Nine-Year Trends in Atrial Fibrillation Prevalence among Romanian Adult Hypertensives: A Post-Hoc Analysis of SEPHAR II-IV Surveys
Abstract
:1. Introduction
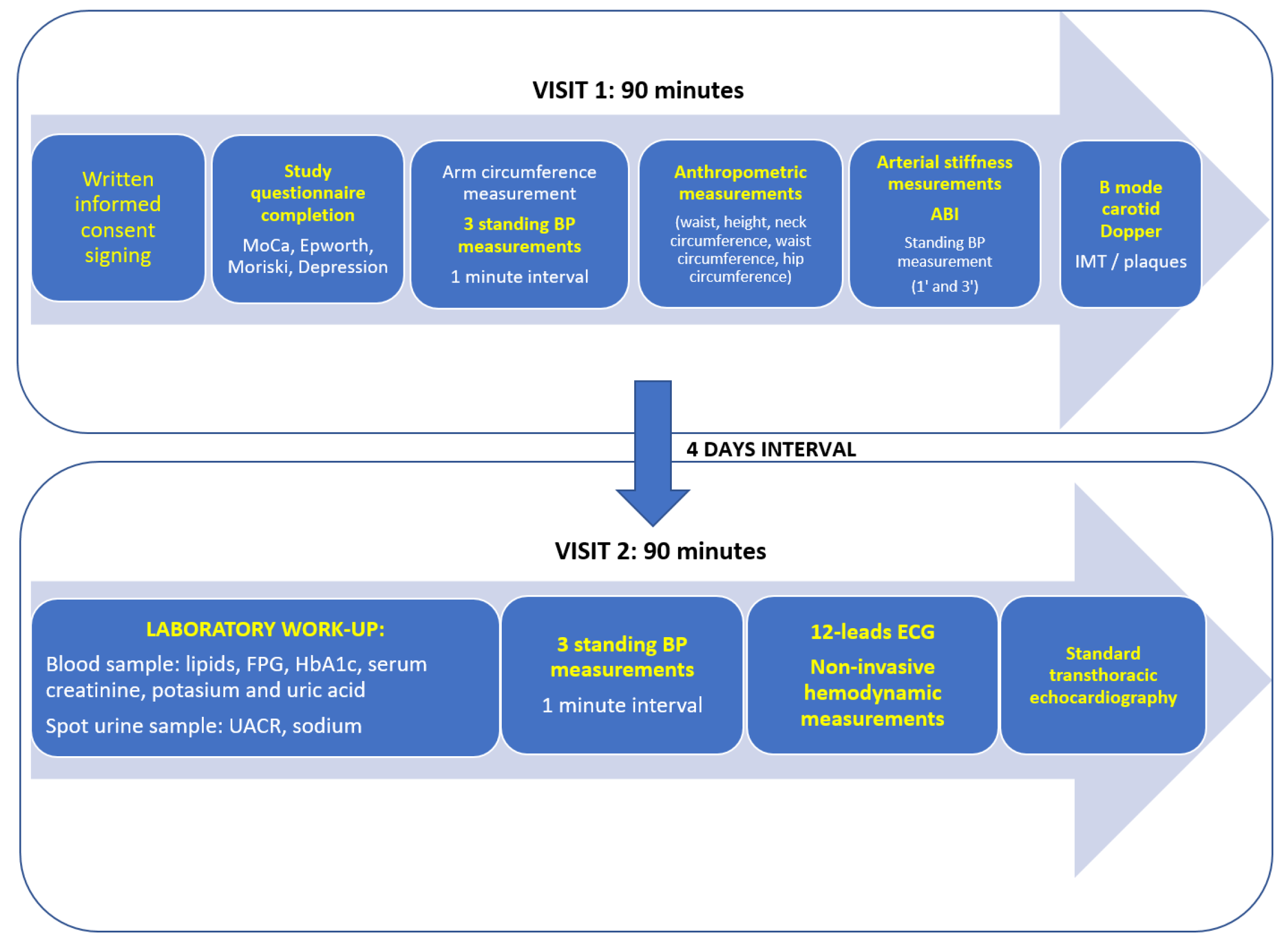
2. Materials and Methods
2.1. Sample Selection and Data Collection in SEPHAR Surveys
2.2. Statistical Analysis
3. Results
3.1. AF Prevalence in Romanian Hypertensive Adults and Future Projections
3.1.1. Overall AF Prevalence in SEPHAR Survey Global Population
3.1.2. Trends of AF Prevalence from 2012 (SEPHAR II) to 2021 (SEPHAR IV)
3.2. Global Epidemiology and Trends of AF-Inducing Risk Factor Epidemiology in SEPHAR Surveys
3.3. Rates of Oral Anticoagulation (OAC) in AF Patients in SEPHAR III and IV Surveys
4. Discussion
4.1. AF Prevalence in Romania Appears to Be Higher than the Average European Prevalence and Has Been Increasing during the Last Decade
4.2. Oral Anticoagulants Are Severely Underutilized Even in High Cardioembolic Risk Subjects
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benjamin, E.J.; Levy, D.; Vaziri, S.M.; D’Agostino, R.B.; Belanger, A.J.; Wolf, P.A. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994, 271, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus Warfarin in Nonvalvular Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.V.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Ave-zum, A.; et al. Apixaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopes, R.D.; Heizer, G.; Aronson, R.; Vora, A.N.; Massaro, T.; Mehran, R.; Goodman, S.G.; Windecker, S.; Darius, H.; Li, J.; et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N. Engl. J. Med. 2019, 380, 1509–1524. [Google Scholar] [CrossRef] [Green Version]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef] [Green Version]
- Esteve-Pastor, M.A.; Rivera-Caravaca, J.M.; Lip, G.Y.H. Hypertension and Atrial Fibrillation: Balancing Stroke and Bleeding Risks. Am. J. Hypertens. 2017, 30, 1063–1065. [Google Scholar] [CrossRef] [Green Version]
- Shantsila, A.; Shantsila, E.; Lip, G.Y.H. Blood pressure targets in atrial fibrillation. Eur. Heart J. 2020, 41, 2860–2862. [Google Scholar] [CrossRef]
- Potpara, T.S.; Dan, G.-A.; Trendafilova, E.; Goda, A.; Kusljugic, Z.; Manola, S.; Music, L.; Musetescu, R.; Badila, E.; Mitic, G.; et al. Stroke prevention in atrial fibrillation and ‘real world’ adherence to guidelines in the Balkan Region: The BALKAN-AF Survey. Sci. Rep. 2016, 6, 20432. [Google Scholar] [CrossRef] [Green Version]
- Dorobanţu, M.; Darabont, R.; Ghiorghe, S.; Georgescu, C.A.; Macarie, C.; Mitu, F.; Lighezan, D.; Musetescu, R.; Pop, C.; Ardeleanu, E.; et al. Hypertension prevalence and control in Romania at a seven-year interval. Comparison of SEPHAR I and II surveys. J. Hypertens. 2014, 32, 39–47. [Google Scholar] [CrossRef]
