Abstract
Pictorial humanization is a useful intervention for the improvement of hospitalized patients’ affective states. Despite benefits in many hospital wards having been well documented, so far, no attention was paid to the Neonatal Intensive Care Unit (NICU). The aim of the present study was to evaluate the levels of distress and the affective perception of the environment experienced by parents of infants hospitalized in a NICU after the implementation of an intervention of pictorial humanization. A sample of 48 parents was recruited, 25 before the intervention was performed (Control Group), and 23 after its implementation (Pictorial Humanization Group). All parents completed the “Rapid Stress Assessment Scale” and “Scales of the Affective Quality Attributed to Place” questionnaires. Despite results showing no significant differences on parental distress, after implementation of pictorial intervention parents reported a perception of the NICU as significantly more pleasant, exciting, and arousing, and less distressing, unpleasant, gloomy, and sleepy. A higher level of distress and a perception of the environment as less relaxing was predicted for the Control Group condition. The present study suggests that the pictorial intervention represents a useful technique to create more welcoming hospital environments and to reduce the negative effects associated with infant hospitalization.
1. Introduction
The hospitalization of a baby in a Neonatal Intensive Care Unit (NICU) represents an unanticipated and highly stressful event not only for the infant but also for his/her parents [1,2,3,4]. The literature has deeply underlined how these parents usually report feelings of loss and uncertainty related to the high risk of serious injury, concern for short and long-term health and development, or even the baby’s death [5,6,7,8]. During hospitalization, parents can often also experience a sense of helplessness, reinforced by the need to delegate the baby’s care to medical staff [9]. Furthermore, the hospital itself can represent a stressor for parents, as the NICU rules (e.g., scheduled visiting hours) and environmental characteristics (such as noises, lights, alarms) could be perceived as unfamiliar and disturbing [10,11,12].
Therefore, parents might show elevated levels of distress, in fact, the literature shows an increased risk of depressive and anxious symptoms compared to parents with healthy children and to parents with children admitted to general pediatric wards [3,11,13,14,15,16,17]. The intensity of parental distress could be particularly severe, leading to the risk of developing post-traumatic stress symptoms [18,19] that could persist for a long time after discharge [20,21].
Parental distress not only impairs parents’ affective status but can adversely affect the quality of parenting [22,23] and the relationship with the infant [6,24], increasing the risk of long-term consequences for child development [7,25,26,27,28,29]. These consequences could be more severe in cases of higher child vulnerability, such as preterm birth. Therefore, the implementation of interventions aimed at supporting the parental role during infant hospitalization is fundamental [30,31,32]. To this end, many interventions may be listed, including educational approaches, psychological support, and psychotherapeutic strategies [33,34,35]. In recent years, many reviews and meta-analyses investigated the quality of these interventions, finding mixed results; while some programs showed beneficial effects on reducing parental distress, others showed only low or moderate positive effects [30,34,36].
Given the complexity of parental experience, the use of different approaches of intervention in combination is recommended [34]. Among these, a relevant kind of program aims to improve hospital environments, making them more suitable for young patients and their families. These interventions aim at promoting patients’ well-being and not just at reducing the levels of discomfort, consistently with the broader definition of health [37].
From this perspective, an important role is played by the intervention of humanization in healthcare environments. According to Environmental Psychology, the physical environment in which a patient receives care could play a significant role in their healing process [38,39]. In this sense, acting on the spatial, physical, and functional characteristics of the places of care, this intervention may positively influence the patients’ well-being and quality of life, reducing environmental stressors and the negative effects of hospitalization [40,41,42,43,44]. The literature has recognized the beneficial effect of specific architectural elements, such as visual (i.e., natural light, intensity of illumination), acoustic (i.e., noise reduction, therapeutic sounds, music), and olfactory characteristics (i.e., improvement of air quality) [39,40,45,46,47,48,49]. Particularly, the use of artwork or colored and pictorial installations has demonstrated positive effects on clinical indicators of health, reducing blood pressure, heart rate, pain threshold, and length of hospitalization [40,50,51,52]. Among these, the presence of nature paintings and prints in particular was associated with an improvement in patients’ conditions [50,51].
Regarding this, interventions based on the so-called “pictorial humanization” represent useful elements to elicit calmness and to decrease anxiety, agitation, and distress [39,52,53]. These interventions consist of installations of murals or panels depicting natural or artistic images. The themes of pictorial intervention are always studied with great sensitivity according to the specific patients to whom they are addressed, in order to trigger a psycho-sensorial reaction that, integrating with the rest of the environment, could favor a reassuring and restorative experience [54,55]. In a hospital context, the beneficial effect of this intervention on patients’ well-being could be associated not only with a distraction effect, but also with the activation of the “cognitive refocusing” coping strategy [56,57,58]. Indeed, the presence of a painting may sustain patients’ attention and interest, helping them to feel more comfortable and familiar in an unknown place [59,60]. Furthermore, themes of painting representing natural landscapes and of bright colors could reduce emotional states such as worrying, anxiety, and agitation [61,62,63,64,65].
Many studies have stated the positive effects of pictorial humanization in increasing well-being of patients admitted to different wards [39,42], such as Psychiatry [65], Radiology [66,67], Stem Cell Transplant Centre [68], and Pediatrics [52,54,69,70,71,72]. Referring to the latter, most of the studies directly assessed the impact of intervention on children [52,69,71,72], while only two studies [54,70] investigated the impact on hospitalized children’s parents. Specifically, both studies assessed parental “affective perception of the environment”, a construct defined by Russell and Pratt [73] to describe the emotional qualities that people attributes to the places that could influences subsequent relations with the environment [73,74]. In pediatric wards, pictorial intervention had a significant positive effect on affective perception of hospital environment [54,70], emphasizing the relevance of these interventions to support family adjustment during child hospitalization. Based on these promising findings, pictorial humanization could represent a useful intervention in the NICU environment, too, reducing the sense of unfamiliarity experienced by infants’ parents and improving their level of distress and the affective perception of the environment. Nevertheless, to our knowledge, until now, no studies have investigated the possible effect of pictorial humanization in the NICU on parental distress and affective states.
