Herbal Medicine Uses for Respiratory System Disorders and Possible Trends in New Herbal Medicinal Recipes during COVID-19 in Pasvalys District, Lithuania
Abstract
:1. Introduction
2. Materials and Methods
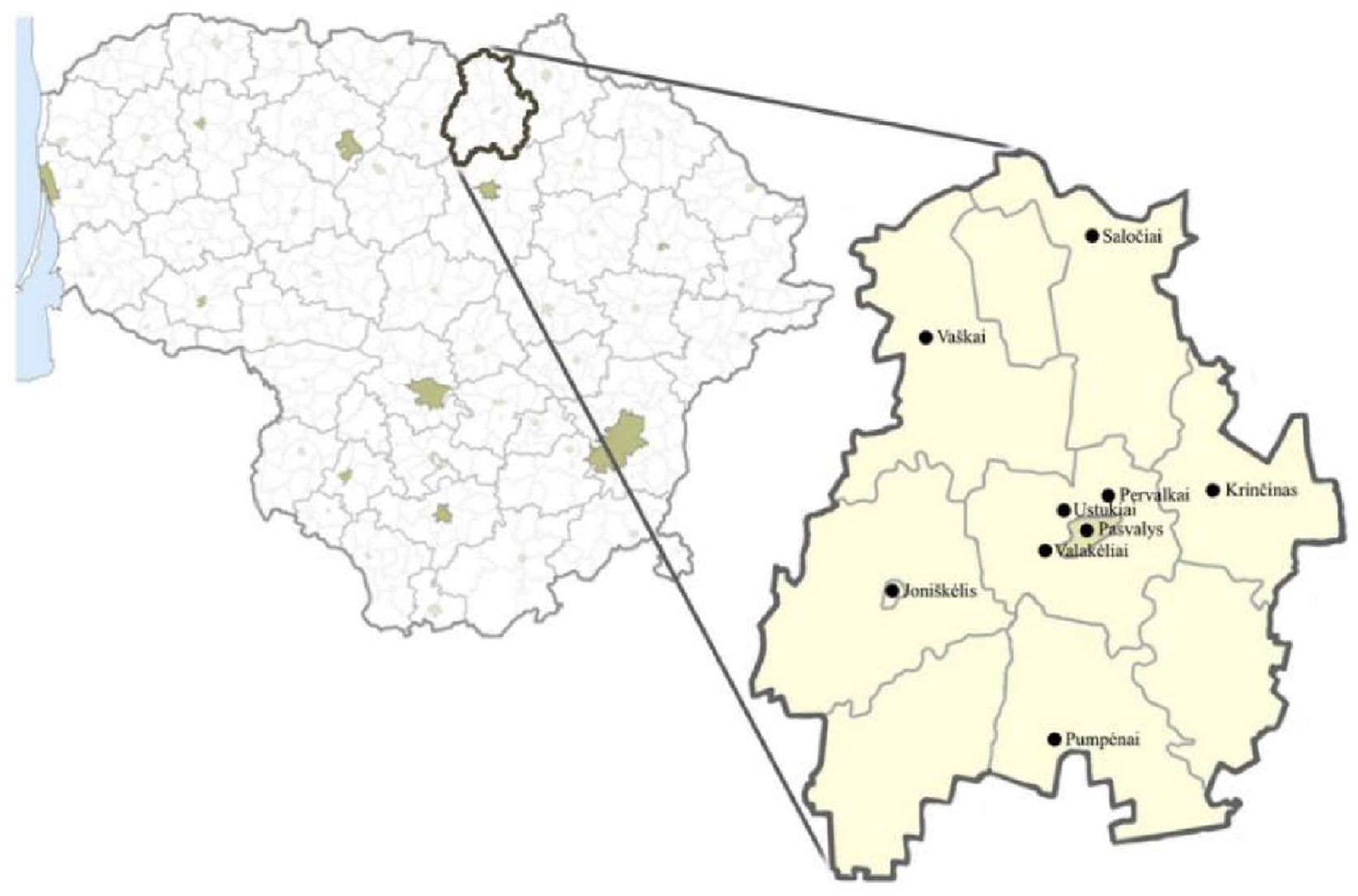
2.1. Study Area
2.2. Methods
Research Organization, Respondents, and Methods
3. Results and Discussion
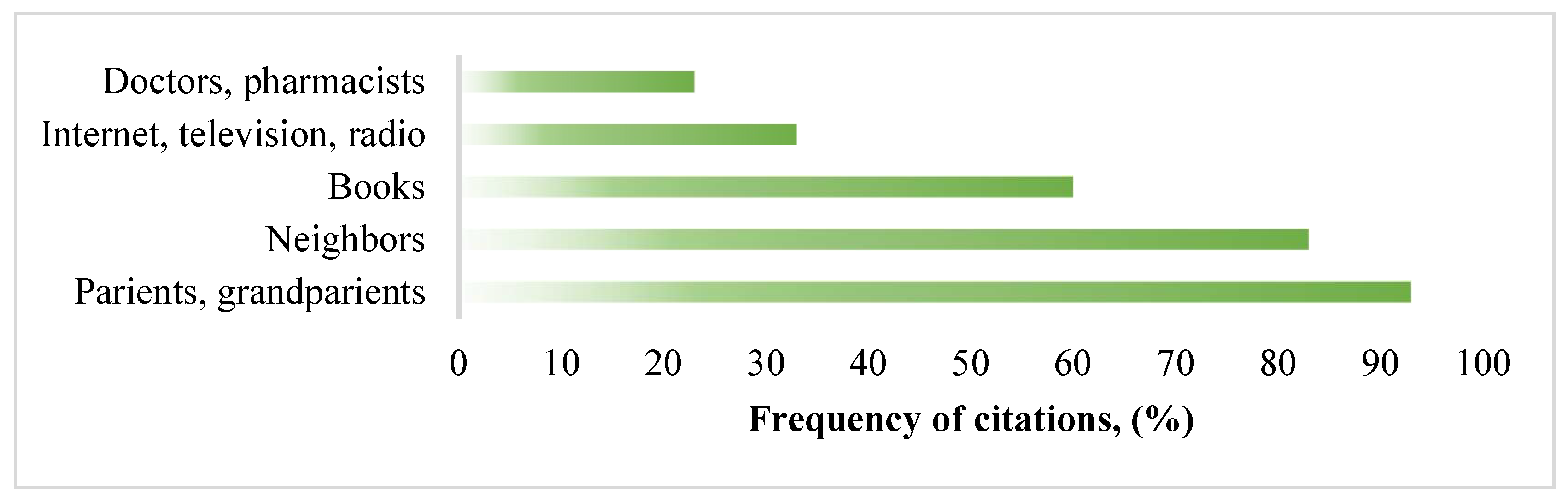
3.1. Demographic Characteristics of Respondents and Sources of Ethnobotanical Knowledge
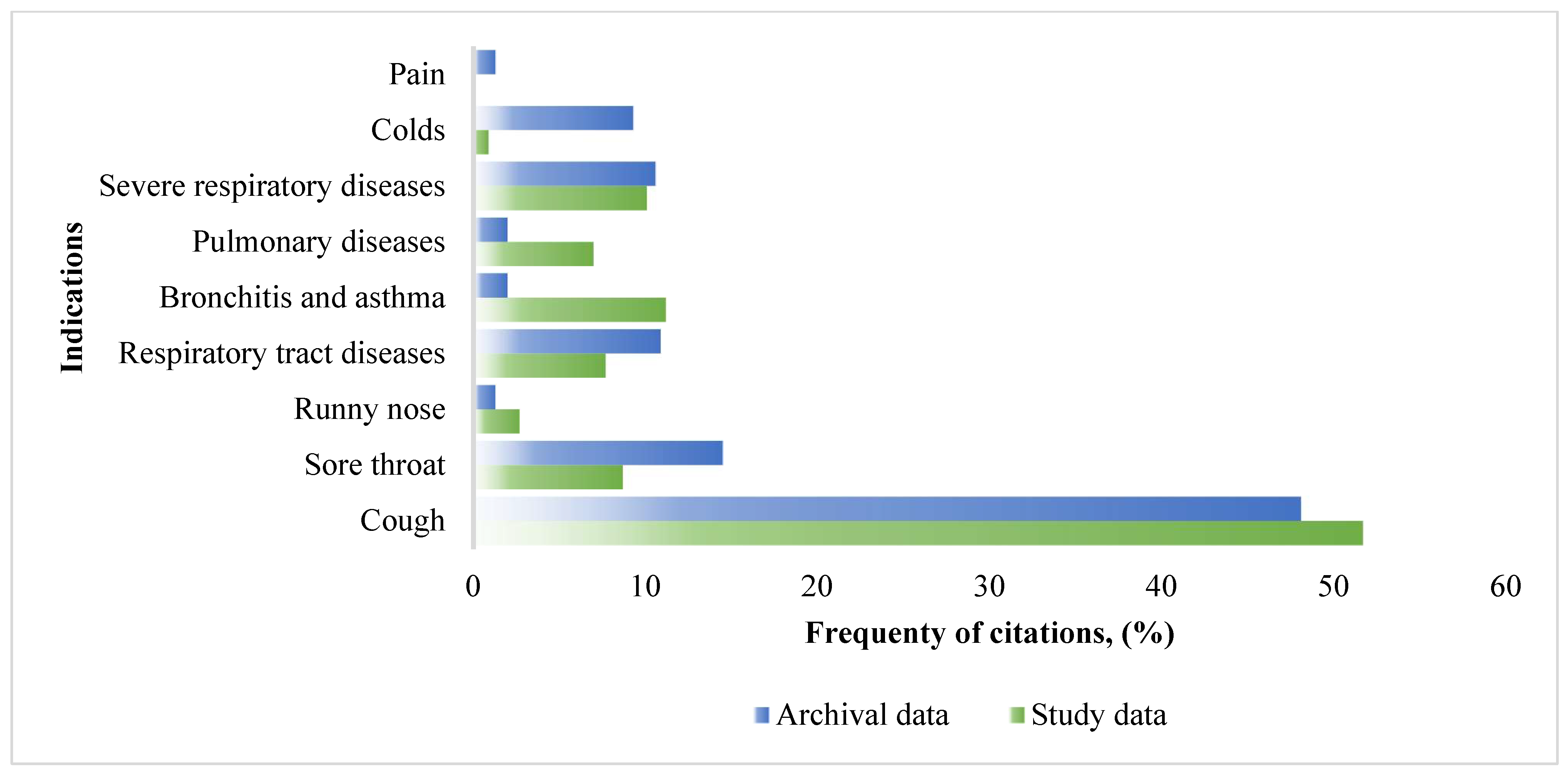
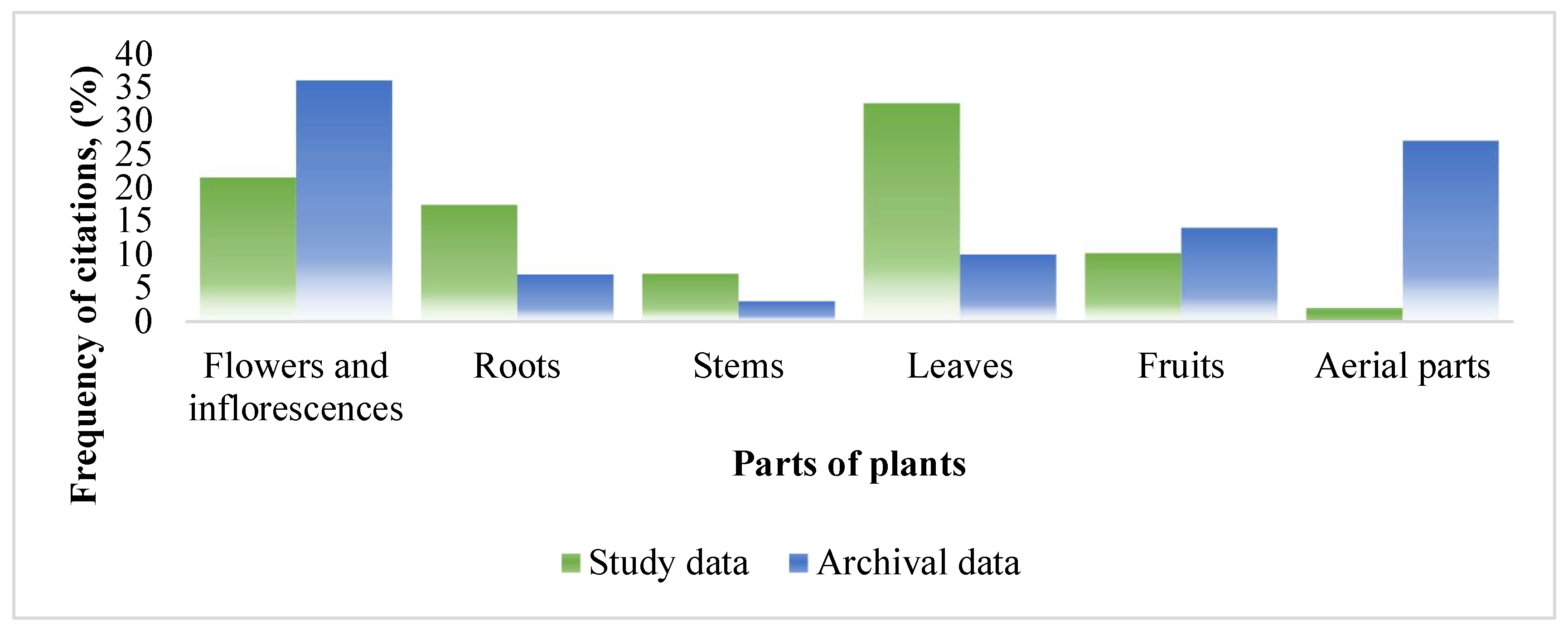
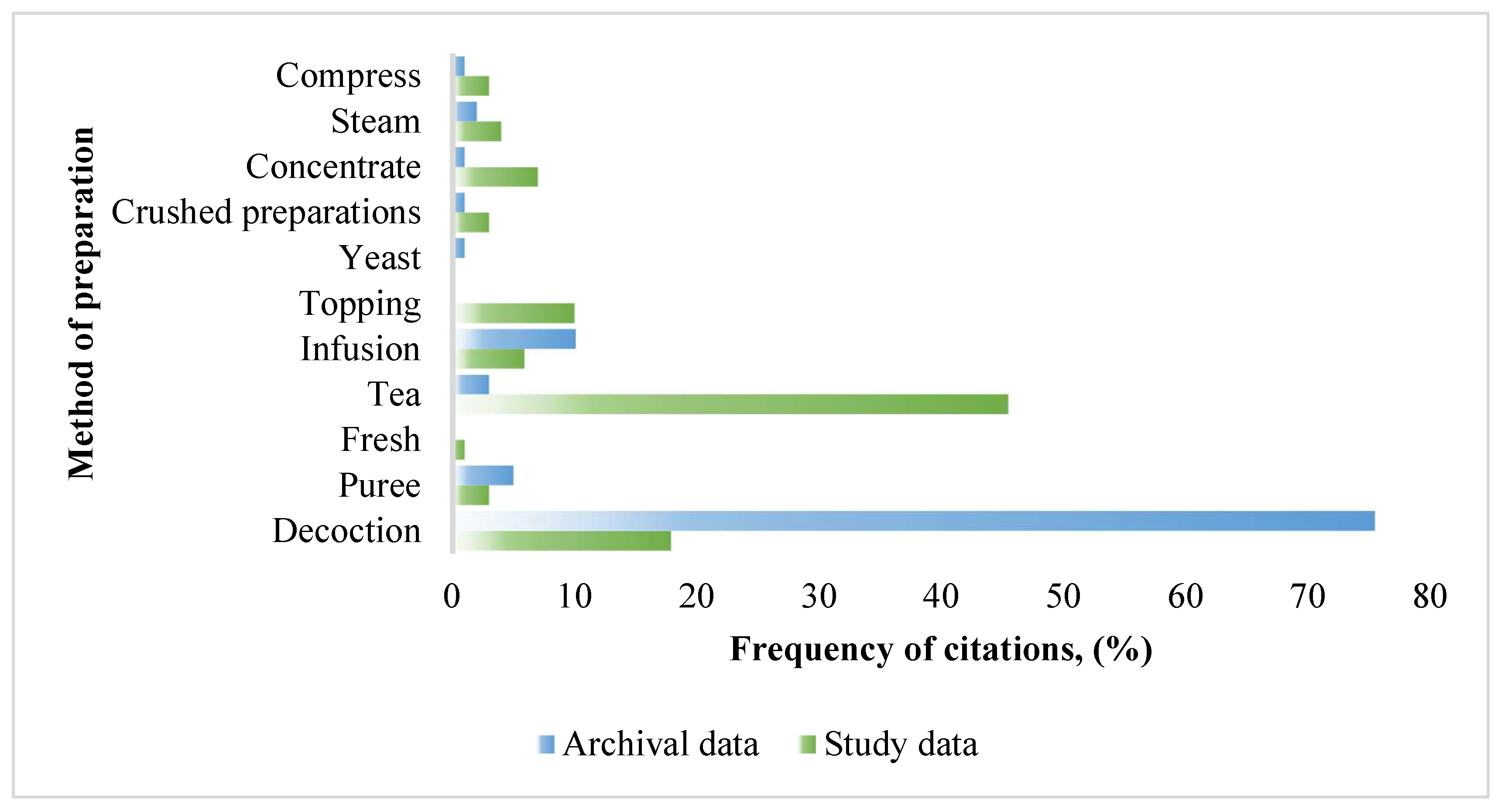
3.2. Indications for Use, the Most Popular Plants and Their Parts, Methods of Preparation
3.3. Safety of Herbal Raw Materials and Possible Trends in New Herbal Medicinal Recipes
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wangkheirakpam, S. Traditional and Folk Medicine as a Target for Drug Discovery. In Natural Products and Drug Discovery; Elsevier Ltd.: Amsterdam, The Netherlands, 2018; Chapter 2; pp. 29–56. [Google Scholar]
