Anxiety and Depression in Patients with Prostate Cancer, at Cancer Diagnosis and after a One-Year Follow-Up
Abstract
:1. Introduction
2. Methods
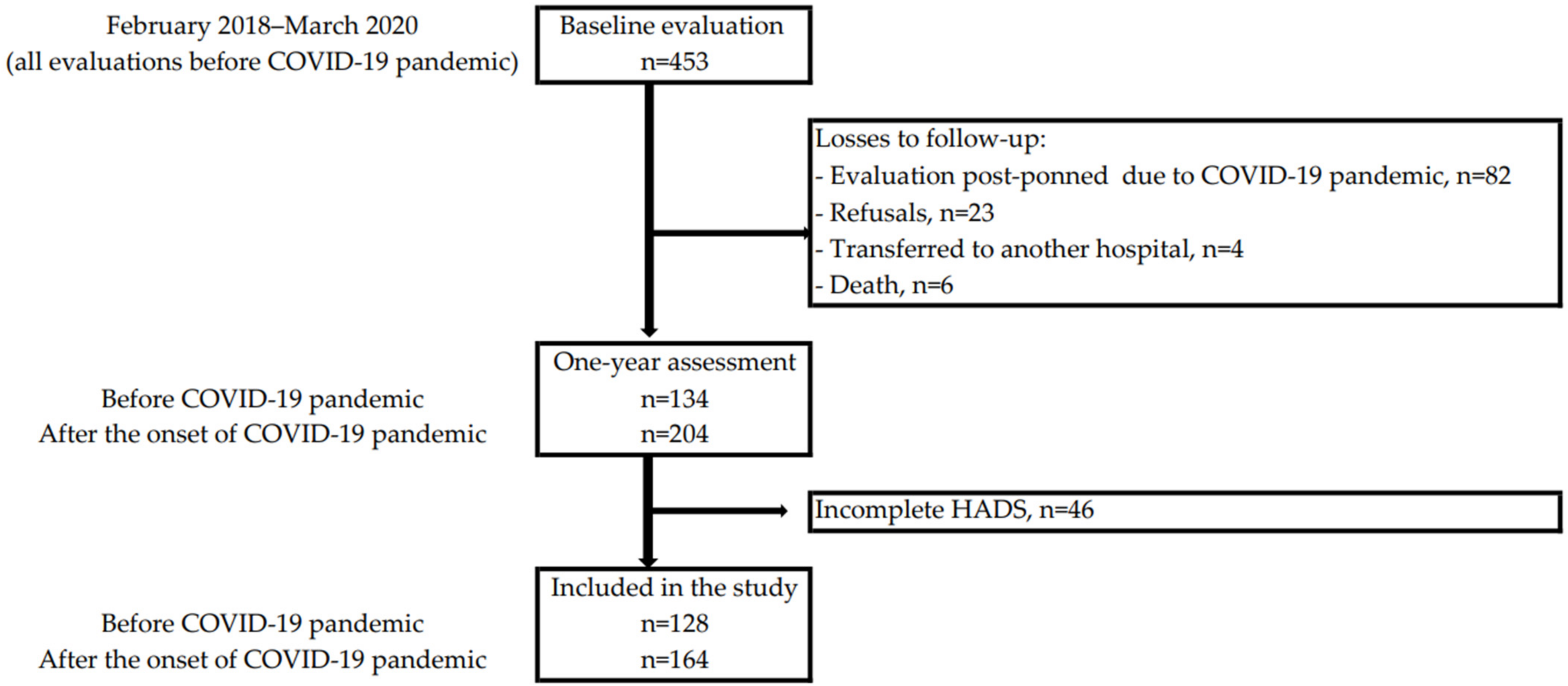
2.1. Setting and Participants
2.2. The Hospital Anxiety and Depression Scale
2.3. Sociodemographic Characteristics of the Participants and Clinical Information
2.4. Data Analysis
2.5. Ethical Approval
3. Results
3.1. Description of Participants
3.2. Variation of Anxiety and Depression over Time
3.3. Factors Associated with Anxiety and Depression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today. Available online: https://gco.iarc.fr/today (accessed on 30 September 2021).
- Ferlay, J.; Laversanne, M.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Tomorrow. Available online: https://gco.iarc.fr/tomorrow (accessed on 30 September 2021).
