How Daily Obstacles Affect Frontline Healthcare Professionals’ Mental Health during Omicron: A Daily Diary Study of Handwashing Behavior
Abstract
1. Introduction
2. Theory and Hypotheses Development
2.1. Coping Theory
2.2. COVID-19 Phobia, Burnout, Work-Related Stress, and Mental Health
2.3. Mediating Role of Burnout and Work-Related Stress
2.4. Handwashing as a Moderator
3. Method
3.1. Sampling and Data Collection Procedures
3.2. Measurement Scale
3.2.1. COVID-19 Phobia Scale
3.2.2. Work Stress Questionnaire
3.2.3. Mental Health
3.2.4. Burnout
3.2.5. Handwashing Frequency
4. Results
4.1. Validation of Measurement Model
4.2. Hypothesis Testing
4.2.1. Mediating Effects of Burnout and Work-Related Stress
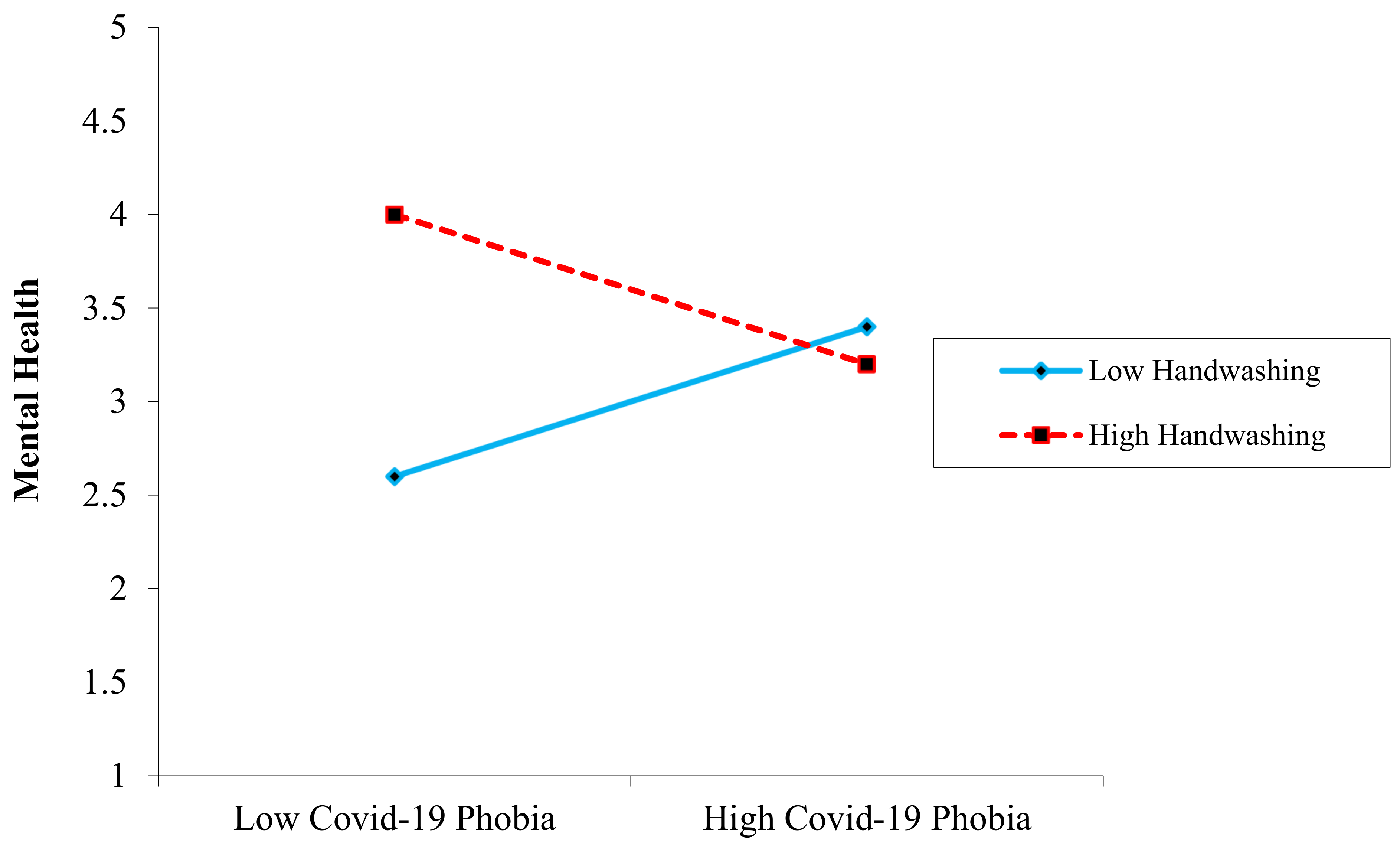
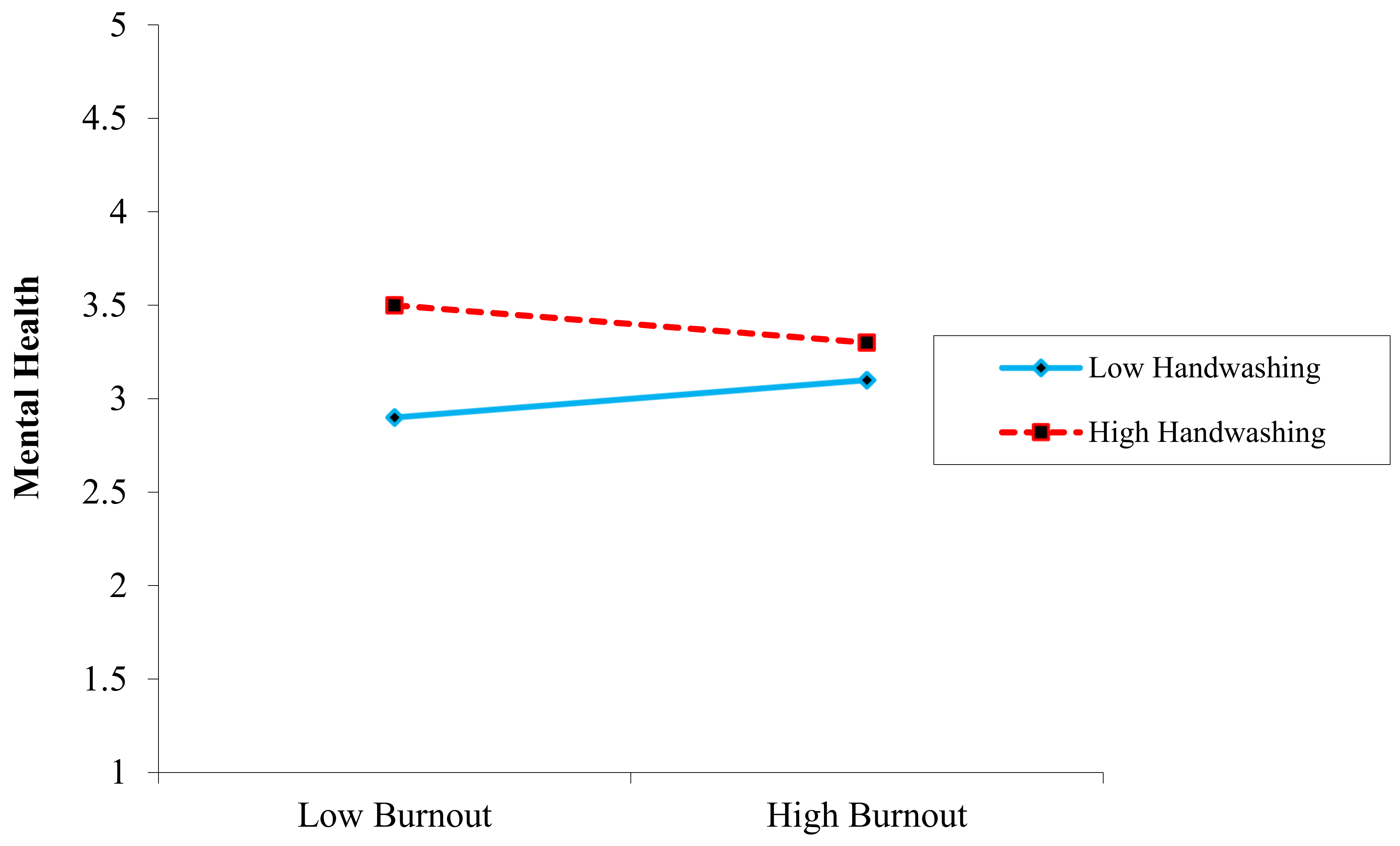
4.2.2. Moderating Effect of Handwashing
5. Discussion
5.1. Theoretical Contribution
5.2. Practical Implications
5.3. Limitations and Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Tiecco, G.; Storti, S.; Degli Antoni, M.; Focà, E.; Castelli, F.; Quiros-Roldan, E. Omicron genetic and clinical peculiarities that may overturn SARS-CoV-2 pandemic: A literature review. Int. J. Mol. Sci. 2022, 23, 1987. [Google Scholar] [CrossRef] [PubMed]
- Wiener, L.; Rosenberg, A.R.; Pennarola, B.; Fry, A.; Weaver, M. Navigating the terrain of moral distress: Experiences of pediatric end-of-life care and bereavement during COVID-19. Palliat. Supportive Care 2021, 19, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Transactional theory and research on emotions and coping. Eur. J. Personal. 1987, 1, 141–169. [Google Scholar] [CrossRef]
- Lazarus, R.S. Toward better research on stress and coping. Am. Psychol. 2000, 55, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Beaudry, A.; Pinsonneault, A. Understanding user responses to information technology: A coping model of user adaptation. MIS Q. 2005, 29, 493–524. [Google Scholar] [CrossRef]
- Roth, S.; Cohen, L.J. Approach, avoidance, and coping with stress. Am. Psychol. 1986, 41, 813. [Google Scholar] [CrossRef]
- Rector, N.A.; Roger, D. The stress buffering effects of self-esteem. Personal. Individ. Differ. 1997, 23, 799–808. [Google Scholar] [CrossRef]
- Honarvar, B.; Lankarani, K.B.; Kharmandar, A.; Shaygani, F.; Zahedroozgar, M.; Rahmanian Haghighi, M.R.; Ghahramani, S.; Honarvar, H.; Daryabadi, M.M.; Salavati, Z.; et al. Knowledge, attitudes, risk perceptions, and practices of adults toward COVID-19: A population and field-based study from Iran. Int. J. Public Health 2020, 65, 731–739. [Google Scholar] [CrossRef]
- Polanin, J.R.; Espelage, D.L.; Grotpeter, J.K.; Spinney, E.; Ingram, K.M.; Valido, A.; El Sheikh, A.; Torgal, C.; Robinson, L. A meta-analysis of longitudinal partial correlations between school violence and mental health, school performance, and criminal or delinquent acts. Psychol. Bull. 2021, 147, 115–133. [Google Scholar] [CrossRef]
- Zellars, K.L. Social anxiety: An overlooked variable in the organizational stress literature. In Exploring the Work and Non-Work Interface; Emerald Group Publishing Limited: London, UK, 2007. [Google Scholar]