- Gukauskiene, L.; Juknyte, K. Lithuanian population attitude to herbal medicine. Int. J. Pharm. Chem. Biol. Sci. 2019, 9, 146–150. [Google Scholar]
- Alarcomicronn, R.; Pardo-de-Santayana, M.; Priestley, C.; Morales, R.; Heinrich, M. Medicinal and local food plants in the south of Alava (Basque Country, Spain). J. Ethnopharmacol. 2015, 176, 207–224. [Google Scholar] [CrossRef] [Green Version]
- Fontefrancesco, M.; Barstow, C.; Grazioli, F.; Lyons, H.; Mattalia, G.; Marino, M.; McKay, A.E.; Soukand, R.; Corvo, P.; Pieroni, A. Keeping or changing? Two different cultural adaptation strategies in the domestic use of home country food plant and herbal ingredients among Albanian and Moroccan migrants in Northwestern Italy. J. Ethnobiol. Ethnomed. 2019, 15, 11–17. [Google Scholar] [CrossRef]
- Aprilio, K.; Wilar, G. Emergence of Ethnomedical COVID-19 Treatment: A Literature Review. Infect. Drug Resist. 2021, 14, 4277–4289. [Google Scholar] [CrossRef]
- Cock, I.E.; Van Vuuren, S.F. The traditional use of southern African medicinal plants for the treatment of bacterial respiratory diseases: A review of the ethnobotany and scientific evaluations. J. Ethnopharmacol. 2020, 263, 113204. [Google Scholar] [CrossRef]
- Agbor, G.A.; Ndjib, R. Systematic Review of Plants Used Against Respiratory Diseases Related to COVID-19 in Africa. J. Drug Deliv. Ther. 2021, 11, 141–153. [Google Scholar] [CrossRef]
- Franco, F.M.; Bussmann, R.W. Rising to the occasion: Outlining Ethnobiologists’ response to the coronavirus (COVID-19) pandemic. Ethnobot. Res. Appl. 2020, 20. [Google Scholar] [CrossRef]
- Vandebroek, I.; Pieroni, A.; Stepp, J.R.; Hanazaki, N.; Ladio, A.; Alves, R.R.N.; Picking, D.; Delgoda, R.; Maroyi, A.; van Andel, T.; et al. Reshaping the future of ethnobiology research after the COVID-19 pandemic. Nat. Plants 2020, 6, 723–730. [Google Scholar] [CrossRef]
