Examining Risk Factors in the Cannabis–Suicide Link: Considering Trauma and Impulsivity among University Students
Abstract
:1. Introduction
The Current Research
- (1)
- Problematic cannabis use would be associated with increased reports of suicidal ideation and suicide attempt.
- (2)
- Impulsive traits would mediate the relationship between higher problematic cannabis use and greater endorsement of suicidal thoughts and behaviors.
- (3)
- Trauma experiences before the age of 18 would moderate the relationship between cannabis use and all suicide outcomes assessed, such that heavier cannabis use would predict greater endorsements of suicide ideation and attempts, especially among those with higher trauma scores (flow diagrams can be found in Supplementary Materials, Figures S1–S3).
2. Methods
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Statistical Analysis
3. Results
3.1. Extent of Suicidal Thoughts and Behaviors
3.2. Problematic Cannabis Use among University Students
3.3. Associations to Problematic Cannabis Use
3.4. Problematic Cannabis Use as a Predictor of Suicidal Outcomes
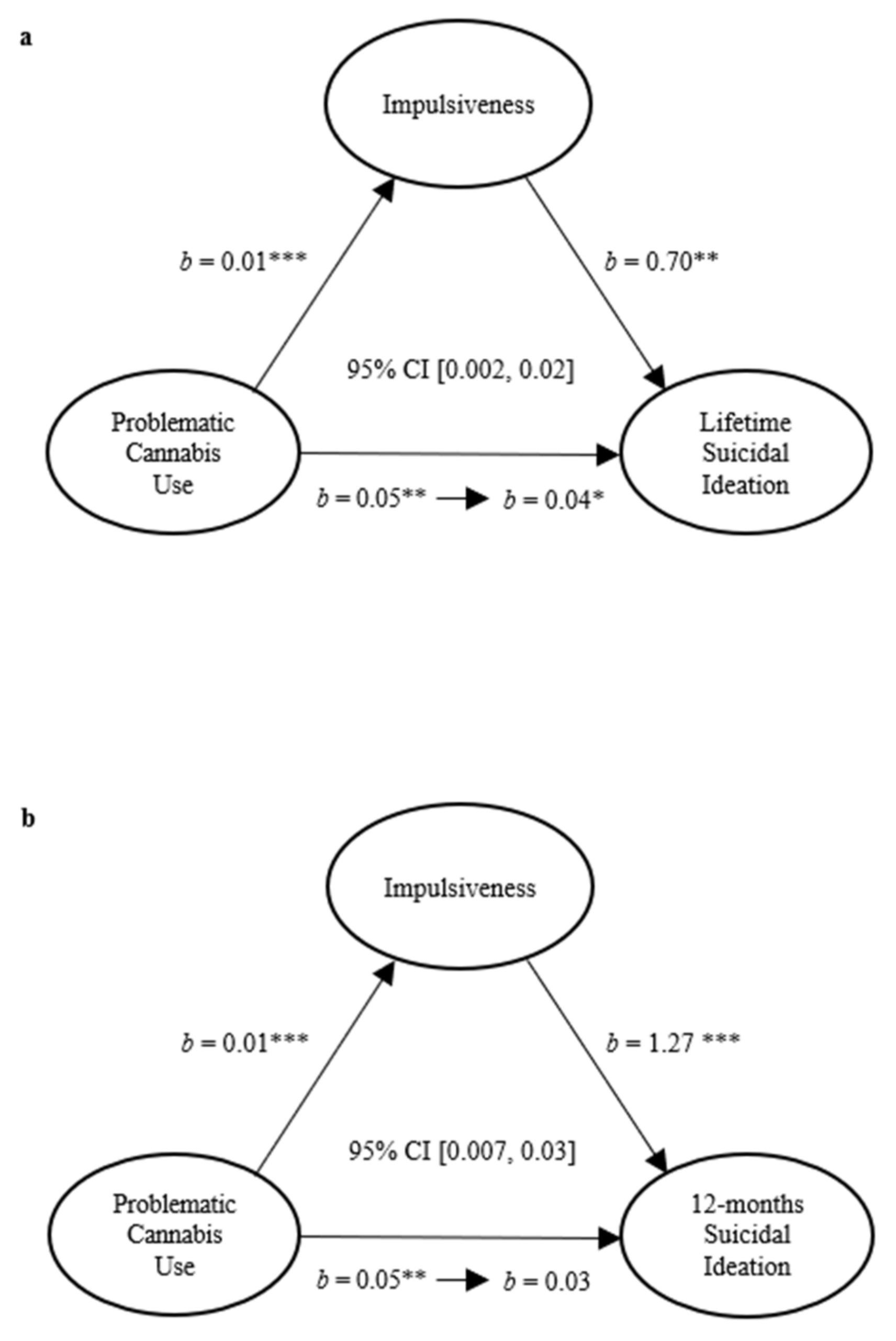
3.5. Mediating Role of Impulsiveness in the Relationship between Problematic Cannabis Use and Suicidal Behaviors
3.6. Moderating Role of Trauma in the Relation between Cannabis Use and Suicide Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Suicide in the World: Global Health Estimates. World Health Organization. License: CC BY-NC-SA 3.0 IGO. 2019. Available online: https://apps.who.int/iris/handle/10665/326948 (accessed on 21 October 2021).