- Davidson, J. Contesting stigma and contested emotions: Personal experience and public perception of specific phobias. Soc. Sci. Med. 2005, 61, 2155–2164. [Google Scholar] [CrossRef]
- Parsons, T.D.; Rizzo, A.A. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: A meta-analysis. J. Behav. Ther. Exp. Psychiatry 2008, 39, 250–261. [Google Scholar] [CrossRef] [PubMed]
- Garaigordobil, M. Predictor variables of happiness and its connection with risk and protective factors for health. Front. Psychol. 2015, 6, 1176. [Google Scholar] [CrossRef][Green Version]
- Van Houtem, C.M.; Aartman, I.H.; Boomsma, D.I.; Ligthart, L.; Visscher, C.M.; De Jongh, A. Is dental phobia a blood-injection-injury phobia? Depress. Anxiety 2014, 31, 1026–1034. [Google Scholar] [CrossRef]
- Wang, Y. Government policies, national culture and social distancing during the first wave of the COVID-19 pandemic: International evidence. Saf. Sci. 2021, 135, 105138. [Google Scholar] [CrossRef]
- Shi, H.; Li, X.; Yang, Z.; Li, T.; Ren, Y.; Liu, T.; Yang, N.; Zhang, H.; Chen, G.; Liang, X. Tourism land use simulation for regional tourism planning using POIs and cellular automata. Trans. GIS 2020, 24, 1119–1138. [Google Scholar] [CrossRef]
- Bozkurt, A.; Sharma, R.C. Emergency remote teaching in a time of global crisis due to CoronaVirus pandemic. Asian J. Distance Educ. 2020, 15, i–vi. [Google Scholar]
- Wanberg, C.R.; Csillag, B.; Douglass, R.P.; Zhou, L.; Pollard, M.S. Socioeconomic status and well-being during COVID-19: A resource-based examination. J. Appl. Psychol. 2020, 105, 1382. [Google Scholar] [CrossRef]
- Koniak, P.; Cwalina, W. Fear of coronavirus and forbid/allow asymmetry as determinants of acceptance of COVID-19 pandemic related restrictions and persistence of attitudes towards these regulations. Soc. Psychol. Bull. 2020, 15, 1–3. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Asmundson, G.J.; Taylor, S. Coronaphobia: Fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020, 70, 102196. [Google Scholar] [CrossRef]
- Arpaci, I.; Karataş, K.; Baloğlu, M. The development and initial tests for the psychometric properties of the COVID-19 Phobia Scale (C19P-S). Personal. Individ. Differ. 2020, 164, 110108. [Google Scholar] [CrossRef] [PubMed]
- Lindinger-Sternart, S.; Kaur, V.; Widyaningsih, Y.; Patel, A.K. COVID-19 phobia across the world: Impact of resilience on COVID-19 phobia in different nations. Couns. Psychother. Res. 2021, 21, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Nagy, G.A.; Fang, C.M.; Hish, A.J.; Kelly, L.; Nicchitta, C.V.; Dzirasa, K.; Rosenthal, M.Z. Burnout and mental health problems in biomedical doctoral students. CBE—Life Sci. Educ. 2019, 18, ar27. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Falcó-Pegueroles, A.; Rosa, D.; Tolotti, A.; Graffigna, G.; Bonetti, L. The psychosocial impact of flu influenza pandemics on healthcare workers and lessons learnt for the COVID-19 emergency: A rapid review. Int. J. Public Health 2020, 65, 1205–1216. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, J.; Luo, C.; Hu, S.; Lin, X.; Anderson, A.E.; Bruera, E.; Yang, X.; Wei, S.; Qian, Y. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J. Pain Symptom Manag. 2020, 60, e60–e65. [Google Scholar] [CrossRef] [PubMed]
