Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall
Abstract
:1. Introduction
2. Materials and Methods
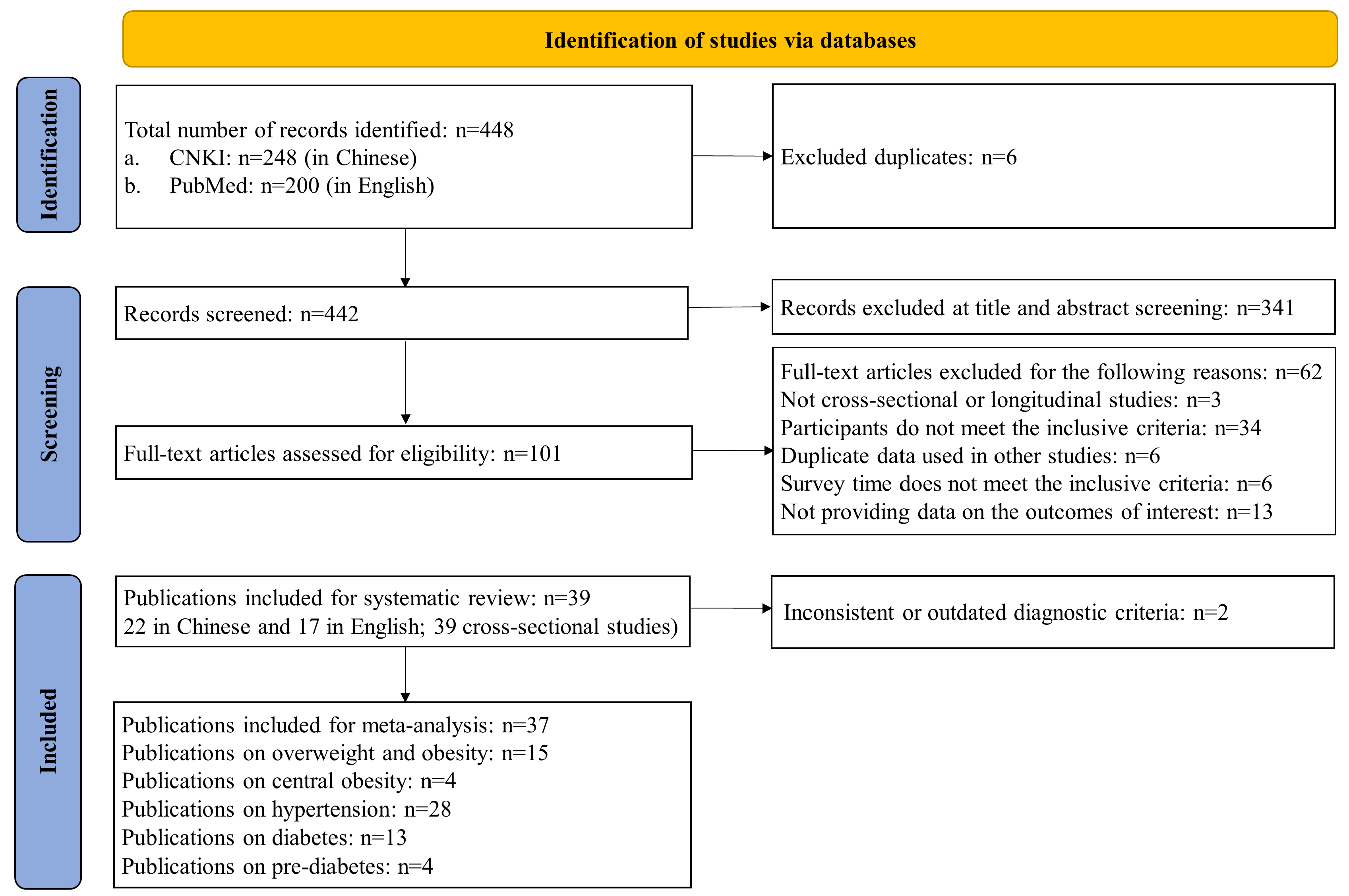
2.1. Data Sources and Search Strategies
2.2. Study Selection: Inclusion and Exclusion Criteria
2.3. Diagnostic Criteria for Overweight/Obesity, Hypertension, and Diabetes
2.4. Data Extraction and Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Studies Included
3.2. Pooled-Prevalence Estimates of Overweight/Obesity, Hypertension, and Diabetes among Tibetans, and Comparison with Average Estimates for China, the US, and the Globe
3.3. Awareness, Treatment, and Control Rates of Hypertension and Diabetes, Compared with China’s National Average
3.4. Risk Factors for Obesity, Hypertension, and Diabetes
4. Discussion
4.1. Double Burden of Malnutrition (DBM) in Tibetans
4.2. High Hypertension Prevalence among Tibetans
4.3. Low Diabetes Prevalence among Tibetans
4.4. Diverse NCD Patterns and Associated Risk Factors in Tibetans
4.5. Hypertension and Diabetes Management
4.6. Study Strengths and Limitations
4.7. Policy Implications and Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations & World Health Organization. Time to Deliver. Third UN High-Level Meeting on Non-Communicable Diseases. Available online: https://www.who.int/ncds/governance/third-un-meeting/brochure.pdf (accessed on 20 December 2021).
- The Chinese National Health Commission. The Nutrition and Health Status of the Chinese People (2020 Report). Available online: http://www.scio.gov.cn/xwfbh/xwbfbh/wqfbh/42311/44583/wz44585/Document/1695276/1695276.htm (accessed on 20 December 2021).
- Di Cesare, M.; Khang, Y.-H.; Asaria, P.; Blakely, T.; Cowan, M.J.; Farzadfar, F.; Guerrero, R.; Ikeda, N.; Kyobutungi, C.; Msyamboza, K.P.; et al. Inequalities in non-communicable diseases and effective responses. Lancet 2013, 381, 585–597. [Google Scholar] [CrossRef] [Green Version]