The general aim of the study was to investigate the level of distress in parents of infants admitted to a hospital NICU, before and after an intervention of pictorial humanization. Specifically, our objectives were:
- (a)
- to investigate the effect of the humanization intervention on the levels of parental distress. We hypothesized that the parents of a hospitalized infant would show lower levels of distress after pictorial humanization intervention than those observed before its implementation;
- (b)
- to evaluate the effect of the pictorial humanization intervention on the affective perception of the environment, assuming more positive responses in the group of parents evaluated after the implementation of the intervention;
- (c)
- to explore whether the dimensions of parental affective perception could be related to the level of parental distress. Indeed, according to the theoretical statement that “the first level of response to the environment is affective […] very generally governs the directions taken by subsequent relations with the environment” [74] (p. 16), an association between parental distress and affective perception of environments could be supposed. Since no previous studies have investigated this relationship, neither in the NICU nor in other hospital wards, no specific hypotheses were developed.
2. Materials and Methods
2.1. Research Design and Participants
The research design of the present study was consistent with previous studies conducted in an Italian context aimed to investigate the effect of pictorial humanization of hospital wards [54,67,70].
The total sample included 48 parents (38 mothers, 10 fathers; mean age: 33.3 ± 6.4 years; range 22–50) of infants hospitalized at the NICU of Bufalini Hospital (Ausl Romagna, Cesena, Italy).
The research consisted of two phases. In the first one, between April and July 2014, the purpose was to measure the level of parental distress and the qualities of affective perception of the non-humanized NICU environment, beforehand implementation of intervention. During this phase, the walls were white and aseptic. For this phase, 25 parents (20 mothers, 5 fathers; mean age: 32.0 ± 6.6) of infants admitted to the NICU were recruited and they represented the Control Group (CG).
At the end of this phase, a large pictorial intervention was implemented in NICU. The pictorial intervention consisted of an extensive decoration work of the corridor of the NICU: panels were affixed to all the walls, covering them entirely. Specifically, the background of the panels was blue, representing a sea landscape, and cartoon characters related to the marine theme (i.e., fish, mermaids, sailors, boats, submarines,…) were painted along all the walls. At the end of implementation, we chose to administer the same questionnaires during the same period of the year as the first administration, to avoid the law of effect.
Therefore, the second phase took place between April and July 2015, and the level of parental distress and the qualities of affective perception were assessed after the intervention of pictorial humanization. A group of 23 parents (19 mothers, 4 fathers; mean age: 34.6 ± 5.9) of infants admitted into the same Unit was recruited; this sample represented the experimental condition in the research design (Pictorial Humanization Group, PHG).
2.2. Procedure and Measures
All the parents were recruited during infant hospitalization at the NICU. One day a week, a psychologist went to visit parents, asking them to take part in the study. If they agreed, the psychologist gave them the informed consent and asked them to stay for 5 min in the area involved into pictorial humanization intervention. After this, they were asked to fill out two questionnaires to measure their level of distress and affective perception of the NICU environment.
The psychologist firstly asked the parents to fill out a demographic form (including the parent’s gender, age, civil status and parity, and the infant’s gender, gestational age, actual weight, twinning, the duration, and the reason for hospitalization).
To assess the level of distress, parents completed the Rapid Stress Assessment Scale (VRS [75]), a questionnaire created for the self-evaluation and perception of one’s own possible stressful reactions. VRS is based on the stress model proposed by Lazarus and Folkman [76], and evaluates the responses to stress in different psychopathologic dimensions; it includes 15 items, subdivided into 5 subscales: Anxiety, Depression, Somatization, Aggressiveness, and Lack of social support. Each item is scored on a 4-point scale (ranging from 0 to 3), and the total score ranges between 0 and 45, where lower scores describe no or low levels of distress, while higher ones indicating high stressful reactions. For each subscale it is possible to obtain a total score. VRS was used in studies on clinical and non-clinical Italian population [13,67,77,78]. In the present study, it was considered suitable to assess the level of possible parental distress as a state-measure in a hospital context, according to a previous study [13].
To assess the parental affective perception of environment, the Italian version of the “Scale of the Affective Quality Attributed to Place” (QAL [73,79,80,81]) was administered. The questionnaire is based on the circumflex model of affective quality attributed to places [73]. This measure consists of 48 adjectives, divided into 8 domains (each one consisting of 6 items), creating 4 bipolar dimensions: relaxing–distressing, exciting–gloomy, pleasant–unpleasant, and arousing–sleepy. Each item is scored on a 7-point rating scale, indicating to what extent each adjective is adequate in describing the target place (0 = not at all appropriate; 6 = completely appropriate). QAL was used in previous studies to assess the affective perceptions of hospital environment [54,67,70]. In the present study we administered the validated version by Perugini et al. [79], that that demonstrated a structural similarity to Russell’s model [73].
2.3. Data Analyses
Descriptive analyses (independent t-test and Pearson’s Chi-square) were conducted to investigate the homogeneity of the two groups (CG and PHG) relating to the main demographic variables for parents and infants.
We then explored whether the level of distress and parental affective perception of the environment differed between CG and PHG. Therefore, we employed two multilevel-ANOVA, considering VRS and QAL scores, respectively, as dependent variables.