- Ferrari, A.J.; Norman, R.E.; Freedman, G.; Baxter, A.J.; Pirkis, J.E.; Harris, M.G.; Page, A.; Carnahan, E.; Degenhardt, L.; Vos, T.; et al. The burden attributable to mental and substance use disorders as risk factors for suicide: Findings from the global burden of disease study 2010. PLoS ONE 2014, 9, e91936. [Google Scholar] [CrossRef]
- Sheldon, E.; Simmonds-Buckley, M.; Bone, C.; Mascarenhas, T.; Chan, N.; Wincott, M.; Gleeson, H.; Sow, K.; Hind, D.; Barkham, M. Prevalence and risk factors for mental health problems in university undergraduate students: A systematic review with meta-analysis. J. Affect. Disord. 2021, 287, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Stevens, C.; Wong, S.H.M.; Yasui, M.; Chen, J.A. The prevalence and predictors of mental health diagnoses and suicide among U.S. college students: Implications for addressing disparities in service use. J. Depress. Anxiety 2019, 36, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Batty, G.D.; Kivimäki, M.; Bell, S.; Gale, C.R.; Shipley, M.; Whitley, E.; Gunnell, D. Psychosocial characteristics as potential predictors of suicide in adults: An overview of the evidence with new results from prospective cohort studies. Transl. Psychiatry 2018, 8, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wasserman, D.; Iosue, M.; Wuestefeld, A.; Carli, V. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World J. Psychiatry 2020, 19, 294–306. [Google Scholar] [CrossRef]
- Mars, B.; Heron, J.; Klonsky, E.D.; Moran, P.; O’Connor, R.C.; Tilling, K.; Wilkinson, P.; Gunnell, D. Predictors of Future Suicide Attempt among Adolescents with Suicidal Thoughts or Non-Suicidal Self-Harm: A Population-Based Birth Cohort Study. Lancet Psychiatry 2019, 6, 327–337. [Google Scholar] [CrossRef] [Green Version]
- Mortier, P.; Cuijpers, P.; Kiekens, G.; Auerbach, R.P.; Demyttenaere, K.; Green, J.G.; Kessler, R.C.; Nock, M.K.; Bruffaerts, R. The prevalence of suicidal thoughts and behaviours among college students: A meta-analysis. Psychol. Med. 2018, 48, 554–565. [Google Scholar] [CrossRef]
- Han, B.; Compton, W.M.; Einstein, E.B.; Volkow, N.D. Associations of suicidality trends with cannabis use as a function of sex and depression status. JAMA Netw. Open 2021, 4, e2113025. [Google Scholar] [CrossRef]
- Campeny, E.; López-Pelayo, H.; Nutt, D.; Blithikioti, C.; Oliveras, C.; Nuño, L.; Maldonado, R.; Florez, G.; Arias, F.; Fernández-Artamendi, S.; et al. The blind men and the elephant: Systematic review of systematic reviews of cannabis use related health harms. Eur. Neuropsychopharmacol. 2020, 33, 1–35. [Google Scholar] [CrossRef]
- Hammond, D.; Goodman, S.; Wadsworth, E.; Rynard, V.; Boudreau, C.; Hall, W. Evaluating the impacts of cannabis legalization: The International Cannabis Policy Study. Int. J. Drug Policy 2020, 77, e102698. [Google Scholar] [CrossRef]
- Pacek, L.R.; Weinberger, A.H.; Zhu, J.; Goodwin, R.D. Rapid increase in the prevalence of cannabis use among people with depression in the United States, 2005–2017: The role of differentially changing risk perceptions. Addiction 2020, 115, 935–943. [Google Scholar] [CrossRef]
- American College Health Association. American College Health Association—National College Health Assessment II: Canadian Consortium Executive Summary Spring. 2019. Available online: https://www.cacuss.ca/files/Research/NCHA-II%20SPRING%202019%20CANADIAN%20REFERENCE%20GROUP%20EXECUTIVE%20SUMMARY.pdf (accessed on 7 October 2021).
