General versus Brachial Plexus Block Anesthesia in Pain Management after Internal Fixation in Patients with Distal Radius Fracture: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Methods of Anesthesia, Operation, and Pain Assessment
2.3. Statistical Analysis
3. Results
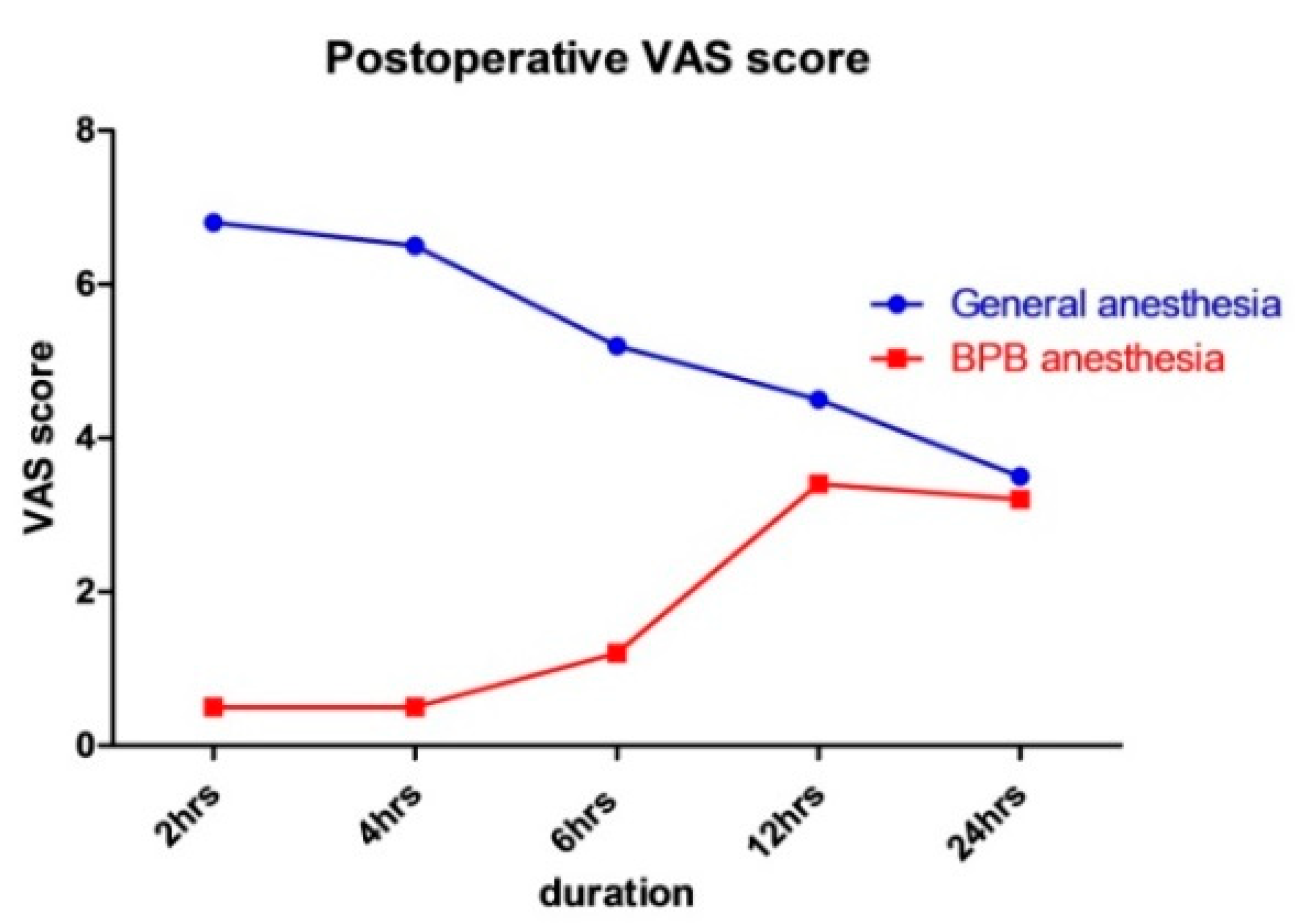
3.1. VAS Scores after Operation
3.2. Sensory Recovery over Time after Surgery with BPB Anesthesia
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Owen, R.; Melton, L.J., 3rd; Johnson, K.; Ilstrup, D.; Riggs, B. Incidence of Colles’ fracture in a North American community. Am. J. Public Health 1982, 72, 605–607. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, B.D.; Ryan, H.; O’Sullivan, O.; Iohom, G. Ultrasound-guided axillary brachial plexus block with 20 milliliters local anesthetic mixture versus general anesthesia for upper limb trauma surgery: An observer-blinded, prospective, randomized, controlled trial. Anesth. Analg. 2009, 109, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Protopsaltis, T.S.; Ruch, D.S. Volar approach to distal radius fractures. J. Hand Surg. 2008, 33, 958–965. [Google Scholar] [CrossRef]
- Orbay, J.L.; Fernandez, D.L. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J. Hand Surg. 2004, 29, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.S.; Strodtbeck, W.M.; Richman, J.M.; Wu, C.L. A comparison of regional versus general anesthesia for ambulatory anesthesia: A meta-analysis of randomized controlled trials. Anesth. Analg. 2005, 101, 1634–1642. [Google Scholar] [CrossRef]
- Shin, Y.D.; Han, J.S.J.A.; Medicine, P. The effect of sono-guided brachial plexus block on postoperative pain control for arthroscopic shoulder surgery: Comparison with general anesthesia. Anesth. Pain Med. 2010, 5, 183–186. [Google Scholar]
- Lee, M.-G.; Kim, H.-S.; Lee, D.-C.; Jung, W.-S.; Chang, Y.-J. A comparison of general anesthesia versus axillary brachial plexus block for hand and wrist surgery in the view of patient satisfaction. Anesth. Pain Med. 2014, 9, 19–23. [Google Scholar]
- Cho, H.; Kwon, H.; Song, S.; Yoo, J.; Kim, M.; Park, S.; Chung, J.; Kim, S.; Park, S.; Ok, S. Quality of postoperative recovery after upper-arm vascular surgery for hemodialysis in patients with end-stage renal disease: A prospective comparison of cervical epidural anesthesia vs general anesthesia. Medicine 2020, 99, e18773. [Google Scholar] [CrossRef]
- Yoo, J.H.; Ryoo, J.H.; You, G.W.J.S.M.S. A Comparison of Combined Superficial Cervical Plexus Block and Interscalene Brachial Plexus Block with General Anesthesia for Clavicle Surgery: Pilot Trial. Soonchunhyang Med. Sci. 2019, 25, 46–52. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Galos, D.K.; Taormina, D.P.; Crespo, A.; Ding, D.Y.; Sapienza, A.; Jain, S.; Tejwani, N.C. Does brachial plexus blockade result in improved pain scores after distal radius fracture fixation? A randomized trial. Clin. Orthop. Relat. Res. 2016, 474, 1247–1254. [Google Scholar] [CrossRef] [Green Version]
- Handoll, H.H.; Madhok, R.; Dodds, C. Anaesthesia for treating distal radial fracture in adults. Cochrane Database Syst. Rev. 2002, 3, CD003320. [Google Scholar] [CrossRef]
