Subtypes of Asthma and Cold Weather-Related Respiratory Symptoms
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Study Population
2.2. Determinant of Interest
2.3. Outcomes
2.4. Covariates
2.5. Statistical Methods
3. Results
3.1. Characteristics of the Study Population
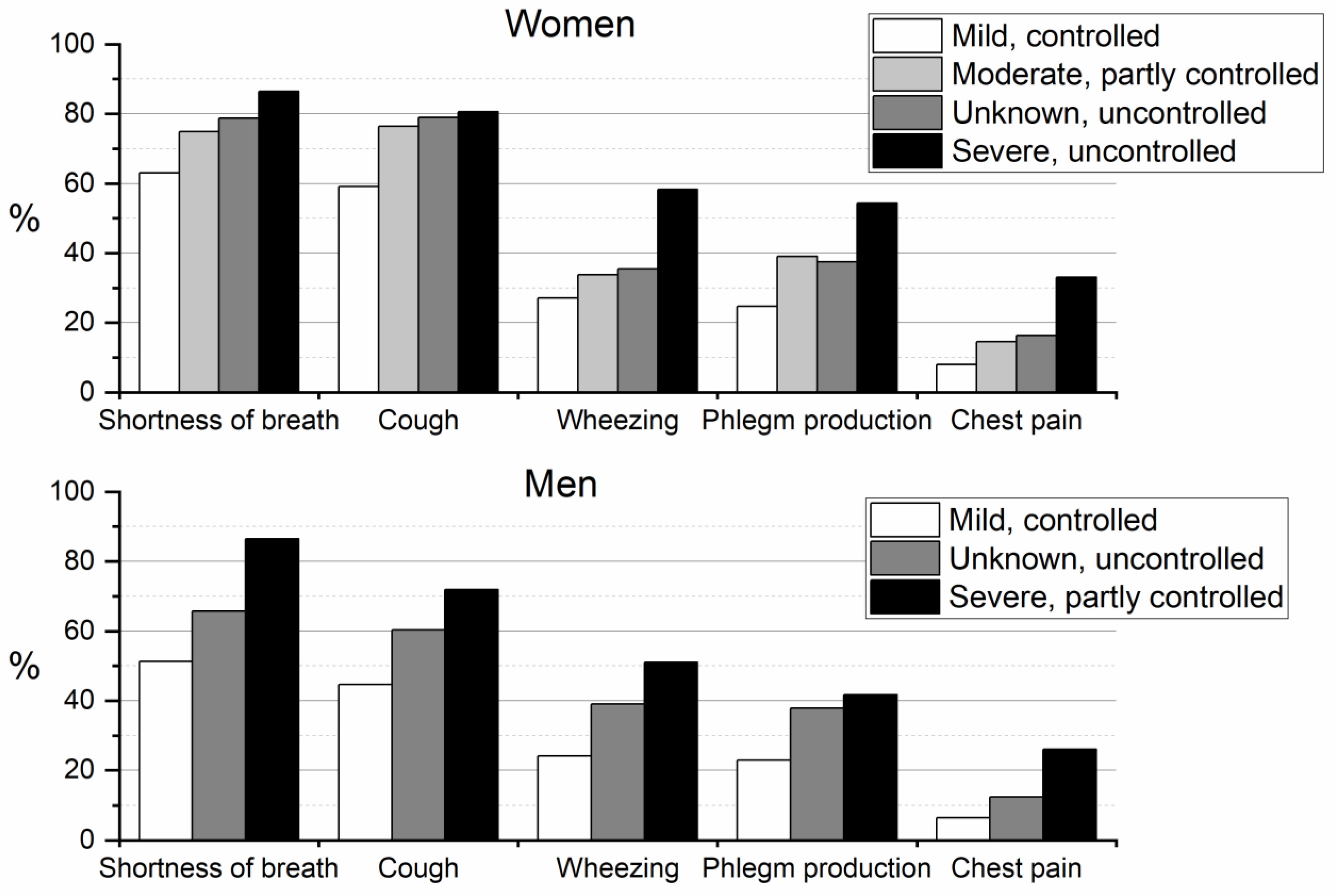
3.2. Cold Weather-Related Symptoms in Relation to the Asthma Subtypes
4. Discussion
4.1. Validity of Results
4.2. Synthesis with Previous Knowledge
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The Global Initiative for Asthma, Global Strategy for Asthma Management and Prevention (2021 Update). 2021. Available online: https://ginasthma.org/gina-reports/ (accessed on 1 October 2021).