- Buckner, J.D.; Lemke, A.W.; Walukevich, K.A. Cannabis use and suicidal ideation: Test of the utility of the Interpersonal-Psychological Theory of Suicide. Psychiatry Res. 2017, 253, 256–259. [Google Scholar] [CrossRef]
- Tabet, A.C.; Meyer, D.G.; Carrisalez, C.; Martinez, J.; Diaz, R.P. The consequences of cannabis use: A review of self-reported use and experiences among college students. J. Dr. Nurs. Pract. 2020, 13, 229–234. [Google Scholar] [CrossRef]
- Mannekote Thippaiah, S.; Iyengar, S.S.; Vinod, K.Y. Exo- and endo-cannabinoids in depressive and suicidal behaviors. Front. Psychiatry 2021, 12, e636228. [Google Scholar] [CrossRef]
- Guvendeger Doksat, N.; Zahmacioglu, O.; Ciftci Demirci, A.; Kocaman, G.M.; Erdogan, A. Association of suicide attempts and non-suicidal self-injury behaviors with substance use and family characteristics among children and adolescents seeking treatment for substance use disorder. Subst. Use Misuse 2017, 52, 604–613. [Google Scholar] [CrossRef]
- Bolanis, D.; Orri, M.; Castellanos-Ryan, N.; Renaud, J.; Montreuil, T.; Boivin, M.; Vitaro, F.; Tremblay, R.E.; Turecki, G.; Côté, S.M.; et al. Cannabis use, depression and suicidal ideation in adolescence: Direction of associations in a population based cohort. J. Affect. Disord. 2020, 274, 1076–1083. [Google Scholar] [CrossRef]
- Gobbi, G.; Atkin, T.; Zytynski, T.; Wang, S.; Askari, S.; Boruff, J.; Ware, M.; Marmorstein, N.; Cipriani, A.; Dendukuri, N.; et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: A systematic review and meta-analysis. JAMA Psychiatry 2019, 76, 426–434. [Google Scholar] [CrossRef]
- Lopez-Quintero, C.; de los Cobos, J.P.; Hasin, D.S.; Okuda, M.; Wang, S.; Grant, B.F.; Blanco, C. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Drug Alcohol Depend. 2011, 115, 120–130. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, A.; Nelson, E.C.; Bucholz, K.K.; Tillman, R.; Grucza, R.A.; Statham, D.J.; Madden, P.A.; Martin, N.G.; Heath, A.C.; Lynskey, M.T. Major depressive disorder, suicidal thoughts and behaviours, and cannabis involvement in discordant twins: A retrospective cohort study. Lancet Psychiatry 2017, 4, 706–714. [Google Scholar] [CrossRef]
- Hengartner, M.P.; Angst, J.; Ajdacic-Gross, V.; Rössler, W. Cannabis use during adolescence and the occurrence of depression, suicidality and anxiety disorder across adulthood: Findings from a longitudinal cohort study over 30 years. J. Affect. Disord. 2020, 272, 98–103. [Google Scholar] [CrossRef]
- Orri, M.; Séguin, J.R.; Castellanos-Ryan, N.; Tremblay, R.E.; Côté, S.M.; Turecki, G.; Geoffroy, M.C. A genetically informed study on the association of cannabis, alcohol, and tobacco smoking with suicide attempt. Mol. Psychiatry 2020, 26, 5061–5070. [Google Scholar] [CrossRef]
