Abstract
Despite the fact that several cases of unsafe pesticide use among farmers in different parts of Africa have been documented, there is limited evidence regarding which specific interventions are effective in reducing pesticide exposure and associated risks to human health and ecology. The overall goal of the African Pesticide Intervention Project (APsent) study is to better understand ongoing research and public health activities related to interventions in Africa through the implementation of suitable target-specific situations or use contexts. A systematic review of the scientific literature on pesticide intervention studies with a focus on Africa was conducted. This was followed by a qualitative survey among stakeholders involved in pesticide research or management in the African region to learn about barriers to and promoters of successful interventions. The project was concluded with an international workshop in November 2021, where a broad range of topics relevant to occupational and environmental health risks were discussed such as acute poisoning, street pesticides, switching to alternatives, or disposal of empty pesticide containers. Key areas of improvement identified were training on pesticide usage techniques, research on the effectiveness of interventions targeted at exposure reduction and/or behavioral changes, awareness raising, implementation of adequate policies, and enforcement of regulations and processes.
1. Introduction
The growing world population continues to put a strain on the agricultural sector and its need for effective and innovative methods of production to ensure food and job security through sufficient yields in crop production. Agriculture is, therefore, a primary sector in most countries, especially in sub-Saharan Africa (SSA), where most of the countries are categorized as low- and middle-income countries (LMICs). In these countries, most citizens rely on small-scale agriculture for food or income; there is a low tax base, and governments are dependent on international funding for projects [1]. Innovative and strategic international partnerships have recently emerged with the goal of sustainable agriculture in Africa to increase income and improve the food security of 30 million smallholder farm households in five agricultural hot spots [2]. In parallel, there is emerging evidence of the impact of climate change on social and economic development due to the fact of reduced agricultural productivity [3]. Unexpected recent plagues, for example, desert locust (Schistocerca gregaria) or the fall armyworm (Spodoptera frugiperda), continue to threaten livelihoods in the agricultural sector in the Global South [4]. These major threats to food supply continue to demand effective pest management strategies, which often include the use of synthetic pesticides. Many pesticides have been classified as persistent and highly hazardous to the environment and human health (e.g., pesticides in the chemical groups of organochlorines, organophosphates, or carbamates). Numerous attempts have been made by international organizations to address these global public health concerns for health and the environment with policies and regulation enforcement including the identification and labeling of highly hazardous pesticides (HHPs) and its categories of harm to health and the environment [5]. Yet, despite these attempts, the global situation of pesticide management reported by the Food and Agriculture Organization of the United Nations (FAO) and the World Health Organization’s (WHO) survey [6] revealed that one-third of the countries they investigated did not have guidelines for HHP use, posing the problem of evaluating products without guidelines. Studies on the knowledge attitudes and practices (KAP) of farmers conclude that insufficient training exists on safe pesticide use practices [7,8] and show noncompliance in the use of personal protective equipment (PPE), resulting from the influence of workers’ socio-cultural context (i.e., gender dynamics and social status), herbicide risk perceptions, and working conditions (i.e., environmental and logistical) [9]. The use of simple models to quantify the risks associated with pesticides to nontarget endpoints before and after registration is also lacking in many African countries [10,11]. There are also concerns regarding exposure for bystanders and farming communities including children engaged in farming activities [12,13,14]. Dietary exposure due to the high concentrations of pesticide residues in food has also been reported in the African region [15,16,17,18,19,20,21,22,23,24].
These conclusions from the literature raise concerns that there is no effective strategy in place to support the diverse and challenging situations in the context of pesticide use, which places the burden of risk largely on poor smallholder farmers and farm workers. An effective strategy may be defined as an activity or set of activities aimed at modifying a process, course of action, or sequence of events in order to change one or several of their characteristics such as the performance of the expected outcome. This may include educational programs, regulation, development and enforcement of new or more stringent policies, other improvements in the environment, or public health promotion campaigns. Interventions that include multiple strategies and a multiplicity of actors—public, private, and civil society—are typically the most effective in producing desired and long-term outcomes. The evidence has shown that interventions create change by (i) influencing individuals’ knowledge, attitudes, beliefs, and skills; (ii) increasing social support; (iii) creating supportive environments, policies, and resources, in other words, promoting a culture of human and environmental health protection [25].
This paper presents the key issues and recommendations raised in a workshop with global pesticide experts regarding their perceptions of the most pressing issues and effective interventions that are contextual for the agricultural sector in Africa and have the potential to improve the situation for the environment and human health.
2. Materials and Methods
2.1. Workshop Preparation
To prepare for the workshop, two main activities were conducted. First, a systematic literature review was conducted to map current geographical research hot spots and identify gaps around environmental and public health risks associated with agriculture pesticide use in the Africa Region [26]. In this review, 391 articles published between 2006 and 2021 were identified that covered 469 study sites with five geographical research hot spots (two in South Africa, two in East Africa, and one in West Africa). The systematic review identified key researchers to invite to participate and important pest problems, research hot spots, and interventions implemented for discussion at the workshop.
Second, a mixed-method content analysis study was conducted. We combined an online survey with 36 stakeholders from 16 different countries, one-to-one interviews with two individuals, and a closed focus group discussion with five relevant researchers and stakeholders in the African agricultural sector. Stakeholders for this survey were identified through the Pesticide Forum Network (PDF) led by the Environmental Division, School of Public Health and Family Medicine, University of Cape Town (UCT), and from the author list of papers identified in the systematic review of pesticide research in the Africa Region.
Based on this information, an online workshop was prepared, scheduled, and successfully held on 15–17 November 2021. The workshop aimed to discuss possible interventions to reduce pesticide exposure in the agricultural sector in Africa. We invited 14 speakers who had also participated in the mixed-method survey. On the first day, we discussed these targets focusing on occupational settings and exposure reduction among workers. On the second day, we primarily addressed interventions related to reducing environmental and public pesticide exposure. On the third day, we focused on policy measures. Each day started with introductory talks followed by a selection of case study presentations.
The workshop delivery approach included a mix of presentations, breakout group discussions, and plenary discussions. To stimulate the breakout group discussion, we started the discussion with polls addressing the main group’s discussion topics. Then, a moderated group discussion took place. Conclusions were shared in a subsequent plenary. The minutes from each session were used for writing this paper.
2.2. Workshop Participants
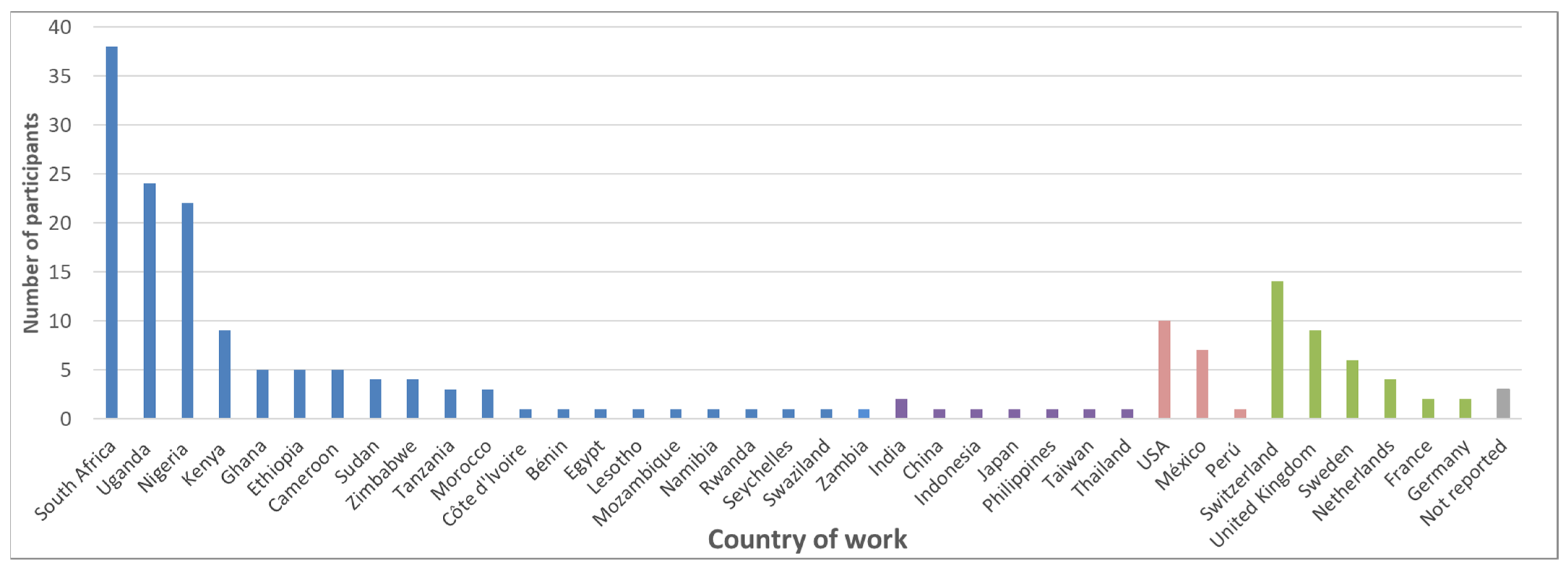
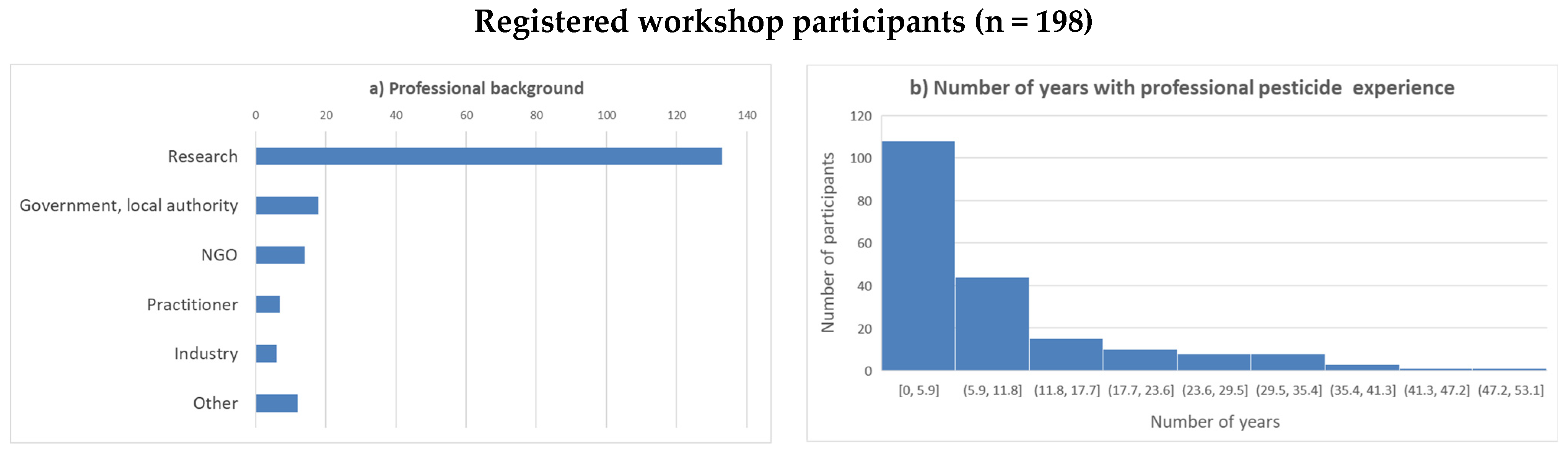
Participation in the workshop was without cost and open to anybody who was interested. Information regarding the workshop was shared publicly through different online platforms, directly with the participants of the mixed-method survey, and within the organizers’ networks. In total, 198 participants from 37 countries registered for the meeting; of those, 53 registered for one or two days only. Most of the participants were from Africa (67%), followed by Europe (18%), America (9%), and Asia (4%) (Figure 1). Most of the participants declared to be researchers (69%), followed by representatives of authorities (10%), nongovernmental organizations (7%), practitioners (4%), and industry (3%). The duration of professional experience with pesticides varied over a wide range (Figure 2).
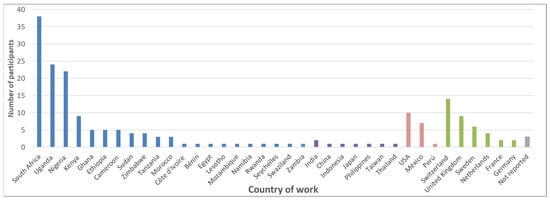
Figure 1.
Country of work of the registered workshop participants (blue = Africa; purple = Asia; red = Americas; green = Europe).
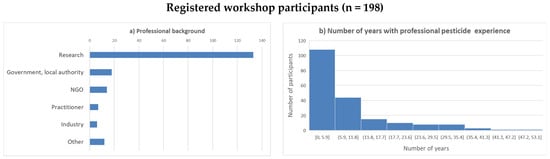
Figure 2.
Registered workshop participants: (a) professional background; (b) number of years of professional pesticide experience.
3. Results
The workshop presentations and recordings are available at https://www.swisstph.ch/en/about/events/interventions-to-reduce-pesticide-exposure-from-agriculture-sector-in-africa/, accessed on 18 July 2022.