- Cordoba-Tovar, L.; Ríos-Geovo, V.; Largacha-Viveros, M.F.; Salas-Moreno, M.; Marrugo-Negrete, J.L.; Ramos, P.A.; Chaverra, L.M.; Jonathan, M.P. Cultural belief and medicinal plants in treating COVID 19 patients of Western Colombia. Acta Ecol. Sin. 2021. [Google Scholar] [CrossRef]
- Villena-Tejada, M.; Vera-Ferchau, I.; Cardona-Rivero, A.; Zamalloa-Cornejo, R.; Quispe-Florez, M.; Frisancho-Triveño, Z.; Abarca-Meléndez, R.C.; Alvarez-Sucari, S.G.; Mejia, C.R.; Yañez, J.A. Use of medicinal plants for COVID-19 prevention and respiratory symptom treatment during the pandemic in Cusco, Peru: A cross-sectional survey. PLoS ONE 2021, 16, e0257165. [Google Scholar] [CrossRef]
- Khadka, D.; Dhamala, M.K.; Li, F.; Aryal, P.C.; Magar, P.R.; Bhatta, S.; Thakur, M.S.; Basnet, A.; Cui, D.; Shi, S. The use of medicinal plants to prevent COVID-19 in Nepal. J. Ethnobiol. Ethnomed. 2021, 17, 26. [Google Scholar] [CrossRef] [PubMed]