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Nikšić, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Estève, J.; et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef] [Green Version]
- Antunes, L.; Santos, L.L.; Bento, M.J. Survival from cancer in the north region of Portugal: Results from the first decade of the millennium. Eur. J. Cancer Prev. 2017, 26, S170–S175. [Google Scholar] [CrossRef] [PubMed]
- Nunes, P.; Pimentel, F.L.; Pina, F.; Rolo, F.; Nunes, P.; KeyPoint, C.C. Registo nacional de cancro da próstata, em Portugal–ReNaCaP. Acta Urol. 2010, 3, 39–45. [Google Scholar]
- Braga, R.; Costa, A.R.; Pina, F.; Moura-Ferreira, P.; Lunet, N. Prostate cancer screening in Portugal: Prevalence and perception of potential benefits and adverse effects. Eur. J. Cancer Prev. 2020, 29, 248–251. [Google Scholar] [CrossRef]
- Gaspar, S.S.; Fernandes, M.; Castro, A.; Oliveira, T.; Dias, J.S.; Dos Reis, J.P. Active surveillance protocol in prostate cancer in Portugal. Actas Urológicas Españolas 2022, 46, 329–339. [Google Scholar]
- Pereira-Lourenço, M.; e Brito, D.V.; Peralta, J.P.; Godinho, R.; Conceição, P.; Reis, M.; Rabaça, C.; Sismeiro, A. Influence of sociodemographic factors on treatment’s choice for localized prostate cancer in Portugal. Arch. Ital. Urol. Androl. 2020, 92, 45–49. [Google Scholar] [CrossRef]
- Batty, G.D.; Russ, T.C.; Stamatakis, E.; Kivimäki, M. Psychological distress in relation to site specific cancer mortality: Pooling of unpublished data from 16 prospective cohort studies. BMJ 2017, 356, j108. [Google Scholar] [CrossRef] [Green Version]
- De Sousa, A.; Sonavane, S.; Mehta, J. Psychological aspects of prostate cancer: A clinical review. Prostate Cancer Prostatic Dis. 2012, 15, 120–127. [Google Scholar] [CrossRef] [Green Version]
- Mundle, R.; Afenya, E.; Agarwal, N. The effectiveness of psychological intervention for depression, anxiety, and distress in prostate cancer: A systematic review of literature. Prostate Cancer Prostatic Dis. 2021, 24, 674–687. [Google Scholar] [CrossRef]
- Prasad, S.M.; Eggener, S.E.; Lipsitz, S.R.; Irwin, M.R.; Ganz, P.A.; Hu, J.C. Effect of depression on diagnosis, treatment, and mortality of men with clinically localized prostate cancer. J. Clin. Oncol. 2014, 32, 2471–2478. [Google Scholar] [CrossRef] [Green Version]
- Watts, S.; Leydon, G.; Birch, B.; Prescott, P.; Lai, L.; Eardley, S.; Lewith, G. Depression and anxiety in prostate cancer: A systematic review and meta-analysis of prevalence rates. BMJ Open 2014, 4, 3901. [Google Scholar] [CrossRef]
- Yiannopoulou, K.G.; Anastasiou, A.I.; Kontoangelos, K.; Papageorgiou, C.; Anastasiou, I.P. Cognitive and Psychological Impacts of Different Treatment Options for Prostate Cancer: A Critical Analysis. Curr. Urol. 2020, 14, 169–177. [Google Scholar] [CrossRef]
- Brunckhorst, O.; Hashemi, S.; Martin, A.; George, G.; van Hemelrijck, M.; Dasgupta, P.; Stewart, R.; Ahmed, K. Depression, anxiety, and suicidality in patients with prostate cancer: A systematic review and meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2020, 24, 281–289. [Google Scholar] [CrossRef]
- Bourke, L.; Boorjian, S.A.; Briganti, A.; Klotz, L.; Mucci, L.; Resnick, M.J.; Rosario, D.J.; Skolarus, T.A.; Penson, D.F. Survivorship and Improving Quality of Life in Men with Prostate Cancer. Eur. Urol. 2015, 68, 374–383. [Google Scholar] [CrossRef] [Green Version]
- Farrington, A.P.; Wilson, G.; Limbrick, H.; Swainston, K. The lived experience of adjustment to prostate cancer. Psychol. Men Masc. 2020, 21, 369–379. [Google Scholar] [CrossRef] [Green Version]