To start the workshop, Samuel Fuhrimann gave an overview regarding the review of the pesticide research literature [9]. In total, 391 articles were identified that described data from 469 study sites. Human risks were addressed in 49% of the study sites and environmental risks in 20%. In many papers addressing human health or environmental risks, environmental samples were analyzed (68%). At a total of 180 (38%) study sites, human subjects were investigated. However, prospective longitudinal studies were only conducted at 18 sites (10%), and interventions on how to reduce pesticide use were only addressed at four sites (2%). High-quality research studies (e.g., large prospective cohort studies or randomized controlled trials) to monitor the (cost)-effectivity of the implemented interventions were missing. This clearly demonstrates the lack of high-quality research, which is needed for evidence-based policy interventions.
Martin Röösli presented the results of the stakeholder survey conducted before the workshop. When asked about the top guiding documents recommended to reduce agriculture pesticide use and its harm to the environment and human health, the following documents were most often named: The International Code of Conduct on Pesticide Management [27], FAO Pesticide Registration Toolkit [28], the WHO Recommended Classification of Hazardous Pesticides [29], and identifying HHPs using FAO and WHO Joint Meeting on Pesticide Management (JMPM) criteria [30]. From the content analysis of the survey, four different targets for interventions aiming at reducing pesticide use were identified: training, research, awareness raising, and policies/regulations. The stakeholders considered the fiscal and multiple economic implications as the main challenges for the implementation of policies to enforce reduced pesticide use. It was emphasized that more focus should be put on the implementation of science in order to bridge the gap between research and efficient implementation.
3.1. Occupational Pesticide Exposure
3.1.1. Problems in the Occupational Setting
Occupational exposure to pesticides among farmers usually occurs in agricultural fields directly in contact with pesticides during spraying and mixing. They become the most vulnerable group to pesticide exposure [31]. Additionally, events such as accidental spills, splashes, and consumption by mistake may result in acute poisonings [32]. In LMIC occupational settings, acute poisonings are one of the most pertinent problems, which was addressed by Erik Jørs. Globally, it is estimated that approximately 385 million cases of unintentional pesticide poisoning occur annually, including approximately 11,000 occupational fatalities [33,34]. The number of such cases is difficult to estimate due to the fact of underreporting and challenging diagnosis. The main reasons for accidental pesticide poisoning are increased accessibility and availability of HHPs; inadequate availability and usage of PPE such as clothes/overalls, shoes, and masks; inadequate washing of pesticide contamination; improper storage; illegal street sellers of pesticides. Sapbamrer et al. (2020) [35] found that the determinants associated with the use of PPE and pesticide safety practices were demographic factors (i.e., education/literacy level, experience of illness, and income); farm structure factors; behavioral and psychosocial factors (i.e., perceptions, attitudes, awareness, norms, and beliefs); training-related factors (i.e., information on pesticides, access to extension services, and training programs). Therefore, it is important to educate this group of workers to change their perceptions and behavior toward safe pesticide use and handling. Among the consequences of acute poisonings are reduced cholinesterase activities, DNA damage [36], and other health complaints [31,36,37,38]. In addition, pesticides are used for suicides, which are most effectively prevented by reduced accessibility [39].
Within the framework of IPM, Paul Jepson discussed the selection of pesticides for reducing human health and environmental risks using the example of the fall armyworm. Farmers lack access to basic information on pest biology and life cycle, efficacious control methods, and application timing and safer use of pesticides, which is exacerbated by limited access to extension services. Agrochemical dealers, who could provide some guidance in selecting lower-risk pesticides, have limited access to training and professional development other than via industry seminars and may, thus, miss out on critical information regarding integrated pest management (IPM). Both farmers and agrochemical dealers lacked PPE onsite [40]. Paul Jepson presented a system to classify 659 pesticides with respect to human and environmental health [41]. A standalone guideline, included within this publication, allows farmers to select lower-risk pesticides to protect applicators, human bystanders, aquatic life, terrestrial wildlife, and pollinators. The system is already in use among millions of certified farms internationally. One practical challenge, however, is that low-risk pesticides are often more costly than HHPs or other high-risk chemicals. This work was based upon an extensive multiscale analysis of pesticide risks in five West African countries [42], which demonstrate some of the highest health and environmental risks ever published.
3.1.2. Case Studies
Insufficient pesticide-related knowledge, attitude, and practices among smallholder farmers and retailers have been documented in Uganda [43,44,45,46], Nigeria [47], and other African countries [48]. As a case study, Aggrey Atuhaire presented a 12 month randomized control trial (October 2020–October 2021) on the effect of targeted information access (i.e., training and SMS reception) on the responsible use and handling of pesticides among smallholder farmers in Uganda (APSENT-Uganda). The study built upon evidence generated over the past six years within the PESTROP-Uganda project, which generated an interdisciplinary evidence base on environmental and public health issues of smallholder farmers in Uganda [44,45,49,50]. The intervention study included a 2 day training workshop on the responsible use of pesticides and a 5 month mobile phone SMS structured campaign on the theme of personal protective clothing, targeting 360 and 180 conventional smallholder farmers, respectively, who had previously been assessed through a baseline survey. Preliminary results comparing baseline and follow-up data indicated that farmers’ knowledge and attitude improvement were not necessarily reflected in their practice. Nevertheless, the results showed notable improvements in certain practices, especially farmers buying and using certain protective clothing such as waterproof pants, long-sleeved jackets, and chemical-resistant gloves. With regards to improvement, knowledge and interpretation of pesticide label pictograms was a key area of high performance for the majority of farmers. Up to 150 products and 50 active ingredients, the majority of which are insecticides and WHO hazard class II pesticides, were found to be used during this time; changes in pesticide use (i.e, toxicity, application frequency, amount, and area) are still being explored. Aggrey Atuhaire pointed out that results of preliminary analyses suggest that information dissemination to farmers shows great potential, but a more holistic approach, beyond information access, is needed to sustainably improve sound management of pesticides among smallholder farmers from an LMIC context. One main catalyst of pesticide awareness in the future would be to leverage the rapidly expanding telecommunication system (such as mobile phones) to reach out to farmers in their own language. This could involve developing a mobile app and transcribing label information to different local languages [51].
Diane Rohlman presented an intervention study focused on changing risk perceptions and behaviors among Egyptian adolescent pesticide applicators. Previous work with this population identified behaviors that increased pesticide exposure (e.g., mixing pesticides with a stick and hygiene behaviors) [52]. Focus groups were used to share this information with the adolescent applicators, their parents, and the Ministry of Agriculture to learn their perspectives and identify feasible ways to reduce exposure. Based on this qualitative research, an educational intervention was developed that targeted three behaviors: using a stick instead of their hand to mix pesticides, minimizing walking in the spray, and bathing and wearing clean clothes [53]. The study found increased awareness of the hazards of pesticides, changes in attitudes, and significant improvements in PPE use after the intervention. Participatory approaches are considered to be the most useful for developing feasible and acceptable interventions.
3.1.3. Discussion of Promoters and Barriers to Switching to Alternatives
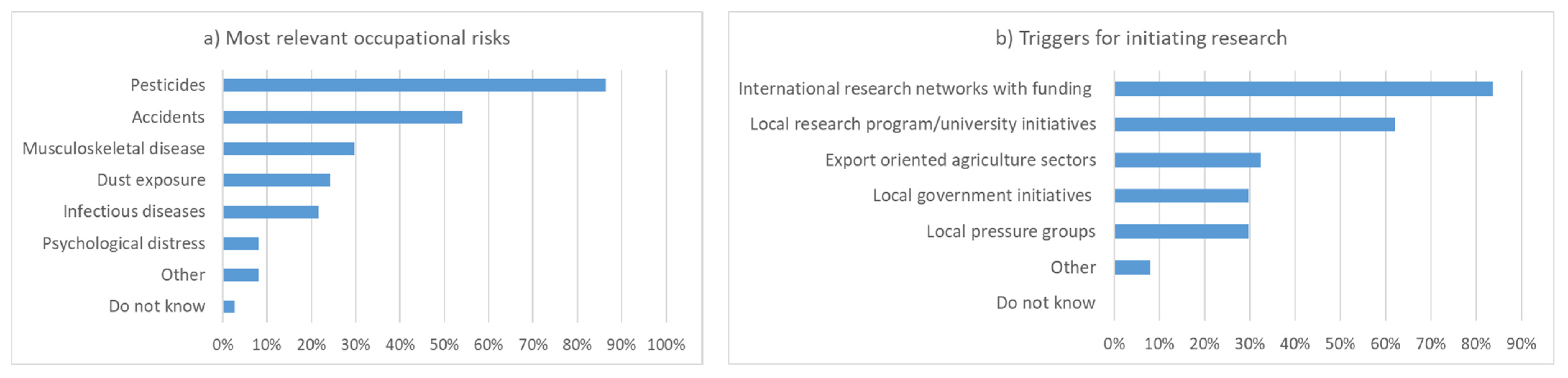
Before the breakout group discussion, workshop participants were asked about the most relevant occupational risks of pesticide applicators. Exposure to pesticides was mentioned most often, followed by injuries and musculoskeletal diseases (Figure 3). Infectious diseases, dust, and psychological distress were considered less relevant. For the initiation of research projects, international networks with funding and local research or university initiatives were considered to be most helpful. When presented with a list of potential topics for occupational health research, all items received high priority (Figure 3).
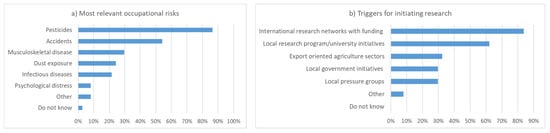
Figure 3.
(a) The most relevant occupational risks of pesticide applicators; (b) the most relevant triggers for initiating research as assessed by the workshop participants (n = 37, up to 3 responses per person).
The topics of these polls were subsequently discussed in depth. In terms of health risks to applicators, it was emphasized that the risk perception of pesticide applicators and farmers is an important aspect. Sometimes, it is challenging to convince farmers that pesticides are a health risk. Only listing health symptoms is usually not sufficient, as farmers need to understand the route of exposure and subsequent acute and chronic health effects. In particular, raising awareness of the potential long-term risks and accompanying long-term economic implications if applicators become ill is a challenge. These hidden costs are less evident to farmers than the short economic benefits of applying pesticides. One also needs to consider cultural issues that may prevent the application of correct protection measures such as “you are not a man if you use protection” or “we have done this for years like this”. Anecdotal reports suggest that the COVID-19 pandemic had an impact on attitudes toward mask wearing. Knowledge transfer to the target population is thus considered to be of high priority. Much of the (important) information is not available in local languages, which is a common barrier for effective communication. In the absence of language skills, red–green color blindness is also a barrier for correctly understanding pictograms. Communication should be “two-way” and include a participatory component to be effective. Collaborating with peer educators was found to work well.
For initiating research projects, raising awareness was considered one of the key triggers. Collaboration with NGOs may be a way to make local politicians aware of the situation. Research projects are often small and have limited reach, although potentially useful for sensitizing the local population. To be effective, one should not look at pesticides in an isolated manner but address them together with other important public health problems, such as reproduction and HIV, or occupational health outcomes such as musculoskeletal diseases and psychological distress. This may allow for larger scale and sustainable interventions by profiting from the mutual co-benefits of the interventions. In terms of international funding, raising awareness at the level of funding bodies is needed. To date, pesticide exposure has relatively little priority. International researchers and stakeholder networks may help break the vicious cycle of little research money, which results in problems with awareness.