Finally, we used a linear regression model with VRS total score as dependent variable and both group condition (CG versus PHG) and QAL scales as possible predictors. Given the small sample size, we conduct two separate analyses considering: firstly, group condition and QAL positive scales (relaxing, exciting, pleasant, arousing) as predictors; secondly, a model including group condition and QAL negative scales (distressing, gloomy, unpleasant, sleepy). Given that a small number of observations leads to a risk of overfitting the model [82,83,84], we counteracted the negative effects of the small sample size by implementing a bootstrap procedure. We initially performed the analysis in the estimation sample by entering all potential predictors and replicated 2000 times using bootstrap resampling [85]. The final enter model was implemented with VRS total scores determined from the bootstrap process.
Data were analyzed using SPSS for Windows version 22.0 (IBM, Armonk, NY, USA). A p value < 0.05 was considered statistically significant.
3. Results
3.1. Descriptive Characteristics
Preliminary analyses showed that the two groups were homogeneous in relation to all parent and infant variables (Table 1).

Table 1.
Descriptive characteristics of sample.
3.2. Effect of the Intervention of Pictorial Humanization on Parental Distress
When we investigated parental distress, no significant differences between groups emerged in any scale of VRS (all p values > 0.05) (Table 2).

Table 2.
Mean scores for VRS scales and total score in CG and PHG parents.
3.3. Effect of the Intervention of Pictorial Humanization on Affective Perception of the NICU Environment
Regarding the affective perception of the NICU environment, significant differences emerged between the two groups in each subscale. Particularly, PHG group showed significantly higher scores than did the CG in three of the four positive scales: pleasant (F(1,45) = 12.367; p = 0.001), exciting (F(1,45) = 16.419; p < 0.0005) and arousing (F(1,45) = 6.317; p = 0.016) (Figure 1).
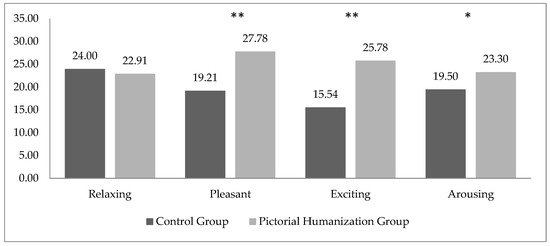
Figure 1.
Mean scores for positive QAL scales in CG and PHG parents. * p < 0.05; ** p < 0.005.
Conversely, no significant differences between CG and PHG were found on relaxing scale (F(1,45) = 0.289; p = 0.594) (Figure 1).
Furthermore, PHG obtained significantly lower scores than did the CG in all the negative scales: distressing (F(1,45) = 4.355; p = 0.043), unpleasant (F(1,45) = 9.078; p = 0.004), gloomy (F(1,45) = 10.808; p = 0.002) and sleepy (F(1,45) = 7.073; p = 0.011) (Figure 2).
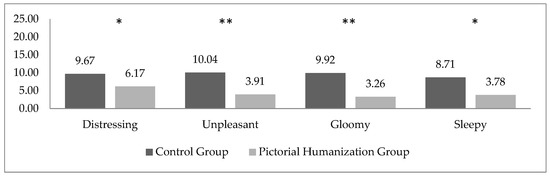
Figure 2.
Mean scores for negative QAL scales in CG and PHG parents. * p < 0.05; ** p < 0.005.
3.4. Potential Predictors of Parental Distress
As mentioned above, two separate regression analyses were conducted to explore the role of group condition and affective perception of environment on parental distress.
The first model predicted the level of distress considering group condition and the four positive scales at QAL (Table 3). A statistically significant regression equation was found (F(5,44) = 6.523, p < 0.0005), with an R2Adjusted = 0.386. According to the model, group condition and scores at relaxing subscale significantly contributed to VRS total Score (β = −0.377, t(5) = −2.422, p = 0.020; β = −0.847, t(5) = −4.894, p < 0.0005, respectively). The direction of these relationships suggested that a higher level of distress was predicted by belonging to the control group condition, namely, CG parents showed an increased probability to have higher VRS total score; a perception of the NICU environment as less relaxing (Table 3).

Table 3.
Regression model identifying the effect of group intervention and QAL positive subscales on VRS total score.
The second model included group condition and the four negative QAL scales and tested their prediction of VRS total score. No statistically significant equation emerged (F(5,44) = 1.525, p > 0.05, R2Adjusted = 0.056).
4. Discussion
The main aim of the present study was to evaluate the effects of an intervention of pictorial humanization on the levels of distress and the affective perception of the environment experienced by parents of infants hospitalized in the NICU. The research is part of a topic of growing interest in the international literature, that is, the implementation of humanization interventions of healthcare environments aimed at increasing patient well-being and reducing the negative effects of hospitalization. The literature has recognized the effects of interventions of humanization on affective perception in several hospital wards, such as Psychiatry, Radiology, Stem Cell Transplant Centre, and Pediatrics [42,52,54,65,66,67,68,69,70,71,72]. Nevertheless, no attention has been paid to the NICUs, often described by parents as unfamiliar, disturbing, and highly distressing environments [10,11,12].
According to the first aim, we analyzed the data to investigate whether the levels of distress in preterm babies’ parents could differ after the intervention of pictorial humanization. Contrary to our hypotheses, no significant differences emerged between the two groups of parents, suggesting that the intervention was not related to global levels of parental distress nor to single dimensions. A possible explanation could be related to the high scores of global distress displayed by parents; the emotional experience of being a parent after infant hospitalization in the NICU is complex and intense [1,2,3,4,17] and could conceal the potential benefits of this kind of intervention. Indeed, looking at the VRS continuous scores in comparison with the VRS scores which emerged from other studies, we found a more intense distress than that of the normative population [67,75,78,79], and of hospital patients, such as women undergoing to breast cancer screening [67] and parents of children undergoing anesthesia for day-hospital surgery [13]. Moreover, the effect of other factors should be taken into consideration; variables related to infant or parents’ condition (i.e., infant gestational age, reason of admission, age, gender), could reduce the effect of the intervention. Further studies should be recommended in order to explore the possible role of these variables.
