuries and Healthy Life Expectancy (HALE) for 195 Countries and Territories, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1260–1344. [Google Scholar] [CrossRef] [Green Version]
- Chan, M. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; World Health Organization: Geneva, Switzerland, 2011; pp. 1–6. [Google Scholar]
- Kassebaum, N.J.; GBD 2013 Anemia Collaborators. The Global Burden of Anemia. Hematol. Oncol. Clin. North Am. 2016, 30, 247–308. [Google Scholar] [CrossRef] [Green Version]
- WHO. Anaemia in Children <5 Years-Estimates by Country; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Kounnavong, S.; Sunahara, T.; Mascie-Taylor, C.G.; Hashizume, M.; Okumura, J.; Moji, K.; Boupha, B.; Yamamoto, T. Effect of daily versus weekly home fortification with multiple micronutrient powder on haemoglobin concentration of young children in a rural area, Lao People’s Democratic Republic: A randomised trial. Nutr. J. 2011, 10, 129. [Google Scholar] [CrossRef] [Green Version]
- Kejo, D.; Petrucka, P.M.; Martin, H.; Kimanya, M.E.; Mosha, T.C. Prevalence and predictors of anemia among children under 5 years of age in Arusha District, Tanzania. Pediatr. Health Med. Ther. 2018, 9, 9–15. [Google Scholar] [CrossRef] [Green Version]
- WHO. Anaemia. 2017. Available online: https://www.who.int/health-topics/anaemia#tab=tab_1 (accessed on 3 November 2021).
- Li, S.; Bo, Y.; Ren, H.; Zhou, C.; Lao, X.; Zhao, L.; Yu, D. Regional Differences in the Prevalence of Anaemia and Associated Risk Factors among Infants Aged 0–23 Months in China: China Nutrition and Health Surveillance. Nutrients 2021, 13, 1293. [Google Scholar] [CrossRef]
- Leung, A.K.; Chan, K.W. Iron deficiency anemia. Adv. Pediatr. 2001, 48, 385–408. [Google Scholar]
- Baranwal, A.; Baranwal, A.; Roy, N. Association of Household Environment and Prevalence of Anemia among Children Under-5 in India. Front. Public Health 2014, 2, 196. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Cheng, X.; Zhao, L.; Ren, H. Based on Chinese Nutrition and Health Surveillance Data. Nutrients 2021, 13, 3705. [Google Scholar] [CrossRef]
- Anteneh, Z.A.; Van Geertruyden, J.P. Spatial Variations and Determinants of Anemia among Under-Five Children in Ethiopia, EDHS 2005–2016. PLoS ONE 2021, 16, e0249412. [Google Scholar] [CrossRef] [PubMed]
- Chandyo, R.K.; Ulak, M.; Adhikari, R.K.; Sommerfelt, H.; Strand, T.A. Prevalence of Iron Deficiency and Anemia among Young Children with Acute Diarrhea in Bhaktapur, Nepal. Healthcare 2015, 3, 593–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harding, K.L.; Aguayo, V.M.; Namirembe, G.; Webb, P. Determinants of Anemia among Women and Children in Nepal and Pakistan: An Analysis of Recent National Survey Data. Matern. Child Nutr. 2018, 14, e12478. [Google Scholar] [CrossRef] [PubMed]
- Mainardi, S. Modelling spatial heterogeneity and anisotropy: Child anaemia, sanitation and basic infrastructure in sub-Saharan Africa. Int. J. Geogr. Inf. Sci. 2021, 26, 387–411. [Google Scholar] [CrossRef]
- Sunuwar, D.R.; Singh, D.R.; Adhikari, B.; Shrestha, S.; Pradhan, P.M.S. Factors Affecting Anaemia among Women of Reproductive Age in Nepal: A Multilevel and Spatial Analysis. BMJ Open 2021, 11, e041982. [Google Scholar] [CrossRef]