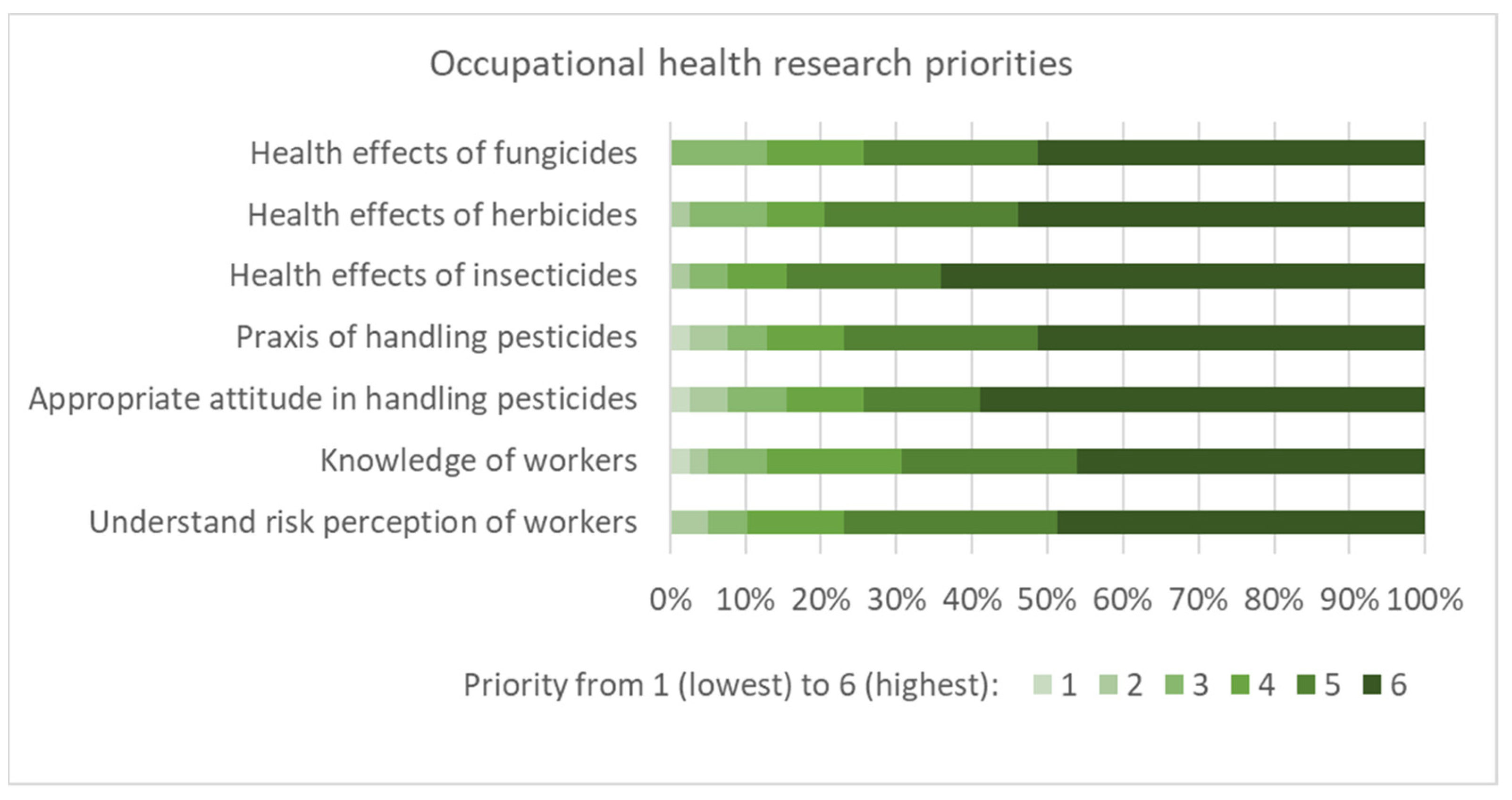
Figure 4 shows that various topics were considered to be of priority for future research. Appropriate attitudes on handling pesticides and the health effects of pesticides obtained a slightly higher priority compared to the other suggestions. In the subsequent discussion, the need for ecotoxicological research and biomonitoring of applicators and the public was also emphasized. Bottom-up approaches, such as first identifying the knowledge gaps of workers, were considered important for effective research. In terms of health effects, acute poisonings and the effects of long-term exposure to low levels were considered to be the most pertinent. Even if uncertainties remain regarding the toxicity of various compounds, research on the most effective prevention was of high relevance for farmers in addition to toxicological research.
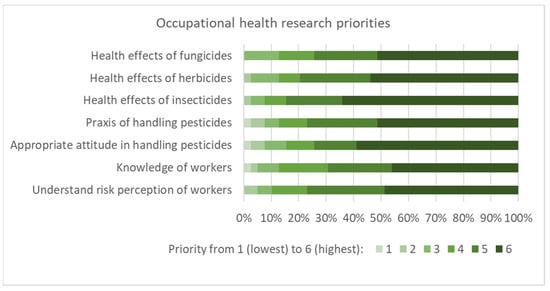
Figure 4.
Proposed occupational health priorities for research as assessed by the workshop participants (n = 39, priority rated from 1 to 6, denoting lowest to highest).
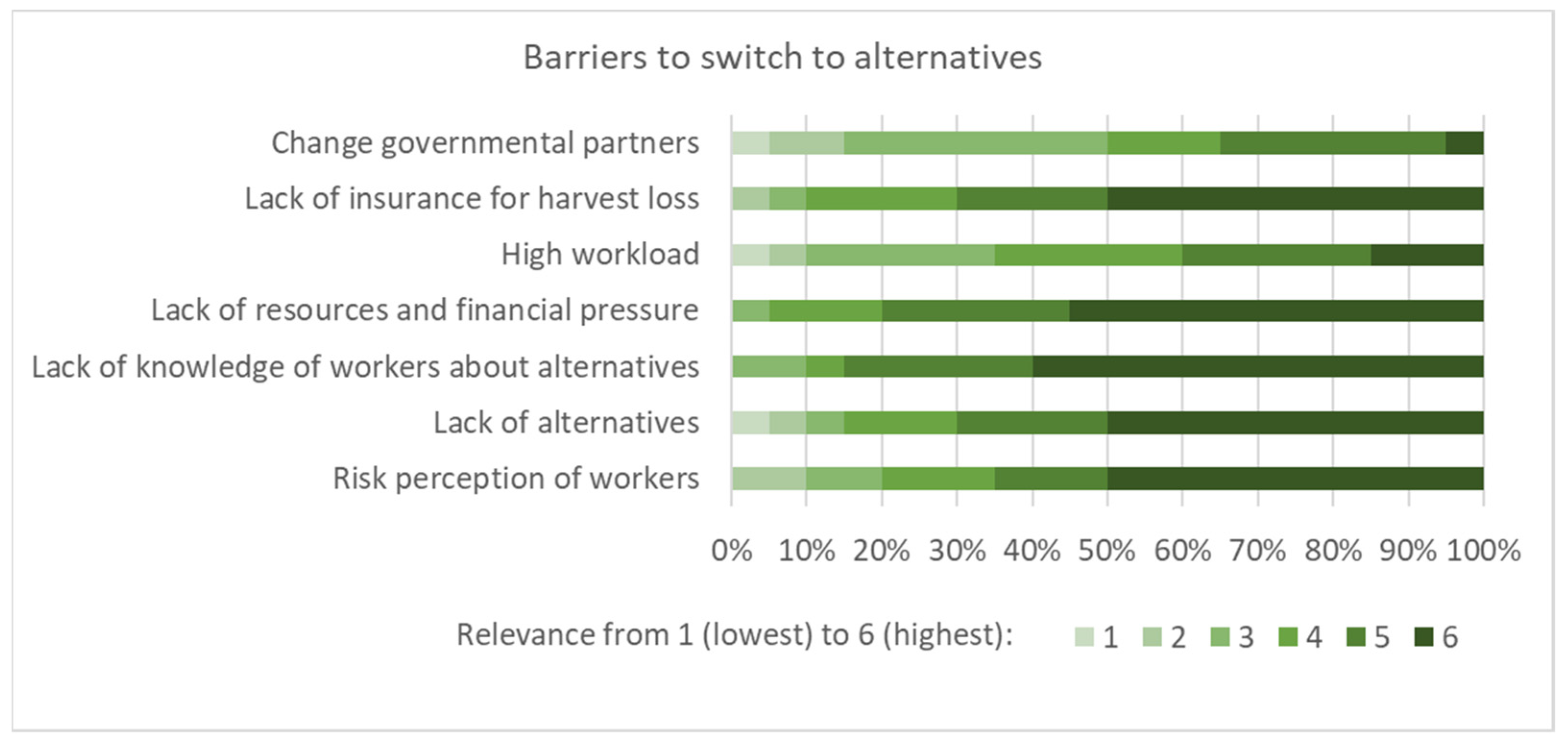
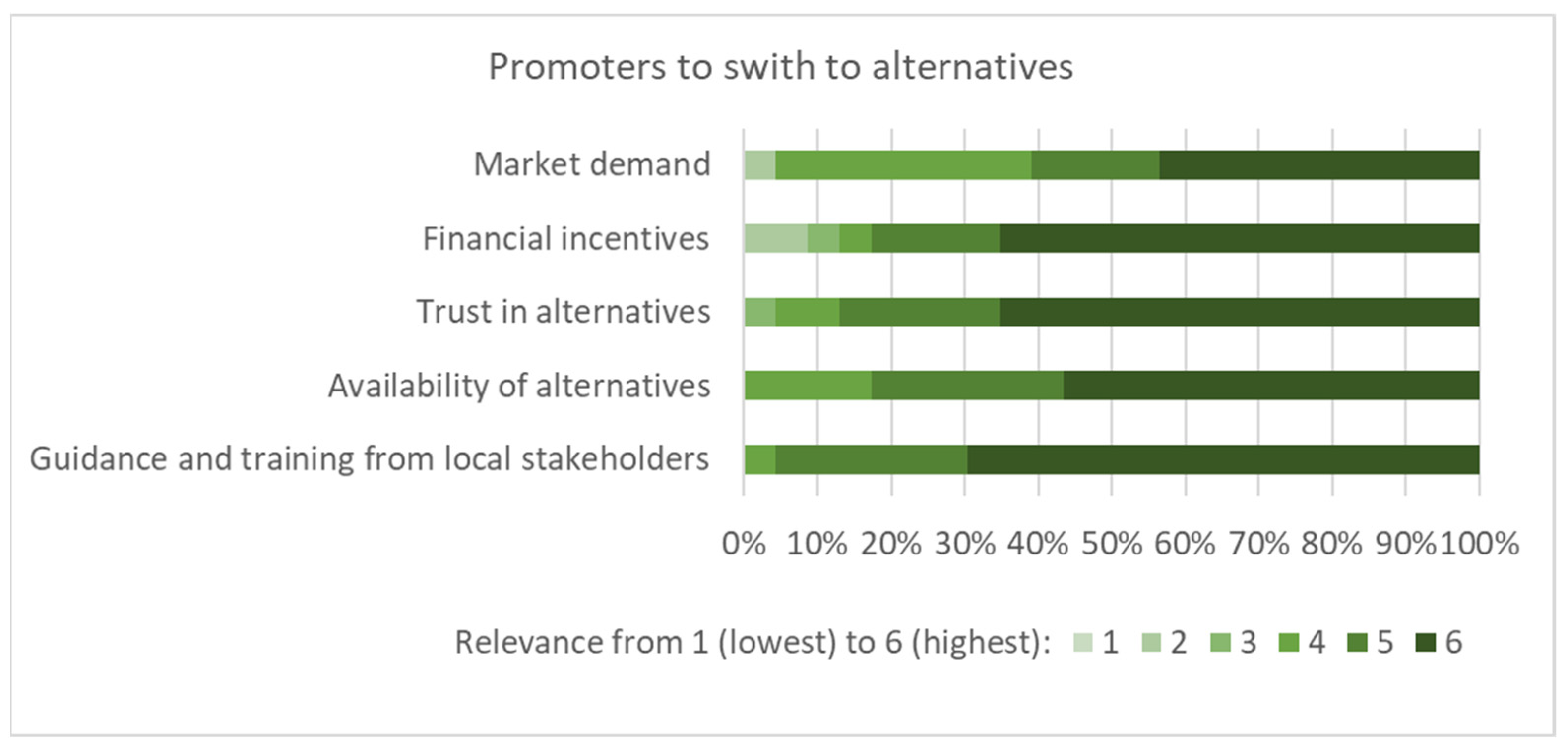
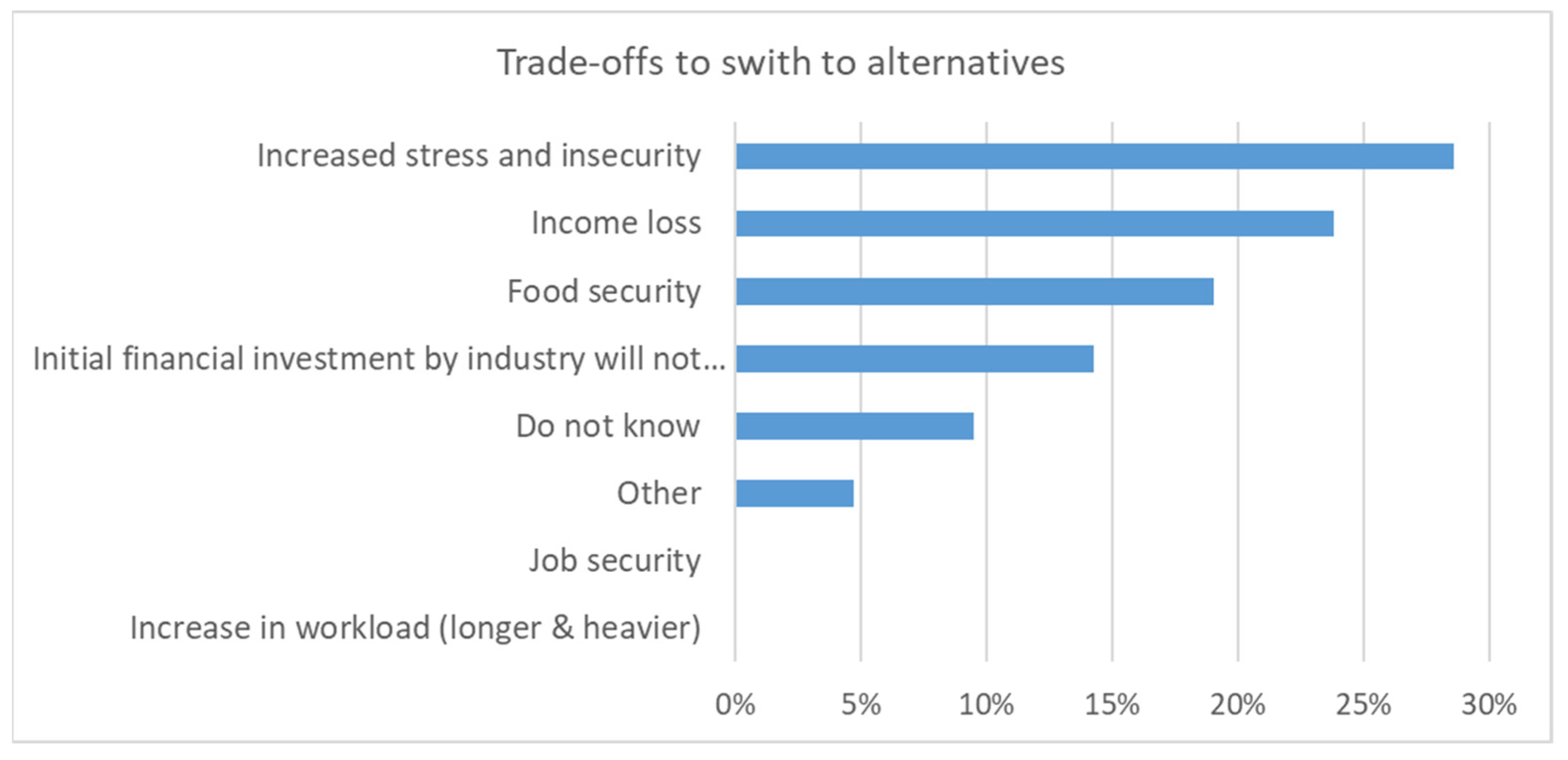
Subsequently, the barriers (Figure 5), promoters (Figure 6), and trade-offs (Figure 7) when switching to alternatives (i.e., reduced pesticide use or organic farming) were discussed. Several participants suggested that barriers received a high degree of consent, such as lack of knowledge, financial pressure, lack of alternatives, risk perception of workers, and lack of insurance for harvest loss. It was also mentioned that low-risk pesticides were more expensive. Several proposed promoters were considered to be relevant for a transformation to low-risk agricultural methods (Figure 6). In terms of trade-offs, stress, insecurity, and income loss were considered the most relevant, whereas an increase in workload and job security obtained little consent from the workshop participants (Figure 7).