- Anderson, I.; Robson, B.; Connolly, M.; Al-Yaman, F.; Bjertness, E.; King, A.; Tynan, M.; Madden, P.R.; Bang, A.; Coimbra, P.C.E.A., Jr.; et al. Indigenous and tribal peoples’ health (The Lancet-Lowitja Institute Global Collaboration): A population study. Lancet 2016, 388, 131–157. [Google Scholar] [CrossRef]
- The Nutrition and Health Status of the Chinese People (2015 Report); People’s Health Press: Beijing, China, 2015.
- Peng, W.; Liu, Y.; Malowany, M.; Chen, H.; Su, X.; Liu, Y. Metabolic syndrome and its relation to dietary patterns among a selected urbanised and semi-urbanised Tibetan population in transition from nomadic to settled living environment. Public Health Nutr. 2021, 24, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Lin, B.Y.; Genden, K.; Shen, W.; Wu, P.S.; Yang, W.C.; Hung, H.F.; Fu, C.-M.; Yang, K.-C. The prevalence of obesity and metabolic syndrome in Tibetan immigrants living in high altitude areas in Ladakh, India. Obes. Res. Clin. Pract. 2018, 12, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Peng, W. Nutritional implications of Tibetan Plateau resettling and urbanization programmes. In United Nations System Standing Committee on Nutrition (UNSCN)—Nutrition; Oenema, S., Campeau, C., Delmuè, D., Eds.; UNSCN: Roma, Italy, 2019; Volume 44, pp. 83–90. [Google Scholar]
- The Chinese National Health Commission. Health Industry Standards of the People’s Republic of China—Criteria of Weight for Adults. 2013. Available online: http://www.nhc.gov.cn/ewebeditor/uploadfile/2013/08/20130808135715967.pdf (accessed on 20 December 2021).
- World Health Organization. Fact Sheet: Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 20 December 2021).
- International Diatetes Federation. The IDF Consensus Worldwide Definition of the Metabolic Syndrome. Available online: https://www.idf.org/webdata/docs/%20IDF_Metasyndrome_definition.pdf (accessed on 20 December 2021).