- Watkins, L.L.; Blumenthal, J.A.; Babyak, M.A.; Davidson, J.R.; McCants, C.B., Jr.; O’Connor, C.; Sketch, M.H., Jr. Phobic anxiety and increased risk of mortality in coronary heart disease. Psychosom. Med. 2010, 72, 664. [Google Scholar] [CrossRef]
- Rapp, D.J.; Hughey, J.M.; Kreiner, G.E. Boundary work as a buffer against burnout: Evidence from healthcare workers during the COVID-19 pandemic. J. Appl. Psychol. 2021, 106, 1169. [Google Scholar] [CrossRef]
- Zheng, L.; Wang, X.; Zhou, C.; Liu, Q.; Li, S.; Sun, Q.; Wang, M.; Zhou, Q.; Wang, W. Analysis of the infection status of healthcare workers in Wuhan during the COVID-19 outbreak: A cross-sectional study. Clin. Infect. Dis. 2020, 71, 2109–2113. [Google Scholar] [CrossRef]
- Caldas, M.P.; Ostermeier, K.; Cooper, D. When helping hurts: COVID-19 critical incident involvement and resource depletion in health care workers. J. Appl. Psychol. 2021, 106, 29. [Google Scholar] [CrossRef]
- Yoneyama, S. Student discourse on Tokokyohi (School Phobia/Refusal) in Japan: Burnout or empowerment? Br. J. Sociol. Educ. 2000, 21, 77–94. [Google Scholar] [CrossRef]
- Peres, M.F.; Mercante, J.P.; Guendler, V.Z.; Corchs, F.; Bernik, M.A.; Zukerman, E.; Silberstein, S.D. Cephalalgiaphobia: A possible specific phobia of illness. J. Headache Pain 2007, 8, 56–59. [Google Scholar] [CrossRef] [PubMed]
- Ogińska-Bulik, N.; Michalska, P. Psychological resilience and secondary traumatic stress in nurses working with terminally ill patients—The mediating role of job burnout. Psychol. Serv. 2020, 18, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Turel, O. Quitting the use of a habituated hedonic information system: A theoretical model and empirical examination of Facebook users. Eur. J. Inf. Syst. 2015, 24, 431–446. [Google Scholar] [CrossRef]
- Manzoni, P.; Eisner, M. Violence between the police and the public: Influences of work-related stress, job satisfaction, burnout, and situational factors. Crim. Justice Behav. 2006, 33, 613–645. [Google Scholar] [CrossRef]
- Almén, N. A cognitive behavioral model Proposing that clinical burnout may maintain itself. Int. J. Environ. Res. Public Health 2021, 18, 3446. [Google Scholar] [CrossRef]
- Griffiths, P.; Ball, J.; Drennan, J.; Dall’Ora, C.; Jones, J.; Maruotti, A.; Pope, C.; Saucedo, A.R.; Simon, M. Nurse staffing and patient outcomes: Strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for Health and Care Excellence Safe Staffing guideline development. Int. J. Nurs. Stud. 2016, 63, 213–225. [Google Scholar]
- Langelaan, S.; Bakker, A.B.; Van Doornen, L.J.; Schaufeli, W.B. Burnout and work engagement: Do individual differences make a difference? Personal. Individ. Differ. 2006, 40, 521–532. [Google Scholar] [CrossRef]