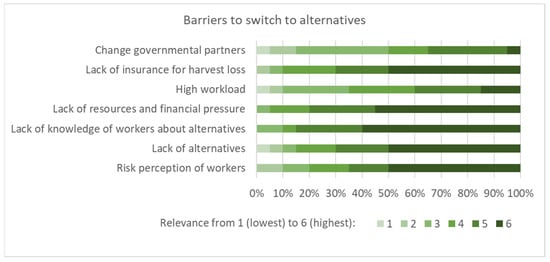
Figure 5.
Potential barriers to switching to alternatives as assessed by the workshop participants (n = 20, importance rated from 1 to 6, denoting lowest to highest).
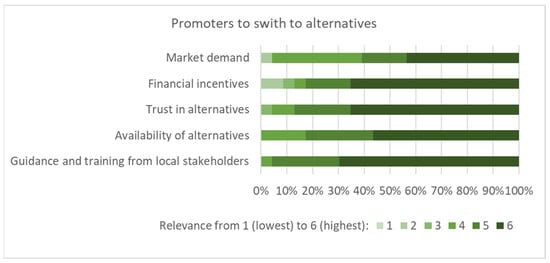
Figure 6.
Factors that may promote switching to alternatives as assessed by the workshop participants (n = 23, importance rated from 1 to 6, denoting lowest to highest).
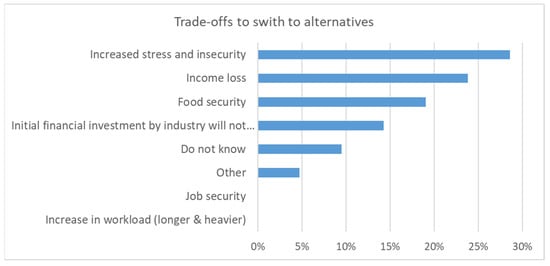
Figure 7.
Trade-offs to switching to alternatives as assessed by the workshop participants (n = 23).
In the discussion, it was emphasized that the size of a farm is critical for transformation processes. A small family farm may be less affected by market factors than a large employer. If a farm is producing for export, they need to adhere to international standards. Thus, international standards are important promoters of transition. Change in consumers’ preferences may eventually also result in pressure to change to alternatives. As a comparison, plastic packaging in supermarkets was reduced due to the pressure from consumers. A transition from conventional farming to alternatives may result in immediate income losses, and farmers need confidence that in the long term this will be compensated with benefits and better environmental conditions. However, it was also questioned to what extent transition really causes income loss. Well-trained farmers may know about working alternatives and saving expenses on pesticides. Thus, profitability may even increase in certain circumstances.
3.2. Environmental and Public Pesticide Exposure
3.2.1. Problems for the Environment and Public Exposure
On the 2nd day of the workshop, James M. Dabrowski introduced the development of decision support tools for managing pesticide risks to aquatic ecosystems and human health in South African water resources [54,55]. Several indicators, such as crop type, growth stage, and meteorological and geographic factors, were tested in the field and could reliably predict relative differences in pesticide concentrations. Simple modeling approaches were reliable and should be used more widely. These novel tools are thus useful for identifying hot spots across a country, prioritizing pesticides based on their risk to human health and the aquatic ecosystem, identifying important transport routes, and for informing which pesticides should be included in monitoring programs.
Aqiel Dalvie discussed lessons from the fields with respect to the implications of interventions. In his studies, he found that sprayers, non-sprayers, farm residents, and neighboring nonfarm residents, including vulnerable groups, were at risk for exposure and possible long-term adverse health effects [12,56,57,58,59,60,61,62,63,64,65]. Proximity is a relevant factor for aerial exposure, but other sources of exposure are also relevant such as drinking water from an open water source, eating crops from the agricultural areas and gardens, or obsolete stocks. Interventions may target the re-entry of workers into orchards/vineyards, PPE for sprayers and non-sprayers, reduction in pesticide usage and alternatives, buffer zones, awareness and education, surveillance, improved legislation and implementation, improved access to health care, and screening and conducting biomonitoring.
Godwin O. Olutona presented their findings of higher levels of organochlorine pesticides (OCPs) above the recommended limit in water and bottom sediment of Aiba reservoir, Iwo [66], as well as in leguminous food crops from selected markets in Ibadan, Nigeria [67]. In addition, an incident was presented concerning 116 students from a secondary school in Doma, Gombe State, and 112 people in Cross River (Nigeria), who fell ill and were hospitalized after eating cowpea contaminated with pesticides [68]. Twenty fast food outlets were closed in Nigeria because of fatalities traced to pesticide residue in their products [69]. Pesticides residues were also detected in malt drinks sold in Nigeria market, which was traced to the pesticide residue used in treating sorghum in 2018 [70].
Samuel Fuhrimann presented the results from a series of recent pesticide exposure assessment studies. An analysis of 27 currently used pesticides at 20 air sampling sites across Africa over seven years demonstrated the ongoing use of pesticides in Africa that are banned in HICs [71]. For epidemiological research and risk management, good knowledge of the exposure situation is needed. Presented examples included seasonal variations in air concentrations of 27 organochlorine pesticides (OCPs) and 25 current-use pesticides (CUPs) [72], the water concentrations of 53 pesticides in catchments across three agricultural areas of South Africa [73], and in-depth studies on personal exposure using silicon wristbands for children and guardians during spraying season [74,75]. From concurrently sampled air and soil samples, it was concluded that, except for chlorpyrifos, soil ingestion generally represented a minor exposure pathway compared to inhalation (i.e., <5%) [76]. He suggested that a pesticide-vigilance system should be introduced, i.e., a post-registration monitoring analogue to current practice for pharmaceutics (pharmacovigilance).
Brenda Eskenazi presented lessons from more than 20 years of research with the Center for the Health Assessment of Mothers and Children of Salinas (CHAMACOS), which is a community–university partnership. Between 1999 and 2000, pregnant mothers were recruited and followed up. The study showed that mothers had higher organophosphate exposure than the US average, and higher levels were associated with various negative effects on the cognitive development and respiratory health of their children [77]. Effects from exposure during pregnancy were still detectable in adolescence. In the subsequent CHAMACOS study, interventions were explored to reduce pesticide exposure. As an example, regarding how different health risks are interrelated, Brenda Eskenazi demonstrated that Californian farm workers were at increased risk of COVID-19 during the pandemic.
3.2.2. Case Studies
Saloshni Naidoo presented various studies on pesticide safety practices amongst small-scale women farmers in KwaZulu-Natal, South Africa. It was initially found that pesticides were stored in the open or even at home, and only a minority locked up pesticides. Handling and re-use of empty pesticide containers also occurred regularly and, thus, is a source of pesticide exposure [78]. After a two-day training program, the situation markedly improved. Access to services was one of the health system challenges identified, as emergency services are not available or far away. Furthermore, the operating hours of some services are not compatible with working hours. There was also limited awareness in the health system of pesticide-related health problems as demonstrated in a case study of acute chlorpyrifos poisoning in pregnancy [79].
Berna van Wendel de Joode presented several tested approaches to reduce occupational and environmental pesticide exposures in Costa Rica embedded in the Infants’ Environmental Health Program (ISA) [80,81]. It was found that communication of study results with the study population, ministries, and industry resulted in significant improvements. By collaboration with key actors, exposures from drift could be successfully reduced. Flexible educational strategies were designed to stimulate social and cognitive development. Utilizing a participatory approach, agro-ecological concepts were discussed and experienced during workshops in the field.
3.2.3. Discussion of Interventions
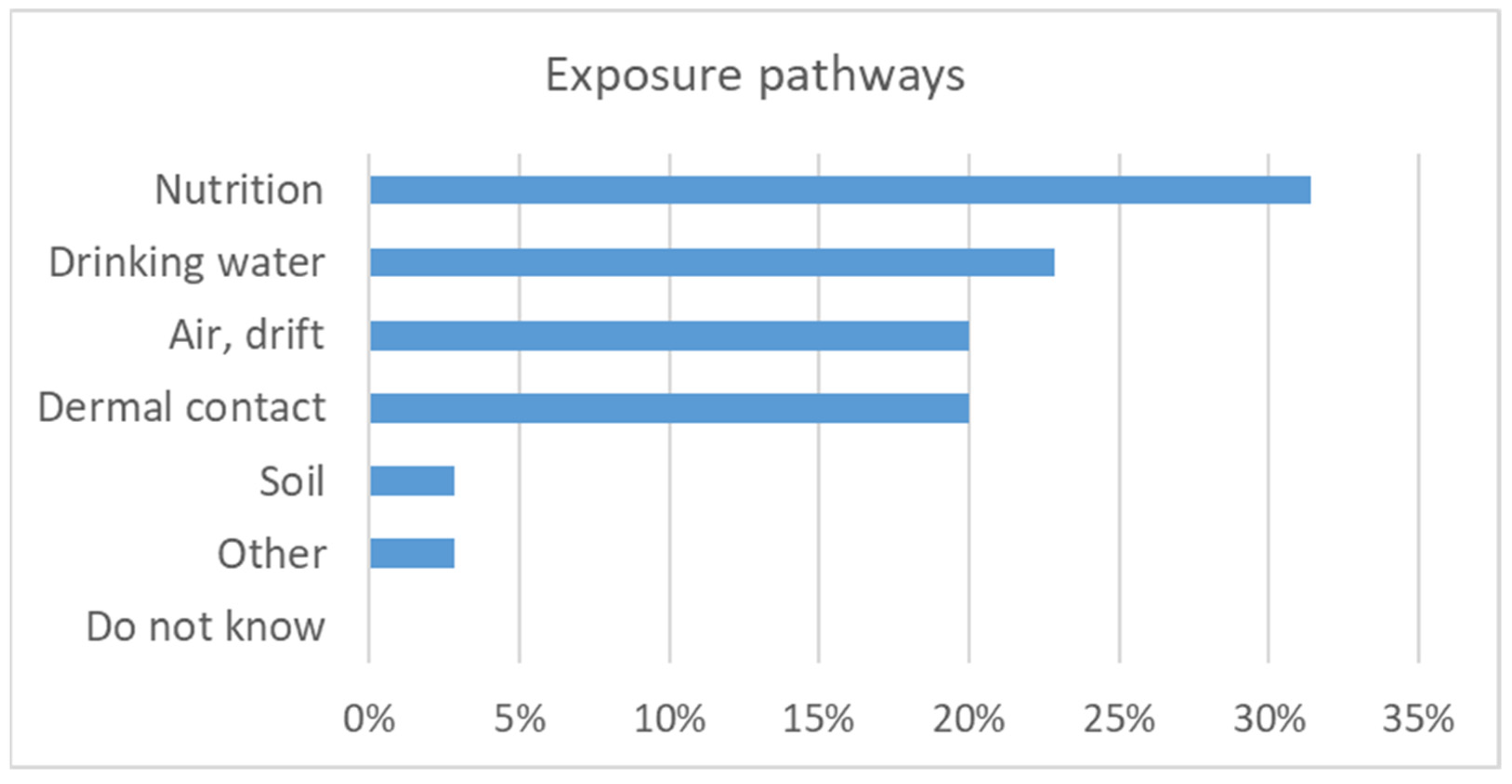
The subsequent discussion was opened by a poll regarding the most relevant exposure pathways for health. Nutrition (i.e., ingestion of pesticide residues in food) was considered to be most relevant followed by drinking water and air including drift and dermal contact (Figure 8).