According to the second aim, we assessed the impact of pictorial humanization intervention on parental affective perception of the NICU, finding a significant effect. Indeed, in almost all scales of QAL significant differences emerged between groups, with more positive outcomes for the PHG parents. This result is consistent with previous studies [49,67,86] and, specifically, with those regarding pediatrics patients’ parents [54,70]. In the present study we found, in particular, that the scores for all negative subscales of QAL (distressing, unpleasant, gloomy and sleepy) were significantly lower after the implementation of intervention. This result has clinical implications, suggesting that this intervention may reduce the sense of unfamiliarity and discomfort reported by parents during their stay in the NICU [10,11,12]. This explanation is further supported by the fact that parents, after the pictorial humanization, obtained higher scores at three of the positive QAL subscales: pleasant, exciting, and arousing. This finding suggests that the parents perceived the NICU environment as a more comfortable place.
Nevertheless, no differences emerged in the case of the relaxing subscale. We could suppose that this result is related to the highly distressing experience of having an infant hospitalized in the NICU. Monti et al. [70] have previously suggested that the severity of the child’s health condition could influence the effects of this kind of intervention. Indeed, despite the parents of their sample displaying significant differences in all the subscales of QAL (globally an improvement after the pictorial humanization), in the case of the exciting subscale the improvement was significant only for parents of children with less severe health conditions, compared to parents whose infants showed chronic illness. Authors suggested that, due to the high level of stress experienced by these last parents, the improvement given by the intervention could be less effective. Considering our results, this explanation could be relevant too, given that all the infants of our sample were experiencing severe health problems due to their prematurity. The difference of significance in QAL subscales of the two studies (exciting vs. relaxing) could be related to the fact the study by Monti et al. [70] regarded the affective perception of a Pediatric Unit including a wide range of child ages (up to 11 years), while our study focused on the NICU environment and included only preterm babies.
Taken together, these results seemed to suggest that the intervention of pictorial humanization is associated with the affective perception of environment but not with parental distress. If this result support the importance of creating more suitable environments for patients and their families [49,87], it should also be considered in addition to approaches focused on patient affective states, especially in contexts where hospitalization is an extremely stressful experience.
Finally, we investigated whether the dimensions of affective parental perception could predict the level of parental distress. The regression model showed that a positive affective perception of environment could significantly contribute to the global level of parental well-being; specifically, distress decreased when parents perceived a more relaxing environment. This result is consistent with previous studies [39,49,88], where guidelines for the contents of pictorial humanization suggested that this intervention should include elements able to promote quietness and restoration. Conversely, colors or themes that could highly stimulate patients were not recommended, because this could increase agitation and worsen health and emotional states [39,49,88].
Interestingly, despite no effects of the intervention on parental distress emerged when MANOVAs were employed, pictorial intervention showed a significant effect in regression analysis, suggesting that parents belonging to control their condition had a higher probability of displaying a high VRS total score. Therefore, despite the humanized environment itself being unable to directly affect parental distress, its impact could emerge only when a positive affective perception of environment was also considered.
Finally, the regression model including QAL negative scales did not reach statistical significance. This unexpected result seemed to suggest that the positive dimensions of affective perceptions of environment contribute more to parental distress than negative ones. Nevertheless, given the exploratory aim of this investigation, and the small size of our analyses, these results should be considered in further investigations in order to be confirmed.
Although promising, the present study results should be considered as preliminary, and some limitations of the study should be noted. First, the results need to be confirmed on larger samples. Despite the sample was large enough to guarantee the sensitivity of our analyses [88,89], the power of the analyses was low, and the testing of more sophisticated hypotheses was not possible [90]. Second, future studies are needed to confirm the results while also controlling for the effects of other variables. Indeed, specific characteristics of parents and infants (i.e., parental age or gender, reason of hospitalization, severity of conditions) could play a relevant role in influencing parental affective reactions [13,17,70]: therefore, all these variables need to be considered for their possible influences on the outcomes. Another limitation of this study relates to the absence of data about the specific characteristics of pictorial intervention. Previous studies [39,48,91] identified the specificity of the effects of the colors, size (single paintings vs. wall coverage) and content (simple images vs. natural landscapes) of pictorial humanization. While we were not able to collect data on the specific elements of the pictorial representations, we are aware that a future study should also investigate this issue.
Notwithstanding the limitations above, the strength of our study is the implementation of pictorial intervention in an NICU, contributing towards making it a suitable environment for fostering the activation of parental resilience rather than simply as a stressor.
Future studies and replications are, however, needed to generalize the results and support further recommendations for clinical care.
5. Conclusions
The present study investigated the possible benefits of pictorial humanization on parental distress and affective perception of environment during infant hospitalization in the NICU. In summary, positive effects of the pictorial intervention were found. Indeed, despite no change in parental distress emerging after implementation of the intervention, it ultimately proved to be a significant contributing factor towards parental states of mind, along with the perception of a highly relaxing environment.
Overall, these results extend previous studies on the effects of pictorial humanization, including the NICU as a hospital ward that could benefit from this intervention. The innovative aspect of our study relates to the implementation of pictorial intervention in a ward recognized as potentially traumatic for parents; coping with the infant hospitalization in the NICU means that the parents have to deal with mixed feelings, ranging from fear of death to optimism, from uncertainty and instability to trust and sense of stability. Therefore, these parents may need special support, fostering the development and the strengthening of emotional resources. More generally, these considerations could suggest the relevance of proposing this kind of intervention in several contexts where parental stress is high, beyond child hospitalization, to support parental adjustment. In this sense, the present study has potential clinical and practical implications for the care of families. The perception of the hospital environment as a cold or hostile place might increase the risk of emotional burden and psychological discomfort for parents. Conversely, a humanized environment could facilitate engagement in behaviors and emotions that support the healing process [92]. Therefore, these parents could regard themselves as being in a warmer and human-friendly environment; in other words, “a place to go, not to stay” [91] (p. 372).