- Naji, L.; Rosic, T.; Dennis, B.; Bhatt, M.; Sanger, N.; Hudson, J.; Mouravska, N.; Thabane, L.; Samaan, Z. The association between cannabis use and suicidal behavior in patients with psychiatric disorders: An analysis of sex differences. Biol. Sex Differ. 2018, 9, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lynskey, M.T.; Glowinski, A.L.; Todorov, A.A.; Bucholz, K.K.; Madden, P.A.F.; Nelson, E.C.; Statham, D.J.; Martin, N.G. Major depressive disorder, suicidal ideation, and suicide attempt in twins discordant for cannabis dependence and early-onset cannabis use. Arch. Gen. Psychiatry 2004, 61, 1026–1032. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delforterie, M.J.; Lynskey, M.T.; Huizink, A.C.; Creemers, H.E.; Grant, J.D.; Few, L.R.; Glowinski, A.L.; Statham, D.J.; Trull, T.J.; Bucholz, K.K.; et al. The relationship between cannabis involvement and suicidal thoughts and behaviors. Drug Alcohol Depend. 2015, 150, 98–104. [Google Scholar] [CrossRef] [Green Version]
- Agrawal, A.; Lynskey, M.T. Cannabis controversies: How genetics can inform the study of comorbidity. Addiction 2014, 109, 360–370. [Google Scholar] [CrossRef]
- Bartoli, F.; Lev-Ran, S.; Crocamo, C.; Carrà, G. the interplay between cannabis use and suicidal behaviours: Epidemiological overview, psychopathological and clinical models. Psychopathology 2018, 24, 180–186. [Google Scholar]
- Kelly, L.M.; Drazdowski, T.K.; Livingston, N.R.; Zajac, K. Demographic risk factors for co-occurring suicidality and cannabis use disorders: Findings from a nationally representative United States sample. Addict. Behav. 2021, 122, e107047. [Google Scholar] [CrossRef] [PubMed]
- Round, J.T.; Fozard, T.E.; Harrison, A.A.; Kolokotroni, K.Z. Disentangling the effects of cannabis and cigarette smoking on impulsivity. J. Psychopharmacol. 2020, 34, 955–968. [Google Scholar] [CrossRef]
- McHugh, C.M.; Chun Lee, R.S.; Hermens, D.F.; Corderoy, A.; Large, M.; Hickie, I.B. Impulsivity in the self-harm and suicidal behavior of young people: A systematic review and meta-analysis. J. Psychiatr. Res. 2019, 116, 51–60. [Google Scholar] [CrossRef]
- O’Donnell, B.F.; Skosnik, P.D.; Hetrick, W.P.; Fridberg, D.J. Decision making and impulsivity in young adult cannabis users. Front. Psychol. 2021, 12, e679904. [Google Scholar] [CrossRef]
- Klonsky, E.D.; May, A. Rethinking impulsivity in suicide. Suicide Life Threat. Behav. 2010, 40, 612–619. [Google Scholar] [CrossRef]
- Oquendo, M.A.; Sullivan, G.M.; Sudol, K.; Baca-Garcia, E.; Stanley, B.H.; Sublette, M.E.; Mann, J.J. Toward a biosignature for suicide. Am. J. Psychiatry 2014, 171, 1259–1277. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, K.; Chartier, K.G.; Wike, T.L.; McDonald, S.E. Adverse childhood experience patterns, major depressive disorder, and substance use disorder in older adults. Aging Ment. Health 2021, 25, 484–491. [Google Scholar] [CrossRef]
- Hinojosa, R.; Nguyen, J.; Sellers, K.; Elassar, H. Barriers to college success among students that experienced adverse childhood events. J. Am. Coll. Health 2019, 67, 531–540. [Google Scholar] [CrossRef]
- Vrana, S.; Lauterbach, D. Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. J. Trauma Stress 1994, 7, 289–302. [Google Scholar] [CrossRef]