- The Chinese National Health Commission. Health Industry Standards of the People’s Republic of China—Screening for Overweight and Obesity among School-Age Children and Adolescents. 2018. Available online: http://www.nhc.gov.cn/ewebeditor/uploadfile/2018/03/20180330094031236.pdf (accessed on 20 December 2021).
- Joint Committee for Guideline R. 2018 Chinese Guidelines for Prevention and Treatment of Hypertension—A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J. Geriatr. Cardiol. 2019, 16, 182–241. [Google Scholar]
- Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin. J. Diabetes Mellitus 2021, 13, 315–409. [Google Scholar]
- Wang, L.; Zhou, B.; Zhao, Z.; Yang, L.; Zhang, M.; Jiang, Y.; Li, Y.; Zhou, M.; Wang, L.; Huang, Z.; et al. Body-mass index and obesity in urban and rural China: Findings from consecutive nationally representative surveys during 2004–2018. Lancet 2021, 398, 53–63. [Google Scholar] [CrossRef]
- Chinese Center for Disease Control and Prevention. Report on Chronic Disease Risk Factor Surveillance in China (2010); Military Medical Science Press: Beijing, China, 2012. [Google Scholar]
- Chinese Center for Disease Control and Prevention. Report on Chronic Disease Risk Factor Surveillance in China (2013); Military Medical Science Press: Beijing, China, 2016. [Google Scholar]
- Wang, L.; Li, X.; Wang, Z.; Bancks, M.P.; Carnethon, M.R.; Greenland, P.; Feng, Y.-Q.; Wang, H.; Zhong, V.W. Trends in Prevalence of Diabetes and Control of Risk Factors in Diabetes Among US Adults, 1999–2018. JAMA 2021, 326, 1–13. [Google Scholar] [CrossRef]
- Fryar, C.D.; Ostchega, Y.; Hales, C.M.; Zhang, G.; Kruszon-Moran, D. Hypertension Prevalence and Control Among Adults: United States, 2015–2016. NCHS Data Brief 2017, 289, 1–8. [Google Scholar]
- International Diatetes Federation. IDF Diabetes Atlas, 9th ed.; IDF: Brussels, Belgium, 2019. [Google Scholar]
- World Health Organization. Global NCD Target Reduce High Blood Pressure; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- NHLBI. Study Quality Assessment Tools (Internet); NHLBI: Bethesda, MD, USA, 2020. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 20 December 2021).
- Xu, R.; Song, Y.; Ma, J.; Zhang, B.; Hu, P. Secular Trend of Overweight and Obesity Prevalence Among Tibetan Primary and High School Students, 1991–2014. Chin. J. Public Health 2017, 33, 1712–1716. [Google Scholar]
- Zhang, M.; Zhang, B. Investigation and Analysis on the Nutritional Status of Tibetan School-age Children in Basu County, Tibet. Tibet. Med. 2019, 40, 79–80. [Google Scholar]
- Chen, N.; Lyu, X. Correlation Analysis of Pre-diabetes Prevalence and Risk Factors in Tibet Plateau. Tibet. Sci. Technol. 2019, 5, 70–72. [Google Scholar]
- Chen, W.; Liu, Q.; Wang, H.; Chen, W.; Johnson, R.J.; Dong, X.; Li, H.; Ba, S.; Tan, J.; Luo, N.; et al. Prevalence and risk factors of chronic kidney disease: A population study in the Tibetan population. Nephrol. Dial. Transpl. 2011, 26, 1592–1599. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Danzenggongji. The Relationship Between Physical Activity and Body Composition of Tibetan Junior High School Students in Lhasa. Chin. J. Sch. Health 2020, 41, 1406–1410. [Google Scholar]