- Huang, Y.C.; Chen, C.Y.; Lin, K.C.; Yang, S.W.; Tarng, Y.W.; Chang, W.N.J.O. Comparison of wide-awake local anesthesia no tourniquet with general anesthesia with tourniquet for volar plating of distal radius fracture. Orthopedics 2018, 42, e93–e98. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H. Acute pain control and accelerated postoperative surgical recovery. Surg. Clin. N. Am. 1999, 79, 431–443. [Google Scholar] [CrossRef]
- Katz, J.; Jackson, M.; Kavanagh, B.P.; Sandler, A.N. Acute pain after thoracic surgery predicts long-term post-thoracotomy pain. Clin. J. Pain 1996, 12, 50–55. [Google Scholar] [CrossRef] [Green Version]
- Holmberg, A.; Hassellund, S.S.; Draegni, T.; Nordby, A.; Ottesen, F.S.; Gulestol, A.; Raeder, J. Analgesic effect of intravenous dexamethasone after volar plate surgery for distal radius fracture with brachial plexus block anaesthesia: A prospective, double-blind randomised clinical trial. Anaesthesia 2020, 75, 1448–1460. [Google Scholar] [CrossRef] [PubMed]
- Fredrickson, M.J.; Ball, C.M.; Dalgleish, A.J.J.R.A.; Medicine, P. A prospective randomized comparison of ultrasound guidance versus neurostimulation for interscalene catheter placement. Reg. Anesth. Pain Med. 2009, 34, 590–594. [Google Scholar] [CrossRef]
- Maurer, K.; Ekatodramis, G.; Rentsch, K.; Borgeat, A.; Analgesia, J.A. Interscalene and infraclavicular block for bilateral distal radius fracture. Anesth. Analg. 2002, 94, 450–452. [Google Scholar] [CrossRef]
- Bhatia, A.; Lai, J.; Chan, V.W.; Brull, R.; Analgesia, J.A. Pneumothorax as a complication of the ultrasound-guided supraclavicular approach for brachial plexus block. Anesth. Analg. 2010, 111, 817–819. [Google Scholar] [CrossRef]
- Buise, M.P.; Bouwman, R.A.; van der Gaag, A.; Piot, V.; Korsten, H.J. Phrenic nerve palsy following interscalene brachial plexus block; a long lasting serious complication. Acta Anaesthesiol. Belg. 2015, 66, 91–94. [Google Scholar]
- De Tran, Q.H.; Clemente, A.; Doan, J.; Finlayson, R.J. Brachial plexus blocks: A review of approaches and techniques. Can. J. Anesth./J. Can. D’anesthésie 2007, 54, 662–674. [Google Scholar] [CrossRef] [PubMed]
- de Mos, M.; De Bruijn, A.; Huygen, F.; Dieleman, J.; Stricker, B.C.; Sturkenboom, M.J.P. The incidence of complex regional pain syndrome: A population-based study. Pain 2007, 129, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Zollinger, P.E.; Tuinebreijer, W.E.; Kreis, R.W.; Breederveld, R.S. Effect of vitamin C on frequency of reflex sympathetic dystrophy in wrist fractures: A randomised trial. Lancet 1999, 354, 2025–2028. [Google Scholar] [CrossRef]
- Roumen, R.; Hesp, W.; Bruggink, E.D. Unstable Colles’ fractures in elderly patients. A randomised trial of external fixation for redisplacement. J. Bone Jt. Surgery Br. Vol. 1991, 73, 307–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dijkstra, P.U.; Groothoff, J.W.; ten Duis, H.J.; Geertzen, J.H. Incidence of complex regional pain syndrome type I after fractures of the distal radius. Eur. J. Pain 2003, 7, 457–462. [Google Scholar] [CrossRef] [Green Version]