- Afifi, T.O.; MacMillan, H.L.; Taillieu, T.; Turner, S.; Cheung, K.; Sareen, J.; Boyle, M.H. Individual- and relationship-level factors related to better mental health outcomes following child abuse: Results from a nationally representative Canadian sample. Can. J. Psychiatry 2016, 61, 776–788. [Google Scholar] [CrossRef] [Green Version]
- Angelakis, I.; Gillespie, E.L.; Panagioti, M. Childhood maltreatment and adult suicidality: A comprehensive systematic review with meta-analysis. Psychol. Med. 2019, 49, 1057–1078. [Google Scholar] [CrossRef] [Green Version]
- Franklyn, S.I.; Stewart, J.; Beaurepaire, C.; Thaw, E.; McQuaid, R.J. Developing symptom clusters: Linking inflammatory biomarkers to depressive symptom profiles. Transl. Psychiatry 2022, 12, 133. [Google Scholar] [CrossRef]
- Adamson, S.J.; Kay-Lambkin, F.J.; Baker, A.L.; Lewin, T.J.; Thornton, L.; Kelly, B.J.; Sellman, J.D. An improved brief measure of cannabis misuse: The Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug Alcohol Depend. 2010, 110, 137–143. [Google Scholar] [CrossRef]
- Bruno, R.; Marshall, S.; Adamson, S. Screening for DSM-5 Cannabis Dependence Using the Cannabis Use Identification Test–Revised. National Institute on Drug Abuse (NIDA). Available online: https://nida.nih.gov/international/abstracts/screening-dsm-5-cannabis-dependence-using-cannabis-use-identification-test-revised (accessed on 8 February 2022).
- Marshall, S. The Cannabis Use Disorder Identification Test—Revised (CUDIT-R): Categorisation and Interpretation. Master’s Thesis, University of Tasmania, Brisbane, Australia, 2012. [Google Scholar]
- Patton, J.H.; Stanford, M.S.; Barratt, E.S. Factor Structure of the Barratt Impulsiveness Scale. J. Clin. Psychol. 1995, 51, 768–774. [Google Scholar] [CrossRef]
- Stanford, M.S.; Mathias, C.W.; Dougherty, D.M.; Lake, S.L.; Anderson, N.E.; Patton, J.H. Fifty years of the Barratt Impulsiveness Scale: An update and review. Pers. Individ. Differ. 2009, 47, 385–395. [Google Scholar] [CrossRef]
- Bernstein, D.P.; Stein, J.A.; Newcomb, M.D.; Walker, E.; Pogge, D.; Ahluvalia, T.; Stokes, J.; Handelsman, L.; Medrano, M.; Desmond, D.; et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003, 27, 169–190. [Google Scholar] [CrossRef]
- Bernstein, D.P.; Ahluvalia, T.; Pogge, D.; Handelsman, L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 340–348. [Google Scholar] [CrossRef]
- Kessler, R.C.; Üstün, B.B. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int. J. Methods Psychiatr. Res. 2004, 13, 93–117. [Google Scholar] [CrossRef]
- Hayes, A.F. Partial, conditional, and moderated mediation: Quantification, inference, and interpretation. Commun. Monogr. 2018, 85, 4–40. [Google Scholar] [CrossRef]
- Serafini, G.; Pompili, M.; Innamorati, M.; Temple, E.C.; Amore, M.; Borgwardt, S.; Girardi, P. the association between cannabis use, mental illness, and suicidal behavior: What is the role of hopelessness? Front. Psychiatry 2013, 4, 125. [Google Scholar] [CrossRef] [Green Version]
- Health Canada. 2019 Canadian Cannabis Survey (CCS). Available online: https://publications.gc.ca/collections/collection_2019/sc-hc/H21-312-2019-2-eng.pdf (accessed on 29 October 2021).