- MoFAlD. Ministry of Federal Affairs and Local Development Kathmandu Karnali Employment Programme Project Implementation Manual October 2014; MoFAlD: Kathmandu, Nepal, 2014. [Google Scholar]
- Rawal ID, L.B.; Kanda, K.; Alam Mahumud, R.; Joshi, D.I.; Mehata, S.; Shrestha, N.I.; Poudel, P.; Karki, S.; Renzaho, A. Prevalence of Underweight, Overweight and Obesity and Their Associated Risk Factors in Nepalese Adults: Data from a Nationwide Survey, 2016. PLoS ONE 2016, 13, e0205912. [Google Scholar] [CrossRef]
- Ministry of Health and Population (MOHP) [Nepal]. New ERA, M.I.I. Nepal Demographic and Health Survey 2016; Population Division Ministry of Health and Population Government of Nepal: Kathmandu, Nepal, 2016. [Google Scholar]
- Ministry of Health and Population (MOHP) [Nepal]. New ERA, M.I.I. Nepal Demographic and Health Survey 2011; Population Division Ministry of Health and Population Government of Nepal: Kathmandu, Nepal, 2011. [Google Scholar]
- Ministry of Health and Population (MOHP) [Nepal]. New ERA, M.I.I. Nepal Demographic And Health Survey 2006; Population Division Ministry of Health and Population Government of Nepal: Kathmandu, Nepal, 2006. [Google Scholar]
- Goheen, M.M.; Wegmüller, R.; Bah, A.; Darboe, B.; Danso, E.; Affara, M.; Gardner, D.; Patel, J.C.; Prentice, A.M.; Cerami, C. Anemia Offers Stronger Protection Than Sickle Cell Trait Against the Erythrocytic Stage of Falciparum Malaria and This Protection Is Reversed by Iron Supplementation. EBioMedicine 2016, 14, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.; Ferguson, R.M.; Corpuz, M.; Gartner, L.M. Maternal Age and Incidence of Low Birth Weight at Term: A Population Study. Am. J. Obstet. Gynecol. 1988, 158, 84–89. [Google Scholar] [CrossRef]
- Menon, M.P.; Yoon, S.S. Prevalence and Factors Associated with Anemia among Children under 5 Years of Age-Uganda, 2009. Am. J. Trop. Med. Hyg. 2015, 93, 521–526. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y. Mother’s Education and Child Health: Is There a Nurturing Effect? Mother’s Education and Child Health: Is There a Nurturing Effect? J. Health Econ. 2006, 28, 413–426. [Google Scholar] [CrossRef]
- dos Santos, R.F.; Gonzalez, E.S.C.; de Albuquerque, E.C.; de Arruda, I.K.G.; Diniz, A.D.S.; Figueroa, J.N.; Pereira, A.P.C. Prevalence of Anemia in under Five-Year-Old Children in a Children’s Hospital in Recife. Brazil. Rev. Bras. Hematol. Hemoter. 2011, 33, 100–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DHS. The DHS Program-Research Topics-Wealth Index. Available online: https://dhsprogram.com/topics/wealth-index/ (accessed on 2 April 2022).
- Moran, P.A.P. The Interpretation of Statistical Maps. J. R. Stat. Soc. Ser. B. 1948, 10, 243–251. [Google Scholar] [CrossRef]
- Ord, J.K.; Getis, A. Local Spatial Autocorrelation Statistics: Distributional Issues and an Application. Geogr. Anal. 1995, 27, 286–306. [Google Scholar] [CrossRef]
- ICF International. Percentage of Children under Age 5 Classified as Having Anemia. The DHS Program STAT Compiler. 2015. Available online: http://www.statcompiler.com (accessed on 3 May 2022).