- Pranskuniene, Z.; Ratkeviciute, K.; Simaitiene, Z.; Pranskunas, A.; Bernatoniene, J. Ethnobotanical Study of Cultivated Plants in Kaisiadorys District, Lithuania: Possible Trends for New Herbal Based Medicines. Evid. Based. Complement. Alternat Med. 2019, 2019, 3940397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pranskuniene, Z.; Dauliute, R.; Pranskunas, A.; Bernatoniene, J. Ethnopharmaceutical knowledge in Samogitia region of Lithuania: Where old traditions overlap with modern medicine. J. Ethnobiol. Ethnomed. 2018, 14, 70. [Google Scholar] [CrossRef] [PubMed]
- Pranskuniene, Z.; Bernatoniene, J.; Simaitiene, Z.; Pranskunas, A.; Mekas, T. Ethnomedicinal Uses of Honeybee Products in Lithuania: The First Analysis of Archival Sources. Evid. Based Complement. Alternat Med. 2016, 2016, 9272635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tilvikas, J. Lietuvininkų Liaudies Medicina Nuo XX a. Vidurio iki XXI a. Pradžios. 2017. Available online: http://www.ekgt.lt/media/dokumentai/veikla/Tyrimai/2017tyrimai/Tilvikas_tyrimas.pdf (accessed on 3 April 2022).
- Pieroni, A.; Vandebroek, I.; Prakofjewa, J.; Bussmann, R.W.; Paniagua-Zambrana, N.Y.; Maroyi, A.; Torri, L.; Zocchi, D.M.; Dam, A.T.K.; Khan, S.M.; et al. Taming the pandemic? The importance of homemade plant-based foods and beverages as community responses to COVID-19. J. Ethnobiol. Ethnomed. 2020, 16, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Alyami, H.S.; Orabi, M.A.A.; Aldhabbah, F.M.; Alturki, H.N.; Aburas, W.I.; Alfayez, A.I.; Alharbi, A.S.; Almasuood, R.A.; Alsuhaibani, N.A. Knowledge about COVID-19 and beliefs about and use of herbal products during the COVID-19 pandemic: A cross-sectional study in Saudi Arabia. Saudi Pharm. J. 2020, 28, 1326–1332. [Google Scholar] [CrossRef]
- AnonymousVisuotine Lietuviu Enciklopedija. Available online: https://www.vle.lt/straipsnis/taurage/ (accessed on 5 January 2022).