- Punnen, S.; Cowan, J.E.; Dunn, L.B.; Shumay, D.M.; Carroll, P.R.; Cooperberg, M.R. A longitudinal study of anxiety, depression and distress as predictors of sexual and urinary quality of life in men with prostate cancer. BJU Int. 2013, 112, E67–E75. [Google Scholar] [CrossRef] [Green Version]
- Sharpley, C.F.; Christie, D.R.H.; Bitsika, V. Variability in Anxiety and Depression over Time Following Diagnosis in Patients with Prostate Cancer. J. Psychosoc. Oncol. 2010, 28, 644–665. [Google Scholar] [CrossRef]
- Bracke, P.; Delaruelle, K.; Dereuddre, R.; van de Velde, S. Depression in women and men, cumulative disadvantage and gender inequality in 29 European countries. Soc. Sci. Med. 2020, 267, 113354. [Google Scholar] [CrossRef]
- Frasquilho, D.; de Matos, M.G.; Marques, A.; Gaspar, T.; Caldas-de-Almeida, J.M. Distress and unemployment: The related economic and noneconomic factors in a sample of unemployed adults. Int. J. Public Health 2016, 61, 821–828. [Google Scholar] [CrossRef]
- Fervaha, G.; Izard, J.P.; Tripp, D.A.; Rajan, S.; Leong, D.P.; Siemens, D.R. Depression and prostate cancer: A focused review for the clinician. Urol. Oncol. Semin. Orig. Investig. 2019, 37, 282–288. [Google Scholar] [CrossRef]
- Araújo, N.; Costa, A.; Lopes-Conceição, L.; Ferreira, A.; Carneiro, F.; Oliveira, J.; Braga, I.; Morais, S.; Pacheco-Figueiredo, L.; Ruano, L.; et al. Androgen-deprivation therapy and cognitive decline in the NEON-PC prospective study during the COVID-19 pandemic. ESMO Open 2022, 7, 100448. [Google Scholar] [CrossRef]
- Khan, K.S.; Mamun, M.A.; Griffiths, M.D.; Ullah, I. The Mental Health Impact of the COVID-19 Pandemic across Different Cohorts. Int. J. Ment. Health Addict. 2022, 20, 380–386. [Google Scholar] [CrossRef]
- Wang, Y.; Duan, Z.; Ma, Z.; Mao, Y.; Li, X.; Wilson, A.; Qin, H.; Ou, J.; Peng, K.; Zhou, F.; et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl. Psychiatry 2020, 10, 263. [Google Scholar] [CrossRef]
- Bandinelli, L.; Ornell, F.; von Diemen, L.; Kessler, F.H.P. The Sum of Fears in Cancer Patients inside the Context of the COVID-19. Front. Psychiatry 2021, 12, 557834. [Google Scholar] [CrossRef]
- Araujo, N.; Morais, S.; Costa, A.R.; Braga, R.; Carneiro, A.F.; Cruz, V.T.; Ruano, L.; Oliveira, J.; Figueiredo, L.P.; Pereira, S.; et al. Cognitive decline in patients with prostate cancer: Study protocol of a prospective cohort, NEON-PC. BMJ Open 2021, 11, e043844. [Google Scholar] [CrossRef]
- Vodermaier, A.; Linden, W.; Siu, C. Screening for emotional distress in cancer patients: A systematic review of assessment instruments. J. Natl. Cancer Inst. 2009, 101, 1464–1488. [Google Scholar] [CrossRef] [PubMed]
- Pais-Ribeiro, J.; Silva, I.; Ferreira, T.; Martins, A.; Meneses, R.; Baltar, M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol. Health Med. 2007, 12, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Instituto Nacional de Estatística. Deliberação 1494/2014, de 29 de Julho. 2014. Available online: https://dre.pt/application/file/55029096 (accessed on 21 October 2021).
- National Institute on Alcohol Abuse and Alcoholism. The Physicians’ Guide to Helping Patients with Alcohol Problems; US Department of Health and Human Services, Public Health Service: Washington, DC, USA, 1995. [Google Scholar]
- Direção Geral da Saúde. Norma 030/2012: Deteção Precoce e Intervenção Breve no Consumo Excessivo de Álcool. 2014. Available online: https://www.google.com.hk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwidi5mEvon5AhXdk1YBHaLnAw8QFnoECA0QAQ&url=https%3A%2F%2Fwww.dgs.pt%2Fdirectrizes-da-dgs%2Fnormas-e-circulares-normativas%2Fnorma-n-0302012-de-28122012-png.aspx&usg=AOvVaw1JLe0CnoCWlHy-4FBgwpGF (accessed on 21 October 2021).