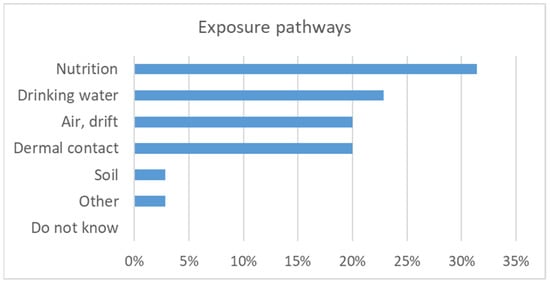
Figure 8.
Most relevant exposure pathways as assessed by the workshop participants (n = 35).
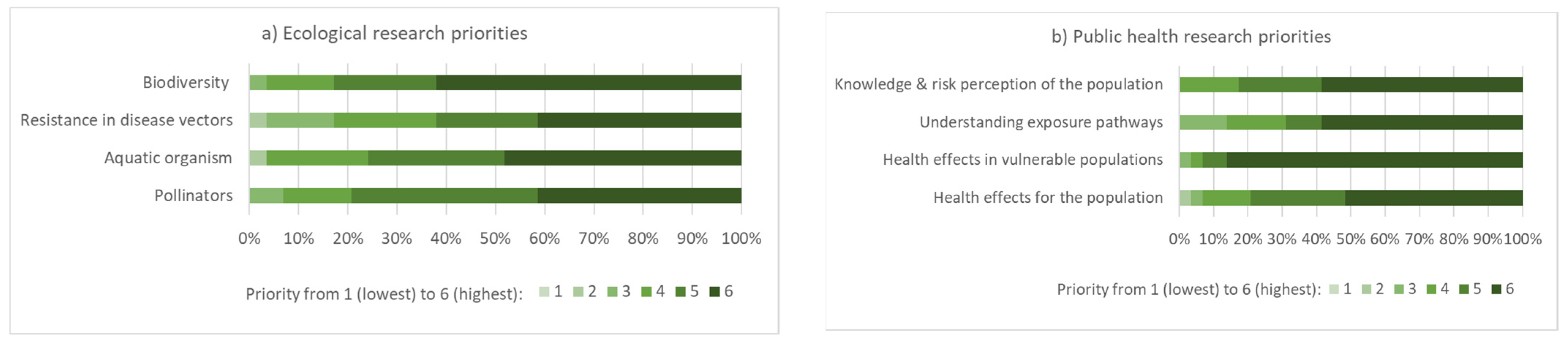
In terms of ecological research priorities, biodiversity and the effect of pesticides on aquatic organisms received the highest score, although the differences were small for the suggested topics (Figure 9). Group discussion revealed pest resistance to pesticides and the effects of pesticides on microbial activity as areas where further research is needed. A challenge in many African countries is the limited number of laboratories with competencies for analysis of environmental samples and the high costs for these types of analyses. This hampers progress in research and in identifying the most critical situations. For health effects research, vulnerable populations were considered a key priority (Figure 9).

Figure 9.
Most relevant a) ecological and b) public health research priorities as assessed by the workshop participants (n = 29, relevance rated from 1 to 6, denoting lowest to highest).
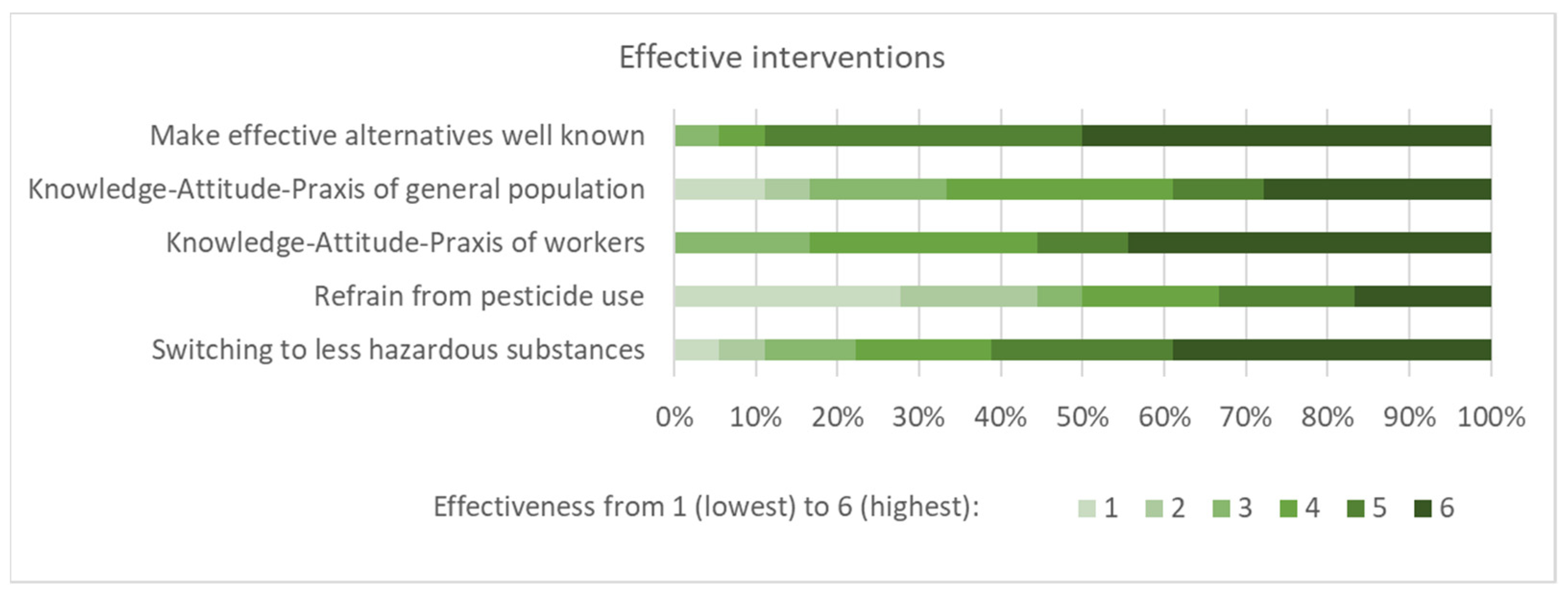
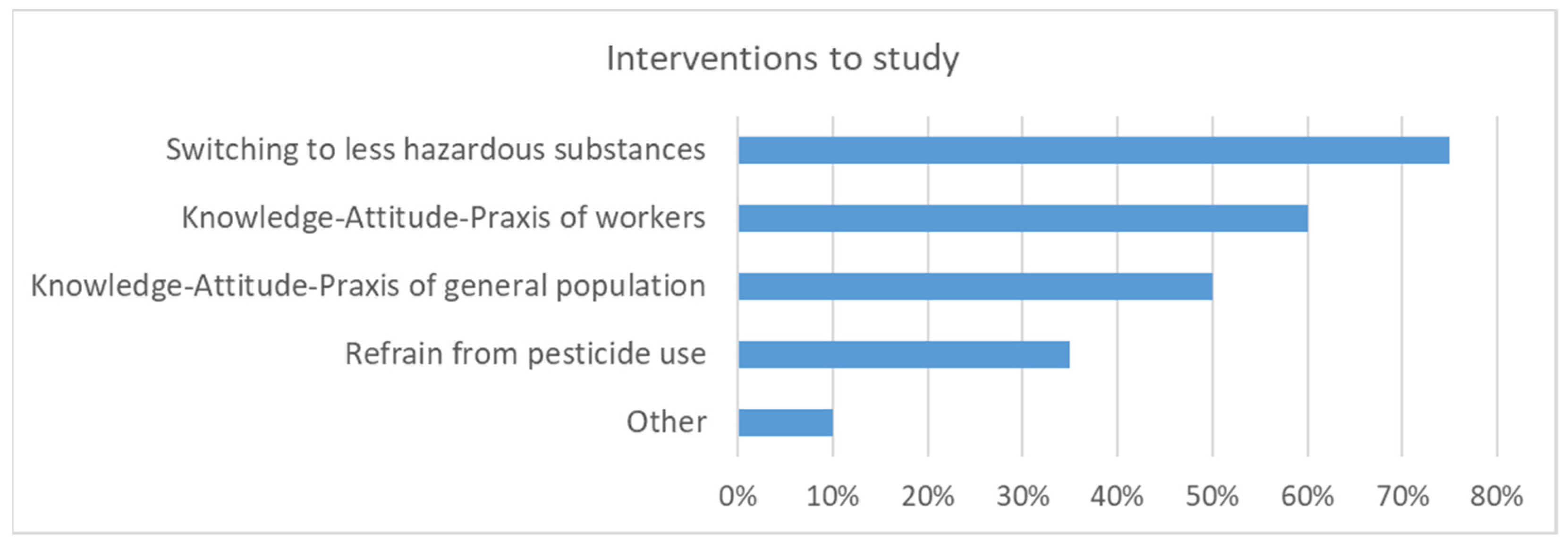
There was a relatively high conviction that making alternatives well known is effective for reducing pesticide levels in the environment (Figure 10). Switching to less hazardous substances and interventions regarding awareness paralleled with the KAP of workers were also considered effective. Nevertheless, additional research on the effectiveness of various interventions was deemed to be important (Figure 11). The highest priority was given to interventions addressing the switch to less hazardous substances and the KAP of workers as well as the general population. Similar to the discussion on occupational research and interventions presented above, participatory approaches with the public were considered the most important. This may also be labeled as citizen science or MARP (“Méthode Active de Recherche Participative”). Participatory approaches may be used for defining research questions, acceptable interventions, and data collection. If the public is involved in data collection, the results need to be communicated to them. The information for the public should not be very technical and not too complicated. Communicating environmental pesticides levels may result in higher awareness and opposition against pesticides. It was noted that in many LMICs, people were mostly focused on food security and less on food safety. To change this mindset, comprehensive data regarding ecological and human health risks are needed. Local data are usually much more convincing than data collected from other countries, even if they would be transferable.
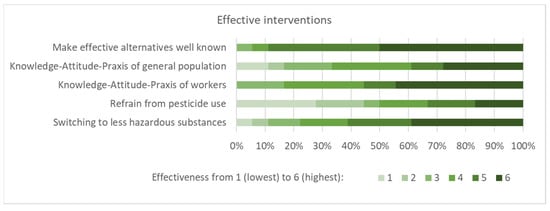
Figure 10.
Rating of the question: which interventions are known to be effective for reducing pesticide exposure in the environment? (n = 18, effectiveness rated from 1 to 6, denoting lowest to highest).
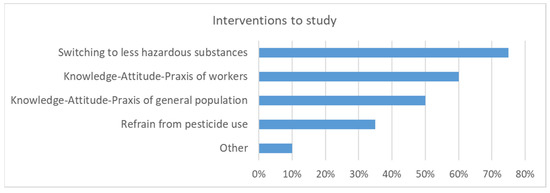
Figure 11.
The effectiveness of which interventions that should be addressed in research as assessed by the workshop participants (n = 20, multiple-choice).
In addition to specific interventions, the need for system changes was emphasized. Agriculture production should move away from monoculture farming, since emergency outbreaks are more common in such a setting. In the case of an emergency (e.g., fall army-worm), there is hardly any alternative to pesticide application in order not to lose the harvest.
It was further discussed that educating the next generation of safety professionals and children may be a sustainable intervention with long-term consequences for the agricultural system. They may influence their parents’ decisions on whether and how to apply pesticides. Conversely, the training of farmers did not always result in a change in behavior.
3.3. Policy Measures
3.3.1. Evidence Needs from a Stakeholder Perspective
Ivy Saunyama discussed what types of evidence are needed from intervention studies for the regulation of pesticides to reduce exposure from the agricultural sector. For the regulator, the most critical evidence is the potential benefits, in terms of minimizing crop losses, reduction of diseases, or protection of buildings, that outweigh the expected risks to applicators, consumers, and the environment. Of note, HHPs are causing the majority of environmental and health problems. The need to take action on HHPs is widely recognized and long-awaited.