- Chowdhury, M.R.K.; Khan, M.M.H.; Khan, H.T.A.; Rahman, M.S.; Islam, M.R.; Islam, M.M.; Billah, B. Prevalence and Risk Factors of Childhood Anemia in Nepal: A Multilevel Analysis. PLoS ONE 2020, 15, e0239409. [Google Scholar] [CrossRef] [PubMed]
- MOHP. National Anemia Control Strategy; MOHP: Kathmandu, Nepal, 2007. [Google Scholar]
- Government of Nepal; Ministry of Health and Population (MOHP). Nepal Health Sector Programme-2 Implementation PLAN; MOHP: Kathmandu, Nepal, 2010. [Google Scholar]
- Verma, V.; Le, T. An analysis of sampling errors for the Demographic Health Surveys. International statistical review. Rev. Int. Stat. 1996, 64, 265–294. [Google Scholar] [CrossRef]
- Shrestha, A.; Bhusal, C.K.; Shrestha, B.; Dev Bhattarai, K. Nutritional Status of Children and Its Associated Factors in Selected Earthquake-Affected VDCs of Gorkha District, Nepal Asmita. Int. J. Pediatr. 2020, 2020, 5849548. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.R.; Sunuwar, D.R.; Shah, S.K.; Sah, L.K.; Karki, K.; Sah, R.K. Food Insecurity during COVID-19 Pandemic: A Genuine Concern for People from Disadvantaged Community and Low-Income Families in Province 2 of Nepal. PLoS ONE 2021, 16, e0254954. [Google Scholar] [CrossRef]
- Awasthi, K.R.; Adefemi, K.; Awasthi, M.S.; Chalise, B. Public Health Interventions for Control of Malaria in the Population Living in the Terai Region of Nepal. J. Nepal Health Res. Counc. 2018, 15, 202–207. [Google Scholar] [CrossRef] [Green Version]
- Campbell, R.K.; Talegawkar, S.A.; Christian, P.; LeClerq, S.C.; Khatry, S.K.; Wu, L.S.; West, K.P., Jr. Seasonal Dietary Intakes and Socioeconomic Status among Women in the Terai of Nepal Rebecca. J. Health Popul. Nutr. 2014, 32, 198–216. [Google Scholar]
- Rijal, K.R.; Adhikari, B.; Ghimire, P.; Banjara, M.R.; Hanboonkunupakarn, B.; Imwong, M.; Chotivanich, K.; Ceintury, K.P.; Lal, B.K.; Thakur, G.; et al. Epidemiology of Plasmodium Vivax Malaria Infection in Nepal. Am. J. Trop. Med. Hyg. 2018, 99, 680–687. [Google Scholar] [CrossRef]
- Chandan Sapkota’s Blog: Poverty by District in Nepal. Available online: http://sapkotac.blogspot.com/2013/07/poverty-by-district-in-nepal.html (accessed on 14 February 2022).
- Adhikari, B.; Mishra, S.R.; Schwarz, R. Transforming Nepal’s Primary Health Care Delivery System in Global Health Era: Addressing Historical and Current Implementation Challenges. Glob. Health 2022, 18, 8. [Google Scholar] [CrossRef] [PubMed]
- Hong, R.; Banta, J.E.; Betancourt, J.A. Relationship between Household Wealth Inequality and Chronic Childhood Under-Nutrition in Bangladesh. Int. J. Equity Health. 2006, 5, 15. [Google Scholar] [CrossRef] [Green Version]
- Hong, R.; Mishra, V. Effect of Wealth Inequality on Chronic Under-Nutrition in Cambodian Children. J. Health Popul. Nutr. 2006, 24, 89–99. [Google Scholar]
- Habyarimana, F.; Zewotir, T.; Ramroop, S. Structured Additive Quantile Regression for Assessing the Determinants of Childhood Anemia in Rwanda. Int. J. Environ. Res. Public Health 2017, 14, 652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, J.R.; Awan, N.; Misu, F. Determinants of Anemia among 6–59 Months Aged Children in Bangladesh: Evidence from Nationally Representative Data. BMC Pediatr. 2016, 16, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Legason, I.D.; Atiku, A.; Ssenyonga, R.; Olupot-Olupot, P.; Barugahare, J.B. Prevalence of Anaemia and Associated Risk Factors among Children in North-Western Uganda: A Cross Sectional Study. BMC Hematol. 2017, 17, 10. [Google Scholar] [CrossRef] [Green Version]