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Amin, M.B. American Joint Committee on Cancer. American Cancer Society. In AJCC Cancer Staging Manual; Amin, M.B., Edge, S.B., Greene, F.L., Byrd, D.R., Brookland, R.K., Washington, M.K., Gershenwald, J.E., Compton, C.C., Hess, K.R., Sullivan, D.C., et al., Eds.; Springer: Chicago IL, USA, 2017; p. 1024. [Google Scholar]
- Baxter, A.J.; Scott, K.M.; Vos, T.; Whiteford, H.A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 2013, 43, 897–910. [Google Scholar] [CrossRef]
- Esser, P.; Mehnert-Theuerkauf, A.; Friedrich, M.; Johansen, C.; Brähler, E.; Faller, H.; Härter, M.; Koch, U.; Schulz, H.; Wegscheider, K.; et al. Risk and associated factors of depression and anxiety in men with prostate cancer: Results from a German multicenter study. Psychooncology 2020, 29, 1604–1612. [Google Scholar] [CrossRef]
- Yu, R.; Li, H. Longitudinal Assessment of Prevalence and Risk Factors of Anxiety and Depression among Prostate Cancer Survivors Post-Resection. Psychiatr. Q. 2021, 92, 995–1009. [Google Scholar] [CrossRef]
- Hansen, H.; Beyer, N.; Frølich, A.; Godtfredsen, N.; Bieler, T. Inter-Day Test-Retest Reproducibility of the CAT, CCQ, HADS and EQ-5D-3L in Patients with Severe and Very Severe COPD. Patient Relat. Outcome Meas. 2021, 12, 117–128. [Google Scholar] [CrossRef]
- Smid, D.E.; Franssen, F.M.; Houben-Wilke, S.; Vanfleteren, L.E.; Janssen, D.J.; Wouters, E.F.; Spruit, M.A. Responsiveness and MCID Estimates for CAT, CCQ, and HADS in Patients with COPD Undergoing Pulmonary Rehabilitation: A Prospective Analysis. J. Am. Med. Dir. Assoc. 2017, 18, 53–58. [Google Scholar] [CrossRef]
- Wynne, S.C.; Patel, S.; Barker, R.E.; Jones, S.E.; Walsh, J.A.; Kon, S.S.; Cairn, J.; Loebinger, M.R.; Wilson, R.; Man, W.D.; et al. Anxiety and depression in bronchiectasis: Response to pulmonary rehabilitation and minimal clinically important difference of the Hospital Anxiety and Depression Scale. Chron. Respir. Dis. 2020, 17, 1479973120933292. [Google Scholar] [CrossRef]
- Brehaut, E.; Neupane, D.; Levis, B.; Wu, Y.; Sun, Y.; Krishnan, A.; He, C.; Bhandari, P.M.; Negeri, Z.; Riehm, K.E.; et al. Depression prevalence using the HADS-D compared to SCID major depression classification: An individual participant data meta-analysis. J. Psychosom. Res. 2020, 139, 110256. [Google Scholar] [CrossRef]
- Mitchell, A.J.; Meader, N.; Symonds, P. Diagnostic validity of the Hospital Anxiety and Depression Scale (HADS) in cancer and palliative settings: A meta-analysis. J. Affect. Disord. 2010, 126, 335–348. [Google Scholar] [CrossRef]
- Sharpley, C.F.; Bitsika, V.; Christie, D.R.H. “The Worst Thing Was”: Prostate Cancer Patients’ Evaluations of Their Diagnosis and Treatment Experiences. Am. J. Men’s Health 2018, 12, 1503–1509. [Google Scholar] [CrossRef] [Green Version]
- Ramalho, M.; Fontes, F.; Ruano, L.; Pereira, S.; Lunet, N. Cognitive impairment in the first year after breast cancer diagnosis: A prospective cohort study. Breast 2017, 32, 173–178. [Google Scholar] [CrossRef] [Green Version]