- Bianchi, R.; Truchot, D.; Laurent, E.; Brisson, R.; Schonfeld, I.S. Is burnout solely job-related? A critical comment. Scand. J. Psychol. 2014, 55, 357–361. [Google Scholar] [CrossRef]
- Morse, G.; Salyers, M.P.; Rollins, A.L.; Monroe-DeVita, M.; Pfahler, C. Burnout in mental health services: A review of the problem and its remediation. Adm. Policy Ment. Health Ment. Health Serv. Res. 2012, 39, 341–352. [Google Scholar] [CrossRef]
- Awa, W.L.; Plaumann, M.; Walter, U. Burnout prevention: A review of intervention programs. Patient Educ. Couns. 2010, 78, 184–190. [Google Scholar] [CrossRef]
- Cummings, G.G.; MacGregor, T.; Davey, M.; Lee, H.; Wong, C.A.; Lo, E.; Muise, M.; Stafford, E. Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int. J. Nurs. Stud. 2010, 47, 363–385. [Google Scholar] [CrossRef]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in nursing: A theoretical review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Cummings, G.G.; Tate, K.; Lee, S.; Wong, C.A.; Paananen, T.; Micaroni, S.P.; Chatterjee, G.E. Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int. J. Nurs. Stud. 2018, 85, 19–60. [Google Scholar] [CrossRef] [PubMed]
- Smida, M.; Khoodoruth, M.A.; Al-Nuaimi, S.K.; Al-Salihy, Z.; Ghaffar, A.; Khoodoruth, W.N.; Mohammed, M.F.; Ouanes, S. Coping strategies, optimism, and resilience factors associated with mental health outcomes among medical residents exposed to coronavirus disease. Brain Behav. 2019, 11, e2320. [Google Scholar]
- Serrão, C.; Duarte, I.; Castro, L.; Teixeira, A. Burnout and depression in portuguese healthcare workers during the COVID-19 pandemic—The mediating role of psychological resilience. Int. J. Environ. Res. Public Health 2021, 18, 636. [Google Scholar] [CrossRef]
- Zhou, J.; Yang, Y.; Qiu, X.; Yang, X.; Pan, H.; Ban, B.; Qiao, Z.; Wang, L.; Wang, W. Serial multiple mediation of organizational commitment and job burnout in the relationship between psychological capital and anxiety in Chinese female nurses: A cross-sectional questionnaire survey. Int. J. Nurs. Stud. 2018, 83, 75–82. [Google Scholar] [CrossRef]
- Zhang, H.; Ye, Z.; Tang, L.; Zou, P.; Du, C.; Shao, J.; Wang, X.; Chen, D.; Qiao, G.; Mu, S.Y. Anxiety symptoms and burnout among Chinese medical staff of intensive care unit: The moderating effect of social support. BMC Psychiatry 2020, 20, 197. [Google Scholar] [CrossRef]
- Chong, S.; Huang, Y.; Chang, C.H. Supporting interdependent telework employees: A moderated-mediation model linking daily COVID-19 task setbacks to next-day work withdrawal. J. Appl. Psychol. 2020, 105, 1408. [Google Scholar] [CrossRef]
- Torrès, O.; Benzari, A.; Fisch, C.; Mukerjee, J.; Swalhi, A.; Thurik, R. Risk of burnout in French entrepreneurs during the COVID-19 crisis. Small Bus. Econ. 2022, 58, 717–739. [Google Scholar] [CrossRef]
- De Clercq, D.; Haq, I.U.; Azeem, M.U. Time-related work stress and counterproductive work behavior: Invigorating roles of deviant personality traits. Pers. Review. 2019, 48, 1756–1781. [Google Scholar] [CrossRef]