Author Contributions
Conceptualization, E.N., A.B. and F.A.; Data curation, M.S., F.G. and A.P.; Formal analysis, E.N.; Methodology, E.N., M.S., A.B. and F.A.; Supervision, E.N., M.S., A.B. and F.A.; Writing—original draft, E.N., F.A., F.G. and A.P.; Writing—review & editing, E.N., F.A., F.G. and A.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and ethically reviewed and approved by the Head of the Neonatal Intensive Care Unit, Bufalini Hospital, Cesena, Italy.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available upon request due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Montirosso, R.; Provenzi, L.; Calciolari, G.; Borgatti, R.; NEO-ACQUA Study Group. Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatr. 2012, 101, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Clottey, M.; Dillard, D.M. Post-traumatic stress disorder and neonatal intensive care. Int. J. Childbirth Educ. 2013, 28, 23–29. [Google Scholar]
- Neri, E.; Agostini, F.; Salvatori, P.; Biasini, A.; Monti, F. Mother-preterm infant interactions at 3 months of corrected age: Influence of maternal depression, anxiety and neonatal birth weight. Front. Psychol. 2015, 6, 1234. [Google Scholar] [CrossRef] [Green Version]
- Neri, E.; Giovagnoli, S.; Genova, F.; Benassi, M.; Stella, M.; Agostini, F. Reciprocal influence of depressive symptoms between mothers and fathers during the first postpartum year: A comparison among full-term, very low, and extremely low birth weight infants. Front. Psychiatry 2020, 11, 578264. [Google Scholar] [CrossRef] [PubMed]
- Seideman, R.Y.; Watson, M.A.; Corff, K.E.; Odle, P.; Haase, J.; Bowerman, J.L. Parent stress and coping in NICU and PICU. J. Pediatric Nurs. 1997, 12, 169–177. [Google Scholar] [CrossRef]
- Muller-Nix, C.; Forcada-Guex, M.; Pierrehumbert, B.; Jaunin, L.; Borghini, A.; Ansermet, F. Prematurity, maternal stress and mother-child interactions. Early Hum. Dev. 2004, 79, 145–158. [Google Scholar] [CrossRef]
- Neri, E.; Genova, F.; Monti, F.; Trombini, E.; Biasini, A.; Stella, M.; Agostini, F. Developmental dimensions in preterm infants during the first year of life: The influence of severity of prematurity and maternal generalized anxiety. Front. Psychol. 2020, 11, 455. [Google Scholar] [CrossRef] [Green Version]
- Zdun-Ryżewska, A.; Nadrowska, N.; Błażek, M.; Białek, K.; Zach, E.; Krywda-Rybska, D. Parent’s Stress Predictors during a Child’s Hospitalization. Int. J. Environ. Res. Public Health 2021, 18, 12019. [Google Scholar] [CrossRef]
- Miles, M.S.; Funk, S.G.; Carlson, J. Parental Stressor Scale: Neonatal intensive care unit. Nurs. Res. 1993, 42, 148–152. [Google Scholar] [CrossRef]
- Grosik, C.; Snyder, D.; Cleary, G.M.; Breckenridge, D.M.; Tidwell, B. Identification of internal and external stressors in parents of newborns in intensive care. Perm. J. 2013, 17, 36–41. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez-Rey, R.; Alonso-Tapia, J.; Colville, G. Prediction of parental posttraumatic stress, anxiety and depression after a child’s critical hospitalization. J. Crit. Care 2018, 45, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Palomares, M.; Fernandez-Rejano, M.; Garrido-Ardila, E.M.; Montanero-Fernandez, J.; Oliva-Ruiz, P.; Rodriguez-Mansilla, J. The Impact of a Preterm Baby Arrival in a Family: A Descriptive Cross-Sectional Pilot Study. J. Clin. Med. 2021, 10, 4494. [Google Scholar] [CrossRef] [PubMed]
- Agostini, F.; Monti, F.; Neri, E.; Dellabartola, S.; de Pascalis, L.; Bozicevic, L. Parental anxiety and stress before pediatric anesthesia: A pilot study on the effectiveness of preoperative clown intervention. J. Health Psychol. 2014, 19, 587–601. [Google Scholar] [CrossRef] [PubMed]
- Neri, E.; De Pascalis, L.; Agostini, F.; Genova, F.; Biasini, A.; Stella, M.; Trombini, E. Parental Book-Reading to Preterm Born Infants in NICU: The Effects on Language Development in the First Two Years. Int. J. Environ. Res. Public Health 2021, 18, 11361. [Google Scholar] [CrossRef]
- Ramírez, M.; Navarro, S.; Clavería, C.; Molina, Y.; Cox, A. Estresores parentales en Unidad de Cuidados Intensivos Pediátricos [Parental stressors in a Pediatric Intensive Care Unit]. Rev. Chil. Pediatr. 2018, 89, 182–189. [Google Scholar] [CrossRef] [Green Version]
- Grunberg, V.A.; Geller, P.A.; Hoffman, C.; Njoroge, W.; Ahmed, A.; Patterson, C.A. Parental mental health screening in the NICU: A psychosocial team initiative. J. Perinatol. 2022, 42, 401–409. [Google Scholar] [CrossRef]
- Genova, F.; Neri, E.; Trombini, E.; Stella, M.; Agostini, F. Severity of preterm birth and perinatal depressive symptoms in mothers and fathers: Trajectories over the first postpartum year. J. Affect. Disord. 2022, 298, 182–189. [Google Scholar] [CrossRef]
- Gondwe, K.W.; Holditch-Davis, D. Posttraumatic stress symptoms in mothers of preterm infants. Int. J. Afr. Nurs. Sci. 2015, 3, 8–17. [Google Scholar] [CrossRef] [Green Version]