- Ernst, J.; Zenger, M.; Schmidt, R.; Schwarz, R.; Brähler, E. Medical and psychosocial care needs of cancer patients: A systematic review comparing urban and rural provisions. Dtsch. Med. Wochenschr. 2010, 135, 1531–1537. [Google Scholar] [CrossRef]
- Ravi, P.; Karakiewicz, P.I.; Roghmann, F.; Gandaglia, G.; Choueiri, T.K.; Menon, M.; McKay, R.R.; Nguyen, P.L.; Sammon, J.D.; Sukumar, S.; et al. Mental health outcomes in elderly men with prostate cancer. Urol. Oncol. Semin. Orig. Investig. 2014, 32, 1333–1340. [Google Scholar] [CrossRef]
- Tian, J.; Chen, Z.-C.; Wu, B.; Meng, X. Comparison of quality of life between urban and rural gastric cancer patients and analysis of influencing factors. World J. Gastroenterol. 2004, 10, 2940–2943. [Google Scholar] [CrossRef] [Green Version]
- Andrykowski, M.A.; Burris, J.L. Use of formal and informal mental health resources by cancer survivors: Differences between rural and nonrural survivors and a preliminary test of the theory of planned behavior. Psycho-Oncology 2010, 19, 1148–1155. [Google Scholar] [CrossRef] [Green Version]
- Beraldi, A.; Kukk, E.; Nest, A.; Schubert-Fritschle, G.; Engel, J.; Heußner, P.; Herschbach, P. Use of cancer-specific mental health resources-is there an urban-rural divide? Support. Care Cancer 2015, 23, 1285–1294. [Google Scholar] [CrossRef]
- Girgis, A.; Boyes, A.; Sanson-Fisher, R.W.; Burrows, S. Perceived needs of women diagnosed with breast cancer: Rural versus urban location. Aust. N. Z. J. Public Health 2000, 24, 166–173. [Google Scholar] [CrossRef]
- Tzelepis, F.; Paul, C.L.; Sanson-Fisher, R.W.; Campbell, H.S.; Bradstock, K.; Carey, M.L.; Williamson, A. Unmet supportive care needs of haematological cancer survivors: Rural versus urban residents. Ann. Hematol. 2018, 97, 1283–1292. [Google Scholar] [CrossRef]
- Karanikolos, M.; Ellis, L.; Coleman, M.P.; McKee, M. Health systems performance and cancer outcomes. J. Natl. Cancer Inst. Monogr. 2013, 2013, 7–12. [Google Scholar] [CrossRef]
- Blanchard, C.M.; Stein, K.; Courneya, K.S. Body Mass Index, Physical Activity, and Health-Related Quality of Life in Cancer Survivors. Med. Sci. Sports Exerc. 2010, 42, 665–671. [Google Scholar]
- Ramp, D.; Mols, F.; Ezendam, N.; Beijer, S.; Bours, M.; Winkels, R.; de Vries, J.; Seidell, J.C.; Kampman, E.; Hoedjes, M. Psychological distress and lower health-related quality of life are associated with need for dietary support among colorectal cancer survivors with overweight or obesity. Supportive Care Cancer 2021, 29, 7659–7668. [Google Scholar] [CrossRef]
- Faul, L.A.; Jim, H.S.; Minton, S.; Fishman, M.; Tanvetyanon, T.; Jacobsen, P.B. Relationship of exercise to quality of life in cancer patients beginning chemotherapy. J. Pain Symptom Manag. 2011, 41, 859–869. [Google Scholar] [CrossRef]
- Gallagher, S.; Bennett, K.M.; Roper, L. Loneliness and depression in patients with cancer during COVID-19. J. Psychosoc. Oncol. 2021, 39, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Henriques, A.; Talih, M.; Pastor-Valero, M.; Fraga, S.; Dias, I.; Matijasevich, A.; Barros, H. A multidimensional perspective of the relation between social isolation and depression among Portuguese older adults. Health Soc. Care Community 2021, 1–10. [Google Scholar] [CrossRef]
