Bibliometric Analysis of Health Technology Research: 1990~2020
Abstract
:1. Introduction
2. Materials and Methods
2.1. Methodology and Tools
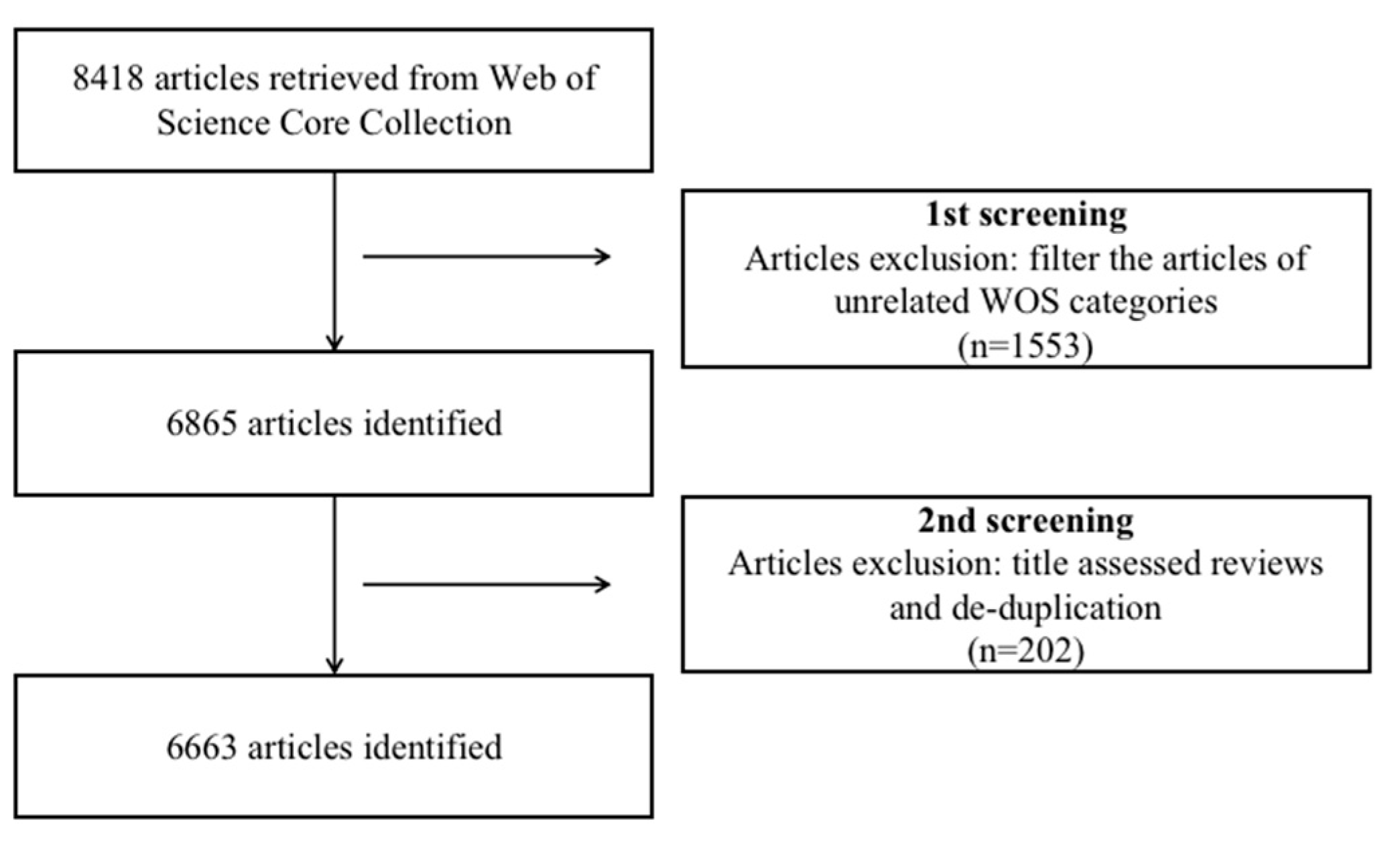
2.2. Data Collection
3. Results
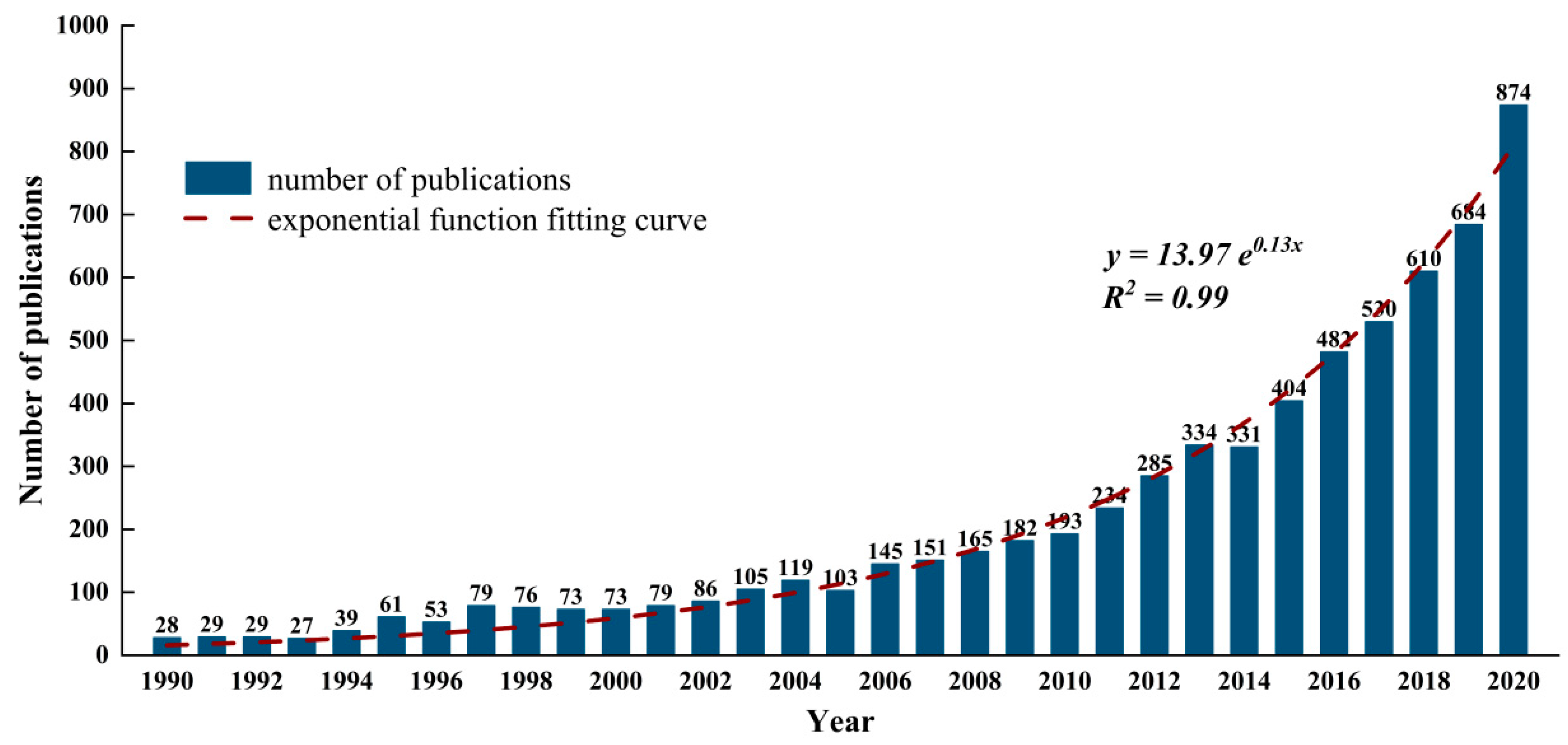
3.1. Publication Trend Analysis
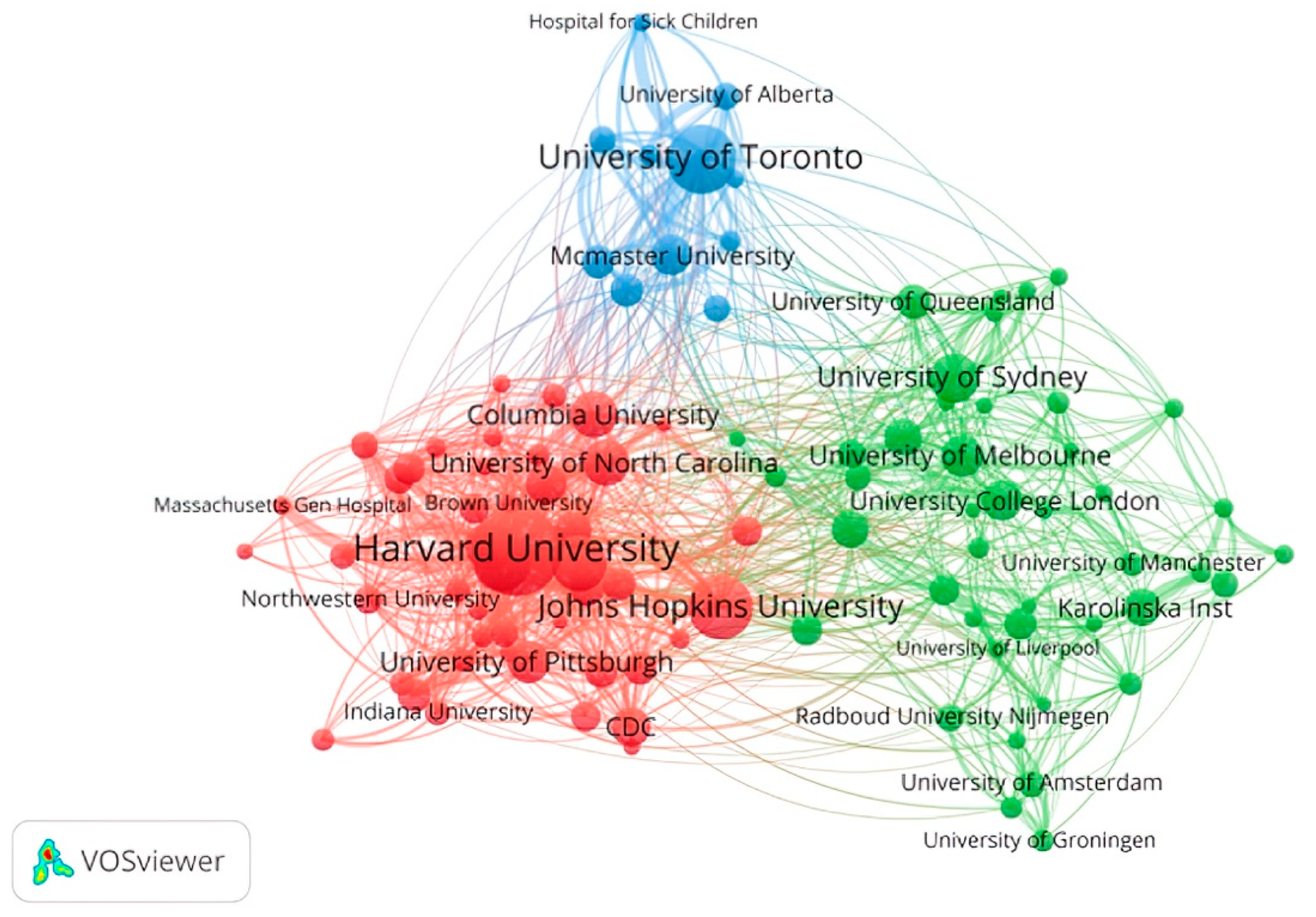
3.2. Distribution Analysis of Authors, Journals, and Institutions
4. Research Topics and Evolution Analysis
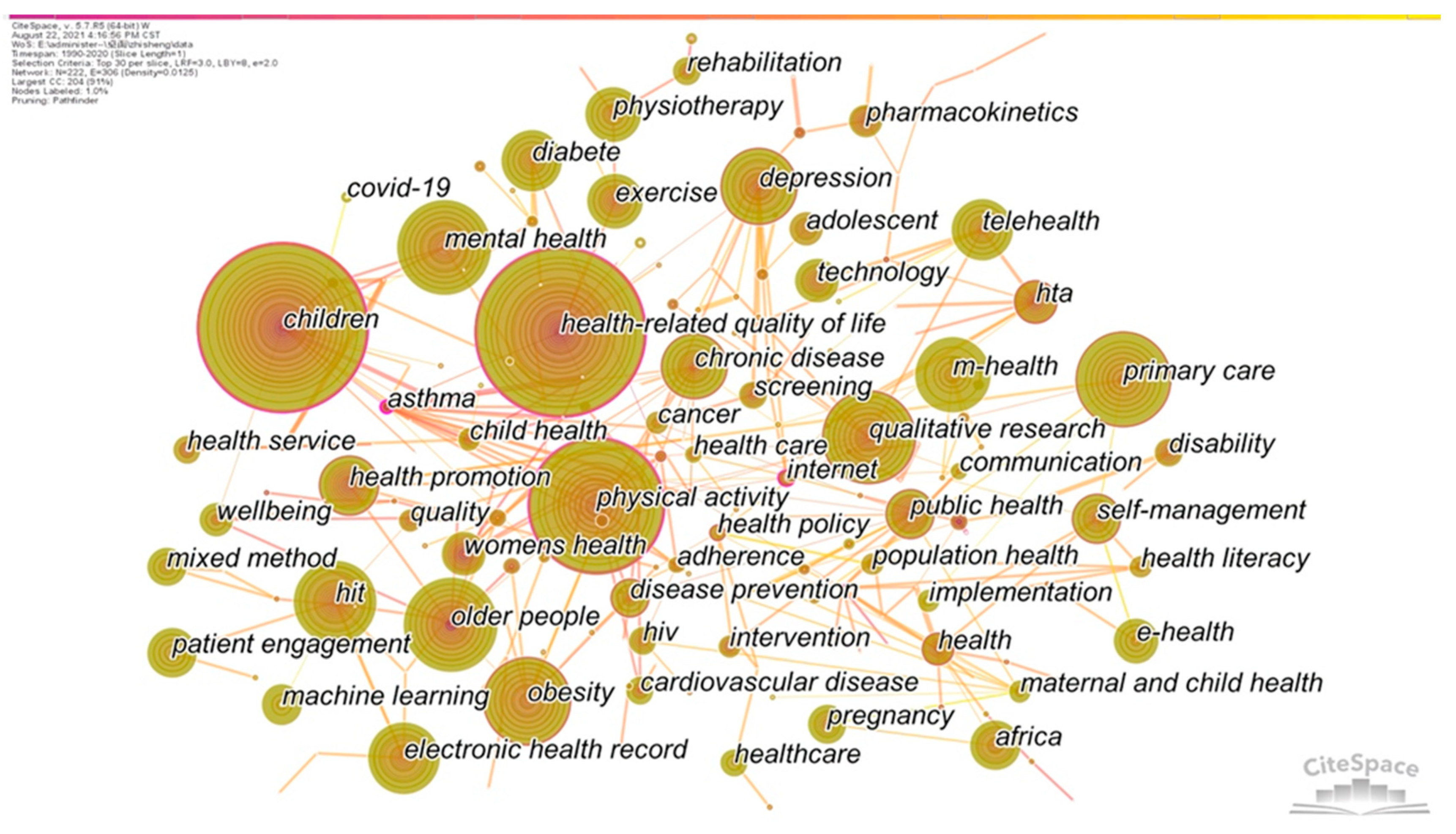
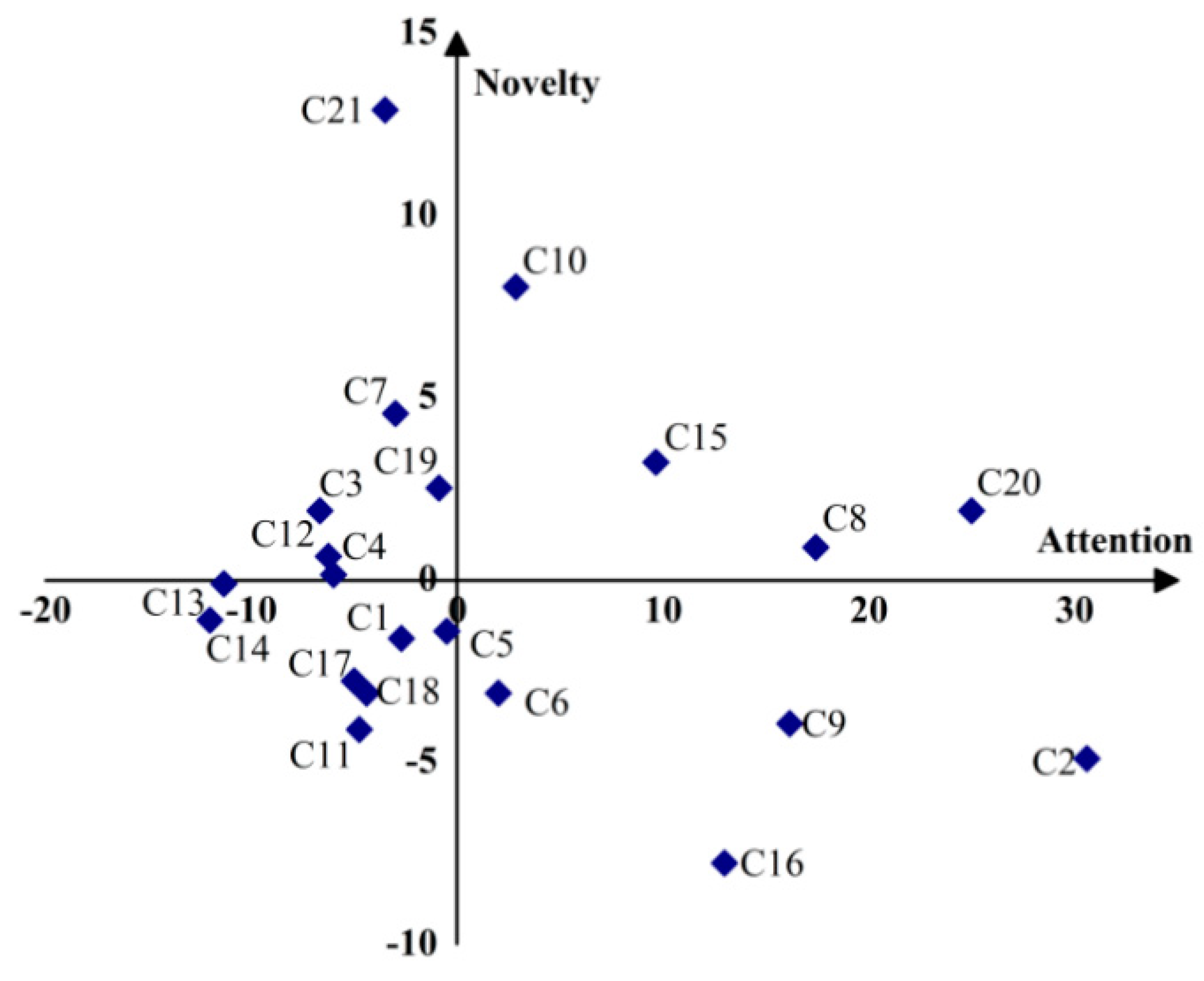
4.1. The Research Topics Analysis
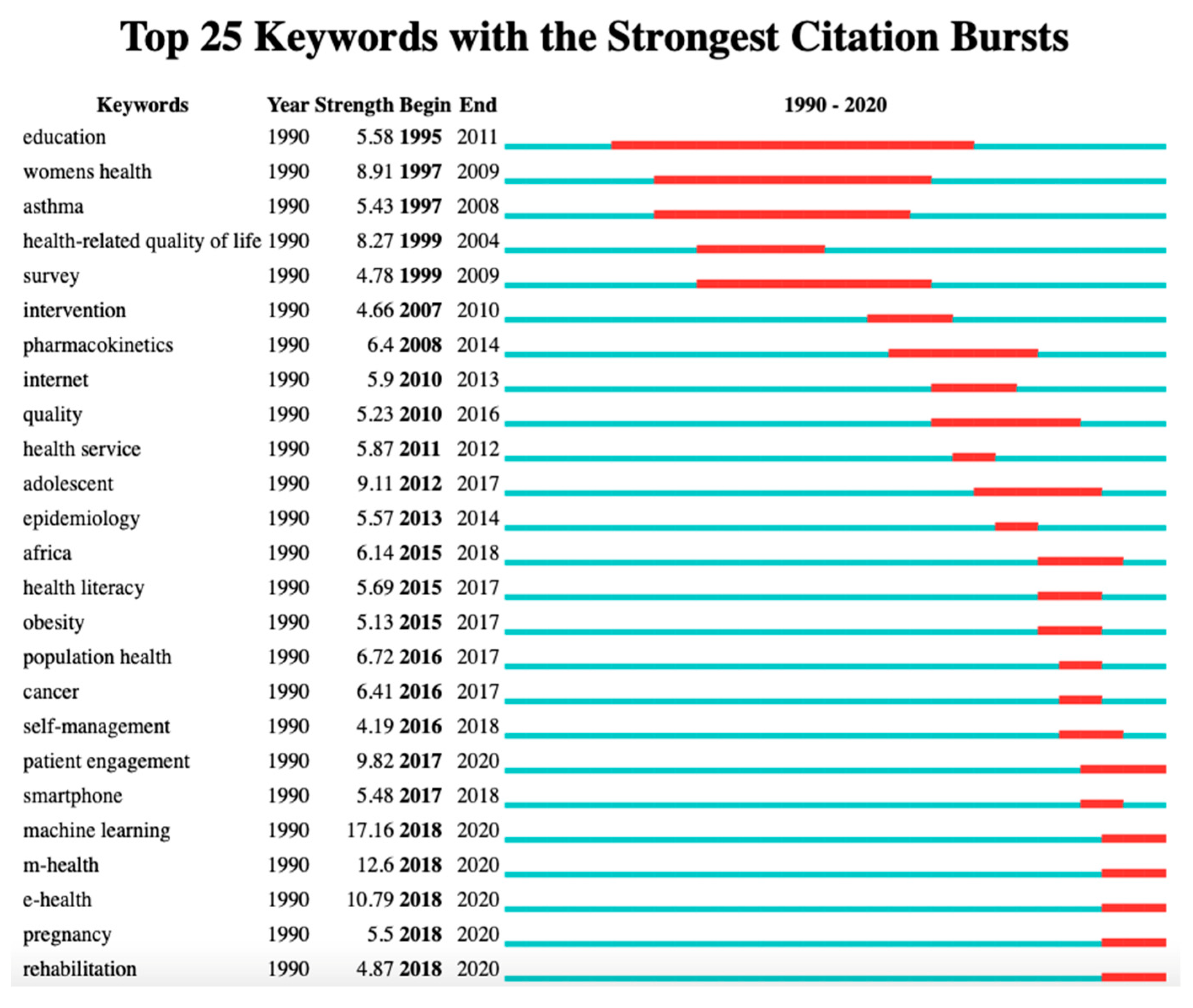
4.2. Research Frontiers Analysis
4.3. Industry 4.0 Technologies Supporting the Health Sector
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oortwijn, W.; Banta, D.; Vondeling, H.; Bouter, L. Identification and priority setting for health technology assessment in The Netherlands: Actors and activities. Health Policy 1999, 47, 241–253. [Google Scholar] [CrossRef]