- Chen, Y.; Yue, L.; He, L.; Yi, B.; Huang, L.; Li, J.; Tang, Y.; Tian, F. Investigation on the Prevalence of Hypertension Among Preschool Children in Gannan Tibetan Autonomous Prefecture. Chin. J. Prev. Contr. Chron. Dis. 2020, 28, 845–847. [Google Scholar]
- Ciren, W.; Luo, Y.; Zhang, Z.; Chen, N.; Lyu, X.; Mneng, S.; Yang, S.; Amina; Basangpuchi; Li, A.; et al. Investigation of Methabollic Syndrom in Adult Tibetan Population in Lhasa, Tibet. Chongqing Yixue 2020, 49, 3912–3915. [Google Scholar]
- Deng, R.; Wang, G.; Hong, P.; Li, J.; Li, Q.; Wan, Y.; Xiong, H. Illness prevalence rate in Tibet, China: Data from the 2018 National Health Service Survey. BMC Public Health 2020, 20, 955. [Google Scholar] [CrossRef]
- Huang, X.; Zhou, Z.; Liu, J.; Song, W.; Chen, Y.; Liu, Y.; Zhang, M.; Dai, W.; Yi, Y.; Zhao, S. Prevalence, awareness, treatment, and control of hypertension among China’s Sichuan Tibetan population: A cross-sectional study. Clin. Exp. Hypertens. 2016, 38, 457–463. [Google Scholar] [CrossRef]
- Huang, Y.; Ruan, Y. The Obesity Status of Three Ethnic Groups in Yunnan Province and the Use of ROC Curve for Early Warning of Hypertension. Soft Sci. Health 2019, 33, 74–78. [Google Scholar]
- Lai, S.; Wang, H.; Qiao, Z.; Zhang, X.; Wu, X.; Taga; Basang; Zhang, Y. Analysis on the Results of the Physical Examination of Tibetan and Chinese Students in Linzhi, Tibet in 2010. Strait J. Prev. Med. 2011, 17, 21–24. [Google Scholar]
- Li, K.; Gesangluobu; Yang, X.; Changjue; Dawaciren; Gusanglamu; Zhang, M.; Ren, D.; Cidanluobu. Investigation and Comparison of the Prevalence of Metabolic Syndrome in Tibetan and Han Nationalities in Tibet Plateau. J. High Alt. Med. 2017, 27, 52–55. [Google Scholar]
- Li, T.; Liu, Y.; Dan, L.; Guo, J.; Xie, J.; Sanlang, P.; Wang, C. The Prevalence and Risk Factors of Metabolic Syndrome Among Plateau Tibetan Population in Aba area, Sichuan: A Cross-sectional Survey. Mordern Prev. Med. 2020, 47, 4235–4240. [Google Scholar]
- Li, X.; Cai, H.; He, J.; Ramachandran, D.; Xie, P.; Huang, Y.; Wang, H.; Liu, Y.; Qiao, Y.; Zhang, Q. Prevalence, awareness, treatment and control of hypertension in Tibetan monks from Gansu Province, Northwest China. Clin. Exp. Hypertens. 2015, 37, 536–541. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Qiao, Y.; Li, B.; Li, C. Prevelance and Awareness onf Hypertension in Gansu Gannan Tibetan Adult Population. China J. Cardiol. 2012, 6, 527–529. [Google Scholar]
- Li, Y.; Teng, D.; Shi, X.; Qin, G.; Qin, Y.; Quan, H.; Shi, B.; Sun, H.; Ba, J.; Chen, B.; et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: National cross sectional study. BMJ 2020, 369, m997. [Google Scholar] [CrossRef] [PubMed]
- Liao, A.; Zhang, J.; Zhao, C.; Li, K. Investigation on The Prevalence of Polycythemia and Hypertension in Tibetan Plateau in Qiongjie County, Tibet’s Agricultural Area. Tibet. Sci. Technol. 2015, 12, 31–32. [Google Scholar]