- De Sousa, R.D.; Rodrigues, A.M.; Gregório, M.J.; Branco, J.D.C.; Gouveia, M.J.; Canhão, H.; Dias, S.S. Anxiety and depression in the portuguese older adults: Prevalence and associated factors. Front. Med. 2017, 4, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Krebber, A.M.H.; Buffart, L.M.; Kleijn, G.; Riepma, I.C.; de Bree, R.; Leemans, C.R.; Becker, A.; Brug, J.; van Straten, A.; Cuijpers, P.; et al. Prevalence of depression in cancer patients: A meta-analysis of diagnostic interviews and self-report instruments. Psycho-Oncology 2014, 23, 121–130. [Google Scholar] [CrossRef]
- Hinz, A.; Krauss, O.; Stolzenburg, J.-U.; Schwalenberg, T.; Michalski, D.; Schwarz, R. Anxiety and depression in patients with prostate cancer and other urogenital cancer: A longitudinal study. Urol. Oncol. Semin. Orig. Investig. 2009, 27, 367–372. [Google Scholar] [CrossRef]
- Korfage, I.J.; Essink-Bot, M.L.; Janssens, A.C.J.W.; Schröder, F.H.; de Koning, H.J. Anxiety and depression after prostate cancer diagnosis and treatment: 5-year follow-up. Br. J. Cancer 2006, 94, 1093–1098. [Google Scholar] [CrossRef]



| Timing of the One-Year Evaluation in Relation to the COVID-19 Pandemic Onset | ||||
|---|---|---|---|---|
| All | Before | After | ||
| n (%) | n (%) | n (%) | p | |
| Age (years) | ||||
| <65 | 85 (29.1) | 32 (25.0) | 53 (32.3) | 0.172 |
| ≥65 | 207 (70.9) | 96 (75.0) | 111 (67.7) | |
| Education (years) | 0.051 | |||
| 1–4 | 145 (49.7) | 74 (57.8) | 71 (43.3) | |
| 5–9 | 65 (22.3) | 20 (15.6) | 45 (27.4) | |
| 10–12 | 37 (12.7) | 15 (11.7) | 22 (13.4) | |
| >12 | 45 (15.4) | 19 (14.8) | 26 (15.9) | |
| Living alone | 0.678 | |||
| No | 263 (92.0) | 114 (91.2) | 149 (92.5) | |
| Yes | 23 (8.0) | 11 (8.8) | 12 (7.5) | |
| Area of residence a | 0.961 | |||
| Urban | 241 (89.3) | 108 (89.3) | 133 (89.3) | |
| Rural | 29 (10.7) | 13 (10.7) | 16 (10.7) | |
| Employment | 0.475 | |||
| Sick leave/unemployed | 13 (4.6) | 6 (4.8) | 7 (4.4) | |
| Employed | 72 (25.4) | 27 (21.8) | 45 (28.1) | |
| Retired | 199 (70.1) | 91 (73.4) | 108 (67.5) | |
| Smoking status | 0.217 | |||
| Never smoker | 127 (44.3) | 53 (42.4) | 74 (45.7) | |
| Ex-smoker | 137 (47.7) | 58 (46.4) | 79 (48.8) | |
| Current smoker | 23 (8.0) | 14 (11.2) | 9 (5.6) | |
| Alcohol consumption b | 0.558 | |||
| ≤10 or 20 g/day | 153 (56.3) | 64 (54.2) | 89 (57.8) | |
| >10 or 20 g/day | 119 (43.8) | 54 (45.8) | 65 (42.2) | |
| Vegetables consumption | 0.063 | |||
| <5 portions/day | 198 (69.0) | 79 (63.2) | 119 (73.5) | |
| ≥5 portions/day | 89 (31.0) | 46 (36.8) | 43 (26.5) | |
| Physical activity c | 0.891 | |||
| <150 min/week | 161 (55.1) | 70 (54.7) | 91 (55.5) | |
| ≥150 min/week | 131 (44.9) | 58 (45.3) | 73 (44.5) | |
| Body mass index (kg/m2) d | 0.297 | |||
| 18.5–24.9 | 65 (26.1) | 36 (30.5) | 29 (22.1) | |
| 25.0–29.9 | 133 (53.4) | 58 (49.2) | 75 (57.3) | |
| ≥30 | 51 (20.5) | 24 (20.3) | 27 (20.6) | |
| Comorbidities | 0.357 | |||
| None | 58 (19.9) | 30 (23.4) | 28 (17.1) | |
| 1–2 | 185 (63.4) | 76 (59.4) | 109 (66.5) | |
| ≥3 | 49 (16.8) | 22 (17.2) | 27 (16.5) | |