3.3.2. Illegal and Street Pesticides
Hanna-Andrea Rother used the example of street pesticides to demonstrate that exposure risks from agricultural pesticides are not limited to crop protection. Street pesticides are either illegal pesticides legally registered for agricultural use and then decanted into unlabeled domestic containers, such as juice bottles, or unregistered prepackaged products [82]. The former poses a high risk for accidental ingestion (e.g., children), but street pesticides may also be the subject of homicides and suicides [83,84,85]. Poverty and housing inequality are key reasons for pest infestation and, thus, interventions need to simultaneously address issues at the individual, community, and regulatory levels to change the context. Regulatory interventions are needed to reduce access to agricultural pesticides by suppliers and consumers. Training and risk communication tools need to address different target groups ranging from street vendors to children and policymakers [86]. For exposure reduction, a broad range of methods are needed using multipronged approaches, including codesigning interventions with the target audience. However, to reduce hazardous exposures to agricultural pesticides in urban settings, firstly, HHPs (especially those banned in the Global North) should be phased out from agricultural use and alternatives implemented [83].
3.3.3. What Policy Is Needed?
Leslie London discussed policy responses to reduce occupational and environmental exposure to pesticides in Africa [87]. Policy is important for import and distribution, usage, regulation, surveillance, and research. Approximately 10% of global imports was by Africa, which corresponds to USD 3 billion, in 2021. Despite rapid growth in pesticide markets, policy enforcement has not kept pace, resulting in fake and counterfeit pesticides, negative environmental impacts, and harm to health. In terms of usage, climate shocks were found to drive food insecurity with the subsequent need of pesticides for buffering. Whereas a lack of risk awareness and peer pressure were responsible for part of the unsafe use, as fairly often farmers were not aware of the risk, but PPE is too expensive or unavailable, and alternatives to chemical control are not available or promoted by government extension agents. To address peer pressure, the promotion of Farmer Field Schools as the mainstream is important. Regulations for retailers and for advertising are often lacking or, if existing, not enforced. Policies that control who purchases and what volumes can be sold, phasing out hidden subsidies for pesticide inputs, and actively reducing sole reliance on chemicals for pest control must supplement strategies reliant on farmer behavior.
3.3.4. Discussion of Stakeholder Perspectives and Policy Options
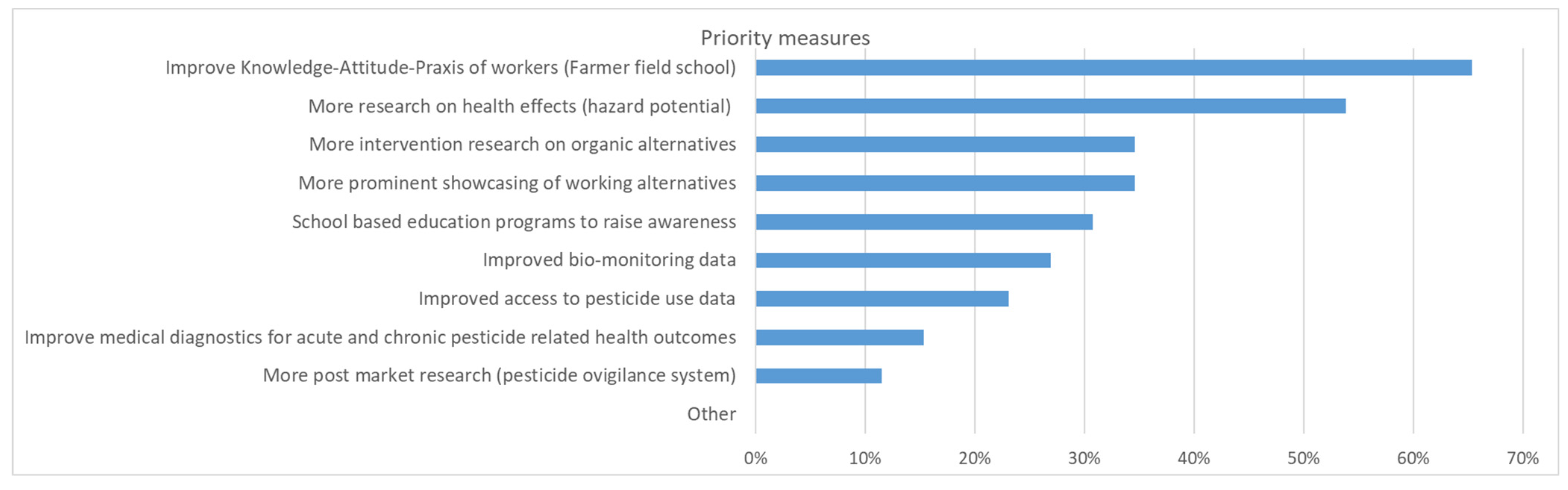
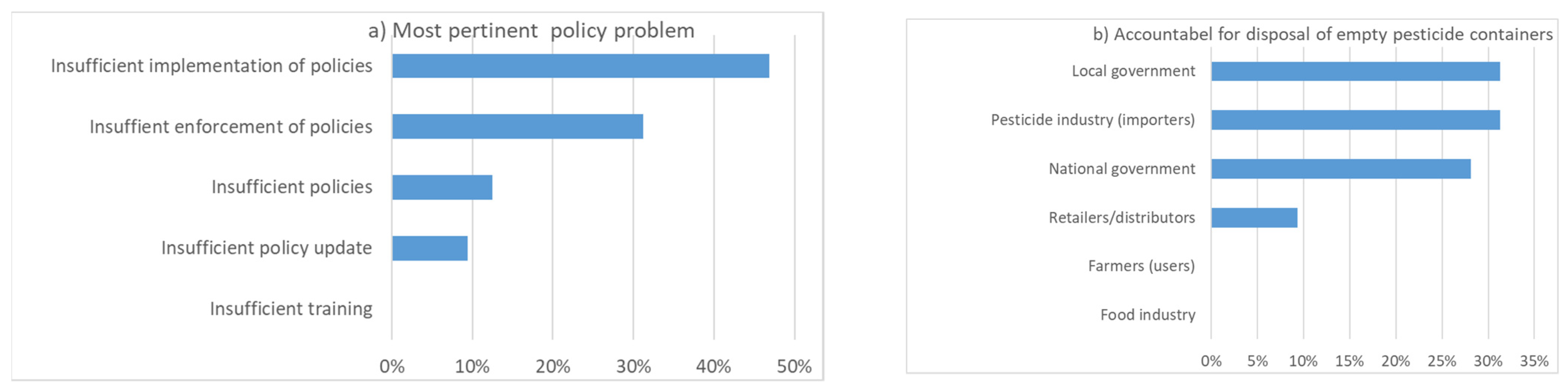
In the subsequent discussion sessions, participants voted on the priority measures to be implemented (Figure 12). The three most commonly selected measures were to improve the knowledge, attitude and practice (KAP) of workers (farmer field school), more research on health effects (hazard potential), and more intervention research on organic alternatives. Strikingly, a majority of participants were convinced that insufficient implementation and enforcement of policies were the most pertinent problems but not the lack of policies (Figure 13). Nevertheless, some participants were surprised to see that many people thought that there were enough policies. Specifically, it was mentioned that incentives were missing to promote less pesticide use.
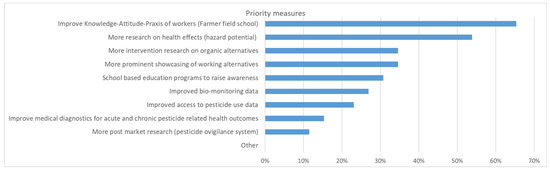
Figure 12.
Which priority measures should be implemented (n = 26, up to 3 responses per person).
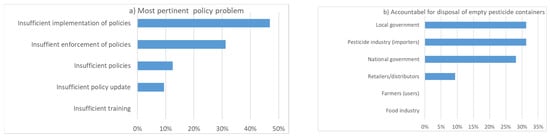
Figure 13.
(a) What is the most pertinent problem when it comes to policy; (b) who should be most accountable for the management/disposal of empty pesticide containers (n = 32).
A lack of resources and research were identified as barriers to faster transition to less hazardous practices. In this context, the responsibility of the pesticide manufacturers and retailers were discussed. In principle, parts of the profit from industry could be used for research. However, this is very sensitive in terms of conflict of interests and would need the careful implementation of firewalls so that selection of research questions, research groups, and research projects is not influenced by the donor. Ideally, such a research fund should be managed by the government.
As a typical example of an important problem, inadequate disposal of obsolete pesticides and empty pesticide containers was mentioned a few times during the workshop. The reasons for this problem are unclear or lack of responsibilities. Often, adequate disposal in practice becomes the personal responsibility of the user (i.e., farmer), which is not ideal according to the workshop participants. There was no clear preference on who should be mainly responsible (Figure 13).
It was suggested that a pesticide vigilance system similar to a pharmacovigilance system would be helpful in identifying the most relevant emerging problems and reacting to them. Some examples of such locally applied surveillance systems were mentioned. Whereas the methods are clear for acute poisoning incidents, such a system is more challenging for capturing long-term and chronic effects.
4. Discussion
To our knowledge, this workshop was the first of its kind in Africa. Overall, a broad range of topics relevant to occupational and environmental health risks and interventions related to a reduction in pesticide use were discussed during the workshop. A lack of intervention and longitudinal studies in the region was identified in the systematic literature review. An integrated strategy to reduce pesticide use includes awareness-raising, training of different populations, and research as well as the implementation and enforcement of policies and regulations. Participatory approaches that include the concerned populations are most effective. In occupational settings, the main barriers for switching to less hazardous alternatives are high costs, lack of awareness, paucity of experiences and knowledge regarding alternatives for specific applications, and a lack of insurance for harvest loss. A lack of resources is the main reason for many of the deficits in this area, most likely due to the fact of inadequate financing and not accounting for the long-term costs related to the negative effects of pesticide exposure for human health and the ecosystem. It also became clear during the workshop that the context of pesticide use was complex and related to poverty, poor education, insufficient housing, and changing climate, to name just a few factors. Multisectoral approaches are needed to improve the situation with many co-benefits for the public health situation. Key are long term strategies, such as capacity building for regulatory agencies, supported by evidence-based policies; continuing education throughout the pesticide supply chain and, ultimately, to farmers; access to actionable science concerning pesticide risk management; the establishment of effective risk communication networks that translate science for end users; viable strategies for scaling up education and communication; an underpinning of consultation, participation, and continuing engagement with end users to determine needs; tracking the status and trends in both adverse impacts and the benefits of interventions.
This workshop report should not be considered a consensus report. Discussions were stimulated with presentations and polling questions. However, the online format did not allow for in-depth discussions. It should also be noted that only a minority of the registered participants voted. At the beginning of the workshop, we also tried a Delphi approach and repeated the polls after the discussion. This resulted only in minor changes and was, thus, not presented in this paper. This may reflect that the discussion time was short and not context specific. Further, it indicates that the participating experts had an established opinion, which may depend on their specific background. Further discussion would be needed to understand different judgments and to derive more specific interventions for various contexts.
The workshop focused mainly on classical agricultural areas and had less focus on countries, such the Congo or Cameroon, that had many forests that were converted to agricultural lands. Fewer data are available on the effects of pesticides on the ecology in such frontier environments.
5. Conclusions
In conclusion, interventions to reduce pesticide use are still not well explored and researched. This workshop calls for more participatory actions and research to improve the situation, in particular for smallholder farmers and surrounding areas to protect their health and well-being. The key areas of improvement identified were training on pesticide usage techniques, research on the effectiveness of interventions targeted at exposure reduction and/or behavioral changes, awareness raising and implementation of adequate policies, and enforcement of regulations and processes. Future research should follow a research translational paradigm, including affected communities, and search for risk reduction co-benefits such as access to health care, dealing with the pandemic, or waste management.
Author Contributions
Conceptualization, A.A., M.A.D., S.F. and M.R.; methodology, A.A., M.A.D., S.F., S.C.-M. and M.R.; workshop presenter, A.A., M.A.D., J.D., B.E., S.F., E.J., P.C.J., L.L., S.N., H.-A.R., D.S.R., M.R., I.S. and B.v.W.d.J.; resources, M.R.; writing—original draft preparation, A.A., M.A.D., S.F. and M.R.; writing—review and editing, all authors; visualization, M.R.; project administration, M.R.; funding acquisition, A.A., M.A.D., S.F. and M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Leading House Africa, mandated by the Swiss State Secretariat for Education, Research, and Innovation. The APC was funded by a voucher. The work reported by DR was funded by Fogarty International Center and National Institute of Environmental Health Sciences (R01ES022163).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Presentations of the workshop and recordings of the talks are available at: https://www.swisstph.ch/en/about/events/interventions-to-reduce-pesticide-exposure-from-agriculture-sector-in-africa/ accessed on 18 July 2022.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- De Graaff, J.; Kessler, A.; Nibbering, J.W. Agriculture and food security in selected countries in Sub-Saharan Africa: Diversity in trends and opportunities. Food Secur. 2011, 3, 195–213. [Google Scholar] [CrossRef] [Green Version]
- AGRA. Partnership for Inclusive Agricultural Transformation in Africa (PIATA). Available online: https://agra.org/piata/ (accessed on 18 July 2022).