- Leung, J.; Chan, G.C.K.; Hides, L.; Hall, W.D. What is the prevalence and risk of cannabis use disorders among people who use cannabis? A systematic review and meta-analysis. Addict. Behav. 2020, 109, e106479. [Google Scholar] [CrossRef]
- Diep, C.; Bhat, V.; Wijeysundera, D.N.; Clarke, H.A.; Ladha, K.S. The association between recent cannabis use and suicidal ideation in adults: A population-based analysis of the NHANES from 2005 to 2018. Can. J. Psychiatry 2021, 67, 259–267. [Google Scholar] [CrossRef]
- Gorfinkel, L.R.; Stohl, M.; Hasin, D. Association of depression with past-month cannabis use among us adults aged 20 to 59 years, 2005 to 2016. JAMA Netw. Open 2020, 3, e2013802. [Google Scholar] [CrossRef]
- Fuller-Thomson, E.; Jayanthikumar, J.; Redmond, M.L.; Agbeyaka, S. Is recovery from cannabis dependence possible? Factors that help or hinder recovery in a national sample of Canadians with a history of cannabis dependence. Adv. Prev. Med. 2020, 2020, e9618398. [Google Scholar] [CrossRef] [Green Version]
- Bagge, C.L.; Borges, G. Acute Substance Use as a Warning Sign for Suicide Attempts: A Case-Crossover Examination of the 48 Hours Prior to a Recent Suicide Attempt. J. Clin. Psychiatry 2017, 78, 691–696. [Google Scholar] [CrossRef]
- Womack, S.R.; Shaw, D.S.; Weaver, C.M.; Forbes, E.E. Bidirectional associations between cannabis use and depressive symptoms from adolescence through early adulthood among at-risk young men. J. Stud. Alcohol Drugs 2016, 77, 287. [Google Scholar] [CrossRef] [Green Version]
- McLaughlin, R.J.; Hill, M.N.; Gorzalka, B.B. A critical role for prefrontocortical endocannabinoid signaling in the regulation of stress and emotional behavior. Neurosci. Biobehav. Rev. 2014, 42, 116–131. [Google Scholar] [CrossRef]
- Morena, M.; Patel, S.; Bains, J.S.; Hill, M.N. Neurobiological interactions between stress and the endocannabinoid system. Neuropsychopharmacology 2016, 41, 80–102. [Google Scholar] [CrossRef] [Green Version]
- Herranz-Herrer, J.; Gil-Benito, E.; Ponte-López, T.; Ortega-Gutiérrez, S.; Macicior, J.; Rosado-Garcia, S.; Sánchez-López, A.J.; Blasco-Fontecilla, H. Serum Endocannabinoid levels in suicide attempters: A pilot study. Eur. Neuropsychopharmacol. 2020, 40, 52–60. [Google Scholar] [CrossRef]
- Van Orden, K.A.; Witte, T.K.; Cukrowicz, K.C.; Braithwaite, S.R.; Selby, E.A.; Joiner, T.E., Jr. The Interpersonal Theory of Suicide. Psychol. Rev. 2010, 117, 575–600. [Google Scholar] [CrossRef] [Green Version]
- Cicchetti, D.; Handley, E.D. Child maltreatment and the development of substance use and disorder. Neurobiol. Stress 2019, 10, 100144. [Google Scholar] [CrossRef]
- Frydecka, D.; Misiak, B.; Kotowicz, K.; Pionke, R.; Krężołek, M.; Cechnicki, A.; Gawęda, Ł. The interplay between childhood trauma, cognitive biases, and cannabis use on the risk of psychosis in nonclinical young adults in Poland. Eur. Psychiatry 2020, 63, e35. [Google Scholar] [CrossRef]
- Morris, V.L.; Huffman, L.G.; Naish, K.R.; Holshausen, K.; Oshri, A.; McKinnon, M.; Amlung, M. Impulsivity as a mediating factor in the association between posttraumatic stress disorder symptoms and substance use. Psychol. Trauma Theory 2020, 12, 659–668. [Google Scholar] [CrossRef]