- Gradl, G.; Gradl, G.; Wendt, M.; Mittlmeier, T.; Kundt, G.; Jupiter, J.B. Non-bridging external fixation employing multiplanar K-wires versus volar locked plating for dorsally displaced fractures of the distal radius. Arch. Orthop. Trauma Surg. 2013, 133, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Fallatah, S.M. Successful management of complex regional pain syndrome type 1 using single injection interscalene brachial plexus block. Saudi J. Anaesth. 2014, 8, 559. [Google Scholar] [CrossRef]
- Wang, L.-K.; Chen, H.-P.; Chang, P.-J.; Kang, F.-C.; Tsai, Y.-C. Axillary brachial plexus block with patient controlled analgesia for complex regional pain syndrome type I: A case report. Reg. Anesth. Pain Med. 2001, 26, 68–71. [Google Scholar]
| General Anesthesia (Group A) | BPB Anesthesia (Group B) | p-Value | ||
|---|---|---|---|---|
| Age (mean) | 71.2 ± 14.5 | 69.5 ± 15.8 | 0.687 | |
| Injured wrist | Right | 14 | 22 | 0.061 |
| Left | 22 | 14 | ||
| Fracture type | A | 1 | 3 | <0.001 |
| B | 0 | 0 | ||
| C1 | 26 | 19 | ||
| C2 | 8 | 13 | ||
| C3 | 1 | 1 | ||
| Operation time (mean, minute) | 31.9 ± 5.2 | 34.0 ± 2.7 | <0.001 |
| Time after Surgery | General Anesthesia (Group A) | BPB Anesthesia (Group B) | p-Value |
|---|---|---|---|
| 2 h | 6.8 ± 2.5 | 0.5 ± 2.3 | <0.001 |
| 4 h | 6.5 ± 2.4 | 0.5 ± 2.4 | <0.001 |
| 6 h | 5.2 ± 2.4 | 1.5 ± 2.4 | <0.001 |
| 12 h | 4.5 ± 2.5 | 3.4 ± 2.7 | <0.001 |
| 24 h | 3.5 ± 2.5 | 3.2 ± 2.2 | 0.142 |
| Average Time (h) | |
|---|---|
| Senses begin to return | 10.5 ± 2.8 |
| Pain begins | 12.4 ± 3.9 |
| Complete recovery of senses | 19.2 ± 4.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nho, J.-H.; Jang, B.-W.; An, C.Y.; Yoo, J.H.; Song, S.; Cho, H.B.; Kim, S.H.; Kim, S.I.; Jung, K.J.; Kim, B. General versus Brachial Plexus Block Anesthesia in Pain Management after Internal Fixation in Patients with Distal Radius Fracture: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 9155. https://doi.org/10.3390/ijerph19159155
Nho J-H, Jang B-W, An CY, Yoo JH, Song S, Cho HB, Kim SH, Kim SI, Jung KJ, Kim B. General versus Brachial Plexus Block Anesthesia in Pain Management after Internal Fixation in Patients with Distal Radius Fracture: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(15):9155. https://doi.org/10.3390/ijerph19159155
Chicago/Turabian StyleNho, Jae-Hwi, Byung-Woong Jang, Chi Young An, Jae Hwa Yoo, Sanghoon Song, Ho Bum Cho, Sang Ho Kim, Soon Im Kim, Ki Jin Jung, and Byungsung Kim. 2022. "General versus Brachial Plexus Block Anesthesia in Pain Management after Internal Fixation in Patients with Distal Radius Fracture: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 15: 9155. https://doi.org/10.3390/ijerph19159155
APA StyleNho, J.-H., Jang, B.-W., An, C. Y., Yoo, J. H., Song, S., Cho, H. B., Kim, S. H., Kim, S. I., Jung, K. J., & Kim, B. (2022). General versus Brachial Plexus Block Anesthesia in Pain Management after Internal Fixation in Patients with Distal Radius Fracture: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(15), 9155. https://doi.org/10.3390/ijerph19159155