- Wang, M. Iron Deficiency and Other Types of Anemia in Infants and Children. Am. Fam. Physician 2016, 93, 270–278. [Google Scholar]
- Chwang, L. Iron Supplementation and Physical Rural Indonesian Children. Am. J. Clin. Nutr. 2018, 13, 496–501. [Google Scholar] [CrossRef]
- Domellöf, M.; Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Fewtrell, M.; Hojsak, I.; Mihatsch, W.; Molgaard, C.; Shamir, R.; et al. Iron Requirements of Infants and Toddlers. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 119–129. [Google Scholar] [CrossRef]
- Camila, M.; Chaparro, P.S.S. Anemia Epidemiology, Pathophysiology, and Etiology in Low- and Middle-Income Countries. Ann. N.Y. Acad. Sci. 2019, 1450, 15–31. [Google Scholar] [CrossRef]
- Semba, R.D.; de Pee, S.; Ricks, M.O.; Sari, M.; Bloem, M.W. Diarrhea and Fever as Risk Factors for Anemia among Children under Age Five Living in Urban Slum Areas of Indonesia. Int. J. Infect. Dis. 2008, 12, 62–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viana, M.B. Anemia and Infection: A Complex Relationship. Rev. Bras. Hematol. Hemoter. 2011, 33, 90–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howard, C.T.; de Pee, S.; Sari, M.; Bloem, M.W.; Semba, R.D. Association of Diarrhea with Anemia among Children under Age Five Living in Rural Areas of Indonesia. J. Trop. Pediatr. 2007, 53, 238–244. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Frequency | Percentage |
|---|---|---|
| Mother’s Age | ||
| 15–24 | 3412 | 39.3 |
| 25–34 | 4156 | 47.9 |
| 35–44 | 1016 | 11.7 |
| Above 45 | 91 | 1.1 |
| Religion | ||
| Hindu | 7367 | 84.9 |
| Buddhist | 589 | 6.8 |
| Muslim | 478 | 5.5 |
| Others | 239 | 2.8 |
| Education level of mother | ||
| No | 4513 | 52.0 |
| Primary | 1612 | 18.6 |
| Secondary | 2078 | 24.0 |
| Higher | 472 | 5.4 |
| Education level of father | ||
| No | 2422 | 27.9 |
| Primary | 2663 | 30.7 |
| Secondary | 1691 | 19.5 |
| Higher | 1385 | 16.0 |
| Don’t know | 514 | 5.9 |
| Type of residence | ||
| Urban | 1824 | 21.0 |
| Rural | 6850 | 79.0 |
| Ethnicity | ||
| Brahmin/Chettri | 2715 | 31.3 |
| Janajati | 1674 | 19.2 |
| Terai others | 1065 | 12.3 |
| Dalit | 1047 | 12.1 |
| Muslim | 349 | 4.0 |
| Newar | 342 | 3.9 |
| Others | 1483 | 17.2 |
| Wealth Index | ||
| Poorest | 2142 | 24.7 |
| Poorer | 1869 | 21.5 |
| Middle | 1854 | 21.4 |
| Richer | 1598 | 18.4 |
| Richest | 1212 | 14.0 |
| No. of under-five children | ||
| 1 to 2 | 7417 | 85.5 |
| 3 and above | 1258 | 14.5 |
| No. of HH size | ||
| 2 to 4 | 2372 | 27.3 |
| 5 to 7 | 3968 | 45.7 |
| 8 and above | 2332 | 26.9 |
| Development Region | ||
| Eastern | 1944 | 22.4 |
| Central | 2848 | 32.8 |
| Western | 2019 | 23.3 |
| Mid-Western | 1014 | 11.7 |
| Far Western | 850 | 9.8 |
| Characteristics | Frequency | Percentage |
|---|---|---|
| Age in months | ||
| 6–11 | 900 | 10.4 |
| 12–23 | 1911 | 22.0 |
| 24–59 | 5864 | 67.6 |
| Sex | ||
| Male | 4443 | 51.1 |
| Female | 4242 | 48.9 |
| Child is twin | ||
| Yes | 75 | 0.9 |
| No | 8600 | 99.1 |
| Birth Size | ||
| Very small | 407 | 4.7 |
| Small | 1136 | 13.1 |
| Average | 5416 | 62.4 |
| Larger and very large | 1708 | 19.7 |
| Don’t know | 8 | 0.1 |
| Preceding birth interval | ||
| 24 months and less | 1448 | 16.7 |
| More than 24 months | 4404 | 50.8 |
| First birth | 2823 | 32.5 |
| Succeeding birth interval | ||
| Last birth | 880 | 75.8 |
| 24 months and less | 1217 | 10.1 |
| More than 24 months | 6578 | 45.0 |
| Underweight | ||
| No | 5559 | 64.1 |
| Yes | 3075 | 35.4 |
| Wasting | ||