- Braquehais, M.D.; Oquendo, M.A.; Baca-García, E.; Sher, L. Is impulsivity a link between childhood abuse and suicide? Compr. Psychiatry 2010, 51, 121–129. [Google Scholar] [CrossRef]
- Rodríguez-Cintas, L.; Daigre, C.; Braquehais, M.D.; Palma-Alvarez, R.F.; Grau-López, L.; Ros-Cucurull, E.; Rodríguez-Martos, L.; Abad, A.C.; Roncero, C. Factors associated with lifetime suicidal ideation and suicide attempts in outpatients with substance use disorders. Psychiatry Res. 2018, 262, 440–445. [Google Scholar] [CrossRef]
- Roy, A. Childhood trauma and impulsivity. Possible relevance to suicidal behavior. Arch. Suicide Res. 2005, 9, 147–151. [Google Scholar] [CrossRef]
- Jardim, G.B.G.; Novelo, M.; Spanemberg, L.; von Gunten, A.; Engroff, P.; Nogueira, E.L.; Neto, A.C. Influence of childhood abuse and neglect subtypes on late-life suicide risk beyond depression. Child Abuse Negl. 2018, 80, 249–256. [Google Scholar] [CrossRef]
- Ihme, H.; Olié, E.; Courtet, P.; El-Hage, W.; Zendjidjian, X.; Mazzola-Pomietto, P.; Consoloni, J.-L.; Deruelle, C.; Belzeaux, R. Childhood trauma increases vulnerability to attempt suicide in adulthood through avoidant attachment. Compr. Psychiatry 2022, 117, 152333. [Google Scholar] [CrossRef]
- Bahk, Y.C.; Jang, S.K.; Choi, K.H.; Lee, S.H. The relationship between childhood trauma and suicidal ideation: Role of maltreatment and potential mediators. Psychiatry Investig. 2017, 14, 37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertule, M.; Sebre, S.B.; Kolesovs, A. Childhood abuse experiences, depression and dissociation symptoms in relation to suicide attempts and suicidal ideation. J. Trauma Dissociation 2021, 22, 598–614. [Google Scholar] [CrossRef]
- De Araújo, R.M.F.; Lara, D.R. More than words: The association of childhood emotional abuse and suicidal behavior. Eur. Psychiatry 2016, 37, 14–21. [Google Scholar] [CrossRef]
- McQuaid, R.J.; Nikolitch, K.; Vandeloo, K.L.; Burhunduli, P.; Phillips, J.L. Sex differences in determinants of suicide risk preceding psychiatric admission: An electronic medical record study. Front. Psychiatry 2022, 13, 892225. [Google Scholar] [CrossRef] [PubMed]
- Shalit, N.; Shoval, G.; Shlosberg, D.; Feingold, D.; Lev-Ran, S. The association between cannabis use and suicidality among men and women: A population-based longitudinal study. J. Affect. Disord. 2016, 205, 216–224. [Google Scholar] [CrossRef]
- Doucette, M.L.; Borrup, K.T.; Lapidus, G.; Whitehill, J.M.; McCourt, A.D.; Crifasi, C.K. Effect of Washington State and Colorado’s cannabis legalization on death by suicides. Prev. Med. 2021, 148, e106548. [Google Scholar] [CrossRef] [PubMed]
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Problematic cannabis use | - | ||||||||
| 2. Lifetime SI | 0.13 ** | - | |||||||
| 3. Past-12-months SI | 0.13 ** | 0.56 ** | - | ||||||
| 4. Lifetime SA | 0.13 ** | 0.36 ** | 0.40 ** | - | |||||
| 5. Childhood trauma | 0.11 * | 0.35 ** | 0.34 ** | 0.33 ** | - | ||||
| 6. Impulsiveness total | 0.18 ** | 0.14 ** | 0.21 ** | 0.09 | 0.16 ** | - | |||
| 7. Attentional | 0.20 ** | 0.23 ** | 0.27 ** | 0.15 ** | 0.21 ** | 0.72 ** | - | ||
| 8. Motor | 0.16 ** | 0.04 | 0.10 * | 0.02 | 0.11 * | 0.79 ** | 0.37 ** | - | |