- Amelink, M.; de Nijs, S.B.; de Groot, J.C.; van Tilburg, P.M.; van Spiegel, P.I.; Krouwels, F.H.; Lutter, R.; Zwinderman, A.H.; Weersink, E.J.; ten Brinke, A.; et al. Three phenotypes of adult-onset asthma. Allergy Eur. J. Allergy Clin. Immunol. 2013, 68, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Brew, B.K.; Chiesa, F.; Lundholm, C.; Örtqvist, A.; Almqvist, C. A modern approach to identifying and characterizing child asthma and wheeze phenotypes based on clinical data. PLoS ONE 2019, 14, e0227091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deliu, M.; Sperrin, M.; Belgrave, D.; Custovic, A. Identification of asthma subtypes using clustering methodologies. Pulm. Ther. 2016, 2, 19–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howard, R.; Rattray, M.; Prosperi, M.; Custovic, A. Distinguishing asthma phenotypes using machine learning approaches. Curr. Allergy Asthma Rep. 2015, 15, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyrkäs, H.; Jaakkola, M.S.; Ikäheimo, T.M.; Hugg, T.T.; Jaakkola, J.J.K. Asthma and allergic rhinitis increase respiratory symptoms in cold weather among young adults. Respir. Med. 2014, 108, 63–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Näyhä, S.; Hassi, J.; Jousilahti, P.; Laatikainen, T.; Ikäheimo, T.M. Cold-related symptoms among the healthy and sick of the general population: National FINRISK Study data, 2002. Public Health 2011, 125, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Harju, T.; Mäkinen, T.; Näyhä, S.; Laatikainen, T.; Jousilahti, P.; Hassi, J. Cold-related respiratory symptoms in the general population. Clin. Respir. J. 2010, 4, 176–185. [Google Scholar] [CrossRef]
- Hyrkäs, H.; Ikäheimo, T.M.; Jaakkola, J.J.K.; Jaakkola, M.S. Asthma control and cold weather-related respiratory symptoms. Respir. Med. 2016, 113, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Mäkikyrö, E.M.S.; Jaakkola, M.S.; Jaakkola, J.J.K. Subtypes of asthma based on asthma control and severity: A latent class analysis. Respir. Res. 2017, 18, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M. The St George’s Respiratory Questionnaire. Respir. Med. 1991, 85 (Suppl. B), 25–31. [Google Scholar] [CrossRef]
- Cruz, A.A.; Togias, A. Upper airways reactions to cold air. Curr. Allergy Asthma Rep. 2008, 8, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Koskela, H.; Tukiainen, H. Facial cooling, but not nasal breathing of cold air, induces bronchoconstriction: A study in asthmatic and healthy subjects. Eur. Respir. J. 1995, 8, 2088–2093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seys, S.F.; Daenen, M.; Dilissen, E.; van Thienen, R.; Bullens, D.M.A.; Hespel, P.; Dupont, L.J. Effects of high altitude and cold air exposure on airway inflammation in patients with asthma. Thorax 2013, 68, 906–913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, W.C.; Meyers, D.A.; Wenzel, S.E.; Teague, W.G.; Li, H.; Li, X.; D’Agostino, R., Jr.; Castro, M.; Curran-Everett, D.; Fitzpatrick, A.M.; et al. Identification of asthma phenotypes using cluster analysis in the severe asthma research program. Am. J. Respir. Crit. Care Med. 2010, 181, 