- Liu, K.; Xu, Y.; Wang, S.; Shi, R.; Gong, S.; Li, X.; Yang, Y.; Chen, X. Buddhist Activities related to Sedentary behavior and Hypertension in Tibetan monks. J. Hum. Hypertens. 2019, 33, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Fang, W.; Chang, L.; Da, Z. Investigation and Analysis of Chronic Diseases of Tibetan Herdsmen in Plateau. Hosp. Admin. J. Chin. PLA 2020, 27, 1166–1169+77. [Google Scholar]
- Meng, Q.; Xu, Y.; Shi, R.; Zhang, X.; Wang, S.; Liu, K.; Chen, X. Effect of religion on hypertension in adult Buddhists and residents in China: A cross-sectional study. Sci. Rep. 2018, 8, 8203. [Google Scholar] [CrossRef]
- Okumiya, K.; Sakamoto, R.; Ishimoto, Y.; Kimura, Y.; Fukutomi, E.; Ishikawa, M.; Suwa, K.; Imai, H.; Chen, W.; Kato, E.; et al. Glucose intolerance associated with hypoxia in people living at high altitudes in the Tibetan highland. BMJ Open 2016, 6, e009728. [Google Scholar] [CrossRef] [Green Version]
- Pan, M.; Dai, X.; Zeng, Z. Investigation of Plateau Hypertension in residents in Muli. J. Mod. Clin. Med. 2014, 40, 295–296. [Google Scholar]
- Peng, W.; Wang, S.; Han, S.; Su, X.; Zhao, L. Double burden of malnutrition in urbanized settled Tibetan communities on the Tibetan plateau. Asia Pac. J. Clin. Nutr. 2020, 29, 161–165. [Google Scholar]
- Peng, Y.; Zeren, L.; Shi, W.; Li, L.; Fang, G.; Xu, H. Prevalence and Risk Factors of Hypertension Among Tibetans in Changdu, Tibet. J. Chongqing Med. Univ. 2020, 45, 552–555. [Google Scholar]
- Sherpa, L.Y.; Stigum, H.; Chongsuvivatwong, V.; Nafstad, P.; Bjertness, E. Prevalence of metabolic syndrome and common metabolic components in high altitude farmers and herdsmen at 3700 m in Tibet. High Alt. Med. Biol. 2013, 14, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Zhou, L.; Chen, J.; Cheng, L.; Zhang, L. Analysis on the Morphological and Development of Tibetan and Han Nationality Among 7- to 18-year-old Primary and Secondary School Students in Sichuan Province. Chin. J. Child Health Care 2020, 28, 637–641. [Google Scholar]
- Song, C.; Chongsuvivatwong, V.; Zhu Luo Bu, O.; Ji, D.; Sang Zhuo Ma, B.; Sriplung, H. Relationship between hypertension and geographic altitude: A cross-sectional survey among residents in Tibet. J. Int. Med. Res. 2020, 48, 300060520903645. [Google Scholar] [CrossRef] [PubMed]
- Sun, P.; Wang, Q.; Zhang, Y.; Huo, Y.; Nima, N.; Fan, J. Association between homocysteine level and blood pressure traits among Tibetans: A cross-sectional study in China. Medicine 2019, 98, e16085. [Google Scholar] [CrossRef]
- Wang, L.; Gao, P.; Zhang, M.; Huang, Z.; Zhang, D.; Deng, Q.; Li, Y.; Zhao, Z.; Qin, X.; Jin, D.; et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017, 317, 2515–2523. [Google Scholar] [CrossRef]
- Xu, S.; Jiayong, Z.; Li, B.; Zhu, H.; Chang, H.; Shi, W.; Gao, Z.; Ning, X.; Wang, J. Prevalence and Clustering of Cardiovascular Disease Risk Factors among Tibetan Adults in China: A Population-Based Study. PLoS ONE 2015, 10, e0129966. [Google Scholar] [CrossRef]