- Baía, I.; Amorim, M.; Silva, S.; Kelly-Irving, M.; de Freitas, C.; Alves, E. Parenting very preterm infants and stress in Neonatal Intensive Care Units. Early Hum. Dev. 2016, 101, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Salomè, S.; Mansi, G.; Lambiase, C.V.; Barone, M.; Piro, V.; Pesce, M.; Sarnelli, G.; Raimondi, F.; Capasso, L. Impact of psychological distress and psychophysical wellbeing on posttraumatic symptoms in parents of preterm infants after NICU discharge. Ital. J. Pediatrics 2022, 48, 13. [Google Scholar] [CrossRef]
- Schuetz Haemmerli, N.; Lemola, S.; Holditch-Davis, D.; Cignacco, E. Comparative Evaluation of Parental Stress Experiences Up to 2 to 3 Years After Preterm and Term Birth. Adv. Neonatal Care Off. J. Natl. Assoc. Neonatal Nurses 2020, 20, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Cummings, E.M.; Keller, P.S.; Davies, P.T. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. J. Child. Psychol. Psychiatry 2005, 46, 479–489. [Google Scholar] [CrossRef] [PubMed]
- De Cock, D.; Birmingham, L.; Watson, K.D.; Kearsley-Fleet, L.; Symmons, D.P.; Hyrich, K.L. Pregnancy outcomes in women with rheumatoid arthritis ever treated with rituximab. Rheumatology 2017, 56, 661–663. [Google Scholar] [CrossRef] [Green Version]
- Woodward, L.J.; Bora, S.; Clark, C.A.; Montgomery-Honger, A.; Pritchard, V.E.; Spencer, C.; Austin, N.C. Very preterm birth: Maternal experiences of the neonatal intensive care environment. J. Perinatol. 2014, 34, 555–561. [Google Scholar] [CrossRef] [Green Version]
- Power, N.; Franck, L. Parent participation in the care of hospitalized children: A systematic review. J. Adv. Nurs. 2008, 62, 622–641. [Google Scholar] [CrossRef]
- Jee, R.A.; Shepherd, J.R.; Boyles, C.E.; Marsh, M.J.; Thomas, P.W.; Ross, O.C. Evaluation and comparison of parental needs, stressors, and coping strategies in a pediatric intensive care unit. Pediatric Crit. Care Med. 2012, 13, e166–e172. [Google Scholar] [CrossRef]
- Neri, E.; Agostini, F.; Baldoni, F.; Facondini, E.; Biasini, A.; Monti, F. Preterm infant development, maternal distress and sensitivity: The influence of severity of birth weight. Early Hum. Dev. 2017, 106–107C, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Bujnowska, A.M.; Rodriguez, C.; Garcia, T.; Areces, D.; Marsh, N.V. Parenting and Future Anxiety: The Impact of Having a Child with Developmental Disabilities. Int. J. Environ. Res. Public Health 2019, 16, 668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandoval-Obando, E.; Alcaide, M.; Salazar-Munoz, M.; Pena-Troncoso, S.; Hernandez-Mosqueira, C.; Gimenez-Serrano, S. Raising Children in Risk Neighborhoods from Chile: Examining the Relationship between Parenting Stress and Parental Adjustment. Int. J. Environ. Res. Public Health 2021, 19, 45. [Google Scholar] [CrossRef]
- Brett, J.; Staniszewska, S.; Newburn, M.; Jones, N.; Taylor, L. A systematic mapping review of effective interventions for communicating with, supporting and providing information to parents of preterm infants. BMJ Open 2011, 1, e000023. [Google Scholar] [CrossRef] [PubMed]
- Penny, K.; Friedman, S.; Halstead, G. Psychiatric support for mothers in the Neonatal Intensive Care Unit. J. Perinatol. 2015, 35, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Treyvaud, K.; Spittle, A.; Anderson, P.J.; O’Brien, K. A multilayered approach is needed in the NICU to support parents after the preterm birth of their infant. Early Hum. Dev. 2019, 139, 104838. [Google Scholar] [CrossRef] [PubMed]
- Matricardi, S.; Agostino, R.; Fedeli, C.; Montirosso, R. Mothers are not fathers: Differences between parents in the reduction of stress levels after a parental intervention in a NICU. Acta Paediatr. 2013, 102, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, T.; Cluxton-Keller, F.; Vullo, G.C.; Tandon, S.D.; Noazin, S. NICU-based Interventions to Reduce Maternal Depressive and Anxiety Symptoms: A Meta-analysis. Pediatrics 2017, 139, e20161870. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sabnis, A.; Fojo, S.; Nayak, S.S.; Lopez, E.; Tarn, D.M.; Zeltzer, L. Reducing parental trauma and stress in neonatal intensive care: Systematic review and meta-analysis of hospital interventions. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2019, 39, 375–386. [Google Scholar] [CrossRef]
- Bedford, Z.; Bench, S. Reviewing interventions supporting parents’ well-being after a child’s intensive care unit discharge. Nurs. Crit. Care 2019, 24, 153–161. [Google Scholar] [CrossRef]
- World Health Organization. Ottawa Charter for Health Promotion; World Health Organization, Regional Office for Europe: Geneva, Switzerland, 1986. [Google Scholar]
- Ulrich, R.S. Effects of interior design on wellness: Theory and recent scientific research. J. Health Care Inter. Des. 1991, 3, 97–109. [Google Scholar]
- Iyendo, T.O.; Uwajeh, P.C.; Ikenna, E.S. The therapeutic impacts of environmental design interventions on wellness in clinical settings: A narrative review. Complementary Ther. Clin. Pract. 2016, 24, 174–188. [Google Scholar] [CrossRef]