- Eldar, R. Health technology: Challenge to public health. Croat. Med. J. 2002, 43, 470–474. [Google Scholar] [PubMed]
- Garrido, M.V.; Gerhardus, A.; Røttingen, J.A.; Busse, R. Developing health technology assessment to address health care system needs. Health Policy 2010, 94, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Sixtieth World Health Assembly WHA60.29 Health Technologies. Available online: https://www.who.int/healthsystems/WHA60_29.pdf (accessed on 25 December 2020).
- Inahta Hta Glossary. Available online: http://htaglossary.net/health-technology (accessed on 25 December 2020).
- Banta, H.D. Perspective: Some conclusions from my life in health technology assessment. Int. J. Technol. Assess. Health Care 2018, 34, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Banta, D.; Jonsson, E. History of HTA: Introduction. Int. J. Technol. Assess. Health Care 2009, 25 (Suppl. S1), 1–6. [Google Scholar] [CrossRef] [Green Version]
- Sadiku, M.N.; Akhare, Y.P.; Musa, S.M. Emerging technologies in healthcare: A tutorial. Int. J. Adv. Sci. Res. Eng. 2019, 5, 199–204. [Google Scholar] [CrossRef]
- Dunn, P.; Hazzard, E. Technology approaches to digital health literacy. Int. J. Cardiol. 2019, 293, 294–296. [Google Scholar] [CrossRef]
- Aceto, G.; Persico, V.; Pescapé, A. Industry 4.0 and health: Internet of things, big data, and cloud computing for healthcare 4.0. J. Ind. Inf. Integr. 2020, 18, 100129. [Google Scholar] [CrossRef]
- Phillips, S.A.; Ali, M.; Modrich, C.; Oke, S.; Elokda, A.; Laddu, D.; Bond, S. Advances in health technology use and implementation in the era of healthy living: Implications for precision medicine. Prog. Cardiovasc. Dis. 2019, 62, 44–49. [Google Scholar] [CrossRef]
- Gottge, S.; Menzel, T.; Forslund, H. Industry 4.0 technologies in the purchasing process. Ind. Manag. Data Syst. 2020, 120, 730–748. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A. Industry 4.0 applications in medical field: A brief review. Curr. Med. Res. Pract. 2019, 9, 102–109. [Google Scholar] [CrossRef]
- Pai, R.R.; Alathur, S. Bibliometric analysis and methodological review of mobile health services and applications in India. Int. J. Med. Inform. 2021, 145, 104330. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Huang, S.; Qiu, C.; Liu, S.; Deng, J.; Jiao, B.; Tan, X.; Ai, L.; Xiao, Y.; Belliato, M.; et al. Monitoring and management of home-quarantined patients with COVID-19 using a WChat-based telemedicine system: Retrospective cohort study. J. Med. Internet Res. 2020, 22, e19514. [Google Scholar] [CrossRef] [PubMed]
- Hynes, D.M.; Weddle, T.; Smith, N.; Whittier, E.; Atkins, D.; Francis, J. Use of health information technology to advance evidence-based care: Lessons from the VA QUERI program. J. Gen. Intern. Med. 2010, 25, 44–49. [Google Scholar] [CrossRef]
- Health Information Technology in the United States: Where We Stand. 2008. Available online: https://folio.iupui.edu/bitstream/handle/10244/784/hitreport.pdf (accessed on 22 May 2021).