| Cancer stage | 0.060 | |||
| Any T, N0, M0 | 250 (85.6) | 104 (81.3) | 146 (89.0) | |
| Any T, N1 and/or M1 | 42 (14.4) | 24 (18.8) | 18 (11.0) | |
| Treatment | 0.003 | |||
| Active surveillance | 15 (5.1) | 1 (0.8) | 14 (8.5) | |
| Curative intent | 251 (86.0) | 111 (86.7) | 140 (85.4) | |
| Palliative intent | 26 (8.9) | 16 (12.5) | 10 (6.1) | |
| Anxiety | Depression | |
|---|---|---|
| % (95% CI) | % (95% CI) | |
| All (n = 292) | ||
| Prevalence at baseline | 7.8 (5.0–11.5) | 3.1 (1.4–5.7) |
| Prevalence at one year | 8.5 (5.6–12.3) | 6.8 (4.2–10.3) |
| One-year cumulative incidence a | 7.0 (4.3–10.7) | 5.3 (3.0–8.5) |
| Stable anxiety/depression b | 2.0 (0.7–4.4) | 1.7 (0.6–4.0) |
| Recovery from anxiety/depression c | 3.8 (1.9–6.6) | 0.3 (0.0–1.9) |
| Before COVID-19 pandemic onset (n = 128) | ||
| Prevalence at baseline | 6.2 (2.7–11.9) | 1.6 (0.2–5.5) |
| Prevalence at one year | 7.8 (3.8–13.9) | 8.6 (4.4–14.8) |
| One-year cumulative incidence a | 7.5 (3.5–13.8) | 7.1 (3.3–13.1) |
| Stable anxiety/depression b | 0.8 (0.0–4.3) | 1.6 (0.2–5.5) d |
| Recovery from anxiety/depression c | 4.7 (1.7–9.9) | 0 (0–2.8) d |
| After COVID-19 pandemic onset (n = 164) | ||
| Prevalence at baseline | 9.1 (5.2–14.6) | 4.3 (1.7–8.6) |
| Prevalence at one year | 8.5 (4.7–13.9) | 5.5 (2.5–10.2) |
| One-year cumulative incidence a | 6.0 (2.8–11.2) | 3.8 (1.4–8.1) |
| Stable anxiety/depression b | 3.0 (1.0–7.0) | 1.8 (0.4–5.3) |
| Recovery from anxiety/depression c | 3.0 (1.0–7.0) | 0.6 (0.0–3.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duarte, V.; Araújo, N.; Lopes, C.; Costa, A.; Ferreira, A.; Carneiro, F.; Oliveira, J.; Braga, I.; Morais, S.; Pacheco-Figueiredo, L.; et al. Anxiety and Depression in Patients with Prostate Cancer, at Cancer Diagnosis and after a One-Year Follow-Up. Int. J. Environ. Res. Public Health 2022, 19, 9122. https://doi.org/10.3390/ijerph19159122
Duarte V, Araújo N, Lopes C, Costa A, Ferreira A, Carneiro F, Oliveira J, Braga I, Morais S, Pacheco-Figueiredo L, et al. Anxiety and Depression in Patients with Prostate Cancer, at Cancer Diagnosis and after a One-Year Follow-Up. International Journal of Environmental Research and Public Health. 2022; 19(15):9122. https://doi.org/10.3390/ijerph19159122
Chicago/Turabian StyleDuarte, Vítor, Natália Araújo, Catarina Lopes, Adriana Costa, Augusto Ferreira, Filipa Carneiro, Jorge Oliveira, Isaac Braga, Samantha Morais, Luís Pacheco-Figueiredo, and et al. 2022. "Anxiety and Depression in Patients with Prostate Cancer, at Cancer Diagnosis and after a One-Year Follow-Up" International Journal of Environmental Research and Public Health 19, no. 15: 9122. https://doi.org/10.3390/ijerph19159122
APA StyleDuarte, V., Araújo, N., Lopes, C., Costa, A., Ferreira, A., Carneiro, F., Oliveira, J., Braga, I., Morais, S., Pacheco-Figueiredo, L., Ruano, L., Tedim Cruz, V., Pereira, S., & Lunet, N. (2022). Anxiety and Depression in Patients with Prostate Cancer, at Cancer Diagnosis and after a One-Year Follow-Up. International Journal of Environmental Research and Public Health, 19(15), 9122. https://doi.org/10.3390/ijerph19159122