| No | 7637 | 88.0 |
| Yes | 992 | 11.4 |
| Stunting | ||
| No | 4525 | 52.2 |
| Yes | 4104 | 47.3 |
| Fever Last 2 weeks | ||
| No | 7012 | 80.8 |
| Yes | 1661 | 19.2 |
| Diarrhea last 2 week | ||
| No | 7682 | 88.6 |
| Yes | 987 | 11.4 |
| Cough last 2 week | ||
| No | 6935 | 79.9 |
| Yes | 1738 | 20.0 |
| 2005 | 2011 | 2016 | |
|---|---|---|---|
| Moran’s Index | 0.170688 | 0.018449 | 0.157314 |
| Expected Index | −0.003861 | −0.003472 | −0.002618 |
| p | 0.0000 | 0.331 | 00000 |
| Z score | 5.18 | 0.7405 | 5.4444 |
| Characteristics | Odd Ratio | 95% CI | p Value |
|---|---|---|---|
| Mother’s age | |||
| 15–24 | 1.731 | 1.132–2.648 | <0.01 |
| 25–34 | 0.723 | 1.384–0.906 | |
| 35–44 | 0.299 | 1.261–0.814 | |
| 45 and above | 1 | 1 | |
| Mother’s Education | |||
| No education | 1.922 | 1.579–2.339 | <0.01 |
| Primary | 1.510 | 1.222–1.866 | |
| Secondary | 1.575 | 1.281–1.936 | |
| Higher | 1 | 1 | |
| Father’s education | |||
| No education | 1.370 | 1.200–1.565 | <0.01 |
| Primary | 1.238 | 1.087–1410 | |
| Secondary | 1.086 | 0.942–1.253 | |
| Higher | 1 | 1 | |
| Wealth index | <0.001 | ||
| Poorest | 1.333 | 1.160–1.533 | |
| Poorer | 1.532 | 1.323–1.774 | |
| Middle | 1.725 | 1.484–2.005 | |
| Richer | 1.481 | 1.272–1.726 | |
| Richest | 1 | 1 | |
| Household size | <0.01 | ||
| 2 to 4 | 0.767 | 0.685–0.860 | |
| 5 to 7 | 0.850 | 0.768–0.940 | |
| 8 and above | 1 | 1 | |
| No. of under-5 children | <0.01 | ||
| 1 to 2 | 0.774 | 0.689–0.869 | |
| 3 and more | 1 | 1 | |
| Age of child (in a month) | |||
| 6 to 11 | 5.327 | 4.538–6.253 | <0.001 |
| 12 to 23 | 3.462 | 3.107–3.857 | |
| 24 to 59 | 1 | 1 | |
| Child is twin | |||
| Yes | 1 | 1 | 0.022 |
| No | 0.588 | 0.383–0.934 | |
| Birth size | |||
| Large than average | 0.782 | 0.684–0.895 | <0.01 |
| Average | 0.542 | 0.866–1.0079 | |
| Small than average | 1 | 1 | |
| Stunting | |||
| Yes | 1.203 | 1.107–1.308 | <0.01 |
| No | 1 | 1 | |
| Underweight | |||
| Yes | 1.358 | 1.245–1.482 | <0.01 |
| No | 1 | 1 | |
| Wasting | |||
| Yes | 1.533 | 1.342–1.752 | <0.01 |
| No | 1 | 1 | |
| Had fever | |||
| Yes | 1 | 1 | <0.01 |
| No | 0.807 | 0.726–0.869 | |
| Had diarrhea | |||
| Yes | 1 | 1 | <0.01 |
| No | 0.686 | 0.601–0.783 | |
| Had Cough | |||
| Yes | 1 | 1 | <0.01 |
| No | 0.794 | 0.715–0.875 | |
| Year of survey | 0.001 | ||
| 2006 | 1 | 1 | |
| 2011 | 0.922 | 0.832–1.023 | |
| 2016 | 1.157 | 1.044–1.283 | |
| Preceding birth interval | |||
| First birth | 1 | 1 | 0.02 |
| 24 months and less | 1.213 | 1.049–1.266 | |
| More than 24 month | 1.152 | 1.070–1.3751 | |
| Succeeding birth interval | |||
| 24 and less | 0482 | 0.426–0.546 | <0.01 |
| More than 24 | 0.562 | 0.488–0.648 | |
| Last birth | 1 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, S.; Acharya, B.K.; Wu, Q. Spatial Variations and Determinants of Anemia among Under-five Children in Nepal, DHS (2006–2016). Int. J. Environ. Res. Public Health 2022, 19, 8664. https://doi.org/10.3390/ijerph19148664
Sharma S, Acharya BK, Wu Q. Spatial Variations and Determinants of Anemia among Under-five Children in Nepal, DHS (2006–2016). International Journal of Environmental Research and Public Health. 2022; 19(14):8664. https://doi.org/10.3390/ijerph19148664
Chicago/Turabian StyleSharma, Shristi, Bipin Kumar Acharya, and Qian Wu. 2022. "Spatial Variations and Determinants of Anemia among Under-five Children in Nepal, DHS (2006–2016)" International Journal of Environmental Research and Public Health 19, no. 14: 8664. https://doi.org/10.3390/ijerph19148664