- Dorobantu, M.; Tautu, O.-F.; Dimulescu, D.; Sinescu, C.; Gusbeth-Tatomir, P.; Arsenescu-Georgescu, C.; Mitu, F.; Lighezan, D.; Pop, C.; Babes, K.; et al. Perspectives on hypertension’s prevalence, treatment and control in a high cardiovascular risk East European country: Data from the SEPHAR III survey. J. Hypertens. 2018, 36, 690–700. [Google Scholar] [CrossRef]
- Unger, T.; Borghi, C.; Charchar, F.; Khan, N.A.; Poulter, N.R.; Prabhakaran, D.; Ramirez, A.; Schlaich, M.; Stergiou, G.S.; Tomaszewski, M.; et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020, 75, 1334–1357. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. Corrigendum to: 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 4194. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019 update: A report from the American heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef]
- Kornej, J.; Börschel, C.S.; Benjamin, E.J.; Schnabel, R.B. Epidemiology of Atrial Fibrillation in the 21st Century. Circ. Res. 2020, 127, 4–20. [Google Scholar] [CrossRef]
- Zoni-Berisso, M.; Lercari, F.; Carazza, T.; Domenicucci, S. Epidemiology of atrial fibrillation: European perspective. Clin. Epidemiol. 2014, 6, 213–220. [Google Scholar] [CrossRef] [Green Version]
- Verdecchia, P.; Angeli, F.; Reboldi, G. Hypertension and Atrial Fibrillation. Circ. Res. 2018, 122, 352–368. [Google Scholar] [CrossRef]
- Krijthe, B.P.; Kunst, A.; Benjamin, E.; Lip, G.Y.; Franco, O.; Hofman, A.; Witteman, J.C.; Stricker, B.H.; Heeringa, J. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur. Heart J. 2013, 34, 2746–2751. [Google Scholar] [CrossRef] [Green Version]
- Liao, L.-Z.; Wen, X.-Y.; Zhang, S.-Z.; Li, W.-D.; Zhuang, X.-D. Hypertension and Atrial Fibrillation: A Study on Epidemiology and Mendelian Randomization Causality. Front. Cardiovasc. Med. 2021, 8, 644405. [Google Scholar] [CrossRef]
- Bilato, C.; Corti, M.; Baggio, G. Prevalence, Functional Impact, and Mortality of Atrial Fibrillation in an Older Italian Population (from the Pro.V.A. Study). AJC 2009, 104, 1092–1097. [Google Scholar] [CrossRef]
- Di Carlo, A.; Bellino, L.; Consoli, D.; Mori, F.; Zaninelli, A.; Baldereschi, M.; Cattarinussi, A.; D’Alfonso, M.G.; Gradia, C.; Sgherzi, B.; et al. Prevalence of atrial fibrillation in the Italian elderly population and projections from 2020 to 2060 for Italy and the European Union: The FAI Project. EP Eur. 2019, 21, 1468–1475. [Google Scholar] [CrossRef]