- Shimada, G. The Impact of Climate-Change-Related Disasters on Africa’s Economic Growth, Agriculture, and Conflicts: Can Humanitarian Aid and Food Assistance Offset the Damage? Int. J. Environ. Res. Public Health 2022, 19, 467. [Google Scholar] [CrossRef]
- Ngowi, A.; Mrema, E.; Kishinhi, S. Pesticide Health and Safety Challenges Facing Informal Sector Workers: A Case of Small-scale Agricultural Workers in Tanzania. New Solut. 2016, 26, 220–240. [Google Scholar] [CrossRef] [PubMed]
- SAICM. Strategy to Address Highly Hazardous Pesticides in the Context of the Strategic Approach to International Chemicals Management. 2019. Available online: http://www.saicm.org/Portals/12/Documents/EPI/HHP%20strategy%20English.pdf (accessed on 18 July 2022).
- WHO. Global Situation of Pesticide Management in Agriculture and Public Health: Report of a 2018 WHO-FAO Survey; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Sosan, M.B.; Akingbohungbe, A.E. Occupational Insecticide Exposure and Perception of Safety Measures among Cacao Farmers in Southwestern Nigeria. Arch. Environ. Occup. Health 2009, 64, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Ndayambaje, B.; Amuguni, H.; Coffin-Schmitt, J.; Sibo, N.; Ntawubizi, M.; Van Wormer, E. Pesticide Application Practices and Knowledge among Small-Scale Local Rice Growers and Communities in Rwanda: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 4770. [Google Scholar] [CrossRef] [Green Version]
- Andrade-Rivas, F.; Rother, H.A. Chemical exposure reduction: Factors impacting on South African herbicide sprayers’ personal protective equipment compliance and high risk work practices. Environ. Res. 2015, 142, 34–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teklu, B.M.; Adriaanse, P.I.; Van den Brink, P.J. Monitoring and risk assessment of pesticides in irrigation systems in Debra Zeit, Ethiopia. Chemosphere 2016, 161, 280–291. [Google Scholar] [CrossRef]
- Teklu, B.M.; Adriaanse, P.I.; Ter Horst, M.M.S.; Deneer, J.W.; Van den Brink, P.J. Surface water risk assessment of pesticides in Ethiopia. Sci. Total Environ. 2015, 508, 566–574. [Google Scholar] [CrossRef]
- Chetty-Mhlanga, S.; Fuhrimann, S.; Basera, W.; Eeftens, M.; Röösli, M.; Dalvie, M.A. Association of activities related to pesticide exposure on headache severity and neurodevelopment of school-children in the rural agricultural farmlands of the Western Cape of South Africa. Environ. Int. 2020, 146, 106237. [Google Scholar] [CrossRef]
- Sosan, M.B.; Akingbohungbe, A.E.; Ojo, I.A.O.; Durosinmi, M.A. Insecticide residues in the blood serum and domestic water source of cacao farmers in Southwestern Nigeria. Chemosphere 2008, 72, 781–784. [Google Scholar] [CrossRef]
- Dalvie, M.A.; Sosan, M.B.; Africa, A.; Cairncross, E.; London, L. Environmental monitoring of pesticide residues from farms at a neighbouring primary and pre-school in the Western Cape in South Africa. Sci. Total Environ. 2014, 466, 1078–1084. [Google Scholar] [CrossRef] [PubMed]
- Ihedioha, J.N.; Ejalonibu, M.A.; Ekere, N.R. Multi-residue Analysis of Organochlorine Pesticides in Cocoa Beans (Theobroma cacao) and Soils from Ondo, Nigeria. Pak. J. Anal. Environ. Chem. 2020, 21, 219–231. [Google Scholar]
- Sulaiman, M.; Maigari, A.; Ihedioha, J.; Lawal, R.; Gimba, A.; Shuaibu, A. Levels and health risk assessment of organochlorine pesticide residues in vegetables from Yamaltu area in Gombe, Nigeria. Fr.-Ukr. J. Chem. 2021, 9, 19–30. [Google Scholar] [CrossRef]
- Kapeleka, J.A.; Sauli, E.; Sadik, O.; Ndakidemi, P.A. Co-exposure risks of pesticides residues and bacterial contamination in fresh fruits and vegetables under smallholder horticultural production systems in Tanzania. PLoS ONE 2020, 15, e0235345. [Google Scholar] [CrossRef] [PubMed]
- Ssemugabo, C.; Guwatudde, D.; Ssempebwa, J.C.; Bradman, A. Pesticide Residue Trends in Fruits and Vegetables from Farm to Fork in Kampala Metropolitan Area, Uganda—A Mixed Methods Study. Int. J. Environ. Res. Public Health 2022, 19, 1350. [Google Scholar] [CrossRef] [PubMed]
- Nuapia, Y.; Chimuka, L.; Cukrowska, E. Assessment of organochlorine pesticide residues in raw food samples from open markets in two African cities. Chemosphere 2016, 164, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Galani, J.H.Y.; Houbraken, M.; Wumbei, A.; Djeugap, J.E.; Folio, D.; Spanoghe, P. Evaluation of 99 Pesticide Residues in Major Agricultural Products from the Western Highlands Zone of Cameroon Using QuEChERS Method Extraction and LC-MS/MS and GC-ECD Analyses. Foods 2018, 7, 184. [Google Scholar] [CrossRef] [Green Version]
- Galani, Y.J.H.; Houbraken, M.; Wumbei, A.; Djeugap, J.F.; Fotio, D.; Gong, Y.Y.; Spanoghe, P. Monitoring and dietary risk assessment of 81 pesticide residues in 11 local agricultural products from the 3 largest cities of Cameroon. Food Control 2020, 118, 107416. [Google Scholar] [CrossRef]
- Galani, Y.J.H.; Houbraken, M.; Wumbei, A.; Djeugap, J.F.; Fotio, D.; Gong, Y.Y.; Spanoghe, P. Contamination of Foods from Cameroon with Residues of 20 Halogenated Pesticides, and Health Risk of Adult Human Dietary Exposure. Int. J. Environ. Res. Public Health 2021, 18, 5043. [Google Scholar] [CrossRef]
- Sosan, M.B.; Adeleye, A.O.; Oyekunle, J.A.O.; Udah, O.; Oloruntunbi, P.M.; Daramola, M.O.; Saka, W.T. Dietary risk assessment of organochlorine pesticide residues in maize-based complementary breakfast food products in Nigeria. Heliyon 2020, 6, e05803. [Google Scholar] [CrossRef]
- Odewale, G.O.; Sosan, M.B.; Oyekunle, J.A.O.; Adeleye, A.O. Assessment of systemic and carcinogenic health risks of persistent organochlorine pesticide residues in four fruit vegetables in south-western Nigeria. Br. Food J. 2022, 124, 1755–1774. [Google Scholar] [CrossRef]
- Afshari, M.; Karimi-Shahanjarini, A.; Khoshravesh, S.; Besharati, F. Effectiveness of interventions to promote pesticide safety and reduce pesticide exposure in agricultural health studies: A systematic review. PLoS ONE 2021, 16, e0245766. [Google Scholar] [CrossRef] [PubMed]
- Fuhrimann, S.; Wan, C.; Blouzard, E.; Veludo, A.; Holtman, Z.; Chetty-Mhlanga, S.; Dalvie, M.A.; Atuhaire, A.; Kromhout, H.; Röösli, M.; et al. Pesticide Research on Environmental and Human Exposure and Risks in Sub-Saharan Africa: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2021, 19, 259. [Google Scholar] [CrossRef]
- FAO; WHO. NSP—International Code of Conduct on Pesticide Management; 2014. Available online: https://www.fao.org/agriculture/crops/thematic-sitemap/theme/pests/code/en/ (accessed on 18 July 2022).
- FAO. Pesticide Registration Toolkit. Available online: https://www.fao.org/pesticide-registration-toolkit/en/ (accessed on 18 July 2022).
- WHO. WHO Recommended Classification of Hazardous Pesticides. Available online: https://www.who.int/ipcs/publications/pesticides_hazard/en/ (accessed on 18 July 2022).
- FAO. Identifying HHPs by FAO and WHO Joint Meeting on Pesticide Management (JMPM) Criteria. Available online: http://www.fao.org/agriculture/crops/thematic-sitemap/theme/pests/code/hhp/en/ (accessed on 18 July 2022).
- Dhananjayan, V.; Jayanthi, P.; Jayakumar, S.; Ravichandran, B. Agrochemicals Impact on Ecosystem and Bio-monitoring. In Resources Use Efficiency in Agriculture; Kumar, S., Meena, R.S., Jhariya, M.K., Eds.; Springer: Singapore, 2020. [Google Scholar] [CrossRef]
- Lebailly, P.; Bouchart, V.; Baldi, I.; Lecluse, Y.; Heutte, N.; Gislard, A.; Malas, J.P. Exposure to Pesticides in Open-field Farming in France. Ann. Occup. Hyg. 2009, 53, 69–81. [Google Scholar] [PubMed]
- Boedeker, W.; Watts, M.; Clausing, P.; Marquez, E. The global distribution of acute unintentional pesticide poisoning: Estimations based on a systematic review. BMC Public Health 2020, 20, 1875. [Google Scholar] [CrossRef]
- Jors, E.; Neupane, D.; London, L. Pesticide Poisonings in Low- and Middle-Income Countries. Environ. Health Insights 2018, 12, 1–3. [Google Scholar] [CrossRef] [Green Version]
- Sapbamrer, R.; Thammachai, A. Factors affecting use of personal protective equipment and pesticide safety practices: A systematic review. Environ. Res. 2020, 185, 109444. [Google Scholar] [CrossRef] [PubMed]
- Dhananjayan, V.; Ravichandran, B.; Panjakumar, K.; Kalaiselvi, K.; Rajasekar, K.; Mala, A.; Avinash, G.; Shridhar, K.; Manju, A.; Wilson, R. Assessment of genotoxicity and cholinesterase activity among women workers occupationally exposed to pesticides in tea garden. Mutat. Res. Genet. Toxicol. Environ. Mutagenesis 2019, 841, 1–7. [Google Scholar]
- Dhaanjayan, V.; Ravichandran, B. Occupational health risk of farmers exposed to pesticides in agricultural activities. Curr. Opin. Environ. Sci. Health 2018, 4, 31–37. [Google Scholar] [CrossRef]
- Venugopal, D.; Karunamoorthy, P.; Beerappa, R.; Sharma, D.; Aambikapathy, M.; Rajasekar, K.; Gaikwad, A.; Kondhalkar, S. Evaluation of work place pesticide concentration and health complaints among women workers in tea plantation, Southern India. J. Expo. Sci Environ. Epidemiol. 2021, 31, 560–570. [Google Scholar] [CrossRef]
- Knipe, D.W.; Gunnell, D.; Eddleston, M. Preventing deaths from pesticide self-poisoning-learning from Sri Lanka’s success. Lancet Glob Health 2017, 5, E651–E652. [Google Scholar] [CrossRef] [Green Version]
- Murray, K.; Jepson, P.C.; Huesing, J. Fall Armyworm for Maize Smallholders in Kenya: An Integrated Pest Management Strategic Plan. 2019. Available online: https://repository.cimmyt.org/bitstream/handle/10883/21259/63345.pdf?sequence=1&isAllowed=y (accessed on 18 July 2022).
- Jepson, P.C.; Murray, K.; Bach, O.; Bonilla, M.A.; Neumeister, L. Selection of pesticides to reduce human and environmental health risks: A global guideline and minimum pesticides list. Lancet Planet Health 2020, 4, e56–e63. [Google Scholar] [CrossRef] [Green Version]
- Jepson, P.C.; Guzy, M.; Blaustein, K.; Sow, M.; Sarr, M.; Mineau, P.; Kegley, S. Measuring pesticide ecological and health risks in West African agriculture to establish an enabling environment for sustainable intensification. Philos. Trans. R. Soc. B: Biol. Sci. 2014, 369, 20130491. [Google Scholar] [CrossRef] [Green Version]
- Diemer, N.; Staudacher, P.; Atuhaire, A.; Fuhrimann, S.; Inauen, J. Smallholder farmers’ information behavior differs for organic versus conventional pest management strategies: A qualitative study in Uganda. J. Clean Prod. 2020, 257, 120465. [Google Scholar] [CrossRef]
- Fuhrimann, S.; Farnham, A.; Staudacher, P.; Atuhaire, A.; Manfioletti, T.; Niwagaba, C.B.; Namirembe, S.; Mugweri, J.; Winkler, M.S.; Portengen, L.; et al. Exposure to multiple pesticides and neurobehavioral outcomes among smallholder farmers in Uganda. Environ. Int. 2021, 152, 106477. [Google Scholar] [CrossRef] [PubMed]
- Staudacher, P.; Fuhrimann, S.; Farnham, A.; Mora, A.M.; Atuhaire, A.; Niwagaba, C.; Stamm, C.; Eggen, R.I.; Winkler, M.S. Comparative Analysis of Pesticide Use Determinants among Smallholder Farmers from Costa Rica and Uganda. Environ. Health Insights 2020, 14, 1–15. [Google Scholar] [CrossRef]
- Atuhaire, A.; Ocan, D.; Jørs, E. Knowledge, attitudes, and practices of tomato producers and vendors in Uganda. Adv. Nutr. Food Sci. 2016, 1, 1–7. [Google Scholar]
- Sosan, M.B.; Oni, O.; Folorunso, D.O. Pesticide handling and associated health risks among agrochemical retailers in Osun State, Nigeria. Ife J. Agric. 2013, 26, 97–110. [Google Scholar] [CrossRef]
- Rodenburg, J.; Johnson, J.M.; Dieng, I.; Senthilkumar, K.; Vandamme, E.; Akakpo, C.; Allarangaye, M.D.; Baggie, I.; Bakare, S.O.; Bam, R.K.; et al. Status quo of chemical weed control in rice in sub-Saharan Africa. Food Secur. 2019, 11, 69–92. [Google Scholar] [CrossRef] [Green Version]
- Mueller, W.; Atuhaire, A.; Mubeezi, R.; van den Brenk, I.; Kromhout, H.; Basinas, I.; Jones, K.; Povey, A.; van Tongeren, M.; Harding, A.H.; et al. Evaluation of two-year recall of self-reported pesticide exposure among Ugandan smallholder farmers. Int. J. Hyg. Environ. Health 2022, 240, 113911. [Google Scholar] [CrossRef]
- Fuhrimann, S.; Van den Brenk, I.; Atuhaire, A.; Mubeezi, R.; Staudacher, P.; Huss, A.; Kromhout, H. Recent pesticide exposure affects sleep: A cross-sectional study among smallholder farmers in Uganda. Environ. Int. 2022, 158, 106878. [Google Scholar] [CrossRef] [PubMed]
- Pacific Northwest Agricultural Safety and Health Center. Bilingual App to Keep Farmworkers Safe. Available online: https://deohs.washington.edu/pnash/blog/bilingual-app-keep-farmworkers-safe (accessed on 18 July 2022).