- Xu, T.; Liu, J.; Zhu, G.; Liu, J.; Han, S. Prevalence of prehypertension and associated risk factors among Chinese adults from a large-scale multi-ethnic population survey. BMC Public Health 2016, 16, 775. [Google Scholar] [CrossRef] [Green Version]
- Xu, T.; Zhu, G.; Liu, J.; Han, S. Gender-specific prevalence and associated risk factors of high normal blood pressure and hypertension among multi-ethnic Chinese adolescents aged 8–18 years old. Blood Press 2015, 24, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Fan, P.; Zhang, X. Tibetan High-altitude Areas of Political Science and Law of Publice Servants to Investigate the Statues of Metabolic Syndrom. Mordern Prev. Med. 2010, 37, 1465–1466+71. [Google Scholar]
- Ye, Z.; Yi, J.; Su, L.; Gu, Q. Prevalence and Related Factors of Hypertension Among Tibetan and Han Adultes at Different Altitudes. Chin. J. Soc. Med. 2018, 35, 508–512. [Google Scholar]
- Zhang, H.; Ma, L.; Zhang, Z.; Jiang, Y.; Zhao, Y.; Yang, L.; Liang, D.; Dong, W.; Liu, L.; Zhao, F.; et al. Distribution characteristics of hypertension, fatty liver, and hyperuricemia in adult Tibetan residents: A survey based on a community in Lhasa. J. Environ. Occup. Med. 2020, 37, 1182–1187. [Google Scholar]
- Zhang, Z.; Luo, Y.; Liu, L.; Lyu, X.; Meng, S.; Basangpuchi; Du, J.; Yang, L. Preliminary investigation on prevalence of pre-diabetes and diabetes among Tibetan adults in Lhasa. Chin. J. Diabetes 2019, 27, 567–571. [Google Scholar]
- Zheng, X.; Yao, D.K.; Zhuo-Ma, C.R.; Tang, J.; Wang, T.R.; Zhang, H.H.; Wang, L.X. Prevalence, self-awareness, treatment, and control of hypertension in Lhasa, Tibet. Clin. Exp. Hypertens. 2012, 34, 328–333. [Google Scholar] [CrossRef]
- Zhu, C.; Bian, H. Analysis of Risk Factors in Tibetan Residdents with Hypertension. J. Clin. Cardiol. 2014, 30, 62–64. [Google Scholar]
- Zhuo, M.; Tang, Y.; Kang, F.; Peng, Y. The Prevalence of Hypertention and its Influencing Factors Among Tibetan in Gannan of Gansu Province. Chin. Prev. Med. 2015, 16, 675–679. [Google Scholar]
- Ramirez-Zea, M.; Kroker-Lobos, M.F.; Close-Fernandez, R.; Kanter, R. The double burden of malnutrition in indigenous and nonindigenous Guatemalan populations. Am. J. Clin. Nutr. 2014, 100, 1644s–1651s. [Google Scholar] [CrossRef] [Green Version]
- Gao, L.; Bhurtyal, A.; Wei, J.; Akhtar, P.; Wang, L.; Wang, Y. Double Burden of Malnutrition and Nutrition Transition in Asia: A Case Study of 4 Selected Countries with Different Socioeconomic Development. Adv. Nutr. 2020, 11, 1663–1670. [Google Scholar] [CrossRef]
- Dang, S.; Yan, H.; Yamamoto, S.; Wang, X.; Zeng, L. Poor nutritional status of younger Tibetan children living at high altitudes. Eur. J. Clin. Nutr. 2004, 58, 938–946. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.C.; Sawaya, A.L.; Wibaek, R.; Mwangome, M.; Poullas, M.S.; Yajnik, C.S.; Demaio, A. The double burden of malnutrition: Aetiological pathways and consequences for health. Lancet 2020, 395, 75–88. [Google Scholar] [CrossRef]