- Heeringa, J.; Van Der Kuip, D.A.M.; Hofman, A.; Kors, J.A.; Van Herpen, G.; Stricker, B.H.C.; Stijnen, T.; Lip, G.Y.H.; Witteman, J.C.M. Prevalence, incidence and lifetime risk of atrial fibrillation: The Rotterdam study. Eur. Heart J. 2006, 27, 949–953. [Google Scholar] [CrossRef] [Green Version]
- Adderley, N.J.; Ryan, R.; Nirantharakumar, K.; Marshall, T. Prevalence and treatment of atrial fibrillation in UK general practice from 2000 to 2016. Heart 2019, 105, 27–33. [Google Scholar] [CrossRef]
- Krittayaphong, R.; Rangsin, R.; Thinkhamrop, B.; Hurst, C.; Rattanamongkolgul, S.; Sripaiboonkij, N.; Yindeengam, A. Prevalence and associating factors of atrial fibrillation in patients with hypertension: A nation-wide study. BMC Cardiovasc. Disord. 2016, 16, 57. [Google Scholar] [CrossRef] [Green Version]
- Cucu, M.A.; Cristea, C.; Calomfirescu, C.; Matei, E.; Galan, A.; Ursu, C.; Rădulescu, S.; Georgescu, D. Raport Național Privind Starea de Sănătate a Populației României; Centrul Naţional de Evaluare şi Promovare a Stării de Sănătate (CNEPSS): Bucharest, Romania, 2020. [Google Scholar]
- Huxley, R.R.; Lopez, F.L.; Folsom, A.R.; Agarwal, S.K.; Loehr, L.R.; Soliman, E.Z.; Maclehose, R.; Konety, S.; Alonso, A. Absolute and Attributable Risks of Atrial Fibrillation in Relation to Optimal and Borderline Risk Factors: The Atherosclerosis Risk in Communities (ARIC) study. Circulation 2011, 123, 1501–1508. [Google Scholar] [CrossRef] [Green Version]
- Verdecchia, P.; Staessen, J.A.; Angeli, F.; de Simone, G.; Achilli, A.; Ganau, A.; Mureddu, G.; Pede, S.; Maggioni, A.P.; Lucci, D.; et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): An open-label randomised trial. Lancet 2009, 374, 525–533. [Google Scholar] [CrossRef]
- Jones, N.R.; Taylor, K.J.; Taylor, C.J.; Aveyard, P. Weight change and the risk of incident atrial fibrillation: A systematic review and meta-analysis. Heart 2019, 105, 1799–1805. [Google Scholar] [CrossRef]
- Aldaas, O.M.; Lupercio, F.; Han, F.T.; Hoffmayer, K.S.; Krummen, D.; Ho, G.; Raissi, F.; Birgersdotter-Green, U.; Feld, G.K.; Hsu, J.C. Meta-analysis of Effect of Modest Weight Loss in Management of Overweight and Obese Patients with Atrial Fibrillation. Am. J. Cardiol. 2019, 124, 1568–1574. [Google Scholar] [CrossRef] [PubMed]
- Proietti, M.; Vitolo, M.; Harrison, S.L.; Lane, D.A.; Fauchier, L.; Marin, F.; Nabauer, M.; Potpara, T.S.; Dan, G.-A.; Boriani, G.; et al. Impact of clinical phenotypes on management and outcomes in European atrial fibrillation patients: A report from the ESC-EHRA EURObservational Research Programme in AF (EORP-AF) General Long-Term Registry. BMC Med. 2021, 19, 256. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Ammentorp, B.; Darius, H.; De Caterina, R.; Le Heuzey, J.