- Čepaitienė, A. The geolect of Pasvalys: A dialectometric approach to dialectal features. Taikom. Kalbot. 2019, 39–74. [Google Scholar] [CrossRef]
- Pasvalys. Available online: https://www.pasvalys.lt/lt/savivaldybe/apie-mus/1744 (accessed on 10 January 2022).
- International Society of Ethnobiology. International Society of Ethnobiology Code of Ethics (with 2008 Additions). 2006. Available online: http://ethnobiology.net/code-of-ethics/ (accessed on 12 December 2021).
- European Medicines Agency. Guideline on the Assessment of Clinical Safety and Efficacy in the Preparation of Community Herbal Monographs for Well-Established and of Community Herbal Monographs/Entries to the Community List for Traditional Herbal Medicinal Products/Substances/Preparations. 2017. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-assessment-clinical-safety-efficacypreparation-eu-herbal-monographs-well-established_en.pdf (accessed on 15 March 2022).
- WFO. 2021: World Flora Online. Available online: http://www.worldfloraonline.org (accessed on 10 March 2022).
- Stevens, P.F. Angiosperm Phylogeny Website, Version 13. 2012. Available online: http://www.mobot.org/MOBOT/research/APweb/ (accessed on 10 March 2022).
- Vilkonis, K.K. Lietuvos Žaliasis Rūbas; Lutute: Kaunas, Lithuania, 2008. [Google Scholar]
- Ragažinskienė, O.; Rimkienė, S.; Sasnauskas, V. Vaistinių Augalų Enciklopedija; Lutute: Kaunas, Lithuania, 2005. [Google Scholar]
- Jankevičienė, R. Botanikos Vardų Žodynas; Botanikos Instituto Leidykla: Vilnius, Lithuania, 1998. [Google Scholar]
- Luo, H.; Tang, Q.; Shang, Y.; Liang, S.; Yang, M.; Robinson, N.; Liu, J. Can Chinese Medicine Be Used for Prevention of Corona Virus Disease 2019 (COVID-19)? A Review of Historical Classics, Research Evidence and Current Prevention Programs. Chin. J. Integr. Med. 2020, 26, 243–250. [Google Scholar] [CrossRef] [Green Version]
- Ekiert, H.M.; Ramawat, K.G.; Arora, J. Medicinal Plants. In Sustainable Development and Biodiversity; Springer: Cham, Switzerland, 2021; Volume 28. [Google Scholar]
- Soukand, R.; Kalle, R. Where does the border lie: Locally grown plants used for making tea for recreation and/or healing, 1970s–1990s Estonia. J. Ethnopharmacol. 2013, 150, 162–174. [Google Scholar] [CrossRef]
- Pranskuniene, Z.; Bajoraite, R.; Simaitiene, Z.; Bernatoniene, J. Home Gardens as a Source of Medicinal, Herbal and Food Preparations: Modern and Historical Approaches in Lithuania. Appl. Sci. 2021, 11, 9988. [Google Scholar] [CrossRef]
- Soukand, R.; Quave, C.L.; Pieroni, A.; Pardo-de-Santayana, M.; Tardio, J.; Kalle, R.; Luczaj, L.; Svanberg, I.; Kolosova, V.; Aceituno-Mata, L.; et al. Plants used for making recreational tea in Europe: A review based on specific research sites. J. Ethnobiol. Ethnomed. 2013, 9, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heinrich, M. Quality and safety of herbal medical products: Regulation and the need for quality assurance along the value chains. Br. J. Clin. Pharmacol. 2015, 80, 62–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Šimkūnaitė, E. Lietuvių Liaudies Medicinos Vaistingieji Augalai. Archival material. Available at Lithuanian Museum of the History of Medicine and Pharmacy of the Lithuanian University of Health Sciences; Lietuvos Medicinos ir Farmacijos Istorijos Muziejus|LSMU (lsmuni.lt): Kaunas, Lithuania, 1948. [Google Scholar]