- Evans, G.W.; McCoy, M.J. When buildings don’t work: The role of architecture in human health. J. Environ. Psychol. 1998, 18, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Nagasawa, Y. The geography of hospitals: A developing approach to the architectural planning of hospitals. In Theoretical Perspectives in Environment-Behavior Research; Wapner, S., Demick, J., Eds.; Kluwer Academic: New York, NY, USA, 2000; pp. 217–227. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Zimring, C.; Barch, X.Z.; Dubose, J.; Seo, H.B.; Choi, Y.S.; Quan, X.; Joseph, A. A review of the research literature on evidence-based healthcare design. Health Environ. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef]
- Gao, C.; Zhang, S. The restorative quality of patient ward environment: Tests of six dominant design characteristics. Build. Environ. 2020, 180, 107039. [Google Scholar] [CrossRef]
- Kaplan, S.; Kaplan, R. Health, supportive environments, and the Reasonable Person Model. Am. J. Public Health 2003, 93, 1484–1489. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.A. The physical environment and patient care. Annu. Rev. Nurs. Res. 1988, 6, 61–84. [Google Scholar] [CrossRef] [PubMed]
- Malkin, J. Creating excellence in healthcare design. J. Health Care Inter. Des. 1991, 3, 27–41. [Google Scholar]
- Verderber, S.; Fine, D.J. Healthcare Architecture in an Era of Radical Transformation; Yale University Press: New Haven, CT, USA, 2000. [Google Scholar] [CrossRef]
- Pressly, P.K.; Heesacker, M. The Physical Environment and Counseling: A Review of Theory and Research. J. Couns. Dev. 2001, 79, 148–160. [Google Scholar] [CrossRef]
- Devlin, A.S.; Arneill, A.B. Health care environments and patient outcomes: A review of the literature. Environ. Behav. 2003, 35, 665–694. [Google Scholar] [CrossRef]
- Ulrich, R.S. How design impacts wellness. Healthc. Forum J. 1992, 35, 20–25. [Google Scholar]
- Ulrich, R.S. Effects of viewing art on health outcomes. In Putting Patients First: Best Practices in Patient Centered-Care, 2nd ed.; Frampton, S.B., Charmel, P.A., Eds.; Jossey Bass: San Francisco, CA, USA, 2009. [Google Scholar]
- Pearson, M.; Gaines, K.; Pati, D.; Colwell, M.; Motheral, L.; Adams, N.G. The Physiological Impact of Window Murals on Pediatric Patients. HERD Health Environ. Res. Des. J. 2019, 12, 116–129. [Google Scholar] [CrossRef]
- Dalke, H.; Little, J.; Niemann, E.; Camgoz, N.; Steadman, G.; Hill, S.; Stott, L. Colour and lighting in hospital design. Opt. Laser Technol. 2006, 38, 343–365. [Google Scholar] [CrossRef]
- Monti, F.; Agostini, F.; Lupi, F.; Gobbi, F.; Pocecco, M. Effetto dell’umanizzazione pittorica sulla percezione delle qualità affettive dell’ambiente in un reparto di pediatria. [Effect of pictorial humanization on affective qualities in a Paediatric Unit]. Psicol. Della Salut. 2008, 2, 125–146. [Google Scholar] [CrossRef]
- Stuckey, H.L.; Nobel, J. The connection between art, healing, and public health: A review of current literature. Am. J. Public Health 2010, 100, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Kirkby, M. Nature as a refuge in children’s environments. Child. Environ. Q. 1989, 6, 7–12. [Google Scholar]
- Appleton, J. The Experience of Landscape, Revised ed.; John Wiley: New York, NY, USA, 1996. [Google Scholar]
- Whitehouse, S.; Varni, J.; Seid, M.; Cooper-Marcus, C.; Ensberg, M.; Jacobs, J.; Mehlenbeck, R. Evaluating a children’s hospital garden environment: Utilization and consumer satisfaction. J. Environ. Psychol. 2001, 21, 301–314. [Google Scholar] [CrossRef] [Green Version]
- Bonaiuto, M.; Bonnes, M.; Parenti, M.E.; Rabazzi, A. Gli effetti dell’umanizzazione dell’ospedale pediatrico sugli utenti. Progett. La Sanità 2001, 64, 54–60. [Google Scholar]
- Fornara, F. La valutazione ambientale multidimensionale: Il caso dei luoghi ospedalieri. La Prof. Di Psicol. 2004, 2, 67–70. [Google Scholar]
- Douglas, C.; Steele, A.; Todd, S.; Douglas, M. Primary care trusts. A room with a view. Health Serv. J. 2002, 112, 28–29. [Google Scholar]
- Ulrich, R.; Zimring, C.; Quan, X.; Joseph, A.; Choudhary, R. The Role of the Physical Environment in the Hospital of the 21st Century: A Once-in-a-Lifetime Opportunity; The Center for Health Design: Concord, CA, USA, 2004. [Google Scholar]
- Caspari, S.; Eriksson, K.; Naden, D. The aesthetic dimension in hospitals--an investigation into strategic plans. Int. J. Nurs. Stud. 2006, 43, 851–859. [Google Scholar] [CrossRef]
- Rollins, J.; Sonke, J.; Cohen, R.; Boles, A.; Li, J. State of the Field Report: Arts in Healthcare; Society for Arts in Healthcare: Washington, DC, USA, 2009. [Google Scholar]
- Nanda, U.; Eisen, S.; Zadeh, R.S.; Owen, D. Effect of visual art on patient anxiety and agitation in a mental health facility and implications for the business case. J. Psychiatr. Ment. Health Nurs. 2011, 18, 386–393. [Google Scholar] [CrossRef]
- Beukeboom, C.J.; Langeveld, D.; Tanja-Dijkstra, K. Stress-reducing effects of real and artificial nature in a hospital waiting room. J. Altern. Complement Med. 2012, 18, 329–333. [Google Scholar] [CrossRef]