- Wild, C.; Langer, T. Emerging health technologies: Informing and supporting Health Policy early. Health Policy 2008, 87, 160–171. [Google Scholar] [CrossRef]
- Lupton, D. Young people’s use of digital health technologies in the global north: Narrative review. J. Med. Internet Res. 2021, 23, e18286. [Google Scholar] [CrossRef]
- Penno, E.; Gauld, R. Change, connectivity, and challenge: Exploring the role of health technology in shaping health care for aging populations in Asia Pacific. Health Syst. Reform 2017, 3, 224–235. [Google Scholar] [CrossRef] [Green Version]
- Sweileh, W.M.; Al-Jabi, S.W.; AbuTaha, A.S.; Zyoud, S.E.H.; Anayah, F.; Sawalha, A.F. Bibliometric analysis of worldwide scientific literature in mobile-health: 2006–2016. BMC Med. Inform. Decis. Mak. 2017, 17, 72. [Google Scholar] [CrossRef] [Green Version]
- Waqas, A.; Teoh, S.H.; Lapão, L.V.; Messina, L.A.; Correia, J.C. Harnessing telemedicine for the provision of health care: Bibliometric and scientometric analysis. J. Med. Internet Res. 2020, 22, e18835. [Google Scholar] [CrossRef]
- Gu, D.; Li, T.; Wang, X.; Yang, X.; Yu, Z. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. Int. J. Med. Inform. 2019, 130, 103947. [Google Scholar] [CrossRef]
- Yang, X.; Wang, X.; Li, X.; Gu, D.; Liang, C.; Li, K.; Zhang, G.; Zhong, J. Exploring emerging IoT technologies in smart health research: A knowledge graph analysis. BMC Med. Inform. Decis. Mak. 2020, 20, 260. [Google Scholar] [CrossRef] [PubMed]
- Sood, S.K.; Rawat, K.S.; Kumar, D. A visual review of artificial intelligence and Industry 4.0 in healthcare. Comput. Electr. Eng. 2022, 101, 107948. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Yang, X.; Deng, S.; Liang, C.; Wang, X.; Wu, J.; Guo, J. Tracking knowledge evolution in cloud health care research: Knowledge map and common word analysis. J. Med. Internet Res. 2020, 22, e15142. [Google Scholar] [CrossRef]
- Anjum, H.F.; Rasid, S.Z.A.; Khalid, H.; Alam, M.M.; Daud, S.M.; Abas, H.; Sam, S.M.; Yusof, M.F. Mapping research trends of blockchain technology in healthcare. IEEE Access 2020, 8, 174244–174254. [Google Scholar] [CrossRef]
- Liu, Z.; Ren, L.; Xiao, C.; Zhang, K.; Demian, P. Virtual reality aided therapy towards health 4.0: A two-decade bibliometric analysis. Int. J. Environ. Res. Public Health 2022, 19, 1525. [Google Scholar] [CrossRef]
- Kim, A.R.; Park, H.Y. Theme trends and knowledge-relationship in lifestyle research: A bibliometric analysis. Int. J. Environ. Res. Public Health 2021, 18, 7503. [Google Scholar] [CrossRef] [PubMed]
- Dang, Q.; Luo, Z.; Ouyang, C.; Wang, L. First Systematic Review on Health Communication Using the CiteSpace Software in China: Exploring Its Research Hotspots and Frontiers. Int. J. Environ. Res. Public Health 2021, 18, 13008. [Google Scholar] [CrossRef] [PubMed]
- Cobo, M.J.; López-Herrera, A.G.; Herrera-Viedma, E.; Herrera, F. An approach for detecting, quantifying, and visualizing the evolution of a research field: A practical application to the Fuzzy Sets Theory field. J. Informetr. 2011, 5, 146–166. [Google Scholar] [CrossRef]
- Small, H. Visualizing science by citation mapping. J. Am. Soc. Inf. Sci. 1999, 50, 799–813. [Google Scholar] [CrossRef]
- Small, H. Co-citation in the scientific literature: A new measure of the relationship between two documents. J. Am. Soc. Inf. Sci. 1973, 24, 265–269. [Google Scholar] [CrossRef]
- Callon, M.; Courtial, J.P.; Turner, W.A.; Bauin, S. From translations to problematic networks: An introduction to co-word analysis. Soc. Sci. Inf. 1983, 22, 191–235. [Google Scholar] [CrossRef]
- Mora, L.; Deakin, M.; Reid, A. Combining co-citation clustering and text-based analysis to reveal the main development paths of smart cities. Technol. Forecast. Soc. Chang. 2019, 142, 56–69. [Google Scholar] [CrossRef]
- Wang, L.; Xia, E.; Li, H.; Wang, W. A bibliometric analysis of crowdsourcing in the field of public health. Int. J. Environ. Res. Public Health 2019, 16, 3825. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Mao, Y.; Ouyang, J.; Zheng, S. A Review of Urban Microclimate Research Based on CiteSpace and VOSviewer Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4741. [Google Scholar] [CrossRef] [PubMed]
- Eck, N.J.V.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar]
- Chen, C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J. Am. Soc. Inf. Sci. Technol. 2006, 57, 359–377. [Google Scholar] [CrossRef] [Green Version]
- Callon, M.; Courtial, J.P.; Laville, F. Co-word analysis as a tool for describing the network of interactions between basic and technological research: The case of polymer chemsitry. Scientometrics 1991, 22, 155–205. [Google Scholar] [CrossRef]
- Law, J.; Bauin, S.; Courtial, J.; Whittaker, J. Policy and the mapping of scientific change: A co-word analysis of research into environmental acidification. Scientometrics 1988, 14, 251–264. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 105906. [Google Scholar]
- Qi, B.; Jin, S.; Qian, H.; Zou, Y. Bibliometric analysis of chronic traumatic encephalopathy research from 1999 to 2019. Int. J. Environ. Res. Public Health 2020, 17, 5411. [Google Scholar] [CrossRef]
- Selva-Pareja, L.; Ramos-Pla, A.; Mercadé-Melé, P.; Espart, A. Evolution of Scientific Production on Health Literacy and Health Education—A Bibliometric Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4356. [Google Scholar] [CrossRef]