- Ekor, M. The growing use of herbal medicines: Issues relating to adverse reactions and challenges in monitoring safety. Front. Pharmacol. 2014, 4, 177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Alami, A.; Fattah, A.; Chait, A. Medicinal plants used for the prevention purposes during the COVID-19 pandemic in Morocco. J. Anal. Sci. Appl. Biotechnolgy 2020, 2, 4–11. [Google Scholar]
- Chen, S.; Dong, L.; Quan, H.; Zhou, X.; Ma, J.; Xia, W.; Zhou, H.; Fu, X. A review of the ethnobotanical value, phytochemistry, pharmacology, toxicity and quality control of Tussilago farfara L. (coltsfoot). J. Ethnopharmacol. 2021, 267, 113478. [Google Scholar] [CrossRef]
- Yang, Y. Use of herbal drugs to treat COVID-19 should be with caution. Lancet. 2020, 395, 1689–1690. [Google Scholar] [CrossRef]
- Gupta, P.K.; Sonewane, K.; Rajan, M. Scientific rationale of Indian AYUSH ministry advisory for COVID-19 prevention, prophylaxis, and immunomodulation. Adv. Trad. Med. 2021, 1–25. [Google Scholar] [CrossRef]
- Mukherjee, P.K.; Efferth, T.; Das, B.; Kar, A.; Ghosh, S.; Singha, S.; Debnath, P.; Sharma, N.; Bhardwaj, P.K.; Haldar, P.K. Role of medicinal plants in inhibiting SARS-CoV-2 and in the management of post-COVID-19 complications. Phytomedicine 2022, 98, 153930. [Google Scholar] [CrossRef]
- Ang, L.; Lee, H.W.; Kim, A.; Lee, J.A.; Zhang, J.; Lee, M.S. Herbal medicine and pattern identification for treating COVID-19: A rapid review of guidelines. Int. Med. Res. 2020, 9, 100407. [Google Scholar] [CrossRef]
- Timalsina, D.; Pokhrel, K.P.; Bhusal, D. Pharmacologic Activities of Plant-Derived Natural Products on Respiratory Diseases and Inflammations. BioMed Res. Int. 2021, 2021, 1636816. [Google Scholar] [CrossRef]
| Data of the Study | Percent | Archival Data | Percent | ||
|---|---|---|---|---|---|
| EMA assessment | Present | 32 | 53.4% | 14 | 20.3% |
| Non present | 28 | 46.6% | 55 | 79.7% | |
| Indications | Correspond to recommendations | 16 | 50% | 7 | 50% |
| Not correspond to recommendations | 16 | 50% | 7 | 50% | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pranskuniene, Z.; Balciunaite, R.; Simaitiene, Z.; Bernatoniene, J. Herbal Medicine Uses for Respiratory System Disorders and Possible Trends in New Herbal Medicinal Recipes during COVID-19 in Pasvalys District, Lithuania. Int. J. Environ. Res. Public Health 2022, 19, 8905. https://doi.org/10.3390/ijerph19158905
Pranskuniene Z, Balciunaite R, Simaitiene Z, Bernatoniene J. Herbal Medicine Uses for Respiratory System Disorders and Possible Trends in New Herbal Medicinal Recipes during COVID-19 in Pasvalys District, Lithuania. International Journal of Environmental Research and Public Health. 2022; 19(15):8905. https://doi.org/10.3390/ijerph19158905
Chicago/Turabian StylePranskuniene, Zivile, Ruta Balciunaite, Zenona Simaitiene, and Jurga Bernatoniene. 2022. "Herbal Medicine Uses for Respiratory System Disorders and Possible Trends in New Herbal Medicinal Recipes during COVID-19 in Pasvalys District, Lithuania" International Journal of Environmental Research and Public Health 19, no. 15: 8905. https://doi.org/10.3390/ijerph19158905
APA StylePranskuniene, Z., Balciunaite, R., Simaitiene, Z., & Bernatoniene, J. (2022). Herbal Medicine Uses for Respiratory System Disorders and Possible Trends in New Herbal Medicinal Recipes during COVID-19 in Pasvalys District, Lithuania. International Journal of Environmental Research and Public Health, 19(15), 8905. https://doi.org/10.3390/ijerph19158905