- Skinner, N.; Pocock, B. Work—life conflict: Is work time or work overload more important? Asia Pac. J. Hum. Resour. 2008, 46, 303–315. [Google Scholar] [CrossRef]
- Parasuraman, S.; Greenhaus, J.H. Toward reducing some critical gaps in work–family research. Hum. Resour. Manag. Rev. 2002, 12, 299–312. [Google Scholar] [CrossRef]
- Haddon, J. The impact of employees’ well-being on performance in the workplace. Strateg. HR Rev. 2018, 17, 72–75. [Google Scholar] [CrossRef]
- He, Q.; Li, T.; Su, Y.; Luan, Y. Instructive messages and lessons from Chinese countermarching nurses of caring for COVID-19 patients: A qualitative study. J. Transcult. Nurs. 2021, 32, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Probst, T.M.; Lee, H.J.; Bazzoli, A. Economic stressors and the enactment of CDC-recommended COVID-19 prevention behaviors: The impact of state-level context. J. Appl. Psychol. 2020, 105, 1397. [Google Scholar] [CrossRef] [PubMed]
- Araujo, C.; Siqueira, M.; Amaral, L. Resilience of Brazilian health-care professionals during the pandemic. Int. J. Qual. Serv. Sci. 2022. [Google Scholar] [CrossRef]
- Jamal, M.T.; Anwar, I.; Khan, N.A.; Saleem, I. Work during COVID-19: Assessing the influence of job demands and resources on practical and psychological outcomes for employees. Asia-Pac. J. Bus. Adm. 2021; ahead-of-print. [Google Scholar] [CrossRef]
- Hamouche, S. COVID-19 and employees’ mental health: Stressors, moderators and agenda for organizational actions. Emerald Open Res. 2020, 2, 15. [Google Scholar] [CrossRef]
- Xue, Y.; Hassan, S.; Bahader, S.; Habib, S. Investigating the Impact of Fear Related to COVID-19 Disease on Situational Humor via Social Networking Sites. Front. Psychol. 2021, 12, 721304. [Google Scholar] [CrossRef]
- Viotti, S. Work-related stress among correctional officers: A qualitative study. Work 2016, 53, 871–884. [Google Scholar] [CrossRef]
- Alenezi, A.M.; Aboshaiqah, A.; Baker, O. Work-related stress among nursing staff working in government hospitals and primary health care centres. Int. J. Nurs. Pract. 2018, 24, e12676. [Google Scholar] [CrossRef] [PubMed]
- Harb, A.; Rayan, A.; Al Khashashneh, O.Z. The relationship between workplace bullying and positive mental health among registered nurses. J. Am. Psychiatr. Nurses Assoc. 2021, 27, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Hobfoll, S.E.; Wells, J.D. Conservation of resources, stress, and aging. In Handbook of Aging and Mental Health; Springer: Boston, MA, USA, 1998; pp. 121–134. [Google Scholar]
- Lee, R.S.; McGrath, P. Dealing with time pressure. Int. J. Stress Manag. 1995, 2, 79–86. [Google Scholar] [CrossRef]
- Aldwin, C.M.; Revenson, T.A. Does coping help? A reexamination of the relation between coping and mental health. J. Personal. Soc. Psychol. 1987, 53, 337. [Google Scholar] [CrossRef]
- World Health Organization. Operational Considerations for COVID-19 Management in the Accommodation Sector: Interim Guidance, 31 March 2020; World Health Organization: Geneva, Switzerland, 2020.