- Zhao, Y.; Guo, J.; Bao, C.; Liang, C.; Jain, H.K. Knowledge graph analysis of human health research related to climate change. Int. J. Environ. Res. Public Health 2020, 17, 7395. [Google Scholar] [CrossRef] [PubMed]
- Price, D.J. Little Science, Big Science... and Beyond; Columbia University Press: New York, NY, USA, 1986. [Google Scholar]
- Scott, B.K.; Miller, G.T.; Fonda, S.J.; Yeaw, R.E.; Gaudaen, J.C.; Pavliscsak, H.H.; Pamplin, J.C. Advanced digital health technologies for COVID-19 and future emergencies. Telemed. E-Health 2020, 26, 1226–1233. [Google Scholar] [CrossRef] [PubMed]
- Aminullah, E.; Erman, E. Policy innovation and emergence of innovative health technology: The system dynamics modelling of early COVID-19 handling in Indonesia. Technol. Soc. 2021, 66, 101682. [Google Scholar] [CrossRef]
- Magrabi, F.; Ammenwerth, E.; Craven, C.K.; Cresswell, K.; DeKeizer, N.F.; Medlock, S.K.; Georgiou, A. Managing Pandemic Responses with Health Informatics—Challenges for Assessing Digital Health Technologies. Yearb. Med. Inform. 2021, 30, 056–060. [Google Scholar] [CrossRef]
- Mukherjee, K. Relevance of the newly defined Health Technology Assessment: COVID-19 and beyond. Int. J. Technol. Assess. Health Care 2021, 37, e44. [Google Scholar] [CrossRef]
- Mahajan, S.; Lu, Y.; Spatz, E.S.; Nasir, K.; Krumholz, H.M. Trends and predictors of use of digital health technology in the United States. Am. J. Med. 2021, 134, 129–134. [Google Scholar] [CrossRef]
- Zaresani, A.; Scott, A. Does digital health technology improve physicians’ job satisfaction and work–life balance? A cross-sectional national survey and regression analysis using an instrumental variable. BMJ Open 2020, 10, e041690. [Google Scholar] [CrossRef]
- Sun, X.; Yan, W.; Zhou, H.; Wang, Z.; Zhang, X.; Huang, S.; Li, L. Internet use and need for digital health technology among the elderly: A cross-sectional survey in China. BMC Public Health 2020, 20, 1386. [Google Scholar] [CrossRef]
- Marsch, L.A. Digital health data-driven approaches to understand human behavior. Neuropsychopharmacology 2021, 46, 191–196. [Google Scholar] [CrossRef]
- Dhingra, D.; Dabas, A. Global strategy on digital health. Indian Pediatrics 2020, 57, 356–358. [Google Scholar] [CrossRef]
- Ye, N.; Kueh, T.B.; Hou, L.; Liu, Y.; Yu, H. A bibliometric analysis of corporate social responsibility in sustainable development. J. Clean. Prod. 2020, 272, 122679. [Google Scholar] [CrossRef]
- Pfeiffer, S. The vision of “Industrie 4.0” in the making—A case of future told, tamed, and traded. Nanoethics 2017, 11, 107–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dragicevic, N.; Ullrich, A.; Tsui, E.; Gronau, N. A conceptual model of knowledge dynamics in the industry 4.0 smart grid scenario. Knowl. Manag. Res. Pract. 2019, 18, 199–213. [Google Scholar] [CrossRef]
- Mariani, M.; Borghi, M. Industry 4.0: A bibliometric review of its managerial intellectual structure and potential evolution in the service industries. Technol. Forecast. Soc. Chang. 2019, 149, 119752. [Google Scholar] [CrossRef]
- Asif, M. Are QM models aligned with Industry 4.0? A perspective on current practices. J. Clean. Prod. 2020, 258, 120820. [Google Scholar] [CrossRef]
- Bruzzone, A.; Massei, M.; Sinelshnkov, K. Enabling strategic decisions for the industry of tomorrow. Procedia Manuf. 2020, 42, 548–553. [Google Scholar] [CrossRef]
- Larrucea, X.; Moffie, M.; Asaf, S.; Santamaria, I. Towards a GDPR compliant way to secure European cross border Healthcare Industry 4.0. Comput. Stand. Interfaces 2020, 69, 103408. [Google Scholar] [CrossRef]
- Tortorella, G.L.; Fogliatto, F.S.; Mac Cawley Vergara, A.; Vassolo, R.; Sawhney, R. Healthcare 4.0: Trends, challenges and research directions. Prod. Plan. Control. 2020, 31, 1245–1260. [Google Scholar] [CrossRef]
- Jayaraman, P.P.; Forkan, A.R.M.; Morshed, A.; Haghighi, P.D.; Kang, Y.B. Healthcare 4.0: A review of frontiers in digital health. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2020, 10, e1350. [Google Scholar] [CrossRef]
- Hathaliya, J.J.; Tanwar, S.; Tyagi, S.; Kumar, N. Securing electronics healthcare records in healthcare 4.0: A biometric-based approach. Comput. Electr. Eng. 2019, 76, 398–410. [Google Scholar] [CrossRef]
- Tortorella, G.L.; Fogliatto, F.S.; Espôsto, K.F.; Vergara, A.M.C.; Vassolo, R.; Mendoza, D.T.; Narayanamurthy, G. Effects of contingencies on healthcare 4.0 technologies adoption and barriers in emerging economies. Technol. Forecast. Soc. Chang. 2020, 156, 120048. [Google Scholar] [CrossRef]
- Tanwar, S.; Parekh, K.; Evans, R. Blockchain-based electronic healthcare record system for healthcare 4.0 applications. J. Inf. Secur. Appl. 2020, 50, 102407. [Google Scholar] [CrossRef]
- Estrela, V.V.; Monteiro, A.C.B.; França, R.P.; Iano, Y.; Khelassi, A.; Razmjooy, N. Health 4.0: Applications, management, technologies and review. Med. Technol. J. 2018, 2, 262–276. [Google Scholar]
- Dimitrov, D.V. Medical internet of things and big data in healthcare. Healthc. Inform. Res. 2016, 22, 156–163. [Google Scholar] [CrossRef]
- Islam, S.R.; Kwak, D.; Kabir, M.H.; Hossain, M.; Kwak, K.S. The internet of things for health care: A comprehensive survey. IEEE Access 2015, 3, 678–708. [Google Scholar] [CrossRef]
- Kwon, S.; Kim, H.; Yeo, W.H. Recent advances in wearable sensors and portable electronics for sleep monitoring. Iscience 2021, 24, 102461. [Google Scholar] [CrossRef] [PubMed]