- Agostini, F.; Neri, E.; Sfondrini, M.S.; Pedilarco, S.; Galotti, S.; Monti, F.; Minelli, M. Percezione delle qualità affettive ambientali e livello di stress in Radiologia Senologica: Effetto di un intervento di Umanizzazione Pittorica. Psicol. Della Salut. 2018, 3, 95–113. [Google Scholar] [CrossRef]
- McCabe, C.; Roche, D.; Hegarty, F.; McCann, S. ‘Open Window’: A randomized trial of the effect of new media art using a virtual window on quality of life in patients’ experiencing stem cell transplantation. Psycho-Oncology 2013, 22, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Eisen, S.L.; Ulrich, R.S.; Shepley, M.M.; Varni, J.W.; Sherman, S. The stress-reducing effects of art in pediatric health care: Art preferences of healthy children and hospitalized children. J. Child Health Care Prof. Work. Child. Hosp. Community 2008, 12, 173–190. [Google Scholar] [CrossRef] [PubMed]
- Monti, F.; Agostini, F.; Dellabartola, S.; Neri, E.; Bozicevic, L.; Pocecco, M. Pictorial intervention in a pediatric hospital environment: Effects on parental affective perception of the unit. J. Environ. Psychol. 2012, 32, 216–224. [Google Scholar] [CrossRef]
- Biddiss, E.; McPherson, A.; Shea, G.; McKeever, P. The design and testing of interactive hospital spaces to meet the needs of waiting children. HERD Health Environ. Res. Des. J. 2013, 6, 49–68. [Google Scholar] [CrossRef] [PubMed]
- Leonard, A.L.; Verster, A.; Coetzee, M. Developing family-friendly signage in a south African paediatric healthcare setting. Curationis 2014, 37, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, J.A.; Pratt, G. A description of the affective quality attributed to environments. J. Personal. Soc. Psychol. 1980, 38, 311–322. [Google Scholar] [CrossRef]
- Ittelson, W.H. Environment and Cognition; Academic Press: New York, NY, USA, 1973. [Google Scholar]
- Tarsitani, L.; Biondi, M. Sviluppo e validazione della scala VRS Valutazione rapida dello stress. Med. Psicosom. 1999, 44, 163–178. [Google Scholar]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal and Coping; Springer Publishing Company: New York, NY, USA, 1984. [Google Scholar]
- Mandarelli, G.; Tarsitani, L.; Tarolla, E.; Robone, C.; Battisti, F.; Picardi, A.; Biondi, M. Stress soggettivo, stato di salute autovalutato e supporto sociale in una popolazione non clinica. Med. Psicosom. 2004, 49, 93–96. [Google Scholar]
- Tomei, G.; Cherubini, E.; Ciarrocca, M.; Biondi, M.; Rosati, M.V.; Tarsitani, L.; Capozzella, A.; Monti, C.; Tomei, F. Assessment of subjective stress in the municipal police force at the start and at the end of the shift. Stress Health: J. Int. Soc. Investig. Stress 2006, 22, 239–247. [Google Scholar] [CrossRef]
- Perugini, M.; Bonnes, M.; Aiello, A.; Ercolani, A.P. Il modello circonflesso delle qualità affettive dei luoghi: Sviluppo di uno strumento valutativo italiano [The circumflex world of affective qualities of places: Development of an Italian evaluative tool]. Test. Psicoter. Metodol. 2002, 9, 131–152. [Google Scholar]
- Russell, J.A.; Ward, L.; Pratt, G. Affective quality attributed to environments: A factor analytic study. Environ. Behav. 1981, 13, 259–288. [Google Scholar] [CrossRef]
- Russell, J.A.; Lanius, U.F. Adaptation level and the affective appraisal of environments. J. Environ. Psychol. 1984, 4, 119–135. [Google Scholar] [CrossRef]
- Austin, P.C.; Steyerberg, E.W. The number of subjects per variable required in linear regression analyses. J. Clin. Epidemiol. 2015, 68, 627–636. [Google Scholar] [CrossRef] [Green Version]
- Henley, S.S.; Golden, R.M.; Kashner, T.M. Statistical modeling methods: Challenges and strategies. Biostat. Epidemiol. 2020, 4, 105–139. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, D.G.; Quintana-Ascencio, P.F. A solution to minimum sample size for regressions. PLoS ONE 2020, 15, e0229345. [Google Scholar] [CrossRef] [Green Version]
- Mick, R.; Ratain, M.J. Bootstrap validation of pharmacodynamic models defined via stepwise linear regression. Clin. Pharmacol. Ther. 1994, 56, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.P.; Diehr, P.; Conrad, D.A.; Davis, J.H.; Leickly, R.; Perrin, E.B. Randomized trial of a patient-centered hospital unit. Patient Educ. Couns. 1998, 34, 125–133. [Google Scholar] [CrossRef]
- Sherman, S.A.; Varni, J.W.; Ulrich, R.S.; Malcarned, V.L. Post-occupancy evaluation of healing gardens in a pediatric cancer center. Landsc. Urban Plan. 2005, 73, 167–183. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Pérez, J.F.G.; Navarro, D.F.; Llobell, J.P. Statistical power of Solomon design. Psicothema 1999, 11, 431–436. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, Rev. ed.; Lawrence Erlbaum Associates, Inc.: Hillsdale, NJ, USA, 1977. [Google Scholar]
- Rashid, M. Environmental Design for Patient Families in Intensive Care Units. J. Healthc. Eng. 2010, 1, 862962. [Google Scholar] [CrossRef]
- Mohammad Moradi, B.; Sobhanardakani, S.; Cheraghi, M. Ecological risk of heavy metals in surface soils of urban parks. Iranian J. Health Environ. 2018, 10, 429–442. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).