315–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oksel, C.; Granell, R.; Haider, S.; Fontanella, S.; Simpson, A.; Turner, S.; Devereux, G.; Arshad, S.H.; Murray, C.S.; Roberts, G.; et al. Distinguishing wheezing phenotypes from infancy to adolescence: A pooled analysis of five birth cohorts. Ann. Am. Thoracic Soc. 2019, 16, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Weinmayr, G.; Keller, F.; Kleiner, A.; Du Prel, J.B.; Garcia-Marcos, L.; Batllés-Garrido, J.; Garcia-Hernandez, G.; Suarez-Varela, M.M.; Strachan, D.P.; Nagel, G. Asthma phenotypes identified by latent class analysis in the ISAAC phase II Spain study. Clin. Exp. Allergy 2013, 43, 223–232. [Google Scholar] [CrossRef] [PubMed]
| Women N (%) | Men N (%) | Total N (%) | |
|---|---|---|---|
| Total | 1303 (65.31) | 692 (34.69) | 1995 |
| Age | |||
| <30 | 141 (10.82) | 71 (10.26) | 212 (10.63) |
| 30–40 | 177 (13.58) | 91 (13.15) | 268 (13.43) |
| 40–50 | 243 (18.65) | 111 (16.04) | 354 (17.74) |
| 50–60 | 428 (32.85) | 218 (31.50) | 646 (32.38) |
| >60 | 314 (24.10) | 201 (29.05) | 515 (25.81) |
| Body mass index | |||
| <25 | 504 (39.56) | 216 (31.58) | 720 (36.77) |
| 25–30 | 420 (32.97) | 286 (41.81) | 706 (36.06) |
| 30–35 | 305 (23.94) | 170 (24.85) | 475 (24.26) |
| >35 | 45 (3.53) | 12 (1.75) | 57 (2.91) |
| Missing | 29 | 8 | 37 |
| Marital status | |||
| Single | 155 (11.91) | 121 (17.51) | 276 (13.86) |
| Marriage/Cohabitation | 963 (74.02) | 498 (72.07) | 1461 (73.34) |
| Divorced, separated or widow | 183 (14.07) | 72 (10.42) | 255 (12.80) |
| Missing | 2 | 1 | 3 |
| Education | |||
| Low | 298 (22.99) | 205 (29.71) | 503 (25.33) |
| Medium | 673 (51.93) | 348 (50.43) | 1021 (51.41) |
| High | 325 (25.08) | 137 (19.86) | 462 (23.33) |
| Missing | 7 | 2 | 9 |
| Smoking | |||
| Current smoker | 231 (17.98) | 134 (19.62) | 365 (18.55) |
| Ex-smoker | 323 (25.14) | 268 (39.24) | 591 (30.03) |
| Never smoked | 731 (56.89) | 281 (41.14) | 1012 (51.42) |
| Missing | 18 | 9 | 27 |
| N (%) | |
|---|---|
| Women | |
| Mild, controlled | 525 (40.29) |
| Moderate, partly controlled | 287 (22.03) |
| Unknown, uncontrolled | 376 (28.86) |
| Severe, uncontrolled | 115 (8.83) |
| Men | |
| Mild, controlled | 193 (27.89) |
| Unknown, uncontrolled | 395 (57.08) |
| Severe, partly controlled | 104 (15.03) |
| No. of Subjects (%) | Crude PR (95% CI) | Adjusted PR (95% CI) | |
|---|---|---|---|
| Shortness of breath | |||
| Mild, controlled | 301 (63.10) | 1.00 | 1.00 |
| Moderate, partly controlled | 191 (74.90) | 1.19 (1.08, 1.31) | 1.17 (1.05, 1.29) |
| Unknown, uncontrolled | 269 (78.65) | 1.25 (1.14, 1.36) | 1.26 (1.14, 1.40) |
| Severe, uncontrolled | 89 (86.41) | 1.37 (1.24, 1.52) | 1.37 (1.23, 1.53) |
| Cough | |||
| Mild, controlled | 282 (59.12) | 1.00 | 1.00 |
| Moderate, partly controlled | 195 (76.47) | 1.29 (1.17, 1.43) | 1.24 (1.12, 1.38) |
| Unknown, uncontrolled | 270 (78.95) | 1.34 (1.22, 1.46) | 1.34 (1.21, 1.49) |
| Severe, uncontrolled | 83 (80.58) | 1.36 (1.21, 1.54) | 1.35 (1.19, 1.53) |
| Wheezing | |||
| Mild, controlled | 129 (27.04) | 1.00 | 1.00 |
| Moderate, partly controlled | 86 (33.73) | 1.25 (0.99, 1.56) | 1.23 (0.97, 1.55) |