- Dinh-Le, C.; Chuang, R.; Chokshi, S.; Mann, D. Wearable Health Technology and Electronic Health Record Integration: Scoping Review and Future Directions. JMIR Mhealth Uhealth 2019, 7, e12861. [Google Scholar] [CrossRef]
- Suver, C.; Kuwana, E. mHealth wearables and smartphone health tracking apps: A changing privacy landscape. Inf. Serv. Use 2021, 41, 71–79. [Google Scholar] [CrossRef]
- Cerchione, R.; Centobelli, P.; Riccio, E.; Abbate, S.; Oropallo, E. Blockchain’s coming to hospital to digitalize healthcare services: Designing a distributed electronic health record ecosystem. Technovation, 2022; in press. [Google Scholar] [CrossRef]
- Esmaeilzadeh, P. Benefits and concerns associated with blockchain-based health information exchange (HIE): A qualitative study from physicians’ perspectives. BMC Med. Inform. Decis. Mak. 2022, 22, 80. [Google Scholar] [CrossRef] [PubMed]
- Kuo, T.T.; Kim, H.E.; Ohno-Machado, L. Blockchain distributed ledger technologies for biomedical and health care applications. J. Am. Med. Inform. Assoc. 2017, 24, 1211–1220. [Google Scholar] [CrossRef] [Green Version]
- Fatoum, H.; Hanna, S.; Halamka, J.D.; Sicker, D.C.; Spangenberg, P.; Hashmi, S.K. Blockchain integration with digital technology and the future of health care ecosystems: Systematic review. J. Med. Internet Res. 2021, 23, e19846. [Google Scholar] [CrossRef]
- Chattu, V.K. A review of artificial intelligence, big data, and blockchain technology applications in medicine and global health. Big Data Cogn. Comput. 2021, 5, 41. [Google Scholar]
- Zhuang, Y.; Chen, Y.W.; Shae, Z.Y.; Shyu, C.R. Generalizable layered blockchain architecture for health care applications: Development, case studies, and evaluation. J. Med. Internet Res. 2020, 22, e19029. [Google Scholar] [CrossRef] [PubMed]
- Ichikawa, D.; Kashiyama, M.; Ueno, T. Tamper-resistant mobile health using blockchain technology. JMIR Mhealth Uhealth 2017, 5, e7938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abunadi, I.; Kumar, R.L. Blockchain and business process management in health care, especially for COVID-19 cases. Secur. Commun. Netw. 2021, 2021, 2245808. [Google Scholar] [CrossRef]
- The Lancet. Artificial intelligence in health care: Within touching distance. Lancet 2017, 390, 2739. [Google Scholar] [CrossRef]
- Shafqat, S.; Kishwer, S.; Rasool, R.U.; Qadir, J.; Amjad, T.; Ahmad, H.F. Big data analytics enhanced healthcare systems: A review. J. Supercomput. 2020, 76, 1754–1799. [Google Scholar] [CrossRef]
- Jameson, J.L.; Longo, D.L. Precision medicine-personalized, problematic, and promising. N. Engl. J. Med. 2015, 372, 2229–2234. [Google Scholar] [CrossRef] [Green Version]
- Smith, H. Clinical AI: Opacity, accountability, responsibility and liability. AI Soc. 2021, 36, 535–545. [Google Scholar] [CrossRef]
- Ruan, Q.; Yang, K.; Wang, W.; Jiang, L.; Song, J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020, 46, 846–848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alimadadi, A.; Aryal, S.; Manandhar, I.; Munroe, P.B.; Joe, B.; Cheng, X. Artificial intelligence and machine learning to fight COVID-19. Physiol. Genom. 2020, 52, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Haleem, A.; Vaishya, R.; Bahl, S.; Suman, R.; Vaish, A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 419–422. [Google Scholar] [CrossRef] [PubMed]
- Bélisle-Pipon, J.C.; Couture, V.; Roy, M.C.; Ganache, I.; Goetghebeur, M.; Cohen, I.G. What makes artificial intelligence exceptional in health technology assessment? Front. Artif. Intell. 2021, 4, 736697. [Google Scholar] [CrossRef]
- Hendrix, N.; Veenstra, D.L.; Cheng, M.; Anderson, N.C.; Verguet, S. Assessing the Economic Value of Clinical Artificial Intelligence: Challenges and Opportunities. Value Health 2022, 25, 331–339. [Google Scholar] [CrossRef]
- Rowe, J.P.; Lester, J.C. Artificial intelligence for personalized preventive adolescent healthcare. J. Adolesc. Health 2020, 67, S52–S58. [Google Scholar] [CrossRef]
- Paul, S.; Riffat, M.; Yasir, A.; Mahim, M.N.; Sharnali, B.Y.; Naheen, I.T.; Rahman, A.; Kulkarni, A. Industry 4.0 applications for medical/healthcare services. J. Sens. Actuator Netw. 2021, 10, 43. [Google Scholar] [CrossRef]
- Yu, W.; Choi, J. Human identification in health care systems using mobile edge computing. Trans. Emerg. Telecommun. Technol. 2020, 31, e4031. [Google Scholar] [CrossRef]
- Lakshmi, G.J.; Ghonge, M.; Obaid, A.J. Cloud based iot smart healthcare system for remote patient monitoring. EAI Endorsed Trans. Pervasive Health Technol. 2021, 7, e4. [Google Scholar] [CrossRef]
- Alabdulatif, A.; Khalil, I.; Forkan, A.R.M.; Atiquzzaman, M. Real-time secure health surveillance for smarter health communities. IEEE Commun. Mag. 2018, 57, 122–129. [Google Scholar] [CrossRef]
| Retrieve | Retrieval Expression |
|---|---|
| #1 | TI = (“health *” or “well *” or “physi *” or “sound*” or “fit *” or “wholesome *”) |
| #2 | TI = (“technology *” or “technique” or “facility” or “device *” or “apparatus” or “tool *” or “equipment” or “machine *” or “means” or “approach *” or “method *” or “solution *” or “procedure *” or “way *”) |
| #3 | TI = (“man *” or “wom?n” or “person” or “people” or “child *” or “adult” or “teenager” or “elder” or “human *” or “citizen” or “population” or “sufferer” or “patient *” or “invalid” or “disease *” or “ill *” or “pathema” or “ailment *” or “malady” or “sick *” or “weak *” or “non-health” or “unhealth *” or “unwell *”or “unsound *” or “indisposed” or “uncomfortable *” or “discomfort *” or “sub-health” or “semi-health”) |