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Mingji, C.; Onakpoya, I.J.; Perera, R.; Ward, A.M.; Heneghan, C.J. Relationship between altitude and the prevalence of hypertension in Tibet: A systematic review. Heart Br. Card. Soc. 2015, 101, 1054–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, W.; Liu, Y.; Liu, Y.; Zhao, H.; Chen, H. Major dietary patterns and their relationship to obesity among urbanized adult Tibetan pastoralists. Asia Pac. J. Clin. Nutr. 2019, 28, 507–519. [Google Scholar] [PubMed]
- Mio, K.; Yamanaka, C.; Matsuoka, T.; Kobayashi, T.; Aoe, S. Effects of β-glucan Rich Barley Flour on Glucose and Lipid Metabolism in the Ileum, Liver, and Adipose Tissues of High-Fat Diet Induced-Obesity Model Male Mice Analyzed by DNA Microarray. Nutrients 2020, 12, 3546. [Google Scholar] [CrossRef] [PubMed]
- Ren, Q.; Lv, X.; Yang, L.; Yue, J.; Luo, Y.; Zhou, L.; Meng, S.; Yang, S.; Puchi, B.; Zhou, X.; et al. Erythrocytosis and Performance of HbA1c in Detecting Diabetes on an Oxygen-Deficient Plateau: A Population-based Study. J. Clin. Endocrinol. Metab. 2020, 105, e1612–e1620. [Google Scholar] [CrossRef]
- do Vale Moreira, N.C.; Montenegro, R.M., Jr.; Meyer, H.E.; Bhowmik, B.; Mdala, I.; Siddiquee, T.; Fernandes, V.O.; Hussain, A. Glycated Hemoglobin in the Diagnosis of Diabetes Mellitus in a Semi-Urban Brazilian Population. Int. J. Environ. Res. Public Health 2019, 16, 3598. [Google Scholar] [CrossRef] [Green Version]
- Bhowmik, B.; Diep, L.M.; Munir, S.B.; Rahman, M.; Wright, E.; Mahmood, S.; Afsana, F.; Ahmed, T.; Khan, A.K.A.; Hussain, A. HbA(1c) as a diagnostic tool for diabetes and pre-diabetes: The Bangladesh experience. Diabet. Med. 2013, 30, e70–e77. [Google Scholar] [CrossRef]
- Santos, J.L.; Pérez-Bravo, F.; Carrasco, E.; Calvillán, M.; Albala, C. Low prevalence of type 2 diabetes despite a high average body mass index in the aymara natives from chile. Nutrition 2001, 17, 305–309. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, L.; Gao, L.; Pan, A.; Xue, H. Health policy and public health implications of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 446–461. [Google Scholar] [CrossRef]
- Chiu, T.H.T.; Pan, W.H.; Lin, M.N.; Lin, C.L. Vegetarian diet, change in dietary patterns, and diabetes risk: A prospective study. Nutr. Diabetes 2018, 8, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Subgroups | Awareness Rate (%) | Treatment Rate (%) | Control Rate (%) | Treatment Control Rate (%) | Interpretation | |
|---|---|---|---|---|---|---|
| A Hypertension | ||||||
| National average | All Male Female Urban Rural | 40.9 37.1 45.3 45.4 37.1 | 32.5 28.6 37.1 38.2 27.7 | 9.7 9.0 10.5 12.7 7.2 | 29.8 31.3 28.4 33.1 22.3 | Data from China Chronic Disease and Risk Factors Surveillance, 2013. |
| 1. Li X.H., 2015, [37] | Adult residents | 16.9 ↓ | 13.2 ↓ | 4.5 ↓ | NA | Conducted in an impoverished Tibetan Autonomous Prefecture in Gansu. The extreme low rates among monks were due to limited access to civil healthcare services, the belief of predestinated disease by Buddha, and poor healthy literacy. |
| Buddhists | 9.5 ↓ | 4.2 ↓ | 1.6 ↓ | |||