- Trougakos, J.P.; Chawla, N.; McCarthy, J.M. Working in a pandemic: Exploring the impact of COVID-19 health anxiety on work, family, and health outcomes. J. Appl. Psychol. 2020, 105, 1234. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy conception of anxiety. Anxiety Res. 1988, 1, 77–98. [Google Scholar] [CrossRef]
- Fiske, A.P.; Haslam, N. Social cognition is thinking about relationships. Curr. Dir. Psychol. Sci. 1996, 5, 143–148. [Google Scholar] [CrossRef]
- Spector, P.E. Perceived control by employees: A meta-analysis of studies concerning autonomy and participation at work. Hum. Relat. 1986, 39, 1005–1016. [Google Scholar] [CrossRef]
- Trakulpipat, C.; Wiwattanapantuwong, J.; Dhammapeera, P.; Tuicomepee, A. “Macbeth Effect”: The link between physical cleanliness and moral judgement. Kasetsart J. Soc. Sci. 2021, 42, 779–786. [Google Scholar]
- Giardini, F.; Vilone, D.; Sánchez, A.; Antonioni, A. Gossip and competitive altruism support cooperation in a Public Good game. Philos. Trans. R. Soc. B 2021, 376, 20200303. [Google Scholar] [CrossRef]
- Frantz, A.; Holmgren, K. The work stress questionnaire (WSQ)–reliability and face validity among male workers. BMC Public Health 2019, 19, 1580. [Google Scholar] [CrossRef] [PubMed]
- Lukat, J.; Margraf, J.; Lutz, R.; van der Veld, W.M.; Becker, E.S. Psychometric properties of the positive mental health scale (PMH-scale). BMC Psychol. 2016, 4, 8. [Google Scholar] [CrossRef] [PubMed]
- Malach-Pines, A. The burnout measure, short version. Int. J. Stress Manag. 2005, 12, 78. [Google Scholar] [CrossRef]
- Peterson, R.A.; Kim, Y. On the relationship between coefficient alpha and composite reliability. J. Appl. Psychol. 2013, 98, 194. [Google Scholar] [CrossRef]
- Meade, A.W.; Johnson, E.C.; Braddy, P.W. Power and sensitivity of alternative fit indices in tests of measurement invariance. J. Appl. Psychol. 2008, 93, 568. [Google Scholar] [CrossRef]
- Shiu, E.; Pervan, S.J.; Bove, L.L.; Beatty, S.E. Reflections on discriminant validity: Reexamining the Bove et al.(2009) findings. J. Bus. Res. 2011, 64, 497–500. [Google Scholar] [CrossRef]
- Jordan, P.J.; Troth, A.C. Common method bias in applied settings: The dilemma of researching in organizations. Aust. J. Manag. 2020, 45, 3–14. [Google Scholar] [CrossRef]
- Tennant, A.; Pallant, J.F. The root mean square error of approximation (RMSEA) as a supplementary statistic to determine fit to the Rasch model with large sample sizes. Rasch Meas Trans 2012, 25, 1348. [Google Scholar]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281. [Google Scholar] [CrossRef]
- Videbeck, S.L. Psychiatric-Mental Health Nursing; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010. [Google Scholar]
- Choi, H.Y.; Ha, J.H. Psychoanalytic Perspectives of Social Phobia: Based on Dazai Osamu’s Novel ‘Human Lost’. Psychoanalysis 2021, 32, 41–51. [Google Scholar] [CrossRef]
- Restauri, N.; Sheridan, A.D. Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: Intersection, impact, and interventions. J. Am. Coll. Radiol. 2020, 17, 921–926. [Google Scholar] [CrossRef] [PubMed]
- Luceño-Moreno, L.; Talavera-Velasco, B.; García-Albuerne, Y.; Martín-García, J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5514. [Google Scholar] [CrossRef] [PubMed]
- Duarte, I.; Teixeira, A.; Castro, L.; Marina, S.; Ribeiro, C.; Jácome, C.; Martins, V.; Ribeiro-Vaz, I.; Pinheiro, H.C.; Silva, A.R.; et al. Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health 2020, 20, 1885. [Google Scholar] [CrossRef] [PubMed]
- Noble, L.J.; Gonzalez, I.J.; Meruva, V.B.; Callahan, K.A.; Belfort, B.D.; Ramanathan, K.R.; Meyers, E.; Kilgard, M.P.; Rennaker, R.L.; McIntyre, C. Effects of vagus nerve stimulation on extinction of conditioned fear and post-traumatic stress disorder symptoms in rats. Transl. Psychiatry 2017, 7, e1217. [Google Scholar] [CrossRef] [PubMed]
- Portoghese, I.; Galletta, M.; Leiter, M.P.; Cocco, P.; D’Aloja, E.; Campagna, M. Fear of future violence at work and job burnout: A diary study on the role of psychological violence and job control. Burn. Res. 2017, 7, 36–46. [Google Scholar] [CrossRef]