| 9. Nonplanning | 0.09 * | 0.06 | 0.13 ** | 0.04 | 0.07 | 0.82 ** | 0.36 ** | 0.49 ** | - |
| Wald | b (SE) | OR | 95% CI | p | R2 | |
|---|---|---|---|---|---|---|
| Lifetime SI | 8.62 | 0.05(0.02) | 1.05 | 1.02, 1.09 | 0.003 | 0.02 |
| Past-12-Months SI | 8.00 | 0.05(0.02) | 1.05 | 1.02, 1.08 | 0.005 | 0.02 |
| Lifetime SA | 8.00 | 0.05(0.02) | 1.06 | 1.02, 1.10 | 0.005 | 0.03 |
| Wald | b (SE) | OR | 95% CI | p | R2 | |
|---|---|---|---|---|---|---|
| Lifetime SI | ||||||
| Impulsiveness | 10.25 | 0.81 (0.25) | 2.26 | 1.37, 3.71 | 0.001 | 0.03 |
| Attentional | 25.69 | 0.98 (0.19) | 2.67 | 1.82, 3.90 | <0.001 | |
| Motor | 0.67 | −0.21 (0.26) | 0.81 | 0.48, 1.35 | 0.41 | 0.07 |
| Nonplanning | 0.02 | −0.03 (0.23) | 0.97 | 0.62, 1.52 | 0.90 | |
| Past-12-Months SI | ||||||
| Impulsiveness | 22.11 | 1.36 (0.29) | 3.90 | 2.21, 6.89 | <0.001 | 0.06 |
| Attentional | 29.14 | 1.16 (0.22) | 3.20 | 2.10, 4.88 | <0.001 | |
| Motor | 0.11 | −0.10 (0.29) | 0.91 | 0.51, 1.61 | 0.74 | 0.11 |
| Nonplanning | 0.73 | 0.22 (0.26) | 1.25 | 0.75, 2.09 | 0.39 | |
| Lifetime SA | ||||||
| Impulsiveness | 3.80 | 0.72 (0.37) | 2.05 | 1.00, 4.23 | 0.05 | 0.01 |
| Attentional | 11.52 | 0.92 (0.27) | 2.50 | 1.47, 4.24 | 0.001 | |
| Motor | 0.54 | −0.28 (0.39) | 0.75 | 0.35, 1.61 | 0.46 | 0.04 |
| Nonplanning | 0.001 | 0.01 (0.34) | 1.01 | 0.52, 1.96 | 0.98 | |
| Wald | b (SE) | OR | 95% CI | p | R2 | |
|---|---|---|---|---|---|---|
| Childhood trauma | ||||||
| Lifetime SI | 54.05 | 0.08 (0.01) | 1.08 | 1.06, 1.10 | <0.001 | 0.18 |
| Past-12-Months SI | 48.27 | 0.06 (0.01) | 1.06 | 1.04, 1.08 | <0.001 | 0.15 |
| Lifetime SA | 43.31 | 0.06 (0.01) | 1.07 | 1.05, 1.08 | <0.001 | 0.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daneshmend, A.Z.B.; Stewart, J.; Jarkas, D.A.; Franklyn, S.I.; Gabrys, R.L.; Patterson, Z.R.; Abizaid, A.; Hellemans, K.G.C.; McQuaid, R.J. Examining Risk Factors in the Cannabis–Suicide Link: Considering Trauma and Impulsivity among University Students. Int. J. Environ. Res. Public Health 2022, 19, 9307. https://doi.org/10.3390/ijerph19159307
Daneshmend AZB, Stewart J, Jarkas DA, Franklyn SI, Gabrys RL, Patterson ZR, Abizaid A, Hellemans KGC, McQuaid RJ. Examining Risk Factors in the Cannabis–Suicide Link: Considering Trauma and Impulsivity among University Students. International Journal of Environmental Research and Public Health. 2022; 19(15):9307. https://doi.org/10.3390/ijerph19159307
Chicago/Turabian StyleDaneshmend, Ayeila Z. B., Jayme Stewart, Dana A. Jarkas, Sabina I. Franklyn, Robert L. Gabrys, Zachary R. Patterson, Alfonso Abizaid, Kim G. C. Hellemans, and Robyn J. McQuaid. 2022. "Examining Risk Factors in the Cannabis–Suicide Link: Considering Trauma and Impulsivity among University Students" International Journal of Environmental Research and Public Health 19, no. 15: 9307. https://doi.org/10.3390/ijerph19159307
APA StyleDaneshmend, A. Z. B., Stewart, J., Jarkas, D. A., Franklyn, S. I., Gabrys, R. L., Patterson, Z. R., Abizaid, A., Hellemans, K. G. C., & McQuaid, R. J. (2022). Examining Risk Factors in the Cannabis–Suicide Link: Considering Trauma and Impulsivity among University Students. International Journal of Environmental Research and Public Health, 19(15), 9307. https://doi.org/10.3390/ijerph19159307