| No. | Authors | Number of Publications | Citations |
|---|---|---|---|
| 1 | Marie-Pierre Gagnon | 9 | 168 |
| 2 | France Legare | 8 | 265 |
| 3 | Brian Maccrindle | 7 | 245 |
| 4 | Ding Li | 7 | 11 |
| 5 | VR Young | 6 | 261 |
| 6 | Francois-Pierre Gauvin | 6 | 229 |
| 7 | Trudy Van Der Weijden | 6 | 157 |
| 8 | Marie Desmartis | 6 | 156 |
| 9 | Johanne Gagnon | 6 | 156 |
| 10 | Julia Abelson | 6 | 139 |
| No. | Journal | Country | Number of Publications | Citations |
|---|---|---|---|---|
| 1 | PLOS ONE | The United States | 125 | 1405 |
| 2 | BMC HEALTH SERVICES RESEARCH | The United Kingdom | 111 | 1196 |
| 3 | BMC PUBLIC HEALTH | The United Kingdom | 93 | 1190 |
| 4 | BMJ OPEN | The United Kingdom | 87 | 503 |
| 5 | JOURNAL OF MEDICAL INTERNET RESEARCH | Canada | 66 | 948 |
| 6 | INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH | Switzerland | 53 | 331 |
| 7 | JMIR MHEALTH AND UHEALTH | Canada | 48 | 320 |
| 8 | INTERNATIONAL JOURNAL OF TECHNOLOGY ASSESSMENT IN HEALTH CARE | The United Kingdom | 45 | 919 |
| 9 | QUALITY OF LIFE RESEARCH | Netherlands | 40 | 1042 |
| 10 | SOCIAL SCIENCE & MEDICINE | The United Kingdom | 37 | 991 |
| Institution | Cluster | Number of Links | Linking Strength | Number of Publications | Citations |
|---|---|---|---|---|---|
| Harvard University | 1 | 60 | 102 | 145 | 3855 |
| University of Toronto | 3 | 35 | 76 | 123 | 2239 |
| Johns Hopkins University | 1 | 60 | 57 | 113 | 3471 |
| University of California, San Francisco | 1 | 52 | 58 | 96 | 2308 |
| University of Washington | 1 | 58 | 50 | 90 | 2961 |
| University of Sydney | 2 | 32 | 41 | 85 | 1358 |
| University of Michigan | 1 | 49 | 41 | 81 | 1727 |
| Columbia University | 1 | 44 | 45 | 77 | 1462 |
| University of North Carolina | 1 | 40 | 33 | 75 | 1603 |
| University of Pittsburgh | 1 | 38 | 39 | 70 | 1676 |
| No. | Research Topic | Keywords (Co-Occurrence Counts) |
|---|---|---|
| C1 | Health management | health (41); pressure (4); physical illness (2); education (13); survey (9); risk (5); outpatient service (10); mortality (2); Africa (44); diagnosis (3) |
| C2 | Child health | health status (2); asthma (16); children (198); guideline (9); health care cost (4); child health (20); parent (17); adherence (2); chronic obstructive pulmonary disease (9); quality of life (189) |
| C3 | Assistive technology | assistive technology (4); disability (22); cerebral palsy (2) |
| C4 | Pharmacokinetics | muraglitazar (2); lc-ms/m (8); pharmacokinetics (28); anti-psychotic (2) |
| C5 | Disease prevention | obesity (73); nutrition (6); diet (6); barriers (2); schoolchildren (2); body composition (14); risk factors (7); disease prevention (40); ethnicity (2); body image (3) |
| C6 | Risk assessment | health education (2); diabetes (56); risk assessment (12); meta-analysis (2) |
| C7 | adolescent health | sexual health (3); young people (7); adolescent (29) |
| C8 | Telemedicine | technology (10); telemedicine (66); HTA (42); qualitative research (94); heart failure (9); patient satisfaction (8); patient reported outcome (5) |
| C9 | Health technology assessment | quality (2); evaluation (14); older people (84); methodology (12); HIT (76); trauma (5) |
| C10 | Digital health technology | m-health (96); mobile phone (6); smart phone (11); task shifting (3); community health workers (3); India (4); digital health (9) |
| C11 | Well-being method | reliability (4); systematic review (2); well-being (27); methods (12) |
| C12 | Internet | breast cancer (5); shared decision making (2); communication (17); Internet (15) |
| C13 | Mass spectrometry | bio-marker (2); human plasma (6); mass spectrometry (4) |
| C14 | Data collection | data collection (2); pediatric (4); focus group (8) |
| C15 | Electronic health record | mental illness (2); evidence-based medicine (2); electronic health record (73) |
| C16 | Physical therapy | dementia (10); physical therapy (53); rehabilitation (24) |
| C17 | Female health | women health (46); geriatric (2); pain (4); rural (4); medicare (2) |
| C18 | Health screening | adult (2); validity (10); screening (21) |
| C19 | Public health | Intervention (19); public health (49); cancer (21); tuberculosis (2); care coordination (3); health disparity (6); reproductive health (3); maternal and child health (18) |
| C20 | Health information technology | primary care (120); empowerment (2); health promotion (53); information technology (10); implementation (20) |
| C21 | COVID-19 prevention | mobile application (11); COVID-19 (16) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luo, X.; Wu, Y.; Niu, L.; Huang, L. Bibliometric Analysis of Health Technology Research: 1990~2020. Int. J. Environ. Res. Public Health 2022, 19, 9044. https://doi.org/10.3390/ijerph19159044
Luo X, Wu Y, Niu L, Huang L. Bibliometric Analysis of Health Technology Research: 1990~2020. International Journal of Environmental Research and Public Health. 2022; 19(15):9044. https://doi.org/10.3390/ijerph19159044
Chicago/Turabian StyleLuo, Xiaomei, Yuduo Wu, Lina Niu, and Lucheng Huang. 2022. "Bibliometric Analysis of Health Technology Research: 1990~2020" International Journal of Environmental Research and Public Health 19, no. 15: 9044. https://doi.org/10.3390/ijerph19159044