- Vignoli, M.; Muschalla, B.; Mariani, M.G. Workplace phobic anxiety as a mental health phenomenon in the job demands-resources model. BioMed Res. Int. 2017, 2017, 3285092. [Google Scholar] [CrossRef]
- Obeid, S.; Lahoud, N.; Haddad, C.; Sacre, H.; Fares, K.; Akel, M.; Salameh, P.; Hallit, S. Factors associated with anxiety among the Lebanese population: The role of alexithymia, self-esteem, alcohol use disorders, emotional intelligence and stress and burnout. Int. J. Psychiatry Clin. Pract. 2020, 24, 151–162. [Google Scholar] [CrossRef]
- Clark, D.M.; Loxton, N.J. Fear, psychological acceptance, job demands and employee work engagement: An integrative moderated meditation model. Personal. Individ. Differ. 2012, 52, 893–897. [Google Scholar] [CrossRef]
- Washburn, D. Theory of Mind Decoding and Reasoning Abilities in Depression, Social Phobia, and Comorbid Conditions; Queen’s University: Kingston, ON, Canada, 2012. [Google Scholar]
- Gerber, M.; Lang, C.; Feldmeth, A.K.; Elliot, C.; Brand, S.; Holsboer-Trachsler, E.; Pühse, U. Burnout and mental health in Swiss vocational students: The moderating role of physical activity. J. Res. Adolesc. 2015, 25, 63–74. [Google Scholar] [CrossRef]
- Lindwall, M.; Ljung, T.; Hadžibajramović, E.; Jonsdottir, I.H. Self-reported physical activity and aerobic fitness are differently related to mental health. Ment. Health Phys. Act. 2012, 5, 28–34. [Google Scholar] [CrossRef]
- Montano, D.; Reeske, A.; Franke, F.; Hüffmeier, J. Leadership, followers’ mental health and job performance in organizations: A comprehensive meta-analysis from an occupational health perspective. J. Organ. Behav. 2017, 38, 327–350. [Google Scholar] [CrossRef]
- Galbraith, C.S.; Merrill, G.B. Academic and work-related burnout: A longitudinal study of working undergraduate university business students. J. Coll. Stud. Dev. 2012, 53, 453–463. [Google Scholar] [CrossRef]
- Rudolph, C.W.; Allan, B.; Clark, M.; Hertel, G.; Hirschi, A.; Kunze, F.; Shockley, K.; Shoss, M.; Sonnentag, S.; Zacher, H. Pandemics: Implications for research and practice in industrial and organizational psychology. Ind. Organ. Psychol. 2021, 14, 1–35. [Google Scholar] [CrossRef]
- Shockley, K.M.; Gabriel, A.S.; Robertson, D.; Rosen, C.C.; Chawla, N.; Ganster, M.L.; Ezerins, M.E. The fatiguing effects of camera use in virtual meetings: A within-person field experiment. J. Appl. Psychol. 2021, 106, 1137. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; De los Santos, J.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Khattak, S.; Khan, M.; Usman, T.; Ali, J.; Wu, D.X.; Jahangir, M.; Haleem, K.; Muhammad, P.; Rauf, M.A.; Saddique, K.; et al. Assessment of General Populations Knowledge, Attitude, and Perceptions Toward the Coronavirus Disease (COVID-19): A Cross-Sectional Study From Pakistan. Front. Med. 2021, 8, 747819. [Google Scholar] [CrossRef]
- Yip, P.S.; Chau, P.H. Physical distancing and emotional closeness amidst COVID-19. Crisis 2020, 41, 153–155. [Google Scholar] [CrossRef] [PubMed]
- Khattak, S.; Faheem, M.; Nawaz, B.; Khan, M.; Khan, N.H.; Ullah, N.; Khan, T.A.; Khan, R.U.; Haleem, K.S.; Ren, Z.G.; et al. Knowledge, Attitude, and Perception of Cancer Patients towards COVID-19 in Pakistan: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 7926. [Google Scholar] [CrossRef]

| Variables | Day 1 M (SD) | Day 2 M (SD) | Day 3 M (SD) | Day 4 M (SD) | Day 5 M (SD) | Day 6 M (SD) | Day 7 M (SD) | Day 8 M (SD) | Day 9 M (SD) | Day 10 M (SD) |
|---|---|---|---|---|---|---|---|---|---|---|
| C-19P | 19.81 (2.11) | 19.17 (2.71) | 19.19 (2.69) | 19.72 (2.33) | 19.49 (2.43) | 19.36 (2.60) | 19.12 (2.86) | 19.31 (2.58) | 19.87 (2.11) | 19.27 (2.37) |
| Burnout | 18.23 (2.67) | 18.92 (2.07) | 18.57 (2.41) | 18.18 (2.81) | 18.84 (2.14) | 18.49 (2.51) | 18.58 (2.35) | 18.18 (2.79) | 18.57 (2.42) | 18.90 (2.09) |
| MH | 4.38 (1.61) | 4.64 (1.35) | 4.58 (1.39) | 4.63 (1.32) | 4.40 (1.57) | 4.71 (1.28) | 4.17 (1.81) | 4.30 (1.68) | 4.09 (1.92) | 4.23 (1.63) |