- Callahan, C.L.; Hamad, L.A.; Olson, J.R.; Ismail, A.A.; Abdel-Rasoul, G.; Hendy, O.; Rohlman, D.S.; Bonner, M.R. Longitudinal assessment of occupational determinants of chlorpyrifos exposure in adolescent pesticide workers in Egypt. Int. J. Hyg. Environ. Health 2017, 220, 1356–1362. [Google Scholar] [CrossRef] [PubMed]
- Rohlman, D.S.; Davis, J.W.; Ismail, A.; Rasoul, G.M.A.; Hendy, O.; Olson, J.R.; Bonner, M.R. Risk perception and behavior in Egyptian adolescent pesticide applicators: An intervention study. BMC Public Health 2020, 20, 678. [Google Scholar] [CrossRef] [PubMed]
- Dabrowski, J.M.; Balderacchi, M. Development and field validation of an indicator to assess the relative mobility and risk of pesticides in the Lourens River catchment, South Africa. Chemosphere 2013, 93, 2433–2443. [Google Scholar] [CrossRef]
- Dabrowski, J.M.; Shadung, J.M.; Wepener, V. Prioritizing agricultural pesticides used in South Africa based on their environmental mobility and potential human health effects. Environ. Int. 2014, 62, 31–40. [Google Scholar] [CrossRef]
- Chetty-Mhlanga, S.; Basera, W.; Fuhrimann, S.; Probst-Hensch, N.; Delport, S.; Mugari, M.; Van Wyk, J.; Röösli, M.; Dalvie, M.A. A prospective cohort study of school-going children investigating reproductive and neurobehavioral health effects due to environmental pesticide exposure in the Western Cape, South Africa: Study protocol. BMC Public Health 2018, 18, 857. [Google Scholar] [CrossRef] [Green Version]
- Molomo, R.N.; Basera, W.; Chetty-Mhlanga, S.; Fuhrimann, S.; Mugari, M.; Wiesner, L.; Röösli, M.; Dalvie, M.A. Relation between organophosphate pesticide metabolite concentrations with pesticide exposures, socio-economic factors and lifestyles: A cross-sectional study among school boys in the rural Western Cape, South Africa. Environ. Pollut. 2021, 275, 116660. [Google Scholar] [CrossRef]
- Dalvie, M.A.; White, N.; Raine, R.; Myers, J.E.; London, L.; Thompson, M.; Christiani, D.C. Long term respiratory health effects of the herbicide, paraquat, among workers in the Western Cape. Occup. Environ. Med. 1999, 56, 391–396. [Google Scholar] [CrossRef] [Green Version]
- Dalvie, M.A.; Myers, J.E.; Thompson, M.L.; Dyer, S.; Robins, T.G.; Omar, S.; Riebow, J.; Molekwa, J.; Kruger, P.; Millar, R. The hormonal effects of long-term DDT exposure on malaria vector-control workers in Limpopo Province, South Africa. Environ. Res. 2004, 96, 9–19. [Google Scholar] [CrossRef]
- Dalvie, M.A.; Naik, I.; Channa, K.; London, L. Urinary dialkyl phosphate levels before and after first season chlorpyrifos spraying amongst farm workers in the Western Cape, South Africa. J. Environ. Sci. Health B 2011, 46, 163–172. [Google Scholar] [CrossRef]
- English, R.G.; Perry, M.; Lee, M.M.; Hoffman, E.; Delport, S.; Dalvie, M.A. Farm residence and reproductive health among boys in rural South Africa. Environ. Int. 2012, 47, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Dalvie, M.A.; Rother, H.A.; London, L. Chemical hazard communication comprehensibility in South Africa: Safety implications for the adoption of the globally harmonised system of classification and labelling of chemicals. Saf. Sci. 2014, 61, 51–58. [Google Scholar] [CrossRef]
- Motsoeneng, P.M.; Dalvie, M.A. Relationship between Urinary Pesticide Residue Levels and Neurotoxic Symptoms among Women on Farms in the Western Cape, South Africa. Int. J. Environ. Res. Public Health 2015, 12, 6281–6299. [Google Scholar] [CrossRef] [Green Version]
- Mwanga, H.H.; Dalvie, M.A.; Singh, T.S.; Channa, K.; Jeebhay, M.F. Relationship between Pesticide Metabolites, Cytokine Patterns, and Asthma-Related Outcomes in Rural Women Workers. Int. J. Environ. Res. Public Health 2016, 13, 957. [Google Scholar] [CrossRef] [Green Version]
- Glass, T.; Dalvie, M.A.; Holtman, Z.; Vorster, A.A.; Ramesar, R.S.; London, L. DNA variants and organophosphate neurotoxicity among emerging farmers in the Western Cape of South Africa. Am. J. Ind. Med. 2018, 61, 11–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olutona, G.O.; Ayano, S.A.; Obayomi-Davies, O. Organochlorine pesticide in water and bottom sediment from Aiba Reservoir (Southwestern Nigeria). Chem. Ecol. 2014, 30, 513–531. [Google Scholar] [CrossRef]
- Olutona, G.O.; Aderemi, M.A. Organochlorine pesticide residue and heavy metals in leguminous food crops from selected markets in Ibadan. Legume Sci. 2019, 1, e3. [Google Scholar] [CrossRef]
- Shaibu, I. National Agency of Food and Drug Administration and Control (NAFDAC) Bans 30 Agricultural Products. Vanguard, 14 May 2008. [Google Scholar]
- Chikwe, A. National Agency of Food and Drug Administration and Control (NAFDAC) Axes 20 Fast Food Outlets. Task Operators On Good Hygiene Practices. Available online: www.nigeriabestforum.com (accessed on 6 July 2020).
- Olutona, G.O.; Livingstone, S.T. Detection of Organochlorine Pesticide (OCPs) Residues and Trace Metals in Some Selected Malt Drinks in Nigeria. Beverages 2018, 4, 65. [Google Scholar] [CrossRef] [Green Version]
- Fuhrimann, S.; Klanova, J.; Pribylova, P.; Kohoutek, J.; Dalvie, M.A.; Röösli, M.; Degrendele, C. Qualitative assessment of 27 current-use pesticides in air at 20 sampling sites across Africa. Chemosphere 2020, 258, 127333. [Google Scholar] [CrossRef]
- Veludo, A.F.; Martins Figueiredo, D.; Degrendele, C.; Masinyana, L.; Curchod, L.; Kohoutek, J.; Kukucka, P.; Martinik, J.; Pribylova, P.; Klanova, J.; et al. Seasonal variations in air concentrations of 27 organochlorine pesticides (OCPs) and 25 current-use pesticides (CUPs) across three agricultural areas of South Africa. Chemosphere 2022, 289, 133162. [Google Scholar] [CrossRef]
- Curchod, L.; Oltramare, C.; Junghans, M.; Stamm, C.; Dalvie, M.A.; Röösli, M.; Fuhrimann, S. Temporal variation of pesticide mixtures in rivers of three agricultural watersheds during a major drought in the Western Cape, South Africa. Water Res. X 2020, 6, 100039. [Google Scholar] [CrossRef] [PubMed]
- Fuhrimann, S.; Mol, H.G.J.; Dias, J.; Dalvie, M.A.; Röösli, M.; Degrendele, C.; Figueiredo, D.M.; Huss, A.; Portengen, L.; Vermeulen, R. Quantitative assessment of multiple pesticides in silicone wristbands of children/guardian pairs living in agricultural areas in South Africa. Sci. Total Environ. 2022, 812, 152330. [Google Scholar] [CrossRef] [PubMed]
- Donald, C.E.; Scott, R.P.; Blaustein, K.L.; Halbleib, M.L.; Sarr, M.; Jepson, P.C.; Anderson, K.A. Silicone wristbands detect individuals’ pesticide exposures in West Africa. R. Soc. Open Sci. 2016, 3, 160433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degrendele, C.; Klanova, J.; Prokes, R.; Pribylova, P.; Senk, P.; Sudoma, M.; Röösli, M.; Dalvie, M.A.; Fuhrimann, S. Current use pesticides in soil and air from two agricultural sites in South Africa: Implications for environmental fate and human exposure. Sci. Total Environ. 2022, 807 Pt 1, 150455. [Google Scholar] [CrossRef] [PubMed]
- Eskenazi, B.; Marks, A.R.; Bradman, A.; Harley, K.; Barr, D.B.; Johnson, C.; Morga, N.; Jewell, N.A. Organophosphate pesticide exposure and neurodevelopment in young Mexican-American children. Environ. Health Perspect. 2007, 115, 792–798. [Google Scholar] [CrossRef]
- Naidoo, S.; London, L.; Rother, H.A.; Burdorf, A.; Naidoo, R.N.; Kromhout, H. Pesticide safety training and practices in women working in small-scale agriculture in South Africa. Occup. Environ. Med. 2010, 67, 823–828. [Google Scholar] [CrossRef] [Green Version]
- Solomon, G.M.; Moodley, J. Acute chlorpyrifos poisoning in pregnancy: A case report. Clin. Toxicol. 2007, 45, 416–419. [Google Scholar] [CrossRef]
- Mora, A.M.; Hoppin, J.A.; Cordoba, L.; Cano, J.C.; Soto-Martinez, M.; Eskenazi, B.; Lindh, C.H.; de Joode, B.V. Prenatal pesticide exposure and respiratory health outcomes in the first year of life: Results from the infants’ Environmental Health (ISA) study. Int. J. Hyg. Environ. Health 2020, 225, 113474. [Google Scholar] [CrossRef]
- de Joode, V. Aerial Application of Mancozeb and Urinary Ethylene Thiourea (ETU) Concentrations among Pregnant Women in Costa Rica: The Infants’ Environmental Health Study (ISA). Environ. Health Perspect. 2014, 122, A321. [Google Scholar]
- Rother, H.A. Pesticide Vendors in the Informal Sector: Trading Health for Income. New Solut. 2016, 26, 241–252. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Chisholm, D.; Eddleston, M.; Gunnell, D.; Fleischmann, A.; Konradsen, F.; Bertram, M.Y.; Mihalopoulos, C.; Brown, R.; Santomauro, D.F.; et al. The cost-effectiveness of banning highly hazardous pesticides to prevent suicides due to pesticide self-ingestion across 14 countries: An economic modelling study. Lancet Glob. Health 2021, 9, E291–E300. [Google Scholar] [CrossRef]
- Balme, K.H.; Roberts, J.C.; Glasstone, M.; Curling, L.; Rother, H.A.; London, L.; Zar, H.; Mann, M.D. Pesticide poisonings at a tertiary children’s hospital in South Africa: An increasing problem. Clin. Toxicol. 2010, 48, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Rother, H.A. Falling Through the Regulatory Cracks Street Selling of Pesticides and Poisoning among Urban Youth in South Africa. Int. J. Occup. Environ. Health 2010, 16, 202–213. [Google Scholar] [CrossRef]
- Godsmark, C.N.; Rother, H.A. Part of the solution—An engaged scholarship approach for the sustainable reduction of street pesticides and poisonings. Glob. Public Health 2019, 14, 1535–1545. [Google Scholar] [CrossRef] [Green Version]
- London, L.; Bailie, R. Challenges for improving surveillance for pesticide poisoning: Policy implications for developing countries. Int. J. Epidemiol. 2001, 30, 564–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).