| Unknown, uncontrolled | 121 (35.48) | 1.31 (1.07, 1.61) | 1.30 (1.02, 1.64) |
| Severe, uncontrolled | 60 (58.25) | 2.15 (1.73, 2.68) | 2.00 (1.56, 2.57) |
| Phlegm production | |||
| Mild, controlled | 118 (24.74) | 1.00 | 1.00 |
| Moderate, partly controlled | 99 (38.98) | 1.58 (1.27, 1.96) | 1.54 (1.22, 1.94) |
| Unknown, uncontrolled | 128 (37.43) | 1.51 (1.23, 1.86) | 1.60 (1.27, 2.01) |
| Severe, uncontrolled | 56 (54.37) | 2.20 (1.74, 2.78) | 2.36 (1.83, 3.03) |
| Chest pain | |||
| Mild, controlled | 38 (7.98) | 1.00 | 1.00 |
| Moderate, partly controlled | 37 (14.57) | 1.82 (1.19, 2.79) | 1.61 (1.03, 2.53) |
| Unknown, uncontrolled | 56 (16.37) | 2.05 (1.39, 3.02) | 2.20 (1.40, 3.48) |
| Severe, uncontrolled | 34 (33.01) | 4.13 (2.74, 6.24) | 4.48 (2.83, 7.09) |
| No of Subjects and Symptom Prevalence | Crude PR (95% CI) | Adjusted PR (95% CI) | |
|---|---|---|---|
| Shortness of breath | |||
| Mild, controlled | 87 (51.18) | 1.00 | 1.00 |
| Unknown, uncontrolled | 222 (65.68) | 1.28 (1.09, 1.51) | 1.44 (1.18, 1.75) |
| Severe, partly controlled | 83 (86.46) | 1.69 (1.43, 2.00) | 1.79 (1.46, 2.21) |
| Cough | |||
| Mild, controlled | 76 (44.71) | 1.00 | 1.00 |
| Unknown, uncontrolled | 204 (60.36) | 1.35 (1.12, 1.63) | 1.38 (1.10, 1.73) |
| Severe, partly controlled | 69 (71.88) | 1.61 (1.30, 1.98) | 1.55 (1.20, 2.00) |
| Wheezing | |||
| Mild, controlled | 41 (24.12) | 1.00 | 1.00 |
| Unknown, uncontrolled | 132 (39.05) | 1.62 (1.20, 2.18) | 1.55 (1.09, 2.19) |
| Severe, partly controlled | 49 (51.04) | 2.12 (1.52, 2.95) | 1.84 (1.26, 2.71) |
| Phlegm production | |||
| Mild, controlled | 39 (22.94) | 1.00 | 1.00 |
| Unknown, uncontrolled | 128 (37.87) | 1.65 (1.21, 2.25) | 1.82 (1.27, 2.59) |
| Severe, partly controlled | 40 (41.67) | 1.82 (1.26, 2.61) | 1.75 (1.14, 2.68) |
| Chest pain | |||
| Mild, controlled | 11 (6.47) | 1.00 | 1.00 |
| Unknown, uncontrolled | 42 (12.43) | 1.92 (1.01, 3.63) | 2.09 (0.97, 4.54) |
| Severe, partly controlled | 25 (26.04) | 4.02 (2.07, 7.81) | 3.84 (1.72, 8.57) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hyrkäs-Palmu, H.; Jaakkola, M.S.; Mäkikyrö, E.M.S.; Jaakkola, J.J.K. Subtypes of Asthma and Cold Weather-Related Respiratory Symptoms. Int. J. Environ. Res. Public Health 2022, 19, 8790. https://doi.org/10.3390/ijerph19148790
Hyrkäs-Palmu H, Jaakkola MS, Mäkikyrö EMS, Jaakkola JJK. Subtypes of Asthma and Cold Weather-Related Respiratory Symptoms. International Journal of Environmental Research and Public Health. 2022; 19(14):8790. https://doi.org/10.3390/ijerph19148790
Chicago/Turabian StyleHyrkäs-Palmu, Henna, Maritta S. Jaakkola, Elina M. S. Mäkikyrö, and Jouni J. K. Jaakkola. 2022. "Subtypes of Asthma and Cold Weather-Related Respiratory Symptoms" International Journal of Environmental Research and Public Health 19, no. 14: 8790. https://doi.org/10.3390/ijerph19148790
APA StyleHyrkäs-Palmu, H., Jaakkola, M. S., Mäkikyrö, E. M. S., & Jaakkola, J. J. K. (2022). Subtypes of Asthma and Cold Weather-Related Respiratory Symptoms. International Journal of Environmental Research and Public Health, 19(14), 8790. https://doi.org/10.3390/ijerph19148790