| WRS | 19.46 (2.51) | 19.09 (2.90) | 19.32 (2.67) | 19.81 (2.66) | 19.71 (2.29) | 19.26 (2.68) | 19.64 (2.38) | 19.10 (2.82) | 19.28 (2.68) | 19.42 (2.49) |
| HW | 1.21 (1.80) | 1.61 (1.29) | 0.89 (1.02) | 1.88 (0.98) | 1.72 (1.34) | 1.41 (1.52) | 0.96 (1.89) | 1.18 (1.72) | 1.80 (1.18) | 0.88 (1.92) |
| Variables | N | Percentage | Variables | N | Percentage |
|---|---|---|---|---|---|
| Gender | Nature of Job | ||||
| Male | 41 | 51.9 | Radiologist | 18 | 22.8 |
| Female | 38 | 48.1 | Pharmacist | 14 | 17.7 |
| Age | Cardiologist | 12 | 15.2 | ||
| Young adult | 46 | 58.2 | Oncologist | 11 | 13.9 |
| Middle adult | 21 | 26.6 | Nurses | 24 | 30.4 |
| Older adult | 12 | 15.2 | Marital status | ||
| Job experience | Single | 44 | 55.7 | ||
| 1–5 years | 13 | 16.5 | Married | 35 | 44.3 |
| 6–10 years | 28 | 35.4 | Family status | ||
| 11–15 years | 28 | 35.4 | Higher | 42 | 53.2 |
| 16–20 years | 10 | 12.7 | Lower | 37 | 46.8 |
| Constructs | F. L | Cronbach α | C. R | AVE |
|---|---|---|---|---|
| C-19P | 0.842–0.939 | 0.89 | 0.87 | 0.71 |
| Burnout | 0.823–0.886 | 0.93 | 0.91 | 0.88 |
| Mental Health | 0.916–0.626 | 0.83 | 0.81 | 0.68 |
| WRS | 0.769–0.857 | 0.90 | 0.91 | 0.85 |
| Handwashing | 0.937–0.959 | 0.91 | 0.89 | 0.87 |
| Variables | Within-Person Variance (e2) | Between-Person Variance (r2) | % of the Within-Person Variance | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|---|
| C-19P | 0.61 | 0.38 | 61.81 | (0.79) | ||||
| Burnout | 0.84 | 0.97 | 44.71 | 0.88 ** | (0.93) | |||
| Mental Health | 3.80 | 3.05 | 67.52 | −0.63 ** | −0.53 ** | (0.89) | ||
| WRS | 2.97 | 2.99 | 59.83 | 0.96 ** | 0.91 ** | −0.60 ** | (0.91) | |
| Handwashing | 0.39 | 0.62 | 58.92 | 0.32 | 0.82 | 27 ** | 0.19 | (0.87) |
| M | 55.82 | 66.26 | 81.71 | 80.02 | 26.02 | |||
| SD | 8.72 | 7.71 | 9.15 | 9.04 | 1.04 |
| Direct and Indirect Effects of COVID-19 Phobia on Mental Health through Burnout and Work-Related Stress | β | LLCI | ULCI | ||
|---|---|---|---|---|---|
| C-19P | Mental Health | −0.53 *** | 0.67 | 0.28 | |
| C-19P | Burnout | Mental Health | −0.45 ** | 0.53 | 0.32 |
| C-19P | Mental Health | −0.40 *** | 0.43 | 0.17 | |
| C-19P | WRS | Mental health | −0.29 ** | 0.36 | 0.15 |
| Variables | B | SE | t | p | R2/Sig. |
|---|---|---|---|---|---|
| HW × C-19P on Mental health | −0.34 | 0.053 | 5.71 | 0.01 | 0.06 ** |
| HW × WRS on Mental health | 0.032 | 0.028 | 0.921 | 0.06 | 0.05 ns |
| HW × Burnout on Mental health | −0.13 | 0.071 | 3.82 | 0.01 | 0.08 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, N.H.; Hassan, S.; Bahader, S.; Fatima, S.; Zaidi, S.M.I.H.; Virk, R.; Jiang, K.; Jiang, E. How Daily Obstacles Affect Frontline Healthcare Professionals’ Mental Health during Omicron: A Daily Diary Study of Handwashing Behavior. Int. J. Environ. Res. Public Health 2022, 19, 8748. https://doi.org/10.3390/ijerph19148748
Khan NH, Hassan S, Bahader S, Fatima S, Zaidi SMIH, Virk R, Jiang K, Jiang E. How Daily Obstacles Affect Frontline Healthcare Professionals’ Mental Health during Omicron: A Daily Diary Study of Handwashing Behavior. International Journal of Environmental Research and Public Health. 2022; 19(14):8748. https://doi.org/10.3390/ijerph19148748
Chicago/Turabian StyleKhan, Nazeer Hussain, Sajid Hassan, Sher Bahader, Sidra Fatima, Syed Muhammad Imran Haider Zaidi, Razia Virk, Kexin Jiang, and Enshe Jiang. 2022. "How Daily Obstacles Affect Frontline Healthcare Professionals’ Mental Health during Omicron: A Daily Diary Study of Handwashing Behavior" International Journal of Environmental Research and Public Health 19, no. 14: 8748. https://doi.org/10.3390/ijerph19148748
APA StyleKhan, N. H., Hassan, S., Bahader, S., Fatima, S., Zaidi, S. M. I. H., Virk, R., Jiang, K., & Jiang, E. (2022). How Daily Obstacles Affect Frontline Healthcare Professionals’ Mental Health during Omicron: A Daily Diary Study of Handwashing Behavior. International Journal of Environmental Research and Public Health, 19(14), 8748. https://doi.org/10.3390/ijerph19148748