-Y.; Schilling, R.J.; Schmitt, J.; Zamorano, J.L. Management of atrial fibrillation in seven European countries after the publication of the 2010 ESC Guidelines on atrial fibrillation: Primary results of the PREvention oF thromboemolic events—European Registry in Atrial Fibrillation (PREFER in AF). EP Eur. 2014, 16, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Laroche, C.; Dan, G.-A.; Santini, M.; Kalarus, Z.; Rasmussen, L.H.; Oliveira, M.M.; Mairesse, G.; Crijns, H.J.; Simantirakis, E.; et al. A prospective survey in European Society of Cardiology member countries of atrial fibrillation management: Baseline results of EURObservational Research Programme Atrial Fibrillation (EORP-AF) Pilot General Registry. EP Eur. 2014, 16, 308–319. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): A case-control study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Frison, L.; Grind, M. Effect of hypertension on anticoagulated patients with atrial fibrillation. Eur. Heart J. 2007, 28, 752–759. [Google Scholar] [CrossRef] [Green Version]
- Wu, Y.; Zhang, C.; Gu, Z.-C. Cost-Effectiveness Analysis of Direct Oral Anticoagulants Vs. Vitamin K Antagonists in the Elderly with Atrial Fibrillation: Insights from the Evidence in a Real-World Setting. Front. Cardiovasc. Med. 2021, 8, 675200. [Google Scholar] [CrossRef]
- Marzec, L.N.; Wang, J.; Shah, N.D.; Chan, P.S.; Ting, H.H.; Gosch, K.L.; Hsu, J.C.; Maddox, T.M. Influence of Direct Oral Anticoagulants on Rates of Oral Anticoagulation for Atrial Fibrillation. J. Am. Coll. Cardiol. 2017, 69, 2475–2484. [Google Scholar] [CrossRef]




| All Subjects, n (%) | Hypertensive Subjects, n (%) | Normotensive Subjects, n (%) | p-Value * | |
|---|---|---|---|---|
| Global population | 297 (5.5) | 209 (8.9) | 88 (2.9) | <0.001 |
| Males | 120 (5.2) | 80 (8) | 40 (3.1) | <0.001 |
| Females | 177 (5.7) | 129 (9.5) | 48 (2.7) | <0.001 |
| <40 years | 25 (1.4) | 9 (3.4) | 16 (1.1) | 0.008 |
| 40–60 years | 75 (3.6) | 41 (4.3) | 34 (3) | 0.126 |
| >60 years | 197 (12.6) | 159 (13.9) | 38 (9) | 0.01 |
| Urban residence | 182 (5.8) | 127 (9.6) | 55 (3) | <0.001 |
| Rural residence | 114 (5.1) | 81 (7.9) | 33 (2.7) | <0.001 |
| T2DM | 74 (11.8) | 68 (14.8) | 6 (3.6) | <0.001 |
| Obesity | 192 (7.2) | 143 (10.1) | 49 (3.9) | <0.001 |
| Risk Factor | Hypertensives with AF | Hypertensives without AF | p-Value |
|---|---|---|---|
| Male gender, n (%) | 80 (38.3) | 921 (42.8) | 0.213 |
| Age, mean ± SD | 66.14 ± 12.23 | 56.76 ± 14.30 | <0.001 |
| Urban residence, n (%) | 127 (61.1) | 1201 (55.9) | 0.164 |