| 2. Li X.H., 2012, [37] | All Urban Rural | 30.4 ↓ 35.7 ↓ 25.2 ↓ | 20.7 ↓ 25.1 ↓ 16.4 ↓ | 5.5 ↓ 6.9 ↓ 4.1 ↓ | NA | Conducted in an impoverished Tibetan Autonomous Prefecture in Gansu. Low education, health illiteracy, and irregular management may be the reasons for low rates. |
| 3. Meng Q.T., 2018, [42] | Adult residents | Conducted in a Tibetan Autonomous Prefecture in Sichuan. Two temples selected were top-ranking Buddhist institutes. Unlike China’s national data, women usually had worse hypertension-awareness and -management rates than men. | ||||
| All Male Female | 52.6 ↑ 56.6 ↑ 48.1 ↑ | 41.3 ↑ 56.6 ↑ 48.1 ↑ | 3.7 ↓ 4.1 ↓ 3.2 ↓ | 8.9 ↓ 8.6 ↓ 9.3 ↓ | ||
| Buddhists | ||||||
| All Male Female | 43.5 ↑ 48.9 ↑ 37.2 ↓ | 30.1 ↓ 33.3 ↑ 26.4 ↓ | 6.2 ↓ 8.6 ↓ 3.4 ↓ | 20.6 ↓ 25.9 ↓ 12.8 ↓ | ||
| 4. Sherpa L.Y., 2013, [47] | All Male Female | 69.4 ↑ 65.3 ↑ 75.2 ↑ | 59.1 ↑ 54.8 ↑ 62.8 ↑ | 19.5 ↑ 23.0 ↑ 16.5 ↑ | 33.0 ↑ 26.3 ↓ 42.1 ↑ | Conducted in two counties of Lhasa, the historical and cultural center of Tibetan areas. Study participants had better diabetes management than China’s national average. |
| 5. Zheng X, 2013, [59] | All Male Female | 63.5 ↑ 65.9 ↑ 61.6 ↑ | 24.3 ↓ 25.6 ↓ 23.2 ↓ | 7.7 ↓ 8.5 ↓ 7.1 ↓ | 31.8 ↑ 33.3 ↑ 30.4 ↑ | Conducted in Lhasa. Most participants were urban residents. The higher educational level among urban residents may explain the better hypertension management compared with other studies. |
| B Diabetes | ||||||
| National average | All Male Female | 38.6 35.5 42.2 | 35.6 32.3 39.4 | 33.0 31.6 34.6 | 36.3 35.5 37.2 | Data from China Chronic Disease and Risk Factors Surveillance, 2013. |
| 1. Sherpa L.Y., 2013, [47] | All Male Female | 29.6 ↓ 25.0 ↓ 31.5 ↓ | 22.2 ↓ 25.0 ↓ 21.0 ↓ | 7.4 ↓ 0.0 ↓ 10.5 ↓ | NA | Conducted in Lhasa. Participants had lower diabetes management than China’s national average. |
| 2. Li Y.Z., 2020, [38] | All | 28.3 ↓ | 43.4 ↑ | 24.3 ↓ | NA | Nationally representative survey, but not Tibetan representative. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peng, W.; Li, K.; Yan, A.F.; Shi, Z.; Zhang, J.; Cheskin, L.J.; Hussain, A.; Wang, Y. Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall. Int. J. Environ. Res. Public Health 2022, 19, 8787. https://doi.org/10.3390/ijerph19148787
Peng W, Li K, Yan AF, Shi Z, Zhang J, Cheskin LJ, Hussain A, Wang Y. Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall. International Journal of Environmental Research and Public Health. 2022; 19(14):8787. https://doi.org/10.3390/ijerph19148787
Chicago/Turabian StylePeng, Wen, Ke Li, Alice F. Yan, Zumin Shi, Junyi Zhang, Lawrence J. Cheskin, Ahktar Hussain, and Youfa Wang. 2022. "Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall" International Journal of Environmental Research and Public Health 19, no. 14: 8787. https://doi.org/10.3390/ijerph19148787
APA StylePeng, W., Li, K., Yan, A. F., Shi, Z., Zhang, J., Cheskin, L. J., Hussain, A., & Wang, Y. (2022). Prevalence, Management, and Associated Factors of Obesity, Hypertension, and Diabetes in Tibetan Population Compared with China Overall. International Journal of Environmental Research and Public Health, 19(14), 8787. https://doi.org/10.3390/ijerph19148787