| Dyslipidemia, n (%) | 173 (84) | 1749 (82.1) | 0.567 |
| Active smoking, n (%) | 30 (14.5) | 414 (19.7) | 0.079 |
| Obesity, n (%) | 108 (52.2) | 993 (46.5) | 0.126 |
| T2DM, n (%) | 68 (37) | 392 (20.4) | <0.001 |
| OSA history, n (%) | 10 (4.9) | 48 (2.3) | 0.032 |
| Hypertension control, n (%) | 134 (64.7) | 1438 (71) | 0.066 |
| HF diagnosis history, n (%) | 84 (41.6) | 166 (7.9) | <0.001 |
| MI history, n (%) | 27 (13.2) | 96 (4.6) | <0.001 |
| Systolic dysfunction, n (%) | 9 (9.3) | 47 (5.1) | 0.100 |
| Diastolic dysfunction, n (%) | 64 (50.4) | 570 (47.3) | 0.515 |
| LA indexed volume, mean ± SD | 44.65 ± 25.42 | 29.52 ± 10.94 | <0.001 |
| Risk Factor | SEPHAR II | SEPHAR III | SEPHAR IV | p-Value |
|---|---|---|---|---|
| Age | 47.03 ± 15.57 | 48.54 ± 17.49 | 51.19 ± 16.61 | <0.001 |
| Hypertension, n (%) | 798 (40.4) | 889 (45.1) | 680 (46) | 0.001 |
| Obesity, n (%) | 535 (27.4) | 684 (34.7) | 579 (39.6) | <0.001 |
| Visceral obesity, n (%) | 1607 (81.7) | 1462 (74.2) | 1114 (76.2) | <0.001 |
| Smoking, n (%) | 532 (27.1) | 470 (23.9) | 383 (25.9) | 0.059 |
| T2DM, n (%) | 201 (10.2) | 240 (12.2) | 186 (20.2) | <0.001 |
| Dyslipidemia, n (%) | 1438 (73) | 1522 (77.3) | 974 (68) | <0.001 |
| OSA, n (%) | 9 (0.5) | 41 (2.2) | 48 (3.2) | <0.001 |
| History of diagnosed HF, n (%) | 80 (4.2) | 129 (6.5) | 89 (6.1) | 0.004 |
| History of myocardial infarction, n (%) | 44 (2.3) | 70 (3.8) | 42 (2.9) | 0.03 |
| Diastolic dysfunction, n (%) | n/A | 827 (42) | 359 (36.8) | 0.007 |
| Systolic dysfunction, n (%) | n/A | 58 (3.7) | 27 (3.8) | 0.999 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cojocaru, C.; Vîjîiac, A.-E.; Gheorghe-Fronea, O.; Mohaiu, T.; Itu, L.; Dorobanțu, M. Nine-Year Trends in Atrial Fibrillation Prevalence among Romanian Adult Hypertensives: A Post-Hoc Analysis of SEPHAR II-IV Surveys. Int. J. Environ. Res. Public Health 2022, 19, 9250. https://doi.org/10.3390/ijerph19159250
Cojocaru C, Vîjîiac A-E, Gheorghe-Fronea O, Mohaiu T, Itu L, Dorobanțu M. Nine-Year Trends in Atrial Fibrillation Prevalence among Romanian Adult Hypertensives: A Post-Hoc Analysis of SEPHAR II-IV Surveys. International Journal of Environmental Research and Public Health. 2022; 19(15):9250. https://doi.org/10.3390/ijerph19159250
Chicago/Turabian StyleCojocaru, Cosmin, Aura-Elena Vîjîiac, Oana Gheorghe-Fronea, Teodora Mohaiu, Lucian Itu, and Maria Dorobanțu. 2022. "Nine-Year Trends in Atrial Fibrillation Prevalence among Romanian Adult Hypertensives: A Post-Hoc Analysis of SEPHAR II-IV Surveys" International Journal of Environmental Research and Public Health 19, no. 15: 9250. https://doi.org/10.3390/ijerph19159250






